The association between stress and psychosis is well established. Experimental stress induction has been shown to lead to changes in positive symptoms across psychosis continuum (Valmaggia et al., 2015; Veling et al., 2016). The pathway from stressors to symptoms involves a stronger negative emotional response (Lincoln et al., 2018) and negative self-esteem (Jongeneel et al., 2018). Experience sampling studies have shown that on a day-to-day basis, sensitivity to stress is related to increased severity of delusions and hallucinations, with a mediating role of negative affect (Lataster et al., 2013; Reininghaus et al., 2016).
The current SARS-CoV-2 pandemic represents a global challenge to the mental health of large populations, in which not only people with severe mental disorders are at risk. National government regulations involving social distancing lead to increasing feelings of loneliness which are associated with the onset and persistence of psychotic symptoms (Michalska da Rocha et al., 2018). Strict regulations aiming to prevent further spread of the pandemic also cause significant burden, such as radical changes in daily routines, leading to feelings of insecurity, worries, anxiety or even hopelessness. On the other hand, a lot of positive protective factors such as solidarity and higher social cohesion have been taking place in the society. Despite the negative predictions from the media, the short-term and long-term impact of the current stressful situation on the subclinical psychotic experiences or mental health in general is yet to be confirmed empirically.
Our aim was to analyze changes in the positive psychotic experiences (PE) during the current pandemic in the non-clinical university student population. The secondary aim was to evaluate how PE are related to affective symptoms, perceived stress, and loneliness.
During the second week of March 2020, The Slovak government took fast and strict regulations to slow down the further spread of the pandemic that included restrictions on the free movement of citizens, universities closures, the obligation to wear a protective mask, and other limitations. At the time of data collection, 485 people in the Slovak Republic were positively tested for SARS-CoV-2, with 1 confirmed death associated with COVID-19. Overall, Slovak Republic is considered as a country which deals with COVID pandemic successfully.
This report is based on data from the research project examining mental health in college students (Hajdúk et al., 2019). The first wave of the project was conducted during October 2018, where 1331 students (undergraduate, graduate, PhD) of Comenius University in Bratislava completed a battery of online questionnaires assessing their mental health status, satisfaction with life, and other variables. 660 of them agreed to be contacted again. Eighteen months later, during the first week of April 2020, an invitation for the follow-up survey was sent. The final sample consisted of 235 participants (77% of females, 36% response rate) with the mean age of M = 23.77 and SD = 4.03.
PE were measured by the positive subscale of Community Assessment of Psychic Experiences (CAPE-42). Depression was assessed by Patient Health Questionnaire (PHQ-9) and anxiety with Generalized Anxiety Disorder Questionnaire (GAD-7). These three measures were administered both at the baseline and the follow-up. At the follow-up, Perceived Stress Scale (PSS-4) and Brief Loneliness Scale were added to the battery.
Repeated measures ANCOVA was used to calculate changes in PE. At follow-up, we statistically controlled for age and gender. The model without covariates lead to significant differences across waves, in that participants had lower frequency of PE at follow-up (F(1,234) = 38.704, p < .001, η2 = 0.142). The model with appropriate correction for demographic factors did not reveal statistical differences in the PE score across time (F(1,232) = 1.010, p = .316, η2 = 0.004). Numerically, participants at the follow-up scored slightly lower in PE. This finding can be explained by the regression to the mean or by fact that prevalence of PE is associated with lower age.
PE at the follow-up were associated with depression (rs = 0.323, p < .001), anxiety (rs = 0.269, p < .001), perceived stress (rs = 0.232, p < .001), and loneliness (rs = 0.285, p < .001). When all measures were added simultaneously to the linear regression model, only depression explained PE above and beyond the effect of other predictors (β = 0.259, p = .011).
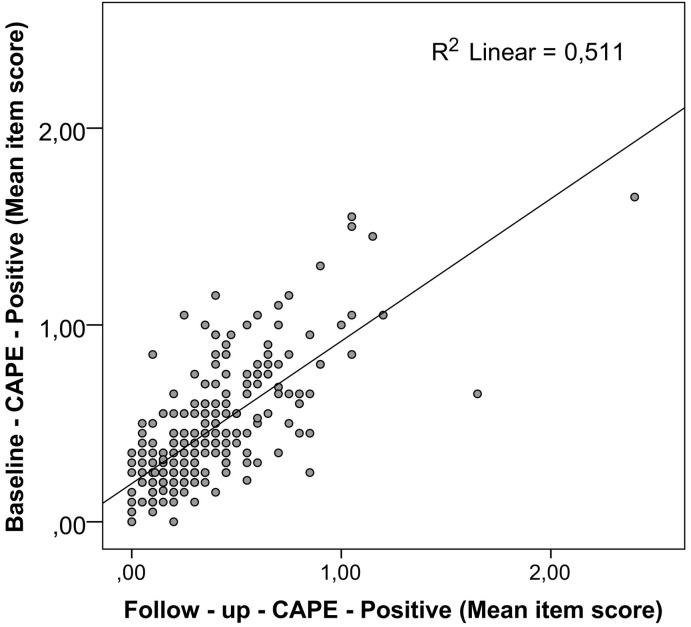
Baseline PE were associated with PE (rs = 0.703, p < .001) (see Fig. 1 .), depression (rs = 0.255, p < .001), anxiety (rs = 0.209, p = .001), perceived stress (rs = 0.209, p = .001), and loneliness (rs = 0.212, p = .001) at the follow-up.
Fig. 1.
Correlation between CAPE score from baseline and follow up.
We found significant longitudinal relationships between PLE and negative affect, especially depression. Our results also provide evidence that loneliness and perceived stress were related to PLE both longitudinally and cross-sectionally. We believe that these results are important for health-related policies across universities. Given their age, students represent a population at higher risk of onset of mental disorders, especially psychotic disorders. National governments and universities should pay increased attention to the systematic protection and monitoring of the mental health and well-being of their students and provide an increased amount of psychosocial support to ameliorate the negative effect of risk factors for severe mental illnesses. This is especially important not only during current crisis. Our results also revealed that PE in the university student population are relatively stable, even during this extremely stressful situation. Contrary to our expectation, the current situation was not associated with an increased level of PE in our sample. At the time of testing, we were at the beginning of world pandemic, therefore its impact on psychotic symptoms may be manifested after a longer period of time. Important protective factors such as increased contact with family members, social support, solidarity, and higher social cohesion in society, however, may also temporarily serve as a buffer against the current stressors. While longitudinal studies with longer follow-ups are necessary for understanding of the potentially complex effects of the current COVID-19-related crisis on mental health and well-being, its short-term impact on psychotic experiences did not appear to materialize in our sample. The extend of COVID-19 pandemic in country might also moderate extent of impact on psychotic experience.
Contributors
MH drafted an initial version of the manuscript and analyzed data. All authors substantially reviewed and edited the first version. The final version of the manuscript was confirmed by all authors.
Ethical aspects
The baseline project was approved by the Ethical Review Board of University Hospital Bratislava and FM CU. Participants at baseline specifically agreed to be contacted for follow up studies and another research projects.
Declaration of competing interest
Authors do not report a conflict of interest related to the content of this letter.
Acknowledgement
The project was supported by grant VEGA: 1/0184/19 and as a result of the following project implementation: Comenius University in Bratislava Science Park supported by the Research and Development Operational Programme funded by the ERDF. Grant number: ITMS 26240220086. We would like to thank Dr. Zuzana Kasanová for her helpful comments.
To the Editor
References
- Hajdúk M., Heretik A., Vašečková B., Forgačová L., Pečeňák J. Prevalence and correlations of depression and anxiety among Slovak college students. Bratisl Med J. 2019;120:695–698. doi: 10.4149/BLL_2019_117. [DOI] [PubMed] [Google Scholar]
- Jongeneel A., Pot-Kolder R., Counotte J., van der Gaag M., Veling W. Self-esteem moderates affective and psychotic responses to social stress in psychosis: a virtual reality study. Schizophr. Res. 2018;202:80–85. doi: 10.1016/j.schres.2018.06.042. [DOI] [PubMed] [Google Scholar]
- Lataster T., Valmaggia L., Lardinois M., van Os J., Myin-Germeys I. Increased stress reactivity: a mechanism specifically associated with the positive symptoms of psychotic disorder. Psychol. Med. 2013;43:1389–1400. doi: 10.1017/S0033291712002279. [DOI] [PubMed] [Google Scholar]
- Lincoln T.M., Sundag J., Schlier B., Karow A. The relevance of emotion regulation in explaining why social exclusion triggers paranoia in individuals at clinical high risk of psychosis. Schizophr. Bull. 2018;44(4):757–767. doi: 10.1093/schbul/sbx135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michalska da Rocha B., Rhodes S., Vasilopoulou E., Hutton P. Loneliness in psychosis: a meta-analytical review. Schizophr. Bull. 2018;44:114–125. doi: 10.1093/schbul/sbx036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reininghaus U., Kempton M.J., Valmaggia L., Craig T.K.J., Garety P., Onyejiaka A., Gayer-Anderson C., So S.H., Hubbard K., Beards S., Dazzan P., Pariante C., Mondelli V., Fisher H.L., Mills J.G., Viechtbauer W., McGuire P., van Os J., Murray R.M., Wykes T., Myin-Germeys I., Morgan C. Stress sensitivity, aberrant salience, and threat anticipation in early psychosis: an experience sampling study. Schizophr. Bull. 2016;42:712–722. doi: 10.1093/schbul/sbv190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valmaggia L.R., Day F., Garety P., Freeman D., Antley A., Slater M., Swapp D., Myin-Germeys I., McGuire P. Social defeat predicts paranoid appraisals in people at high risk for psychosis. Schizophr. Res. 2015;168:16–22. doi: 10.1016/j.schres.2015.07.050. [DOI] [PubMed] [Google Scholar]
- Veling W., Pot-Kolder R., Counotte J., van Os J., van der Gaag M. Environmental social stress, paranoia and psychosis liability: a virtual reality study. Schizophr. Bull. 2016;42:1363–1371. doi: 10.1093/schbul/sbw031. [DOI] [PMC free article] [PubMed] [Google Scholar]