Key Points
Question
Does internal fixation surgery, compared with nonoperative functional bracing, improve functional outcomes for patients with closed displaced humeral shaft fractures?
Findings
In this randomized clinical trial that included 82 adults with humeral shaft fractures, mean scores for functional outcome at 12 months (as measured with the Disabilities of Arm, Shoulder and Hand score; range, 0 to 100 points; minimal clinically important difference, 10 points) were 8.9 points in the surgery group and 12.0 points in the functional bracing group, a 3-point difference that was not statistically significant.
Meaning
Among patients with closed displaced humeral shaft fractures, internal fixation surgery, compared with nonoperative functional bracing, did not significantly improve functional outcomes at 12 months.
Abstract
Importance
Humeral shaft fractures traditionally have been treated nonsurgically, but there has been a steady increase in the rate of surgery over the past 2 decades without high-quality evidence to justify the trend.
Objective
To compare the effectiveness of surgical treatment with open reduction and internal plate fixation to nonsurgical treatment with functional bracing in the treatment of closed humeral shaft fractures.
Design, Setting, and Participants
Randomized clinical trial conducted at 2 university hospital trauma centers in Finland, enrollment between November 2012 and January 2018 with a final follow-up of January 2019. A total of 82 adult patients with closed, unilateral, displaced humeral shaft fracture met criteria for inclusion. Patients were excluded if they had cognitive disabilities preventing them from following the protocol or had multimorbidity or multiple trauma.
Interventions
Patients were randomly assigned to surgical treatment with open reduction and internal plate fixation (n = 38) or to nonsurgical treatment with functional bracing (n = 44).
Main Outcome and Measure
The primary outcome was Disabilities of Arm, Shoulder and Hand (DASH) score at 12 months (range, 0 to 100 points, 0 denotes no disability and 100 extreme disability; minimal clinically important difference, 10 points).
Results
Among 82 patients who were randomized (mean age, 48.9 years; 38 women [46%]; 44 men [54%]), 78 (95%) completed the trial. Thirteen (30%) of the patients assigned to functional bracing underwent surgery during the 12-month follow-up period to promote healing of the fracture. At 12 months, the mean DASH score was 8.9 (95% CI, 4.2 to 13.6) in the surgery group and 12.0 (95% CI, 7.7 to 16.4) in the bracing group (between-group difference, −3.1 points; 95% CI, −9.6 to 3.3; P = .34). Eleven patients (25%) allocated to functional bracing developed fracture nonunion. Three patients (8%) allocated to surgery developed a temporary radial nerve palsy.
Conclusions and Relevance
Among patients with closed humeral shaft fracture, internal fixation surgery, compared with nonoperative functional bracing, did not significantly improve functional outcomes at 12 months. However, the substantial amount of treatment crossover from nonoperative to surgical treatment should be considered when interpreting the trial results.
Trial Registration
ClinicalTrials.gov Identifier: NCT01719887
This randomized trial compares the effects of open reduction and internal fixation vs functional bracing for treating patients with closed displaced humeral shaft fractures.
Introduction
Humeral shaft fractures have been estimated to account for 1% to 3% of all fractures. They are usually caused by simple falls, motor vehicle crashes, and sports injuries. Humeral shaft fractures were estimated to lead to approximately 60 000 emergency department visits in the United States alone in 2008.1,2,3
Historically, the treatment of humeral shaft fractures has primarily been nonoperative, using either splints, casts, or functional bracing.4 The most common concern related to nonoperative treatment is nonunion with a reported incidence as high as 33%.5,6,7,8,9 For surgery, the rates of nonunion have ranged from 0% to 13%.10 However, surgery is associated with other harms, such as infection and iatrogenic radial nerve palsy.11,12 The only existing randomized clinical trial comparing functional bracing with surgery found no clinically important differences in reported outcomes, but 15% of the patients treated with a brace had secondary surgery due to nonunion.13 Despite the scarcity of evidence, the rate of surgical treatment has increased steadily: in 2011, up to 60% of humeral shaft fractures were treated surgically in the United States.14
This randomized clinical trial assessed the effectiveness of surgical treatment with open reduction and internal plate fixation vs nonsurgical treatment with functional bracing in the treatment of closed displaced humeral shaft fractures.
Methods
The FISH trial patient recruitment was conducted at the Helsinki and Tampere university hospitals in Finland from November 2012 to January 2018. Both sites are the primary regional referral centers for orthopedic trauma in their respective areas. The protocol of this trial (Supplement 1) was approved by the institutional review board of the Helsinki and Uusimaa Hospital District and has been published.15 The study was conducted in accordance with the Declaration of Helsinki. All patients gave written informed consent.
Participants
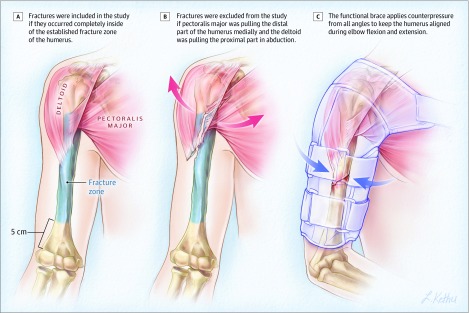
We enrolled patients 18 years or older referred to the emergency departments of the 2 participating trauma centers with a unilateral, displaced, and closed humeral shaft fracture (Figure 1 and Figure 2). Patients were excluded if they had a history of or had a condition affecting the function of the injured upper limb; pathological fracture; other concomitant injury affecting the same upper limb; other fracture; internal organ, brachial plexus, or vascular injury requiring surgery; cognitive disabilities preventing them from following the protocol; multimorbidity; or multiple trauma. Detailed inclusion and exclusion criteria are shown in eTable 1 in Supplement 2.
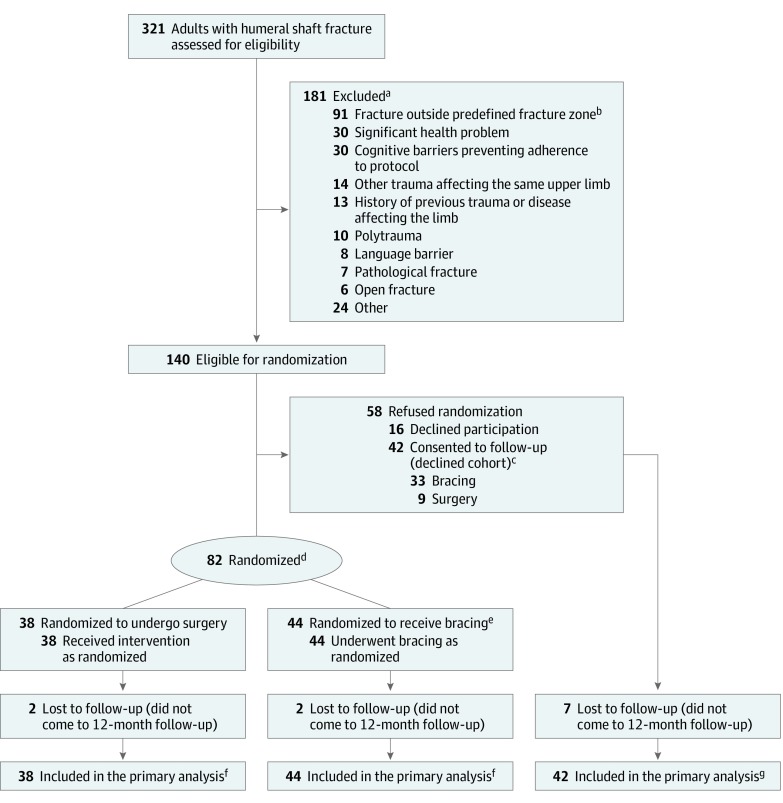
Figure 1. Enrollment, Randomization, and Analysis of Patients in the FISH Trial.
aThe reasons for exclusion are given in eTable 5 in Supplement 2. Patients could have had more than 1 reason for exclusion.
bQualifying fractures had to be in the area delimited proximally by the superior border of the pectoralis major tendon attachment and distally by the line lying 5 cm from the upper border of the olecranon fossa as evaluated from the x-ray.
cPatients who declined randomization were invited to participate in an observational cohort (declined cohort) that followed the study protocol and were treated according to their preference.
dBlock randomization conducted in groups of 4 with stratification by status of radial nerve and fracture type.
eThirteen patients randomized to the bracing group underwent surgery during the 12-month follow-up but were analyzed in the bracing group for the primary analysis.
fAll randomized patients with any data were included in the primary analysis. See eTable 6 in Supplement 2 for details on missing data.
gThe declined cohort was analyzed separately from the randomized cohort. All patients with any data were included in the analysis.
Figure 2. Illustration of the Fracture Zone, Excluded Fracture Type, and a Functional Brace.
Randomization
We used a block randomization (block size of 4, revealed to the study group only after data analysis) with separate, computer-generated randomization lists for both study centers, prepared by a statistician with no involvement in the trial. Two-fold stratification was used: status of the radial nerve, defined as (intact, paresthesia, or mild motor deficit; or either subtotal or total motor palsy) and fracture type (AO Foundation and Orthopaedic Trauma Association type A [simple fracture] or either type B [wedge fragment] or type C [multifragmentary fracture]).16 A research nurse with no involvement in the clinical care of patients prepared sequentially numbered, opaque, sealed envelopes according to the randomization lists. The envelopes were kept in a secure location at both study centers. After obtaining consent, a surgeon-member of the study group randomized participants by opening the next available numbered envelope to undergo either surgery or functional bracing.
Interventions
Surgery
In the surgery group, a standard open reduction and internal fixation was carried out with plate and screws. The surgery was performed either by or under the supervision of an experienced attending orthopedic trauma surgeon (experience defined in Supplement 2) within 14 days of the fracture. Patients were allowed to move their arm immediately postoperatively but were instructed to avoid weight-bearing until 6 weeks after surgery.
Functional Bracing
In the bracing group, a trained plaster technician applied a functional brace (Figure 2) that covered the arm from shoulder to elbow but left the motion of both of these joints free. Patients were given written and verbal instructions on how to cope with the brace and how to tighten it as the swelling subsided and were told to wear the brace until fracture union. The rehabilitation protocol followed the protocol by Sarmiento et al17 with minor modifications: active non–weight-bearing exercises of the elbow and hand and pendulum exercises of the shoulder were allowed immediately, followed by assisted exercises of the shoulder at 3 weeks, and finally, gradual weight-bearing at 6 weeks.
All patients had appointments with a physical therapist at 3 and 9 weeks to guide the recovery according to a structured rehabilitation program (eTables 2 and 3 in Supplement 2).
Prospective Observational Cohort
Eligible patients who did not consent to be randomized were then offered a possibility to participate in a concurrent prospective observational cohort (declined cohort). Those consenting to participate in the observational cohort received standard care (either surgery or bracing) according to their preference. Postoperative treatment and outcome measures were the same as in the randomized groups.
Outcomes
The primary outcome was Disabilities of Arm, Shoulder and Hand (DASH) score at 12 months. DASH is a validated, responsive, widely used patient-reported outcome measure for upper limb–related physical function and symptoms (score range, 0-100; 0 denotes no disability and 100 extreme disability; minimal clinically important difference [MCID], 10).18,19 When this trial began, we had originally decided to measure 3 primary outcomes: the DASH score, pain at rest, and pain in activities, all measured at 6 weeks and at 3, 6, and 12 months. During the recruitment phase, but before any data were assessed, the steering committee decided to include only the DASH score at 12 months as the primary outcome.
Secondary outcomes included pain at rest and pain on activities, both measured on an 11-point scale (0 to 10 numerical rating scale); the Constant-Murley outcome score, a widely used shoulder function score (range, 0 to 100; higher scores denote better function; MCID, 8.3) 20,21; elbow range of motion; DASH score at other follow-up time points; DASH work, sports, or performing arts modules (for details, see footnotes to Table 1); and the 15-dimensional (15D) tool,22 a generic health-related quality-of-life instrument (range, 0 to 1; higher scores denote better quality of life; MCID, 0.03). The patients’ general satisfaction with the function of the shoulder, elbow, and the entire injured upper limb was assessed on an 11-point scale. The proportion of patients with an acceptable symptomatic state was determined using patient’s global assessment of satisfaction regarding the injured arm and was elicited with the question, “How satisfied are you with the overall condition of your injured upper limb and its effect on your daily life?” Responses were given on a 7-point Likert scale. “Very satisfied” and “Satisfied” were categorized as having acceptable symptomatic state. All other responses—“Somewhat satisfied,” “Neither satisfied nor dissatisfied,” “Somewhat dissatisfied,” “Dissatisfied,” and “Very dissatisfied”—were categorized as not having an acceptable symptomatic state. The proportion of clinically recovered patients was determined at each follow-up time point. Patients reporting a DASH score within an MCID (10 points) of their preinjury score were considered to have adequate clinical recovery. The patients were also asked at 12 months to assess whether they would choose the same treatment again if they sustained a similar kind of injury later (yes or no).
Table 1. Baseline Demographics and Clinical Characteristicsa.
| Characteristic | No. (%) of patients | ||
|---|---|---|---|
| Surgery (n = 38) |
Bracing (n = 44) |
Declined cohort (n = 42) |
|
| Age at allocation, mean (SD) [range], y | 49.6 (18.2) [19-81] | 48.4 (16.2) [19-80] | 44.6 (17.3) [20-83] |
| Women | 18 (47.4) | 20 (45.5) | 16 (38.1) |
| Men | 20 (52.6) | 24 (54.5) | 26 (61.9) |
| Weight, mean (SD), kg | 83.5 (21.2) | 85.0 (15.6) | 84.4 (17.2) |
| Height, mean (SD), cm | 173 (9) | 174 (9) | 175 (10) |
| BMI, mean (SD) | 27.7 (5.9) | 28.1 (4.1) | 27.4 (4.4) |
| Smokers | 12 (31.6) | 9 (20.4) | 10 (23.8) |
| Radial nerve palsyb | 3 (7.9) | 2 (4.5) | 3 (7.1) |
| AO/OTA classification, type | |||
| A (simple) | 34 (89.5) | 36 (81.8) | 30 (68.2) |
| B (wedge fragment) | 4 (10.5) | 7 (15.9) | 11 (25.0) |
| C (segmental) | 0 | 1 (2.3) | 1 (2.2) |
| Fracture location, shaftc | |||
| Proximal | 2 (5.3) | 5 (11.4) | 2 (4.8) |
| Mid | 35 (92.1) | 37 (84.1) | 32 (76.2) |
| Distal | 1 (2.6) | 2 (4.5) | 8 (19.0) |
| Injury mechanismd | |||
| Low energy | 34 (89.5) | 38 (86.4) | 38 (90.5) |
| High energy | 4 (10.5) | 6 (13.6) | 4 (9.5) |
| Dominant limb injured | 20 (52.6) | 18 (40.9) | 22 (52.4) |
| Preinjury DASH scoree | |||
| Median (IQR) | 0.0 (0.0-2.5) | 0.4 (0.0-2.5) | 0.4 (0.0-1.9) |
| Optional work module, mean (SD)f | 0 | 0.2 (1.2) | 0.2 (1.2) |
| No. | 26 | 27 | 28 |
| Optional sports or performing arts module, mean (SD)f | 0 | 0.3 (1.4) | 1.0 (3.4) |
| No. | 23 | 19 | 26 |
| Preinjury 15D score, mean (SD)g | 0.95 (0.05) | 0.94 (0.05) | 0.94 (0.09) |
Abbreviations: AO/OTA, AO Foundation and Orthopaedic Trauma Association16; BMI, body mass index, calculated as weight in kilograms divided by height in meters squared; DASH, Disabilities of Arm, Shoulder and Hand; IQR, interquartile range.
Patients are included in the surgery and bracing groups as they were randomized.
Patients were categorized having radial nerve palsy when subtotal or total motor palsy was noted. Normal function, mild motor weakness, or sensory disturbance was categorized as no radial nerve palsy. Patients were stratified according to radial nerve status.
Fracture location is defined by the third of the diaphysis where the center of the fracture is located.
Injury mechanism is classified as high energy if the height of fall was over standing height or if the fracture was sustained in a traffic accident.
Widely used assessment and validated 30-item tool assessing upper-extremity symptoms in daily life (range, 0 [none] to 100 [extreme disability]). Values lower than 10 points represent a mean value in a randomly selected population aged between 20 and 60 years. Ten points is generally regarded as a minimal clinically important difference in DASH score.
Optional modules comprise 4 questions assessing the effect on work, sports, or performing arts (range, 0 [none] to 100 [extreme disability]). Ten points or lower indicate minimal limitations on performance, at most.
The 15-dimensional instrument is a generic health-related quality-of-life instrument (range, 1 [full health] to 0 [death]). Values higher than 0.9 are comparable with randomly selected Finnish population aged 30 years or older. At baseline the patient was asked to report the situation just before the fracture.
The questionnaires were administered at baseline and at each follow-up visit at 6 weeks, and at 3, 6, and 12 months after randomization (eTable 4 in Supplement 2). At baseline, we collected data on demographic and clinical characteristics and asked the patients to recall their status before fracture using DASH and the 15D questionnaires. At each follow-up visit, we assessed fracture union and potential complications—such as implant failure, malunion, and refracture—both clinically and using anteroposterior and lateral radiographs.
After the primary completion of the trial, a member of the study group not involved in the initial treatment of the given patient collected data on complications, adverse events, and reoperations from medical reports. Adverse events were categorized as serious or minor. For the adjudication of fracture nonunion and malunion, a panel of experienced orthopedic surgeons assessed all radiographs and patient reports. Nonunion was defined as no bridging fracture callus in 3 of the 4 cortices in anteroposterior and lateral radiographs taken at 3 months or later after the fracture and a notion of clinically verified motion at the fracture site.
Blinding
Outcome assessors carrying out objective measures were blinded to the treatment group during the follow-up visits by having the patients wear a long-sleeved shirt and not verbally reveal their study group.
Statistical Methods
The study was powered to detect a 10-point difference (SD, 14.68 points) in the DASH score18,23 between groups. The sample size of 35 participants per group was needed for 80% power and under the assumption of a 2-sided type I error rate of 5% to demonstrate that surgery had a clinically meaningful advantage over functional bracing. Anticipating a loss to follow-up of 12.5%, we planned to recruit 80 patients.
The trial was designed to ascertain whether after 12 months surgery was more effective than functional bracing. The primary analyses were performed according to randomization groups. The bracing group includes patients who later underwent surgery during the study period. We also conducted preplanned per-protocol and as-treated analyses. The per-protocol analysis included the surgery group, bracing group with no surgery, and the preplanned crossover group subanalysis of patients who could not follow the protocol for the entire study. In the as-treated analysis, the groups were analyzed according to their last treatment modality (surgery or nonoperative treatment). The numbers in the surgery group increased as patients in the bracing group had undergone surgery.
The primary comparison between groups was performed using a mixed-model repeated-measures analysis of variance. Study group and time of assessment (baseline, 6 weeks, 3, 6, and 12 months) were included as fixed factors, patients as random factors. The model included interactions between study group and time of assessment. Change from baseline was estimated with the baseline value as the covariate. The model was used to quantify the treatment effect as the absolute difference between the groups in DASH score (mean and 95% CIs) and P value at 12 months. A similar model was used to analyze secondary outcomes where applicable (pain at rest and during activities, 15D score, Constant-Murley Score). For categorical response variables, effects were analyzed using marginal logistic regression analysis. Because of the potential for type I error due to multiple comparisons, findings for analyses of secondary end points should be interpreted as exploratory. The mixed-model repeated-measures analysis of variance model allows missing data. No data were thus imputed. Patients with at least some data were included in the analysis. A post hoc sensitivity analysis with study site as a fixed factor was performed.
We interpreted the results of the trial according to a blinded data interpretation scheme.24 Briefly, an independent statistician provided the writing committee with blinded results from the preliminary analyses, the groups labeled as group A and group B. The committee considered the interpretation of the results until a consensus was reached and agreed upon in writing on the alternative interpretations of the findings. Once a consensus was reached, the minutes of the meeting were signed by all committee members (eAppendix in Supplement 2). After this common agreement was reached, the data manager broke the randomization code and the correct interpretation was chosen.
An independent statistician unaware of the group assignments performed all the analyses according to the previously published statistical analysis plan.15 The statistical analysis plan, outlining our statistical methods in more detail, is provided in Supplement 1. The threshold for statistical significance was set at level .05 with 2-sided testing. The data were analyzed using Stata version 15.1 with the “mixed” procedure (StataCorp LLC).
Results
Characteristics of the Patients
Of the 321 patients assessed for eligibility, 181 were excluded (eTable 5 in Supplement 2). Another 58 declined randomization. In the end, a total of 82 patients underwent randomization (Figure 1); 38 were assigned to undergo surgery, and 44, functional bracing. The baseline characteristics of the 2 groups were similar (Table 1). Four patients were lost to follow-up, 2 from each group. For a summary of missing data, see eTable 6 in Supplement 2.
Primary Outcome
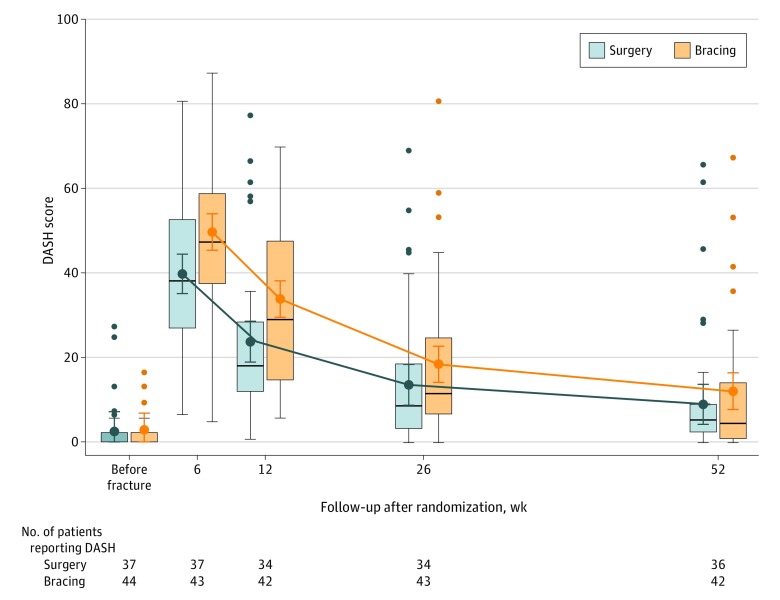
The mean DASH score in the surgery group was 8.9 (95% CI, 4.2 to 13.6) and 12.0 (95% CI, 7.7 to 16.4) in the bracing group at 12 months. There was no statistically significant difference between group means (surgery minus functional bracing; −3.1 points [95% CI, −9.6 to 3.3]; Table 2).
Table 2. Disabilities of Arm, Shoulder and Hand Scores for Primary and Secondary Outcomes at 12 Monthsa.
| Outcome | Mean (95% CI) | Between-group mean difference (95% CI) | P value | |
|---|---|---|---|---|
| Surgery (n = 38) | Bracing (n = 44) | |||
| Primary outcome | ||||
| DASH scoreb | 8.9 (4.2 to 13.6) | 12.0 (7.7 to 16.4) | −3.1 (−9.6 to 3.3) | .34 |
| Secondary outcomes | ||||
| Painc | ||||
| At rest | 0.94 (0.37 to 1.51) | 0.65 (0.12 to 1.18) | 0.29 (−0.49 to 1.07) | .47 |
| On activities | 2.21 (1.39 to 3.03) | 1.72 (0.95 to 2.49) | 0.49 (−0.65 to 1.63) | .40 |
| Constant-Murley scored | 78.1 (72.1 to 84.0) | 76.4 (70.9 to 81.8) | 1.7 (−6.4 to 9.8) | .68 |
| Elbow ROM, degreese | 143.5 (137.6 to 149.3) | 136.8 (131.4 to 142.2) | 6.6 (−1.3 to 14.6) | .10 |
| 15D scoreb | 0.95 (0.93 to 0.97) | 0.92 (0.90 to 0.94) | 0.03 (−0.01 to 0.07) | .13 |
| DASH module scoreb | ||||
| Work | 5.2 (0 to 15.3) | 8.0 (0 to 18.4) | −2.9 (−17.4 to 11.6) | .70 |
| Sports or performing arts | 6.7 (0 to 19.3) | 27.9 (15.4 to 40.3) | −21.2 (−38.9 to −3.4) | .02 |
| Patients with acceptable symptomatic state, %f | 82 (70 to 94) | 68 (54 to 82) | 14 (−6 to 34) | .16 |
| Adequate clinical recovery, %g | 86 (74 to 98) | 73 (59 to 87) | 13 (−5 to 31) | .15 |
| Satisfactionh | ||||
| Shoulder function | 8.5 (7.7 to 9.3) | 8.0 (7.3 to 8.7) | 0.5 (−0.6 to 1.6) | .36 |
| Elbow function | 9.0 (8.3 to 9.7) | 8.8 (8.2 to 9.4) | 0.2 (−0.7 to 1.2) | .62 |
| Upper-extremity function | 8.6 (7.8 to 9.4) | 7.6 (6.9 to 8.4) | 1.0 (−0.1 to 2.1) | .08 |
| Patients willing to repeat the same treatment, %i | 97 (91 to 100) | 71 (58 to 85) | 26 (11 to 40) | .003 |
Abbreviations: DASH, Disabilities of Arm, Shoulder and Hand; ROM, range of motion.
Complete data set of primary and secondary outcomes at different time points is given in Supplement 2. The 13 patients in the bracing group who had surgery are included in the bracing group. Point estimates are derived from the mixed-model repeated-measures analysis of variance using all available data. Trajectories of the analysis including the crossover group separately are presented in eFigure 2 (Supplement 2).
See Table 1 footnotes for scale definitions.
Ranges from 0 (no pain) to 10 (worst imaginable pain).
Assesses shoulder pain (0-15 points), activities of daily living (0-20 points), ROM (0-40), and strength (0-25 points) subscales. The total score ranges from 0 to 100; higher scores indicate better function. Scores of approximately 85 points are considered normal for those aged 40 to 60 years.
Measured by the physical therapist using goniometer and calculated using the difference in degrees between full flexion and full extension.
Patients with an acceptable symptomatic state was determined using patient’s global assessment of satisfaction regarding the injured arm. For patient-reported assessment language, see the Methods section.
DASH score within a minimal clinically important difference (10 points) of their preinjury score were considered to have adequate clinical recovery.
Satisfaction with shoulder, elbow, and upper-extremity function was reported on a 0 to 10 scale, for which 0 is the worst and 10 is the best condition.
Responses were given as yes or no.
Secondary Outcomes
There was a statistically significant between-group difference in the DASH score at 6 weeks of −9.9 points (95% CI, −16.3 to −3.5). The surgery group had a mean score of 39.8 (95% CI, 35.1 to 44.5) and the bracing group, 49.7 (95% CI, 45.4 to 54.0). At 3 months, the between-group difference was −10.1 points (95% CI, −16.6 to −3.6). The surgery group had a mean score of 23.8 (95% CI, 18.9 to 28.6); bracing group, 33.8 (95% CI, 29.5 to 38.1), reaching the threshold of clinical significance (MCID, 10 points) (Figure 3).
Figure 3. Disabilities of Arm, Shoulder and Hand Score Over Time.
The colored error bars indicate 95% CIs of the point estimates of group means; boxes, 25th and 75th percentiles of observed values; horizontal lines within boxes, median Disabilities of Arm, Shoulder and Hand (DASH) scores; black error bars, highest and lowest values within 1.5 times the interquartile range; data points beyond the error bars, individual values outside of this range. The 13 patients in the bracing group who underwent surgery are included in the bracing group. The “before fracture” time point represents patients’ perception of their DASH score prior to fracture. One patient did not report the DASH score at baseline (eTable 6, footnote c); no imputation was performed for missing data (eTable 7 for data and eFigure 3 for parallel line plot [Supplement 2]).
At 6 weeks, the surgery group had a pain-on-activities score mean of 4.4 points (95% CI, 3.6 to 5.2) and the bracing group, 5.6 points (95% CI, 4.8 to 6.3), a statistically significant between-group difference of −1.2 points (95% CI, −2.3 to −0.1); however, this difference did not reach the threshold for clinical importance (MCID, 1.5 points).
The Constant-Murley score had a statistically significant between-group difference at 6 weeks of 30.7 points (95% CI, 22.8 to 38.7; MCID, 8.3 points) with a mean score for the surgery group of 53.3 (95% CI, 47.5 to 59.2); the bracing group, 22.6 (95% CI, 17.2 to 28.0). The 3 month between-group difference was 14.9 points (95% CI, 6.9 to 22.9). The surgery group had a mean score of 61.9 (95% CI, 56.0 to 67.8); the bracing group, 46.9 (95% CI, 41.5 to 52.3). At 6 months, the between-group difference was 8.8 points (95% CI, 0.8 to 16.9). The surgery group had a mean score of 73.1 (95% CI, 67.1 to 79.0); the bracing group, 64.3 (95% CI, 58.9 to 69.7).
Eighty-six percent (95% CI, 74% to 98%) of the patients treated initially with surgery and 73% (95% CI, 59% to 87%) of those randomized initially to bracing reached the predetermined threshold for adequate clinical recovery at 12 months after the injury (no statistically significant difference between the groups, with the between-group difference of 13% (95% CI, −5% to 31%). A significantly higher proportion of patients, 97% (95% CI, 91% to 100%) in the surgery group than the 71% (95% CI, 58% to 85%) in the bracing group reported that they would prefer the same initial treatment if sustaining a similar fracture again (between-group difference, 26% [95% CI, 11% to 40%]). Table 2 summarizes the outcomes at the primary time point, at 12 months. All other time points are presented in eTable 7 and eFigure 1 in Supplement 2.
Adverse Events and Crossovers
Serious adverse events included 1 cardiac arrhythmia warranting cardioversion immediately postoperatively in the surgery group and 1 pulmonary embolism in the bracing group 4 weeks after the fracture. Both patients were older than 70 years and had associated comorbid conditions prior to sustaining the fracture. There were also 7 minor adverse events in the surgery group, including 3 temporary secondary radial nerve palsies, all of which resolved within 12 months, and 2 superficial wound infections treated with oral antibiotics. In the bracing group, there were 11 fracture nonunions (25%) and 13 of the 44 patients (30%) had secondary surgery during the 12-month follow-up period (crossover group). There were 4 other minor adverse events, 3 of which were related to secondary surgeries. For details on adverse events and crossovers, see Table 3.
Table 3. Adverse Events and Crossoversa.
| Description | No. of patients | |
|---|---|---|
| Surgery (n = 38) | Bracing (n = 44) | |
| Serious adverse event | ||
| Cardiovascular b | 1 | 1 |
| Minor adverse event | ||
| Fracture nonunionc | 0 | 11 |
| Refractured | 0 | 1 |
| Secondary temporary radial nerve palsye | 3 | 1 |
| Superficial wound infectionf | 2 | 1 |
| Wound seroma | 1 | 0 |
| Shoulder adhesive capsulitis | 1 | 1 |
| Loss of reductiong | 0 | 1 |
| Sensory disturbance in the forearmh | 0 | 1 |
| Reason for crossover to surgery | ||
| Nonunion (time range, 3-7.5 mo) | 8 | |
| Loss of reduction (at 6 wk) | 1 | |
| Refracture (at 8 mo) | 1 | |
| Intolerable pain in the fracture site (at 1 wk) | 1 | |
| Not tolerating the bracing (at 1 and 6 wk) | 2 | |
The 13 patients in the bracing group who had surgery are included in the bracing group.
One person in the surgery group had a cardiac arrhythmia warranting cardioversion in the recovery room after the operation. The patient has a history of cardiac arrhythmias. One person in the bracing group had a pulmonary embolism 4 weeks after the initial trauma and the reason for embolism was evaluated to be decreased mobility and staying mainly in bed because of the humeral fracture.
Eight patients underwent surgery at 12 months. The definition for nonunion and indication for an operation promoting union was no bridging fracture callus in 3 of the 4 cortices in x-ray (anteroposterior and lateral view) and clinically tested mobility in the fracture site at 12 weeks or later after the fracture. The proportion of patients with a fracture union observed in each group is presented in eTable 12 in Supplement 2.
One patient with 35° varus malunion underwent surgery due to a refracture of the humerus when doing bench press in the gym 8 months after the initial trauma. The fracture healed uneventfully.
All secondary radial nerve palsies resolved completely within 12 months. One patient in the bracing group had the secondary palsy after operation due to nonunion of the fracture.
All superficial wound infections healed with oral antibiotics without surgical intervention. One patient in the bracing group developed a superficial infection after surgical treatment due to loss of reduction.
The patient underwent surgery at 6 weeks after the initial trauma. The proximal side of the fracture was threatening the skin integrity.
The patient had a minor sensory disturbance of lateral antebrachial cutaneous nerve after the operation, which was done due to intolerable pain at the fracture site at one week after the initial trauma. The sensory disturbance was permanent.
Sensitivity and Subgroup Analyses
We performed sensitivity and subgroup analyses as prespecified in the protocol.15 At 12 months, there was no statistically significant differences between the groups in DASH scores. In the per-protocol analysis, the between-group difference was 0.4 points (95% CI, −6.5 to 7.4). The surgery group had a mean of 8.9 points (95% CI, 4.3 to 13.6) and the bracing group without crossovers had a mean of 8.5 points (95% CI, 3.4 to 13.6). The between-group difference in the as-treated analysis was 3.1 points (95% CI, −2.9 to 9.0). In the as-treated analysis, the DASH score for the surgery group with crossovers was 11.8 points (95% CI, 7.8 to 15.7) and for the bracing group without crossovers, 8.7 points (95% CI, 3.8 to 13.6) (eTable 8 in Supplement 2).
We also performed a post hoc sensitivity analysis with study site as a fixed effect in the statistical model and found no statistical significance in the between-group mean DASH score at 12 months with a difference of −3.1 points (95% CI, −9.6 to 3.3). The surgery group had a mean DASH score of 8.9 points (95% CI, 4.2 to 13.7); the bracing group, 12.0 points (95% CI, 7.7 to 16.4) (eTable 9 in Supplement 2). There was a statistically significant difference in the DASH score at 12 months between the subgroup of 13 patients with delayed surgery and initially surgically treated patients with the between-group mean difference of −11.1 points (95% CI, −20.1 to −2.1; surgery group 8.9 [95% CI 4.3 to 13.6]; crossover group 20.0 [95% CI, 12.3 to 27.7]) in favor of the initial surgery group (eTables 8 and 9 and eFigure 2 in Supplement 2).
Declined Cohort
Of the 58 eligible patients declining randomization, 42 consented to be followed up. Nine chose surgery and 33 functional bracing as their preferred treatment (Figure 1). At 12 months, there was no statistically significant difference between the groups, the between-group mean difference in the DASH score was 3.6 points (95% CI, −9.5 to 16.7). The surgery group had a mean score of 13.8 points (95% CI, 2.1 to 25.6) and the bracing group, 10.3 points (95% CI, −9.5 to 16.7) (eTable 10 in Supplement 2). The rates of fracture nonunions were 2 of 9 patients (22%) who underwent surgery and 6 of 33 patients (18%) who were treated with bracing (eTable 11 in Supplement 2).
Discussion
This multicenter randomized clinical trial involving patients with closed displaced humeral shaft fractures showed that surgery, compared with functional bracing, did not result in improved upper extremity function at 12 months.
To our knowledge, there has been only 1 previous randomized clinical trial13 comparing surgery using a minimally invasive plate osteosynthesis with functional bracing in the treatment of humeral shaft fractures. The DASH score for surgery exceeded that for bracing by 6 points at 6 months, which fell short of the predefined MCID of 10 points. In that trial,13 the rate of fracture nonunions was 15% in the bracing group, which is comparable with the corresponding rates observed in this trial, 11 of 44 (25%) (Table 3) and in the declined cohort, 6 of 33 (18%) (eTable 11 in Supplement 2). Although there were no fracture nonunions in patients randomized to surgery, there were 2 fracture nonunions in the surgically treated patients in the declined cohort. The overall rates of nonunion in this study, including randomized and nonrandomized patients were 2 of 47 patients (4%) who underwent surgery and 17 of 77 patients (22%) treated with bracing. These rates are consistent with the existing literature.7,8,9,10
Although the upper-extremity function was not significantly different in the 2 treatment groups at 12 months, the findings suggest that initial surgery provides a faster and more predictable course of recovery than functional bracing. This contention is based on the trajectories of outcomes (Figure 3; eFigures 1 and 2 in Supplement 2) and the high incidence of crossovers from functional bracing to surgery due to adverse events (Table 3). Thirteen of the 44 patients (30%) initially randomized to functional bracing underwent operative repair of their fracture during the 12-month follow-up period. These patients had lower upper-extremity function scores than did patients initially treated with surgery (eFigure 2 in Supplement 2).
Given the eligibility criteria, the findings of this trial are primarily applicable to patients able to engage in treatment plans with isolated, closed humeral shaft fractures treated in a high-volume trauma unit. Low loss to follow-up (5%) and inclusion of the declined cohort strengthen the generalizability of the findings.
Implications of the findings are sensitive to available resources. At a policy level, the faster return to function after initial surgery needs to be weighed against the inherent risks and resources required for surgery because approximately 70% of patients healed uneventfully with functional bracing in this trial. At an individual patient level, the findings support shared decision-making. Practitioners need to ascertain that patients’ values and preferences are respected while ensuring that patients are fully informed and capable of weighing the trade-off between the potential benefits and risks related to both treatment options. More reliable inferences about the comparative effectiveness of surgery and nonoperative treatment of humeral shaft fractures can be made after the 2 similarly designed ongoing randomized trials25,26 are completed.
Limitations
This study has several limitations. First, the results of this trial are not applicable to all displaced humeral shaft fractures, for 50% (91 of 181) of screened patients were excluded due to a fracture that extended either too proximally (n = 56) or too distally (n = 35) (eTable 5 in Supplement 2). These fractures generally require surgery and/or fracture fixation different from the procedure used in this trial (periarticular fracture fixation implants). Second, only patients able to engage in the protocol with closed, isolated fractures were included in this study, and patients with more complex injuries or comorbidities were excluded. Third, the estimates on the incidence of adverse events specific to certain procedures are subject to considerable uncertainty due to the relatively small sample size.
Conclusions
Among patients with closed humeral shaft fracture, internal fixation surgery, compared with nonoperative functional bracing, did not significantly improve functional outcomes at 12 months. However, the substantial amount of treatment crossover from nonoperative to surgical treatment should be considered when interpreting the trial results.
Trial Protocol and Statistical Analysis Plan
eTable 1. Inclusion and exclusion criteria used in the FISH trial
eTable 2. Rehabilitation protocol
eTable 3. Interventions
eTable 4. Schedule of enrollment, interventions and assessments
eTable 5. Reasons for exclusion in 181 patients
eTable 6. Missing data items (no. of patients)
eTable 7. Primary and Secondary Outcomes at Different Time Points
eTable 8. Sensitivity analysis: as-treated and per protocol with crossover group
eTable 9. Sensitivity analysis: Study site as a fixed effect in the statistical mode
eTable 10. DASH of the declined cohort
eTable 11. Adverse events and crossovers in the declined cohort
eTable 12. Proportion of patients with union of the fracture
eFigure 1. Trajectories of secondary outcomes
eFigure 2. Trajectories of Per Protocol analysis with Crossover group
eFigure 3. Parallel line plot of the surgery and bracing groups with crossovers
eAppendix. Blinded data interpretation meeting notes
Data Sharing Statement
References
- 1.Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37(8):691-697. doi: 10.1016/j.injury.2006.04.130 [DOI] [PubMed] [Google Scholar]
- 2.Tytherleigh-Strong G, Walls N, McQueen MM. The epidemiology of humeral shaft fractures. J Bone Joint Surg Br. 1998;80(2):249-253. doi: 10.1302/0301-620X.80B2.0800249 [DOI] [PubMed] [Google Scholar]
- 3.Kim SH, Szabo RM, Marder RA. Epidemiology of humerus fractures in the United States: nationwide emergency department sample, 2008. Arthritis Care Res (Hoboken). 2012;64(3):407-414. doi: 10.1002/acr.21563 [DOI] [PubMed] [Google Scholar]
- 4.Sarmiento A, Kinman PB, Galvin EG, Schmitt RH, Phillips JG. Functional bracing of fractures of the shaft of the humerus. J Bone Joint Surg Am. 1977;59(5):596-601. doi: 10.2106/00004623-197759050-00004 [DOI] [PubMed] [Google Scholar]
- 5.Toivanen JAK, Nieminen J, Laine HJ, Honkonen SE, Järvinen MJ. Functional treatment of closed humeral shaft fractures. Int Orthop. 2005;29(1):10-13. doi: 10.1007/s00264-004-0612-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Denard A Jr, Richards JE, Obremskey WT, Tucker MC, Floyd M, Herzog GA. Outcome of nonoperative vs operative treatment of humeral shaft fractures: a retrospective study of 213 patients. Orthopedics. 2010;33(8). doi: 10.3928/01477447-20100625-16 [DOI] [PubMed] [Google Scholar]
- 7.Westrick E, Hamilton B, Toogood P, Henley B, Firoozabadi R. Humeral shaft fractures: results of operative and non-operative treatment. Int Orthop. 2017;41(2):385-395. doi: 10.1007/s00264-016-3210-7 [DOI] [PubMed] [Google Scholar]
- 8.Harkin FE, Large RJ. Humeral shaft fractures: union outcomes in a large cohort. J Shoulder Elbow Surg. 2017;26(11):1881-1888. doi: 10.1016/j.jse.2017.07.001 [DOI] [PubMed] [Google Scholar]
- 9.Serrano R, Mir HR, Sagi HC, et al. Modern results of functional bracing of humeral shaft fractures: a multicenter retrospective analysis. J Orthop Trauma. 2020;34(4):206-209. doi: 10.1097/BOT.0000000000001666 [DOI] [PubMed] [Google Scholar]
- 10.Kurup H, Hossain M, Andrew JG. Dynamic compression plating versus locked intramedullary nailing for humeral shaft fractures in adults. Cochrane Database Syst Rev. 2011;19(6):CD005959. doi: 10.1002/14651858.CD005959.pub2 [DOI] [PubMed] [Google Scholar]
- 11.Claessen FMAP, Peters RM, Verbeek DO, Helfet DL, Ring D. Factors associated with radial nerve palsy after operative treatment of diaphyseal humeral shaft fractures. J Shoulder Elbow Surg. 2015;24(11):e307-e311. doi: 10.1016/j.jse.2015.07.012 [DOI] [PubMed] [Google Scholar]
- 12.Zhao J-G, Wang J, Meng X-H, Zeng X-T, Kan S-L. Surgical interventions to treat humerus shaft fractures: a network meta-analysis of randomized controlled trials. PLoS One. 2017;12(3):e0173634. doi: 10.1371/journal.pone.0173634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Matsunaga FT, Tamaoki MJS, Matsumoto MH, Netto NA, Faloppa F, Belloti JC. Minimally invasive osteosynthesis with a bridge plate versus a functional brace for humeral shaft fractures: a randomized controlled trial. J Bone Joint Surg Am. 2017;99(7):583-592. doi: 10.2106/JBJS.16.00628 [DOI] [PubMed] [Google Scholar]
- 14.Schoch BS, Padegimas EM, Maltenfort M, Krieg J, Namdari S. Humeral shaft fractures: national trends in management. J Orthop Traumatol. 2017;18(3):259-263. doi: 10.1007/s10195-017-0459-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rämö L, Taimela S, Lepola V, Malmivaara A, Lähdeoja T, Paavola M. Open reduction and internal fixation of humeral shaft fractures versus conservative treatment with a functional brace: a study protocol of a randomised controlled trial embedded in a cohort. BMJ Open. 2017;7(7):e014076. doi: 10.1136/bmjopen-2016-014076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kellam JF, Meinberg EG, Agel J, Karam MD, Roberts CS. Introduction: fracture and dislocation classification compendium-2018: International Comprehensive Classification of Fractures and Dislocations Committee. J Orthop Trauma. 2018;32(suppl 1):S1-S170. doi: 10.1097/BOT.0000000000001063 [DOI] [PubMed] [Google Scholar]
- 17.Sarmiento A, Zagorski JB, Zych GA, Latta LL, Capps CA. Functional bracing for the treatment of fractures of the humeral diaphysis. J Bone Joint Surg Am. 2000;82(4):478-486. doi: 10.2106/00004623-200004000-00003 [DOI] [PubMed] [Google Scholar]
- 18.Gummesson C, Atroshi I, Ekdahl C. The Disabilities of the Arm, Shoulder, and Hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet Disord. 2003;4:11. doi: 10.1186/1471-2474-4-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beaton DE, Katz JN, Fossel AH, Wright JG, Tarasuk V, Bombardier C. Measuring the whole or the parts? validity, reliability, and responsiveness of the Disabilities of the Arm, Shoulder, and Hand outcome measure in different regions of the upper extremity. J Hand Ther. 2001;14(2):128-146. doi: 10.1016/S0894-1130(01)80043-0 [DOI] [PubMed] [Google Scholar]
- 20.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;(214):160-164. doi: 10.1097/00003086-198701000-00023 [DOI] [PubMed] [Google Scholar]
- 21.Hao Q, Devji T, Zeraatkar D, et al. Minimal important differences for improvement in shoulder condition patient-reported outcomes: a systematic review to inform a BMJ Rapid Recommendation. BMJ Open. 2019;9(2):e028777. doi: 10.1136/bmjopen-2018-028777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sintonen H. The 15D instrument of health-related quality of life: properties and applications. Ann Med. 2001;33(5):328-336. doi: 10.3109/07853890109002086 [DOI] [PubMed] [Google Scholar]
- 23.Hunsaker FG, Cioffi DA, Amadio PC, Wright JG, Caughlin B. The American Academy of Orthopaedic Surgeons outcomes instruments: normative values from the general population. J Bone Joint Surg Am. 2002;84(2):208-215. doi: 10.2106/00004623-200202000-00007 [DOI] [PubMed] [Google Scholar]
- 24.Järvinen TLN, Sihvonen R, Bhandari M, et al. Blinded interpretation of study results can feasibly and effectively diminish interpretation bias. J Clin Epidemiol. 2014;67(7):769-772. doi: 10.1016/j.jclinepi.2013.11.011 [DOI] [PubMed] [Google Scholar]
- 25.Berry GK. Operative and nonoperative treatment of humeral shaft fractures. ClinicalTrials.gov. Accessed December 8, 2019. https://clinicaltrials.gov/ct2/show/NCT00878319
- 26.Oliver WM, Carter TH, Graham C, et al. A prospective randomised controlled trial of operative versus non-operative management of fractures of the humeral diaphysis: the Humeral Shaft Fracture Fixation (HU-FIX) Study protocol. Trials. 2019;20(1):475. doi: 10.1186/s13063-019-3576-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol and Statistical Analysis Plan
eTable 1. Inclusion and exclusion criteria used in the FISH trial
eTable 2. Rehabilitation protocol
eTable 3. Interventions
eTable 4. Schedule of enrollment, interventions and assessments
eTable 5. Reasons for exclusion in 181 patients
eTable 6. Missing data items (no. of patients)
eTable 7. Primary and Secondary Outcomes at Different Time Points
eTable 8. Sensitivity analysis: as-treated and per protocol with crossover group
eTable 9. Sensitivity analysis: Study site as a fixed effect in the statistical mode
eTable 10. DASH of the declined cohort
eTable 11. Adverse events and crossovers in the declined cohort
eTable 12. Proportion of patients with union of the fracture
eFigure 1. Trajectories of secondary outcomes
eFigure 2. Trajectories of Per Protocol analysis with Crossover group
eFigure 3. Parallel line plot of the surgery and bracing groups with crossovers
eAppendix. Blinded data interpretation meeting notes
Data Sharing Statement