Highlights
-
•
Subjective cognitive complaints predict sickness absence.
-
•
Age and prior absence also predict sickness absence in an additive fashion.
-
•
Maintenance of resources is important in knowledge-intensive occupations.
Keywords: Subjective cognitive complaints, Screening questionnaire, Occupational healthcare, Self-reported data, Sickness allowance, Register data
Abstract
Knowledge-intensive work requires capabilities like monitoring multiple sources of information, prioritizing between competing tasks, switching between tasks, and resisting distraction from the primary task(s). We assessed whether subjective cognitive complaints (SCC), presenting as self-rated problems with difficulties of concentration, memory, clear thinking and decision making predict sickness absence (SA) in knowledge-intensive occupations. We combined SCC questionnaire results with reliable registry data on SA of 7743 professional/managerial employees (47% female). We excluded employees who were not active in working life, on long-term SA, and those on a work disability benefit at baseline. The exposure variable was the presence of SCC. Age and SA before the questionnaire as a proxy measure of general health were treated as confounders and the analyses were conducted by gender. The outcome measure was the accumulated SA days during a 12-month follow-up. We used a hurdle model to analyse the SA data. SCC predicted the number of SA days during the 12-month follow-up. The ratio of the means of SA days was higher than 2.8 as compared to the reference group, irrespective of gender, with the lowest limit of 95% confidence interval 2.2. In the Hurdle model, SCC, SA days prior to the questionnaire, and age were additive predictors of the likelihood of SA and accumulated SA days, if any. Subjective cognitive complaints predict sickness absence in knowledge-intensive occupations, irrespective of gender, age, or general health. This finding has implications for supporting work ability (productivity) among employees with cognitively demanding tasks.
1. Introduction
Subjective cognitive complaints (SCC) are comprehended as difficulties of concentration, memory, clear thinking and decision making (Stenfors et al., 2013a, Stenfors et al., 2013b). SCC involve problems with mental executive capacity to monitor multiple sources of data, prioritize competing tasks, switch between tasks, and resist distraction from the task. All these are also associated with impairment of work ability (WA) (Barbe et al., 2018). SCC often co-occur with other common psychological health problems, including chronic stress, exhaustion, sleeping problems, and depression (Stenfors et al., 2013a). The prevalence of SCC increases by age (Burmester et al., 2016). Among older employees, the contributors to cognitive decline include disease burden, e.g., depressive symptoms and poor sleep quality (LaMonica et al., 2019). It has also been suggested that SCC reduce WA in phases that are not yet characterized by clinical illness (Aasvik et al., 2015), but compelling evidence is scarce.
Sickness absence (SA) causes a considerable burden both on an individual level and in the societal context. The OECD countries spend approximately 2% of their gross domestic product (GDP) on sickness benefits (Organisation for Economic Co-operation and Development, (OECD), 2010). The average rates of SA of working time across Europe vary between 3% and 6%. In Finland, SA accounts for 4.3% (9.9 days) of work time (Edwards & Greasley, 2010). A Eurofound study estimated that the cost of absences was approximately 20 billion euros in Finland, a country with a labour force of 2.4 million, in 2010 (Edwards & Greasley, 2010).
SA is a complex, multifactorial phenomenon determined by personal, socio-demographical, lifestyle- and health-related factors. Other factors such as the role of the health care system, legislation, and organizations’ physical and psychosocial risk factors also play a role in SA (Janssens et al., 2014, Loisel et al., 2001, Szubert et al., 2016). Psychosocial risks have been recognized as causing poor health and SA (Catalina-Romero et al., 2015, Clausen et al., 2014, Janssens et al., 2014, Strømholm et al., 2015, Sundstrup et al., 2018), also in the Finnish setting (Hinkka et al., 2013, Laaksonen et al., 2010, Väänänen et al., 2004). However, as employees need a medical certificate to qualify for SA in Finland (Social Insurance Institution of Finland, 2017), the immediate reason for SA is always labelled as a medical diagnosis.
The aim of the present study was to assess weather SCC predict SA. We evaluated how a SCC questionnaire used in clinical practice to recognize early phase cognitive impairment (Ahveninen et al., 2014) predicts SA among respondents from various knowledge-intensive, sedentary occupations. We considered the potential confounding effects of gender, age, and prior SA days as a proxy measure of general health. Our underlining hypothesis was that SCC, indicating hampered cognition in demanding tasks, predicts SA.
2. Materials and methods
2.1. Study design, ethics and setting
The study design was a retrospective analysis of prospectively collected register data. We had access to a large nationwide database of one occupational health service (OHS) provider, which included both responses to the questionnaire and registry data on SA.
The Tampere University Research Ethics Board approved the study (ETL-code R16074), and it was conducted in accordance with the Declaration of Helsinki. We strictly adhered to data privacy.
The study setting was OHS in Finland within the context of Finnish SA legislation. In most cases, permanent employees are paid a full salary from the first day of their SA, for up to three months. After ten working days, an employer receives sickness allowance from the Kela (The Social Insurance Institution of Finland), which is a state institution that manages the basic security of people living in Finland in different life situations. The sickness allowance is provided based on an application, in which the employer reports the data concerning SA periods and dates. After three months employee starts to receive sickness allowance from Kela and salary is no longer paid by the employers. An employee receives Kela sickness allowance for a maximum of one year of work disability from the same illness. If work disability lasts for longer than one year, the responsibility of providing benefits shifts to pension insurance companies. Therefore, in the present study, the primary outcome was defined as SA days during the 12-month follow-up after the questionnaire.
2.2. Participants
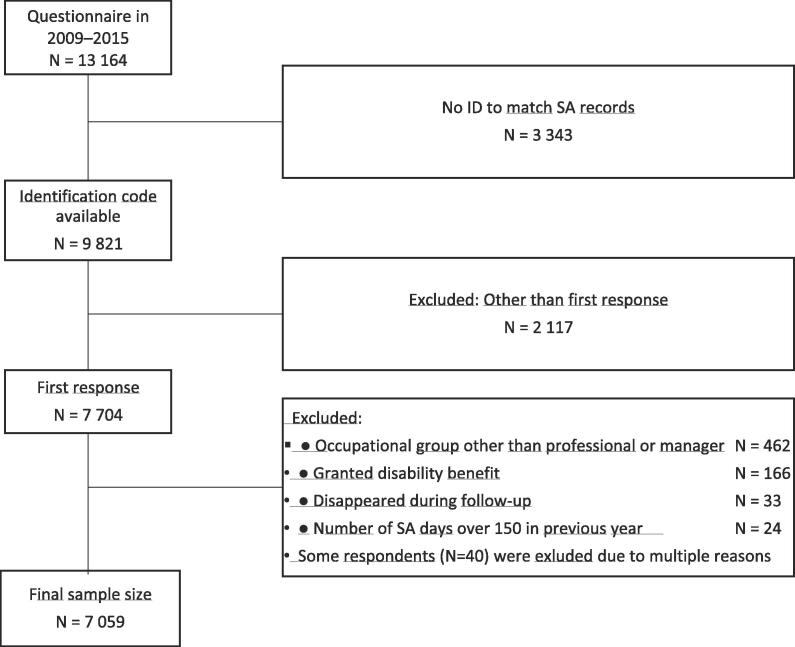
The study participants were professional and managerial employees aged 18–68 years, who had completed a questionnaire (N = 13 164) during 2009–2015 as a part of nationwide OHS services in one particular service provider. The archival data of SA covered years 2008–2016. Fig. 1 illustrates the study flow.
Fig. 1.
Study flow.
The questionnaire was completed as a part of an occupational health surveillance program. Usually, occupational health surveillance is conducted every three years, and some of the employees had participated in multiple surveillances during 2008–2016. Exclusion criteria were unknown identification code (N = 3343), other than first response (N = 2087), previously granted permanent disability benefit (N = 81), and another occupational group than a professional/manager (N = 462).
The final sample size was N = 7059. The exact response rate is not available, because the exact number of invitations was not available in the registry data. In a previous cohort study with the same instrument, the response rate was 64% (Ahveninen et al., 2019). In the present study the participants were mainly from the information and communication industries (47%); professional, scientific and technical activities (23%); public administration; defence and compulsory social security (9%); and education (7%) (Finland. Tilastokeskus, 1979). The corresponding figures in Finland, according to official statistics, are 4%, 11%, 7% and 11% (Findicator, 2018).
2.3. Questionnaire
The online questionnaire is used in Finland as a part of preventive OHS by one nationwide provider to recognize employees at risk of exhaustion and to target interventions for those in need. The questionnaire includes a set of nine screening questions, derived from various theoretical frameworks, assessing psychosocial workload and individual resources for coping. If any of the trigger questions indicates potential psychosocial problems at work, seven additional questions concerning cognitive function are asked. Table 1 shows the topics and cut-off limits of the trigger questions.
Table 1.
Topics and cut-off limits for the trigger questions.
| Topic | Cut-off limits* |
|---|---|
|
≥45 h/week. |
|
Continuous perception of pressure and job strain. |
|
Completely disagree. |
|
With the current working tempo, individual resources remain adequate at the maximum for another 6 months. |
|
The last time when felt well and energized was already over 3 months ago. |
|
Poor. |
|
Feeling overloaded, but able to cope. |
|
Three or less on a scale from 1 to 10 (1 = extremely tired, 10 = extremely energetic). |
|
At least three nights per week. |
If any of the trigger questions met or exceeded the cut-off, the additional seven questions concerning subjective cognitive complaints (SCC) were asked.
Table 2 shows the topics for the seven questions that are used to calculate the SCC score. The response options for the SCC categories were 1) I strongly disagree, 2) I somewhat disagree, 3) I somewhat agree, and 4) I strongly agree with the question. The SCC score is calculated as the average of the sum of the seven questions. Cut-off limit for the abnormal SCC score, ≥2.4, is based on a preliminary non-published study (N = 30), where participants responded to the SCC questions and conducted neuropsychological examinations. Cronbach’s alpha for the SCC score in our data was 0.98.
Table 2.
The topics for the questions that formed subjective cognitive complaints (SCC) score.
| 1 | Memory difficulties |
| 2 | Difficulties in planning and organizing own work tasks |
| 3 | Forgetting agreed issues and work tasks |
| 4 | Difficulties in concentration |
| 5 | Delays in recollection |
| 6 | Disruptions to thinking |
| 7 | Difficulties in recollection |
Variables
2.4. Outcome measure
The outcome measure was SA from work. SA was operationalized as the accumulated number of SA days during the 12-month follow up after the questionnaire. This included the number of days and periods absent because of sickness. We combined overlapping and consecutive SA. We did not include maternity or paternity leave and absence from work to care for a sick child as SA.
2.5. Exposure variable
We classified the results concerning SCC as follows. First, the respondents who did not indicate any problems with the psychosocial screening questions, and therefore were not asked the SCC questions, were classified as belonging to the reference class. Second, we categorized the SCC score into normal/abnormal, based on the a priori cut-off limit. Thus, the exposure variable consists of three categories: 1) reference (no psychosocial load); 2) some psychosocial load, but normal SCC score; and 3) psychosocial load and abnormal SCC score.
2.6. Potential confounding factors
We identified potential confounders in the study as gender (Messing et al., 2003, Messing and Mager Stellman, 2006), age (Osmotherly & Attia, 2006), general health (Ferrie et al., 2009, Kivimäki et al., 2003), and socioeconomic status (Bouville et al., 2018). We stratified the analyses by gender and included age (five categories) as a potential confounder. Of the available options, we chose to include accumulated SA days before the questionnaire (continuous variable) as a generic measure of health and well-being. Socioeconomic status was operationalized as occupational group and this potential confounder was controlled by the selection of the respondents, who included employees with professional/managerial status only. Other occupational groups (blue-collar workers and clerical employees) were excluded from the study due to small numbers.
2.7. Statistical methods
Baseline characteristics are presented using descriptive statistics. We calculated the patterns with SA means (SD) and the ratio of means with 95% confidence intervals from the questionnaire SCC classes, separately by gender.
There were complex interactions between gender and other variables in our data and we performed all analyses stratified by gender and occupational group as has also been suggested earlier (Messing et al., 2003).
A particular challenge when modelling SA data is that a large number of employees have no absenteeism (Taimela et al., 2007). We tried mixture regression, zero-inflated negative binomial regression, and the Hurdle model. The first two approaches yielded problems when estimating the model's parameters. We chose the Hurdle model, which allows the study of the presence of SA and its duration separately. It provides a combination of two statistical models: logistic regression model determines whether the outcome is zero or positive, and truncated negative binomial regression models the part of the actual counts. We used truncated negative binomial regression because it also accounted for the overdispersion in the counts data (Niedhammer et al., 2013, Taimela et al., 2007). The actual estimation of the model parameters was conducted using R library pscl (Jackman, 2012) with R 3.4.4 software version. We used 95% confidence intervals to report the estimated odds ratios (with 95% CI), based on the binary part, and the estimated risk ratios, based on the regression coefficients of the part of the count with the covariates.
3. Results
The final study sample consisted of the 7059 professional and managerial employees who had responded to the questionnaire for the first time in 2009–2015 (Fig. 1). The average age of the participants was 46.7 years (SD 9.8; range 19.2–67.3). Of them, 45% (N = 3205) were female. The excluded respondents were slightly older on the average (51.8 years, SD 11.9; t 14.1, p < 0.005) and a larger proportion of them were men (55%; chi-squared 90.3, p < 0.005) than of the participants.
The SCC result was classified less likely within the abnormal category in the under-30 age group than the older age groups (Table 3). 13% of the males belonged to the abnormal SCC category, while the respective figure for females was 15% (chi-squared 130.69, p < 0.005). The proportion of respondents with zero SA days was higher in the at least50 age group than the younger age groups for both genders (OR = 1.24, p < 0.003 for the females, and OR = 1.43, p < 0.005 for males) (Table 3). The average number of SA days among the “susceptible to any SA” group was higher among the females.
Table 3.
Prevalence of abnormal subjective cognitive complaints (SCC) and number of days on sickness absence (SA) during 12-month follow-up by gender and age.
| SCC (%) |
% with zero SA days | Days on sick leave |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Gender | Age | Subjects, N | N/A# | normal | abnormal | Median | Upper quartile | Mean of all values | Mean of non-zero values | |
| Male | <30 | 190 | 36 | 59 | 5 | 55 | 0 | 3.75 | 3.0 | 6.8 |
| ≥30 and <40 | 987 | 37 | 53 | 10 | 50 | 0 | 3 | 4.4 | 8.9 | |
| ≥40 and <50 | 1135 | 30 | 55 | 15 | 54 | 0 | 4 | 5.6 | 12.3 | |
| ≥50 and <60 | 1242 | 29 | 57 | 14 | 62 | 0 | 3 | 4.8 | 12.4 | |
| ≥60 | 300 | 26 | 59 | 15 | 61 | 0 | 3.25 | 4.9 | 12.4 | |
| All | 3854 | 32 | 56 | 13 | 56 | 0 | 3 | 4.9 | 11.1 | |
| Female | <30 | 171 | 14 | 73 | 13 | 41 | 2 | 5.5 | 5.2 | 8.7 |
| ≥30 and <40 | 661 | 21 | 62 | 17 | 41 | 2 | 6 | 8.1 | 13.8 | |
| ≥40 and <50 | 935 | 22 | 58 | 20 | 43 | 2 | 6.5 | 7.1 | 12.6 | |
| ≥50 and <60 | 1201 | 20 | 61 | 19 | 47 | 1 | 7 | 7.7 | 14.4 | |
| ≥60 | 237 | 17 | 65 | 19 | 52 | 0 | 7 | 8.6 | 17.8 | |
| All | 3205 | 20 | 61 | 19 | 45 | 1 | 6 | 7.5 | 13.6 | |
| All | 7059 | 26 | 58 | 15 | 51 | 0 | 5.5 | 6.1 | 12.4 | |
# N/A indicates the group of the participants who did not indicate any problems with the psychosocial screening questions, and therefore were not asked the SCC questions.
Belonging to the abnormal SCC category predicted higher mean SA values during the follow-up, regardless of gender. The ratio of means for SA days varied between 2.8 and 3.1 among those in the abnormal SCC category and the reference category, depending on gender. The lowest limit of the 95% confidence interval (CI) was 2.1 (Table 4).
Table 4.
Sickness absence by different subjective cognitive complaints (SCC) category and gender: means and ratio of means.
| Male |
Female |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SA days |
SA days |
||||||||||||
| Psychosocial load§ | SCC | Participants (N) | Median | Mean | SD | Ratio of means | 95% CI | Participants (N) | Median | Mean | SD | Ratio of means | 95% CI |
| No | N/A# | 1215 | 0 | 3.5 | 9.6 | ref. | 648 | 1 | 5.2 | 14.2 | ref. | ||
| Yes | NORMAL | 2142 | 0 | 4.3 | 14.3 | 1.2 | 1.0–1.5 | 1962 | 1 | 6.2 | 15.5 | 1.2 | 0.9–1.5 |
| Yes | Ab-normal | 497 | 2 | 10.6 | 30.4 | 3.1 | 2.2–4.1 | 595 | 3 | 14.5 | 31.2 | 2.8 | 2.1–3.7 |
Bold values denote statistical significance at the p < 0.05 level.
Psychosocial load refers to the results of the screening questionnaire.
N/A indicates the group of the participants who did not indicate any problems with the psychosocial screening questions, and therefore were not asked the SCC questions.
The results of fitting the Hurdle model are displayed in Table 5. The Model 1 includes the crude estimates and the Model 2 is adjusted with age (five classes) and the number of SA days during the 12 months preceding the questionnaire. We conducted the analyses stratified by gender. In the Model 1, the odds ratio (OR) for being susceptible to any SA in the abnormal SCC category was 1.70 (1.35–2.13) for the females and 1.45 (1.17–1.78) for the males. The corresponding rate ratios (RR) for SA duration were 2.62 (2.06–3.33) for the females and 3.25 (2.49–4.25) for the males. In the Model 2, the ORs were 1.45 (1.15–1.84) and 1.35 (1.09–1.67), respectively, and the RRs were 2.39 (1.89–3.01) and 2.21 (1.72–2.82), respectively.
Table 5.
Predicting propensity to be susceptible versus immune to any sickness absence (Logistic model) and duration of sickness absence, if susceptible (Zero-truncated negative binomial (NB) part) in negative binomial Hurdle model. The Model 1 is unadjusted and includes subjective cognitive complaints (SCC) only. The Model 2 is adjusted for age and prior sick leaves as covariates.
| Logistic model (0 vs. > 0) |
Zero-truncated NB (>0) |
||||
|---|---|---|---|---|---|
| Explanatory variable | N | OR | 95%CI | RR | 95%CI |
| MALE | |||||
| Model 1 (unadjusted) | |||||
| (Intercept) | 0.85 | 0.76–0.95 | 3.04 | 2.34–3.94 | |
| No psychosocial load | 1215 | 1.00 | ref. | 1.00 | ref. |
| Psychosocial load, but normal SCC | 2142 | 0.79 | 0.69–0.91 | 1.59 | 1.31–1.92 |
| Abnormal SCC | 497 | 1.45 | 1.17–1.78 | 3.25 | 2.49–4.25 |
| Model 2 (adjusted) | |||||
| (Intercept) | 0.94 | 0.80–1.10 | 2.51 | 2.00–3.16 | |
| No psychosocial load | 1215 | 1.00 | ref. | 1.00 | ref. |
| Psychosocial load, but normal SCC | 2142 | 0.79 | 0.68–0.91 | 1.34 | 1.12–1.60 |
| Abnormal SCC | 497 | 1.35 | 1.09–1.67 | 2.21 | 1.72–2.82 |
| Age ≥30 and <40 | 987 | 1.00 | ref. | 1.00 | ref. |
| Age <30 | 190 | 0.89 | 0.65–1.22 | 0.96 | 0.66–1.41 |
| Age ≥40 and <50 | 1135 | 0.84 | 0.70–1.00 | 1.52 | 1.24–1.87 |
| Age ≥50 and <60 | 1242 | 0.63 | 0.53–0.74 | 1.59 | 1.29–1.96 |
| Age ≥60 | 300 | 0.66 | 0.50–0.86 | 1.58 | 1.13–2.21 |
| SA before the questionnaire | 1.049 | 1.038–1.060 | 1.034 | 1.026–1.042 | |
| FEMALE | |||||
| Model 1 (unadjusted) | |||||
| (Intercept) | 1.10 | 0.94–1.28 | 5.83 | 4.76–7.14 | |
| No psychosocial load | 648 | 1.00 | ref. | 1.00 | ref. |
| Psychosocial load, but normal SCC | 1962 | 1.04 | 0.87–1.25 | 1.20 | 0.98–1.47 |
| Abnormal SCC | 595 | 1.70 | 1.35–2.13 | 2.62 | 2.06–3.33 |
| Model 2 (adjusted) | |||||
| (Intercept) | 1.10 | 0.89–1.36 | 5.01 | 3.96–6.33 | |
| No psychosocial load | 648 | 1.00 | ref. | 1.00 | ref. |
| Psychosocial load, but normal SCC | 1962 | 1.00 | 0.84–1.20 | 1.21 | 1.00–1.47 |
| Abnormal SCC | 595 | 1.45 | 1.15–1.84 | 2.39 | 1.89–3.01 |
| Age ≥30 and <40 | 661 | 1.00 | ref. | 1.00 | ref. |
| Age <30 | 171 | 1.08 | 0.77–1.54 | 0.64 | 0.46–0.91 |
| Age ≥40 and <50 | 935 | 0.87 | 0.71–1.07 | 0.91 | 0.74–1.12 |
| Age ≥50 and <60 | 1201 | 0.78 | 0.64–0.94 | 1.18 | 0.97–1.45 |
| Age ≥60 | 237 | 0.63 | 0.47–0.86 | 1.52 | 1.09–2.13 |
| SA before the questionnaire | 1.051 | 1.040–1.062 | 1.020 | 1.014–1.026 | |
Logistic model refers to model component for predicting membership to subpopulation A with high propensity to zero absence, and Zero-truncated NB to the component predicting days on sick leave among susceptible subpopulation B. To facilitate interpretation, for zero-inflation we show odds ratios associated with complementary propensity to having any sickness absence—that is, inclusion in subpopulation B. Bold values denote statistical significance at the p < 0.05 level.
The likelihood to have zero SA was higher in the older age groups, but higher age predicted higher SA count if any. SA prior to the questionnaire predicted both susceptibility to SA and the number of SA days during the follow-up.
4. Discussion
4.1. Key results
Subjective cognitive complaints (SCC) predicted both the likelihood of SA and the number of SA days, if any, in both genders in primarily knowledge-intensive occupations. Of note, the independent role of SCC as a predictor of SA remained also in the adjusted model where age and prior sickness absence days as a proxy measure of general health were accounted for. This indicates that SCC is an early indicator of future SA risks in cognitively demanding occupations.
4.2. Strengths and weaknesses of the study
One of the strengths of our study is the extensive, registry based and prospectively collected data from various industries. The recorded SA data quality in terms of coverage, accuracy, and consistency over time was better than that which could be achieved through self-reports (Stapelfeldt et al., 2012). We were also able to control key potential confounders such as age, gender and general health.
Analysis of the predictors and determinants of SA is difficult with traditional statistical methods because a substantial fraction is clustered at zero SA days. Also, the residual variability in the non-zero part of the SA distribution exceeds that predicted by a Poisson model for counts. Although the Hurdle model (Smithson & Merkle, 2013) was perhaps not able to deal with all the complexity associated with this type of response variable, among computationally feasible approaches it is clearly more appropriate than the simpler alternative models in dealing with both the extra-zero component and the overdispersion.
We do not know the exact response rate in our study, nor have any information of the non-respondents, which must be considered as potential limitations. A “healthy worker effect’’ may be present since health of employed people is generally better than that of the unemployed population, or if employees with worse health level had not responded (Korkeila et al., 2001). This potential bias would underestimate the associations as the respondents would have less cognitive complaints, and possibly less SA than non-respondents. Similar bias would potentially result from a “healthy worker survival effect”, which means that only healthiest and strongest will remain in the working life (Nordström et al., 2016). Moreover, we did not include those who are on long-term SA or those who had already been granted a disability benefit before the questionnaire. All this might underestimate the associations. It may also be possible that the healthiest employees might not respond to the questionnaire, which would have an opposite effect on our estimates. Moreover, the study population consisted solely of professionals and managers. Generalizations to other occupational groups must thus be made cautiously.
Another limitation of our study is the lack of proper psychometric validation of the SCC questionnaire. It has previously been studied in a preliminary study only, using a selected population from one information technology company (Ahveninen et al., 2014). However, Cronbach’s alpha was in our study at an acceptable level for the SCC (0.98). In the present study, we focused on the predictive validity of abnormal SCC on SA.
4.3. Similarities with and differences to previous studies
In an earlier preliminary cohort study among professional/managerial employees (N = 180), 42% of those with abnormal SCC category had long-term SA (over 30 days) (Ahveninen et al., 2014). Another cohort study (N = 2898) found that the abnormal SCC category had an association with an increasing number of SA days (13.9 SA days/employee/year) compared to those with normal SCC category (5.3 SA days/employee/year) (Ahveninen et al., 2019). Our study is line with these earlier studies.
Most studies focusing on the association between SCC and SA have included employees with health-related conditions, such as depression (Salomonsson et al., 2018) or stress-related symptoms (burnout/exhaustion) (Salvagioni et al., 2017). Obviously these conditions are related to sickness absence (Ahola et al., 2008, Kansaneläkelaitos et al., 2018, Kausto et al., 2017), but we are not aware of other prospective cohort studies that would be focusing on how SCC affects SA behavior.
The length of the SA varies by age (Bouville et al., 2018), depending on the underlying diagnosed disease. The older seem to have longer spells of SA than the younger (Dekkers-Sánchez et al., 2008, Donders et al., 2012, Salonen et al., 2018), but the younger seem to have more frequently short spells of SA than the older (Sumanen et al., 2015, Taimela et al., 2007). This is in line with our results: The propensity to have zero SA days was higher in the over 50-year age groups for both genders. Our results also provide further support to a connection between prior and future SA, as has been reported earlier (Cohen and Golan, 2007, Laaksonen et al., 2011).
Further research is needed to understand the causal pathways between psychosocial loading, cognitive performance, SCC, illnesses and SA. We also suggest studying whether the questionnaire predicts permanent work disability. The effectiveness and cost-effectiveness of interventions targeted to the risk groups also warrant further research.
5. Conclusion
Our results indicate that subjective cognitive complaints predict sickness absence in knowledge-intensive occupations, irrespective of gender, age, or general health. Thus, SCC seems to act as an early indicator of future SA risks in cognitively demanding occupations. This finding has implications for supporting work productivity among employees with cognitively demanding tasks.
What is already known about this subject?
The prevalence of subjective cognitive complaints, like difficulties of concentration, memory, clear thinking and decision making, increases with age. They also often coincide with chronic stress, exhaustion, sleeping problems, and depression, but little is known about their associations with sickness absence.
What are the new findings?
Subjective cognitive complaints predicted both the likelihood of sickness absence and the count of sickness absence days, if any, during 12-month follow-up among both genders in knowledge-intensive occupations after adjustments with age and prior sickness absence.
How might this impact on policy or clinical practice in the foreseeable future?
In knowledge-intensive occupations, subjective cognitive complaints act as an early indicator in identifying employees who are at an increased risk of sickness absence.
6. Additional Information
Contributions: MP, JU, HAR, JO, and ST participated in planning the study. MK and TN conducted the statistical analyses. MP, HAR, HAH, and ST interpreted the results. MP and ST wrote the first draft of the manuscript, and all authors commented and approved the final manuscript as submitted.
Funding: This work was supported by Terveystalo, Evalua International, and the University of Tampere.
Patient consent: This study used solely secondary data retrieved from registers.
Ethical approval: The Tampere University Research Ethics Board approved the study. (ETL code R16074).
Data sharing statement: No additional data are available due to data privacy reasons.
Declaration of interest: MP reports personal fees from a Finnish Work Environment Fund scholarship received during the conduct of the study; HAR and HAH are employed by Terveystalo; ST is employed by Evalua International; JU, JO, MK, and TN are employed by the University of Tampere; JO reports receiving personal fees from Terveystalo during the conduct of the study. There are no other competing interests to declare.
Declaration of submission: The Corresponding Author has the right to grant on behalf of all authors and does grant on behalf of all authors, an exclusive license (or non-exclusive licence for UK Crown and US Federal Government employees) on a worldwide basis to Preventive Medicine Reports, and its Licensees to permit this article (if accepted) to be published and to exploit all subsidiary rights, as set out in our license. The article has not been previously published and is not under consideration for publication elsewhere.
CRediT authorship contribution statement
Minna Pihlajamäki: Conceptualization, Project administration, Writing - original draft. Heikki Arola: Methodology, Writing - review & editing. Heini Ahveninen: Methodology, Writing - review & editing. Jyrki Ollikainen: Methodology, Data curation, Writing - review & editing. Mikko Korhonen: Formal analysis, Writing - review & editing. Tapio Nummi: Formal analysis, Writing - review & editing. Jukka Uitti: Conceptualization, Supervision, Writing - review & editing. Simo Taimela: Conceptualization, Supervision, Writing - review & editing.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2020.101103.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Aasvik J.K., Woodhouse A., Jacobsen H.B., Borchgrevink P.C., Stiles T.C., Landrø N.I. Subjective memory complaints among patients on sick leave are associated with symptoms of fatigue and anxiety. Front. Psychol. 2015;6:1338. doi: 10.3389/fpsyg.2015.01338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahola K., Kivimäki M., Honkonen T., Virtanen M., Koskinen S., Vahtera J., Lönnqvist J. Occupational burnout and medically certified sickness absence: a population-based study of finnish employees. J. Psychosom. Res. 2008;64(2):185–193. doi: 10.1016/j.jpsychores.2007.06.022. [DOI] [PubMed] [Google Scholar]
- Ahveninen, H., Arola, H., Ollikainen, J., 2019. Kysely tunnistaa sairauspoissaoloriskin tietotyössä. Suomen Lääkärilehti, 19(74), 1198–1207. Originally published in Finnish, English summary. [Can knowledge-intensive workers at risk of absenteeism be identified using a questionnaire? Finnish Med. J. 19(74), 1198–207].
- Ahveninen, H., Rintala, J., Ollikainen, J., Suhonen, J., Arola Heikki, 2014. TyöOptimi-kysely auttaa tunnistamaan työssäkäyvän kognitiivisia ja muistioireita. Suomen Lääkärilehti, 14(4), 207–214. Originally published in Finnish, English summary. [WorkOptimum questionnaire helps to detect memory and cognitive symptoms among working people. Finnish Medical Journal 14(4), 207–14].
- Barbe T., Kimble L.P., Rubenstein C. Subjective cognitive complaints, psychosocial factors and nursing work function in nurses providing direct patient care. J. Adv. Nurs. 2018;74(4):914–925. doi: 10.1111/jan.13505. [DOI] [PubMed] [Google Scholar]
- Bouville G., Dello Russo S., Truxillo D. The moderating role of age in the job characteristics–absenteeism relationship: a matter of occupational context? J. Occup. Organiz. Psychol. 2018;91(1):57–83. [Google Scholar]
- Burmester B., Leathem J., Merrick P. Subjective cognitive complaints and objective cognitive function in aging: a systematic review and meta-analysis of recent cross-sectional findings. Neuropsychol. Rev. 2016;26(4):376–393. doi: 10.1007/s11065-016-9332-2. [DOI] [PubMed] [Google Scholar]
- Catalina-Romero C., Sainz J.C., Pastrana-Jiménez J.I., García-Diéguez N., Irízar-Muñoz I., Aleixandre-Chiva J.L., Gonzalez-Quintela A., Calvo-Bonacho E. The impact of poor psychosocial work environment on non-work-related sickness absence. Soc. Sci. Med. 2015;138:210–216. doi: 10.1016/j.socscimed.2015.06.009. [DOI] [PubMed] [Google Scholar]
- Clausen T., Burr H., Borg V. Do psychosocial job demands and job resources predict long-term sickness absence? an analysis of register-based outcomes using pooled data on 39,408 individuals in four occupational groups. Int. Arch. Occup. Environ. Health. 2014;87(8):909–917. doi: 10.1007/s00420-014-0936-7. [DOI] [PubMed] [Google Scholar]
- Cohen A., Golan R. Predicting absenteeism and turnover intentions by past absenteeism and work attitudes. Career Develop. Int. 2007;12(5):416–432. doi: 10.1108/13620430710773745. [DOI] [Google Scholar]
- Dekkers-Sánchez P.M., Hoving J.L., Sluiter J.K., Frings-sen M.H.W. Factors associated with long-term sick leave in sick-listed employees: a systematic review. Occup. Environ. Med. 2008;65(3):153–157. doi: 10.1136/oem.2007.034983. [DOI] [PubMed] [Google Scholar]
- Denise Albieri Jodas Salvagioni, Francine Nesello Melanda, Arthur Eumann Mesas, Alberto Durán González, Flávia Lopes Gabani, Selma Maffei de Andrade,.2017. Physical, psychological and occupational consequences of job burnout: a systematic review of prospective studies. PLoS One, 12(10), e0185781. doi:10.1371/journal.pone.0185781. [DOI] [PMC free article] [PubMed]
- Donders, Nathalie C.G.M., Bos, J.T., van der Velden, K., van der Gulden, Joost W.J., 2012. Age differences in the associations between sick leave and aspects of health, psychosocial workload and family life: A cross-sectional study. BMJ Open, 2(4), e000960. doi:10.1136/bmjopen-2012-000960. [DOI] [PMC free article] [PubMed]
- Edwards, P., Greasley, K., 2010. Absence from work. Report of the European Working Conditions Observatory. Published on internet 20 July 2010 [cited in December 2018]. Retrieved from: https://www.eurofound.europa.eu/publications/report/2010/absence-from-work.
- Ferrie J.E., Vahtera J., Kivimaki M., Westerlund H., Melchior M., Alexanderson K., Head J., Chevalier A., Leclerc A., Zins M., Goldberg M., Singh-Manoux A. Diagnosis-specific sickness absence and all-cause mortality in the GAZEL study. J. Epidemiol. Community Health. 2009;63(1):50–55. doi: 10.1136/jech.2008.074369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Findicator. Official Statistics of Finland. (2018). Employed persons by industry. Published on internet 11 April 2019. Accessed October 2019. Retrieved from: https://suhdannepalvelu.stat.fi/en/12.
- Finland. Tilastokeskus, 1979. Toimialaluokitus (TOL) = standard industrial classification (SIC). Retrieved from http://www.stat.fi/meta/luokitukset/toimiala/001-2008/index_en.html.
- Hinkka K., Kuoppala J., Väänänen-Tomppo I., Lamminpää A. Psychosocial work factors and sick leave, occupational accident, and disability pension: a cohort study of civil servants. J. Occup. Environ. Med. 2013;55(2):191–197. doi: 10.1097/JOM.0b013e31827943fe. [DOI] [PubMed] [Google Scholar]
- Jackman, S., 2012. Pscl: Classes and methods for R developed in political science computation laboratory, Stanford University. Accessed September 2018. Retrieved from: https://cran.r-project.org/web/packages/pscl/citation.html.
- Janssens H., Clays E., De Clercq B., Casini A., De Bacquer D., Kittel F., Braeckman L. The relation between psychosocial risk factors and cause-specific long-term sickness absence. Eur. J. Pub. Health. 2014;24(3):428–433. doi: 10.1093/eurpub/cku009. [DOI] [PubMed] [Google Scholar]
- Kansaneläkelaitos, K., Folkpensionsanstalten, F. & Social Insurance Institution of Finland, 2018. Kelan sairausvakuutustilasto 2017. Only published in Finnish and Swedish [Health Insurance Statistics 2017]. Published on internet 24 September 2018. Accessed July 2018. Retrieved from: http://hdl.handle.net/10138/244518.
- Kausto J., Pentti J., Oksanen T., Virta L.J., Virtanen M., Kivimäki M., Vahtera J. Length of sickness absence and sustained return-to-work in mental disorders and musculoskeletal diseases: a cohort study of public sector employees. Finland: Scand. J. Work Environ. Health. 2017 doi: 10.5271/sjweh.3643. [DOI] [PubMed] [Google Scholar]
- Kivimäki M., Head J., Ferrie J.E., Shipley M.J., Vahtera J., Marmot M.G. Sickness absence as a global measure of health: evidence from mortality in the whitehall II prospective cohort study. BMJ. 2003;327(7411):364. doi: 10.1136/bmj.327.7411.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korkeila K., Suominen S., Ahvenainen J., Ojanlatva A., Rautava P., Helenius H., Koskenvuo M. Non-response and related factors in a nation-wide health survey. Eur. J. Epidemiol. 2001;17(11):991–999. doi: 10.1023/a:1020016922473. 1020016922473. [DOI] [PubMed] [Google Scholar]
- Laaksonen M., Pitkäniemi J., Rahkonen O., Lahelma E. Work arrangements, physical working conditions, and psychosocial working conditions as risk factors for sickness absence: Bayesian analysis of prospective data. Ann. Epidemiol. 2010;20(5):332–338. doi: 10.1016/j.annepidem.2010.02.004. [DOI] [PubMed] [Google Scholar]
- LaMonica H.M., Hickie I.B., Ip J., Ireland C., Mowszowski L., English A., Glozier N., Naismith S.L. Disability in older adults across the continuum of cognitive decline: unique contributions of depression, sleep disturbance, cognitive deficits and medical burden. Int. Psychogeriatr. 2019;1–15 doi: 10.1017/S1041610218002144. [DOI] [PubMed] [Google Scholar]
- Loisel P., Durand M.J., Berthelette D., Vezina N., Baril R., Gagnon D., Larivière C., Tremblay C. Disability prevention: new paradigm for the management of occupational back pain. Dis. Manage. Health Outcomes. 2001;9(7):351–360. doi: 10.2165/00115677-200109070-00001. [DOI] [Google Scholar]
- Messing K., Punnett L., Bond M., Alexanderson K., Pyle J., Zahm S., Wegman D., Stock S., de Grosbois S. Be the fairest of them all: challenges and recommendations for the treatment of gender in occupational health research. Am. J. Ind. Med. 2003;43(6):618. doi: 10.1002/ajim.10225. http://kipublications.ki.se/Default.aspx?queryparsed=id:19271499 Retrieved from. [DOI] [PubMed] [Google Scholar]
- Messing K., Mager Stellman J. Sex, gender and women's occupational health: the importance of considering mechanism. Environ. Res. 2006;101(2):149–162. doi: 10.1016/j.envres.2005.03.015. [DOI] [PubMed] [Google Scholar]
- Laaksonen Mikko, Kääriä Sanna-Mari, Leino-Arjas Päivi, Lahelma Eero. Different domains of health functioning as predictors of sickness absence – a prospective cohort study. Scand. J. Work Environ. Health. 2011;37(3):213–218. doi: 10.5271/sjweh.3131. [DOI] [PubMed] [Google Scholar]
- Niedhammer I., Chastang J., Sultan-Taïeb H., Vermeylen G., Parent-Thirion A. Psychosocial work factors and sickness absence in 31 countries in europe. Eur. J. Pub. Health. 2013;23(4):622–629. doi: 10.1093/eurpub/cks124. [DOI] [PubMed] [Google Scholar]
- Nordström K., Hemmingsson T., Ekberg K., Johansson G. Sickness absence in workplaces. Int. J. Occup. Med. Environ. Health. 2016;29(2):315. doi: 10.13075/ijomeh.1896.00522. http://urn.kb.se/resolve?urn=urn:nbn:se:su:diva-126184 Retrieved from. [DOI] [PubMed] [Google Scholar]
- Organisation for Economic Co-operation and Development, (OECD). (2010). Sickness, disability and work: Breaking the barriers: A synthesis of findings across OECD countries Aufl. ed.). Paris: OECD Publishing. doi://dx.doi.org/10.1787/9789264088856-en.
- Osmotherly P., Attia J. The healthy worker survivor effect in a study of neck muscle performance measures in call-centre operators. Work. 2006;26(4):399–406. [PubMed] [Google Scholar]
- Salomonsson S., Hedman-Lagerlöf E., Öst L. Sickness absence: A systematic review and meta-analysis of psychological treatments for individuals on sick leave due to common mental disorders. Psychol. Med. 2018;48(12):1954–1965. doi: 10.1017/S0033291718000065. [DOI] [PubMed] [Google Scholar]
- Salonen L., Blomgren J., Laaksonen M., Niemelä M. Sickness absence as a predictor of disability retirement in different occupational classes: a register-based study of a working-age cohort in finland in 2007–2014. BMJ Open. 2018;8(5) doi: 10.1136/bmjopen-2017-020491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smithson, M., Merkle, E.C., 2013. Generalized linear models for categorical and continuous limited dependent variables (second edition ed.). Taylor & Francis group, Boca Raton, FL 33487-2742: CRC Press.
- Social Insurance Institution of Finland, & Kela. (2017). Sickness allowance. Published on internet 19 September 2016, last modified 17 January 2019. Accessed October 2019. Retrieved from: https://www.kela.fi/web/en/sickness-allowance.
- Stapelfeldt C.M., Jensen C., Andersen N.T., Fleten N., Nielsen C.V. Validation of sick leave measures: self-reported sick leave and sickness benefit data from a danish national register compared to multiple workplace-registered sick leave spells in a danish municipality. BMC Public Health. 2012;12(1):661. doi: 10.1186/1471-2458-12-661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stenfors C.U.D., Marklund P., Hanson L.L.M., Theorell T., Nilsson L. Subjective cognitive complaints and the role of executive cognitive functioning in the working population: a case-control study. PLoS ONE. 2013;8(12) doi: 10.1371/journal.pone.0083351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stenfors C.U.D., Hanson Magnusson L., Oxenstierna G., Theorell T., Nilsson L. Psychosocial working conditions and cognitive complaints among swedish employees. PLoS ONE. 2013;8(4) doi: 10.1371/journal.pone.0060637. http://urn.kb.se/resolve?urn=urn:nbn:se:su:diva-89710 Retrieved from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strømholm T., Pape K., Ose S., Krokstad S., Bjørngaard J. Psychosocial working conditions and sickness absence in a general population: A cohort study of 21,834 workers in norway (the HUNT study) J. Occup. Environ. Med. 2015;57(4):386–392. doi: 10.1097/JOM.0000000000000362. [DOI] [PubMed] [Google Scholar]
- Sumanen H., Pietiläinen O., Lahti J., Lahelma E., Rahkonen O. Sickness absence among young employees: trends from 2002 to 2013. J. Occup. Health. 2015;57(5):474–481. doi: 10.1539/joh.14-0236-OA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundstrup E., Hansen A.M., Mortensen E.L., Poulsen O.M., Clausen T., Rugulies R., Møller A., Andersen L.L. Retrospectively assessed psychosocial working conditions as predictors of prospectively assessed sickness absence and disability pension among older workers. BMC Public Health. 2018;18(1):149. doi: 10.1186/s12889-018-5047-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szubert Z., Makowiec-Dąbrowska T., Merecz D., Sobala W. Predictors of short- and long-term sickness absence in female post office workers in poland. Int. J. Occup. Med. Environ. Health. 2016;29(4):539–562. doi: 10.13075/ijomeh.1896.00795. [DOI] [PubMed] [Google Scholar]
- Taimela S., Läärä E., Malmivaara A., Tiekso J., Sintonen H., Justén S., Aro T. Self-reported health problems and sickness absence in different age groups predominantly engaged in physical work. Occup. Environ. Med. 2007;64(11):739–746. doi: 10.1136/oem.2006.027789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Väänänen A., Kalimo R., Toppinen-Tanner S., Mutanen P., Peiró J.M., Kivimäki M., Vahtera J. Role clarity, fairness, and organizational climate as predictors of sickness absence. Scand. J. Public Health. 2004;32(6):426–434. doi: 10.1080/14034940410028136. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.