Abstract
Background:
There is no consensus regarding the best treatment approach for middle-aged patients with anterior cruciate ligament (ACL) injuries. Chronic ACL-deficient knees are often associated with instability as well as secondary meniscal and cartilage lesions. ACL reconstruction (ACLR) has achieved satisfactory outcomes in younger patients; however, the effectiveness and safety of ACLR in middle-aged patients remain uncertain.
Purpose:
To compare the patient-reported functional scores, arthrometric outcomes, and complications of primary ACLR between older (≥50 years) and younger (<50 years) patients.
Study Design:
Systematic review; Level of evidence, 3.
Methods:
We conducted a systematic review of cohort studies that compared the clinical outcomes of ACLR between patients aged ≥50 years and those aged <50 years. The Cochrane Central Register of Controlled Trials, Embase, and MEDLINE databases were searched for relevant studies. The Methodological Index for Non-randomized Studies (MINORS) criteria was used to assess the risk of bias and conducted a random-effects meta-analysis to combine the data, and the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach was used to evaluate the overall quality of the body of retrieved evidence. The primary outcome was knee functional outcomes, and secondary outcomes were arthrometric outcomes of ACLR and complications.
Results:
This study included 4 retrospective cohort studies with a total of 287 participants (129 in the older group and 158 in the younger group). All included studies reported significant improvements in clinical outcomes in both groups after ACLR. No significant differences were noted in the improvement of International Knee Documentation Committee (IKDC) scores (mean difference [MD], 0.20 [95% CI, −2.65 to 3.05]; P = .89) and Lysholm scores (MD, −1.98 [95% CI, −6.93 to 2.98]; P = .43) between the 2 groups. No significant differences were observed in anteroposterior stability or risk of complications between the groups.
Conclusion:
ACLR may be performed in middle-aged patients (≥50 years) without concern for inferior clinical and arthrometric results compared with younger patients (<50 years).
Keywords: ACL, ACL reconstruction, older patients, systematic review, meta-analysis
The incidence of isolated anterior cruciate ligament (ACL) tears is 68.6 per 100,000 person-years.34 ACL-deficient knees may cause chronic knee instability, cartilage injuries, and complex unrepairable meniscal tears.18,26,40 Affected patients are required to give up the practice of highly demanding sports, reduce their workload, and even adopt a sedentary lifestyle, which directly affects their quality of life. With improvements in instrumental and surgical techniques, arthroscopic ACL reconstruction (ACLR) has demonstrated promising clinical outcomes.17 In terms of societal and economic impacts, arthroscopic ACLR is more cost-effective than nonoperative treatment.25 Therefore, ACLR has become the mainstay of treatment for ACL insufficiency in young and active patients and for those who fail nonoperative therapy or do not want to change an active lifestyle.22,31
The treatment for ACL injuries in middle-aged patients remains controversial. Because older patients may not perform highly demanding activities and they may have inferior surgical outcomes due to pre-existing knee chondral injuries, nonoperative treatment is usually preferred. However, with a longer life expectancy and improved physiological health, older people participate in more physically demanding sports than previously.3,6 In addition, because nonoperative treatment for ACL injuries was reported to be associated with a relatively high risk for reinjuries and residual instability,9 more middle-aged patients have undergone ACLR to prevent decreased knee function and to maintain an active lifestyle.37,41
Previous studies have mainly focused on patients older than 40 years, finding similar clinical outcomes between patients older than 40 years and those younger than 25 years after ACLR.21,23 Although several studies have reported no significant difference in clinical outcomes after ACLR between patients older than 50 years and young patients,3,17,32 few have systematically reviewed the literature to compare the benefits and adverse outcomes of ACLR between these patient groups.
In this study, we systematically evaluated the outcomes of ACLR in patients older than 50 years. Our hypothesis was that patients older than 50 years would have outcomes comparable to those of patients younger than 50 years after arthroscopic ACLR.
Methods
Search Strategy
The reporting in this systematic review follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.30 Studies that included patients who underwent arthroscopic ACLR and compared patients older than 50 years with those younger than 50 years were eligible for inclusion. We searched for relevant studies in the Cochrane Central Register of Controlled Trials (CENTRAL), Embase, and MEDLINE databases from inception to April 30, 2019 using the following keywords: “anterior cruciate ligament” and “age.” We used both MeSH terms and free text and utilized Boolean operators to combine them in searching. The search strategy is detailed in the Appendix. Furthermore, we checked ongoing studies on this topic from the United States National Institutes of Health trial registry (http://clinicaltrials.gov). Moreover, we contacted experts in this specialty for any ongoing investigations or unpublished data on this issue. In addition, we went through the references of potential studies for potentially eligible trials. No language restriction was applied.
Selection Criteria
We included studies that (1) were randomized controlled trials or comparative studies and (2) compared the outcomes of patients older than 50 years and those younger than 50 years after arthroscopic ACLR. We excluded (1) studies that involved revision surgery without separate data, (2) nonhuman studies, (3) single-arm case series without a control group, and (4) studies with no usable data. After removing duplicates, 2 authors (C.-W.T. and L.-T.K.) independently selected studies according to the inclusion criteria. Irrelevant studies were eliminated after checking the titles and abstracts, then the full text of potentially relevant studies was obtained. We also confirmed the inclusion of these studies after checking the full text against the inclusion and exclusion criteria. Disputes were resolved through discussion, and the opinion of a third author (C.-C.C.) was requested if necessary.
Data Extraction
There were 2 authors (C.-W.T. and L.-T.K.) who independently extracted data from the included studies using a standardized data collection form. The following information was included: first author, year of publication, study design (patient selection and concealment), details of the participants (eg, number, age, and sex), type of tendon graft, fixation device for the tendon graft, and outcome data, which included functional scores, knee anteroposterior (AP) stability, and adverse events. A third author (C.-C.C.) arbitrated when the 2 authors disagreed.
The primary outcome was knee function, measured by functional scores. Our secondary outcomes included knee AP stability as measured using an arthrometer, as well as adverse events, including arthrofibrosis and the need for secondary procedures.
Quality Assessment
The same 2 authors (C.-W.T. and L.-T.K.) independently evaluated the risk of bias of the included randomized controlled trials using The Cochrane Collaboration’s tool.12,13 A third author (C.-C.C.) arbitrated when the 2 authors disagreed. We used the Methodological Index for Non-randomized Studies (MINORS) to assess the methodological quality of nonrandomized studies.39
The same 2 authors independently evaluated the quality of the body of evidence using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach.36 We assessed 5 domains and rated the strength of evidence for each outcome (GRADEpro, Version 2.0; McMaster University).10
Data Synthesis and Statistical Analysis
We conducted a random-effects meta-analysis for all outcomes to address the expected inherent clinical heterogeneity among the included studies.7 Data were expressed as the risk ratio (RR) with a 95% confidence interval (CI) for dichotomous data and as the mean difference (MD) or standardized MD with a 95% CI for continuous data. A P value <.05 was considered statistically significant. Chi-square and I 2 statistics were used to assess statistical heterogeneity with a level of significance set at P < .10. I 2 values of 0.0%-24.9%, 25.0%-49.9%, 50.0%-74.9%, and 75.0%-100.0% indicated no, low, moderate, and high heterogeneity, respectively.14,15 A subgroup analysis was performed if there was significant heterogeneity. In addition, between-study variance was estimated using tau-square (τ2) statistics.13 We calculated the mean and variance from the reported median, range, and sample size if the standard deviation of continuous data was not reported in the published article.16 When the standard deviation and range were not available, variance was estimated from the P value using the t test. If there were no raw data for analysis, we used a software program to extract the details from published graphs.29 Forest plots were used to report the synthetic results. Review Manager 5.3 (The Nordic Cochrane Centre, The Cochrane Collaboration) was used for the meta-analysis.
Results
Study Selection
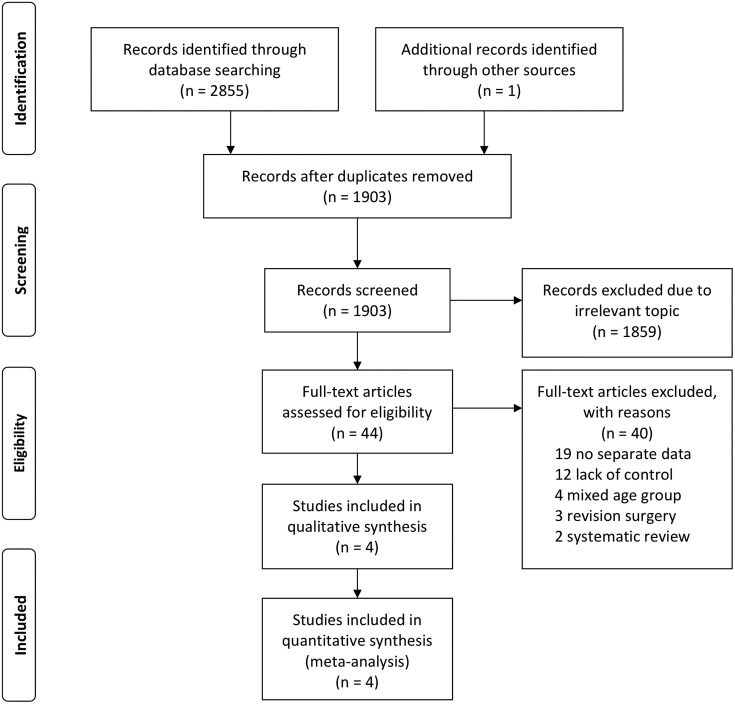
A total of 2855 records were identified after searching the CENTRAL, MEDLINE, and Embase databases (Figure 1). An additional record was identified from the references of an included study, and no ongoing trials were detected after searching the trial registry and consulting specialists. We eliminated 953 duplicates, leaving 1903 records. Of these, 1859 records were excluded after checking their titles and abstracts. After checking the full text of the remaining 44 studies against the inclusion and exclusion criteria, 40 records were excluded, 19 for not having separate data, 12 for lack of a control group, and the remaining 9 for other reasons. Ultimately, 4 nonrandomized studies were included in this review (Figure 1).3,17,20,32
Figure 1.
PRISMA flow diagram of the study.
The 4 included studies,3,17,20,32 consisted of 287 participants (129 in the older group and 158 in the younger group) (Table 1). These studies were published between 2011 and 2019, and their sample size ranged from 40 to 90 participants. All included studies examined patients with ACL deficiency who underwent arthroscopic ACLR. With the exception of Cinque et al,3 the studies excluded patients with high-grade (grade 3 or 4) chondral injuries,17 advanced osteoarthritis (OA) (joint space narrowing >50%),20,32 and multiple ligament injuries. One study32 included patients with acute ACL deficiency; another study20 included patients with chronic ACL deficiency; and the third study3 included both patients with acute and chronic ACL deficiency, although the distribution across the 2 groups did not differ. Most of the included studies evaluated patients for more than 2 years,3,17,32 except for Kim et al,20 who evaluated patients for 1 year only. The details of patient characteristics, as well as the inclusion and exclusion criteria, are presented in Table 1.
Table 1.
Characteristics of Included Studiesa
| Author (Year) | Inclusion and Exclusion Criteria | Patients (M/F), n | Age,b y | Time to Surgery,c mo | Follow-up,d mo | Outcomes | Qualitye |
|---|---|---|---|---|---|---|---|
| Osti32 (2011) | Inclusion: ACL deficiency Exclusion: previous knee surgery or lower limb fracture, severe OA (joint space narrowing >50%), severe associated ligament injury |
O: 20 (12/8) Y: 20 (12/8) |
O: 56 (50-62) Y: 27 (17-30) |
O: 2.87 (2.40-3.33) Y: 2.80 (2.37-3.13) |
O: 32 (24-49) Y: 33 (24-44) |
Lysholm, IKDC, AP laxity (KT-1000 arthrometer), radiological evaluation, physical examination (Lachman, pivot shift), complications | 14/24 |
| Cinque3 (2017) | Inclusion: age 20-30 and 50-70 y, ACL deficiency Exclusion: previous knee infection or fracture, previous cartilage or meniscal surgery |
O: 33 (14/19) Y: 52 (33/19) |
O: 56 (50-62) Y: 27 (17-30) |
O: 21 acute/12 chronic Y: 30 acute/22 chronic |
O: 37.2 Y: 40.8 | SF-12, WOMAC, Lysholm, IKDC, Tegner, complications | 20/24 |
| Iorio17 (2018) | Inclusion: age >50 y, ACL deficiency Exclusion: severe associated ligament injury other than ACL, grade 3 or 4 cartilage damage,f BMI >29.9 kg/m2, previous knee surgery |
O: 36 (28/8) Y: 36 (25/11) |
O: 54.0 ± 3.69 Y: 32.5 ± 2.73 |
N/A | O: 64 (60-72) Y: 78 (60-84) |
Lysholm, IKDC, Tegner, AP laxity (KT-1000 arthrometer), OA change (radiological evaluation), mean time to return to sports | 19/24 |
| Kim20 (2019) | Inclusion: ACL deficiency Exclusion: previous ACL surgery, multiple knee ligament injury, ipsilateral lower limb surgery, severe OA (joint space narrowing >50%) |
O: 40 (40/0) Y: 50 (50/0) |
O: 52.8 ± 2.5 Y: 28.9 ± 5.1 |
O: 23.8 (16.5-30.1) Y: 20.5 (12.4-28.7) |
O: 12 Y: 12 |
Lysholm, IKDC, AP laxity (KT-2000 arthrometer), isokinetic strength | 19/24 |
aACL, anterior cruciate ligament; AP, anteroposterior; BMI, body mass index; F, female; IKDC, International Knee Documentation Committee; M, male; N/A, not available; O, older group; OA, osteoarthritis; SF-12, Short Form–12; WOMAC, Western Ontario and McMaster Universities Arthritis Index; Y, younger group.
bExpressed as mean ± SD or median (range).
cExpressed as No. or mean (95% CI).
dExpressed as mean, or median (range).
eEvaluated according to the Methodological Index for Non-randomized Studies (MINORS).
fEvaluated using the Outerbridge classification.
Single-bundle ACLR was used as the surgical technique in all of the included studies. The transtibial femoral tunnel drilling technique was used in 1 study,32 whereas the anteromedial femoral tunnel drilling technique was used in the remaining 3 studies.3,17,20 Also, 3 of the included studies reported information on the tendon grafts. A gracilis and semitendinosus tendon (GST) autograft was used in 2 of the included studies,17,20 and a bone–patellar tendon–bone (BPTB) autograft and allograft were both used in the study by Cinque et al.3 Additional surgical details are presented in Table 2.
Table 2.
Surgical Details of Included Studiesa
| Author (Year) | Associated Cartilageb or Ligamentous Injury, n | Meniscal Injury (Repair/Resection), n |
Graft Type | Tunnel Technique | Fixation Method |
|---|---|---|---|---|---|
| Osti32 (2011) | O: 1 I/3 II/4 III/2 IV Y: 1 I/3 II/1 III/0 IV |
O: 11 (1/10) Y: 8 (2/6) |
N/A | Transtibial single bundle | N/A |
| Cinque3 (2017) | O: 17 I/6 II/6 III/4 IV Y: 43 I/2 II/6 III/1 IV Concomitant ligament injury: O: 14 FCL/6 MCL Y: 7 FCL/5 MCL |
O: 31 (16/15) Y: 42 (30/12) |
O: 18 BPTB allograft/15 BPTB autograft Y: 19 BPTB allograft/33 BPTB autograft |
Anteromedial single bundle | Femur: cannulated titanium interference screw Tibia: cannulated titanium interference screw |
| Iorio17 (2018) | N/A | N/A | Double GST autograft | Anteromedial single bundle | Femur: Swing-Bridge device Tibia: Evolgate device |
| Kim20 (2019) | N/A | O: 37 (21/16) Y: 41 (29/12) |
Quadruple GST autograft | Anteromedial single bundle | Femoral: cortical suspensory device (Endobutton CL) Tibia: bioabsorbable interference screw with post tie |
aBPTB, bone–patellar tendon–bone; FCL, fibular collateral ligament; GST, gracilis and semitendinosus tendon; MCL, medial collateral ligament; N/A, not available; O, older group; Y, younger group.
bEvaluated using the Outerbridge classification.
Study Quality
All included studies were nonrandomized controlled studies, and the risk of bias within the studies was analyzed according to the MINORS.39 The scores varied from 14 to 20 (median, 19) for comparative studies (maximum score, 24). Most studies had a clear aim and appropriate endpoints; however, the unbiased endpoint assessment and prospectively calculated sample size were rarely mentioned (Table 1).
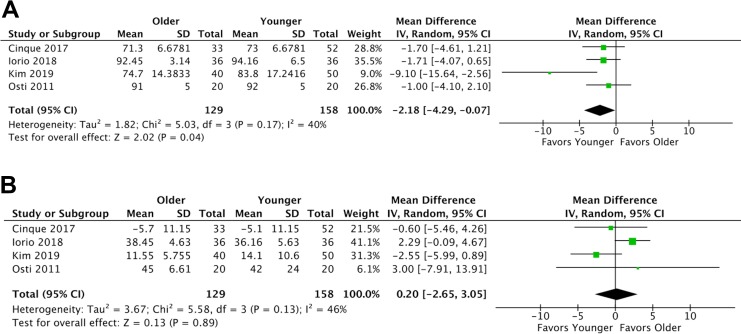
IKDC Score
A summary of all results from the meta-analysis is presented in Table 3. All 4 included studies reported preoperative and postoperative International Knee Documentation Committee (IKDC) scores for the 2 groups. The older and younger groups had similar preoperative IKDC scores among all included studies. The meta-analysis revealed that the younger group had a significantly higher IKDC score than the older group at the end of follow-up (MD, −2.18 [95% CI −4.29 to −0.07]; P = .04) (Figure 2A and Table 3). No significant difference in the improvement of IKDC scores was noted between the younger and older groups (MD, 0.20 [95% CI, −2.65 to 3.05]; P = .89) (Figure 2B and Table 3).
Table 3.
Clinical and Functional Outcomesa
| No. of Studies | No. of Patients | MD/RR (95% CI) | P Value | |
|---|---|---|---|---|
| IKDC | ||||
| Absolute scoreb | 4 | 287 | –2.18 (–4.29 to –0.07) | .04 |
| Improvementc | 4 | 287 | 0.20 (–2.65 to 3.05) | .89 |
| Lysholm | ||||
| Absolute scoreb | 4 | 287 | –1.87 (–3.90 to 0.15) | .07 |
| Improvementc | 4 | 287 | –1.98 (–6.93 to 2.98) | .43 |
| Tegner | ||||
| Absolute scoreb | 2 | 157 | –0.53 (–1.09 to 0.04) | .07 |
| Improvementc | 2 | 157 | –0.10 (–0.69 to 0.49) | .75 |
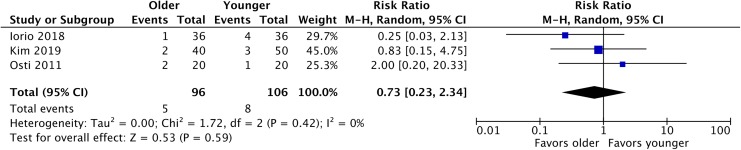
| Knee AP stability | 3 | 202 | 0.73 (0.23 to 2.34) | .59 |
aAP, anteroposterior; IKDC, International Knee Documentation Committee; MD, mean difference; RR, risk ratio.
bAt 1 to 2 years after index surgery.
cDifference between the last follow-up and baseline.
Figure 2.
Forest plot of International Knee Documentation Committee (IKDC) scores. (A) Total score at the end of follow-up. (B) Improvement at the end of follow-up from baseline.
Lysholm Knee Score
All 4 of the included studies reported preoperative and postoperative Lysholm scores for the 2 groups. Overall, the older and younger groups had similar preoperative Lysholm scores. The meta-analysis revealed that these 2 groups had similar Lysholm scores at the end of follow-up (MD, −1.87 [95% CI, −3.90 to 0.15]; P = .07) (Figure 3A and Table 3). Moreover, the improvement in Lysholm scores was not significantly different between the older and younger patients (MD, −1.98 [95% CI, −6.93 to 2.98]; P = .43) (Figure 3B and Table 3). Significant heterogeneity existed across these studies (I 2 = 63%; P = .04).
Figure 3.
Forest plot of Lysholm knee scores. (A) Total score at the end of follow-up. (B) Improvement at the end of follow-up from baseline.
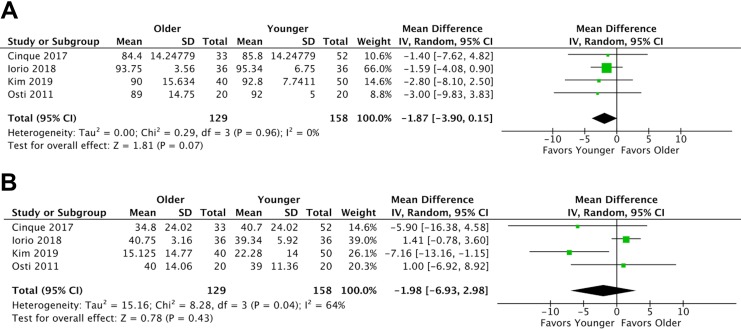
Return to Physical Activity
Of the 4 included studies, 3 evaluated return to physical activity between older and younger patients.3,17,32 One study used the IKDC score,32 and the other 2 studies used the Tegner activity scale.3,17 The meta-analysis revealed no significant difference in Tegner scores at the end of follow-up (MD, −0.53 [95% CI, −1.09 to 0.04]; P = .07) (Figure 4A and Table 3) or in the improvement of Tegner scores between the younger and older groups (MD, −0.10 [95% CI, −0.69 to 0.49]; P = .75) (Figure 4B and Table 3).
Figure 4.
Forest plot of Tegner activity scores. (A) Total score at the end of follow-up. (B) Improvement at the end of follow-up from baseline.
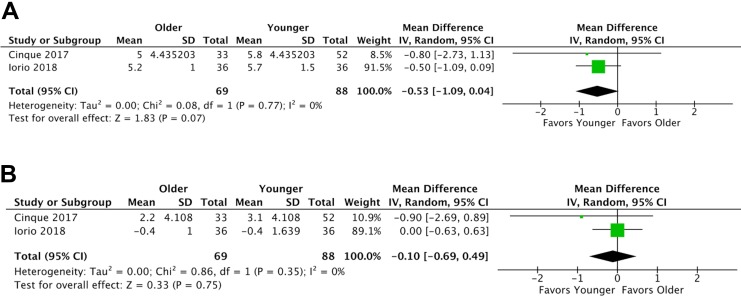
Knee AP Stability
Postoperative knee AP stability was measured by the mean side-to-side difference at maximal manual traction. Instability was defined as a mean side-to-side difference of greater than 5 mm. We found that 3 of the included studies reported outcomes in knee AP stability.17,20,32 In 2 studies,17,32 patients were evaluated with a KT-1000 arthrometer (MEDmetric) and in 1 study20 with a KT-2000 arthrometer (MEDmetric). The incidence of knee AP laxity was 5.2% (5/96) in the older group and 7.5% (8/106) in the younger group. The meta-analysis revealed no difference between the 2 groups (RR, 0.73 [95% CI, 0.23-2.34]; P = .59) (Figure 5 and Table 3).
Figure 5.
Forest plot of postoperative knee laxity.
Complications
All 4 studies assessed postoperative complications, including ACL graft failure, arthrofibrosis, and the need for revision surgery after ACLR. Osti et al32 reported 1 case of ACL graft failure in the older group. The incidence of arthrofibrosis was 12% (4/33) in the older group and 13% (7/52) in the younger group in the study by Cinque et al3; no significant difference in the rate of arthrofibrosis was noted between the groups. No complications were recorded in the other 2 studies.17,20
GRADE Findings
We used the GRADE approach to rate the overall quality of the evidence indicating that ACLR outcomes did not differ between patients older versus younger than 50 years. Overall, the quality of evidence was very low. The quality of evidence was downgraded by the high risk of selection bias (lack of randomization), performance bias (lack of blinding in participants), and imprecision. Details of the judgment are presented in Tables 4 and 5.
Table 4.
Overall Quality of Evidence According to GRADE Assessmenta
| No. of Patients/Studies | Certainty Assessment | ||||||
|---|---|---|---|---|---|---|---|
| Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | Overall Certainty of Evidenceb | ||
| IKDC score | 287/4 (observational) | Not serious | Not serious | Not serious | Seriousc | None | Very low |
| Lysholm score | 287/4 (observational) | Not serious | Not serious | Not serious | Seriousc | None | Very low |
| Tegner score | 157/2 (observational) | Not serious | Not serious | Not serious | Seriousc | None | Very low |
| Knee laxity | 202/3 (observational) | Not serious | Not serious | Not serious | Seriousc | None | Very low |
aGRADE, Grading of Recommendations Assessment, Development and Evaluation; IKDC, International Knee Documentation Committee.
bOverall certainty of evidence: very low, low, moderate, and strong.
cDid not meet optimal information size criterion.
Table 5.
Overall Study Findingsa
| No. of Patients | Relative Effect (95% CI) |
Anticipated Absolute Effect | |||
|---|---|---|---|---|---|
| Younger Group | Older Group | Younger Group | Older Group | ||
| IKDC score | 158 | 129 | — | Mean IKDC score, 20.76 | MD, 0.2 higher (2.65 lower to 3.05 higher) |
| Lysholm score | 158 | 129 | — | Mean Lysholm score, 35 | MD, 1.98 lower (6.93 lower to 2.98 higher) |
| Tegner score | 88 | 69 | — | Mean Tegner score, –0.02 | MD, 0.10 lower (0.69 lower to 0.49 higher) |
| Knee laxity | 8/106 (7.5%) | 5/96 (5.2%) | RR, 0.73 (0.23 to 2.34) |
75 per 1000 | 20 fewer per 1000 (58 fewer to 101 more) |
aIKDC, International Knee Documentation Committee; MD, mean difference; RR, risk ratio.
Discussion
We systematically evaluated and compared the efficacy and safety of arthroscopic ACLR between patients older than 50 years and those younger than 50 years. Our study results indicated that patients older than 50 years had comparable results in terms of knee stability and improvement of knee function, based on IKDC, Lysholm, and Tegner scores, to those of younger patients. Because of their low incidence, we are uncertain if there is a difference in terms of complications between the 2 groups. Thus, we found that ACLR was an effective procedure for treating ACL insufficiency in patients older than 50 years.
The potentially high risk of unfavorable outcomes, including arthrofibrosis and OA progression, has been a major concern in older patients undergoing ACLR.1,6 Pre-existing chondral lesions and a prolonged time from injury to surgery are risk factors for OA progression after ACLR,4 and preoperative cartilage lesions have been associated with poor clinical outcomes after ACLR.8 In the current review, 3 of the included studies reported preoperative cartilage status: 1 study excluded patients with high-grade chondral lesions (Outerbridge grade 3 and 4).17 The other 2 studies included patients who had undergone concomitant treatment for various cartilage conditions, including radiofrequency ablation and microfracture.3,32 In addition, a prolonged time from injury to surgery of more than 1 year has been associated with an increased number and severity of cartilage lesions in ACL-deficient knees.26,27 In this review, patients in the study by Kim et al20 underwent surgery within an average of 20 months from injury, and those in the study by Iorio et al17 underwent surgery no longer than 2 years from injury. One of the studies enrolled patients with both acute and chronic ACL injuries.3 The variety of pre-existing chondral injuries and prolonged times to surgery in the included studies, which affected the clinical outcomes in an unpredictable manner, may have caused difficulties in the interpretation of findings.
In this review, 2 of the included studies reported outcomes at more than 3 years. Cinque et al3 and Osti et al32 both revealed no significant OA progression after ACLR in patients older than 50 years. An 11.3% (95% CI, 6.4%-19.1%) rate of OA progression after ACLR was reported in a 2018 systematic review.4 Patient age and time from injury to surgery were associated with an increased likelihood of posttraumatic OA after ACLR.3 In this review, the influence of pre-existing chondral injuries and time to surgery was similar across the 2 groups in each study, which may erase some bias in the interpretation of the combined results. Moreover, the improvement in clinical outcomes did not differ between the 2 groups, which implies that patients older than 50 years can have similar clinical outcomes to those of younger patients, regardless of pre-existing chondral lesions and potential OA changes after ACLR.
Despite dissimilar clinical outcomes, both meniscal repair and meniscectomy are acceptable treatments for concomitant meniscal injuries in patients with a chronic ACL injury.5,26,35,38 Cohen et al5 reported an increased incidence of arthrosis and poor function at long-term follow-up (10-15 years) after ACLR with meniscectomy. Singh et al38 revealed that ACL deficiency with concomitant meniscal injuries was not related to poor outcomes at short-term follow-up (3.5 years). A systematic review published in 2019 compared the outcomes after concurrent meniscectomy versus meniscal repair in ACLR.35 It revealed that the 2 groups had equivocal results at short-term follow-up (2 years), except for the Knee injury and Osteoarthritis Outcome Score, which favored meniscal resection over meniscal repair.35 The meniscal repair group had less anterior knee joint laxity but a higher reoperation rate.35 In the current review, 3 of the included studies reported the details of concurrent meniscal treatment.3,20,32 The older group had a total of 79 meniscal injuries, of which 38 were treated by meniscal repair and 41 by meniscectomy. The younger group had a total of 91 meniscal injuries, of which 61 were treated by meniscal repair and 30 by meniscectomy. Although the younger group had a higher incidence of meniscal repair procedures than did the older group, the 2 groups had comparable results in terms of clinical function and anterior knee laxity. Thus, we found that patients older than 50 years could still have satisfactory function after ACLR, regardless of the type of concurrent meniscal treatment.
Among the studies included in the current review, various types of tendon grafts were used: namely, the BPTB autograft and allograft,3 the doubled hamstring tendon autograft,17 and the quadrupled hamstring tendon autograft.20 According to previous studies,11,33,42 both the BPTB and GST grafts can lead to satisfactory clinical outcomes. However, considering the reduced donor site morbidity and potentially fewer problems encountered with the extensor mechanism in ACLR with hamstring tendon autograft or allograft, several authors have suggested these procedures in older patients with relatively low functional demands.1,19,24,28 Furthermore, despite a higher risk of graft failure, the use of allografts for primary ACLR is gaining popularity, given that the clinical outcomes are comparable between allografts and autografts.43 For patients aged ≥50 years, relatively lower physical demands do not push the inherent limitations of the allograft, and the benefit of reduced donor site discomfort could counteract the potential risks of disease transmission and later tissue integration. In this review, the graft failure rate was 0% in 3 of the included studies,3,17,20 and 1 graft failure was reported in the older group in the study by Osti et al.32 Moreover, based on the combined data in the current study, satisfactory outcomes, including in terms of clinical function and joint stability, were achieved with all types of tendon grafts including the BPTB autograft, BPTB allograft, 2-stranded hamstring tendon autograft, and 4-stranded hamstring tendon autograft, without a significant difference between the 2 study groups. Therefore, restoring joint stability might be of more importance than focusing on graft choice.
The evaluation of IKDC scores was conducted for both knee function and symptoms based on the level of sport participation and inconvenience in daily activities and psychological anxiety.2 We found that older patients could still obtain satisfactory functional scores, considering that they may have lower expectations in terms of daily activities or choose a less demanding sport for their knees as compensation. In this review, although the combined results indicated that the older group had slightly inferior IKDC scores than the younger group at the end of follow-up, only 1 of the included studies reported that the difference reached a significant level.20 Overall, the improvement was not significantly different between these 2 groups. That is, patients older than 50 years still had knee functional improvements postoperatively, similarly to younger patients. Therefore, in the absence of pre-existing physical contraindications, ACLR is an option for patients in their 50s who wish to improve their quality of life and regain the level of physical activity they had before the injury.3
Heterogeneity
Various factors might have led to the level of heterogeneity observed among the studies analyzed in this review. First, the concomitant knee status, including ligament and cartilage status, varied considerably among the 4 studies. Second, the surgical procedures were not identical across the studies. Therefore, surgical factors such as opioid dosage and surgeon experience might have contributed to heterogeneity.
Strengths and Limitations
This study has several strengths. First, it is the first systematic review and meta-analysis to compare the outcomes after ACLR between patients older than 50 years and younger patients. Second, we searched the 3 largest and most comprehensive databases for relevant studies. Third, the GRADE approach was used to evaluate the strength of the evidence for each outcome.
There are several limitations in this systematic review. First, all included studies followed a retrospective design, which implies inherent limitations of methodological quality. Second, as previously mentioned, the variation in numerous factors, including surgical and clinical factors, might have increased the heterogeneity. The number of variables limits the generalizability of our findings. Third, this review did not include studies with a control group of nonoperatively managed patients. Therefore, we could not comment on this issue, considering that nonoperative treatment still plays a role in older patients without high functional demands. Fourth, all included studies only reported the short-term to midterm outcomes after ACLR. We do not know whether surgery changed the long-term outcomes, for example, in terms of knee arthrosis. Fifth, because of their low incidence in all included studies, we are uncertain if there is a difference in terms of complications between the 2 groups.
Conclusion
The current evidence demonstrates that patients older than 50 years had comparable outcomes after arthroscopic ACLR with those of patients younger than 50 years. In the absence of contraindications, patients older than 50 years should consider undergoing ACLR to regain daily activity function and improve their quality of life. This study offers orthopaedic surgeons a reference when making decisions on the treatment of ACL insufficiency in patients older than 50 years.
APPENDIX
Database Search Strategy
Cochrane Central Register of Controlled Trials Search Strategy (April 30, 2019)
MeSH descriptor: [Anterior Cruciate Ligament] this term only (647)
MeSH descriptor: [Anterior Cruciate Ligament Reconstruction] this term only (316)
((anterior near/2 cruciate* near/2 ligament*) or ACL): ti, ab, kw (Word variations have been searched) (2598)
#1 or #2 or #3 (2598)
(ag* or yea* or old or older): ti, ab, kw (865306)
(50 or fifty or fifties): ti, ab, tw (194117)
#4 and #5 and #6 [trial] (232)
MEDLINE Search Strategy (April 30, 2019)
exp Anterior Cruciate Ligament/ (10306)
exp Anterior Cruciate Ligament Reconstruction/ (4028)
((anterior adj2 cruciate$ adj2 ligament$) or ACL).tw. (20909)
or/1-3 (22482)
(ag* or yea* or old* or old).tw. (7523786)
(50 or 50 s or fifty or fifties).tw. (1343941)
and/4-6 (1054)
Embase Search Strategy (April 30, 2019)
‘Anterior cruciate ligament’/exp
‘Anterior cruciate ligament reconstruction’/exp
‘Anterior cruciate ligament rupture’/exp
‘Anterior cruciate ligament injury’’/exp (2923)
(anterior NEAR/2 cruciate* NEAR/2 ligament*) or ACL): ab, ti (18924)
#1 or #2 or #3 or #4 or #5 (28847)
(age or aged or year or years or old* or old): ab, ti (6646188)
(50 or 50 s or fifty or fifties): ab, ti (2186718)
#6 and #7 and #8 (1569)
Footnotes
Final revision submitted November 17, 2019; accepted January 3, 2020.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Blyth MJ, Gosal HS, Peake WM, Bartlett RJ. Anterior cruciate ligament reconstruction in patients over the age of 50 years: 2- to 8-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2003;11(4):204–211. [DOI] [PubMed] [Google Scholar]
- 2. Chaory K, Poiraudeau S. Rating scores for ACL ligamentoplasty. Ann Readapt Med Phys. 2004;47(6):309–316. [DOI] [PubMed] [Google Scholar]
- 3. Cinque ME, Chahla J, Moatshe G, et al. Outcomes and complication rates after primary anterior cruciate ligament reconstruction are similar in younger and older patients. Orthop J Sports Med. 2017;5(10):2325967117729659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cinque ME, Dornan GJ, Chahla J, Moatshe G, LaPrade RF. High rates of osteoarthritis develop after anterior cruciate ligament surgery: an analysis of 4108 patients. Am J Sports Med. 2018;46(8):2011–2019. [DOI] [PubMed] [Google Scholar]
- 5. Cohen M, Amaro JT, Ejnisman B, et al. Anterior cruciate ligament reconstruction after 10 to 15 years: association between meniscectomy and osteoarthrosis. Arthroscopy. 2007;23(6):629–634. [DOI] [PubMed] [Google Scholar]
- 6. Dahm DL, Wulf CA, Dajani KA, Dobbs RE, Levy BA, Stuart MA. Reconstruction of the anterior cruciate ligament in patients over 50 years. J Bone Joint Surg Br. 2008;90(11):1446–1450. [DOI] [PubMed] [Google Scholar]
- 7. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. [DOI] [PubMed] [Google Scholar]
- 8. Filardo G, de Caro F, Andriolo L, Kon E, Zaffagnini S, Marcacci M. Do cartilage lesions affect the clinical outcome of anterior cruciate ligament reconstruction? A systematic review. Knee Surg Sports Traumatol Arthrosc. 2017;25(10):3061–3075. [DOI] [PubMed] [Google Scholar]
- 9. Fu FH, Bennett CH, Lattermann C, Ma CB. Current trends in anterior cruciate ligament reconstruction, part 1: biology and biomechanics of reconstruction. Am J Sports Med. 1999;27(6):821–830. [DOI] [PubMed] [Google Scholar]
- 10. GRADEpro GDT: GRADEpro Guideline Development Tool [software]. Hamilton, Canada: McMaster University (developed by Evidence Prime; ); 2015. [Google Scholar]
- 11. Gupta R, Sood M, Malhotra A, et al. Low re-rupture rate with BPTB autograft and semitendinosus gracilis autograft with preserved insertions in ACL reconstruction surgery in sports persons. Knee Surg Sports Traumatol Arthrosc. 2018;26(8):2381–2388. [DOI] [PubMed] [Google Scholar]
- 12. Higgins JP, Altman DG, G, øtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomized trials. BMJ. 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Higgins JP, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 (updated March 2011) London: The Cochrane Collaboration; 2011. Available at: http://handbook.cochrane.org. Accessed December 15, 2018. [Google Scholar]
- 14. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. [DOI] [PubMed] [Google Scholar]
- 15. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Iorio R, Iannotti F, Ponzo A, et al. Anterior cruciate ligament reconstruction in patients older than fifty years: a comparison with a younger age group. Int Orthop. 2018;42(5):1043–1049. [DOI] [PubMed] [Google Scholar]
- 18. Kay J, Memon M, Shah A, et al. Earlier anterior cruciate ligament reconstruction is associated with a decreased risk of medial meniscal and articular cartilage damage in children and adolescents: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2018;26(12):3738–3753. [DOI] [PubMed] [Google Scholar]
- 19. Khan RM, Prasad V, Gangone R, Kinmont JC. Anterior cruciate ligament reconstruction in patients over 40 years using hamstring autograft. Knee Surg Sports Traumatol Arthrosc. 2010;18(1):68–72. [DOI] [PubMed] [Google Scholar]
- 20. Kim DK, Park G, Kuo LT, Park WH. Patients older than 50 years had similar results of knee strength and anteroposterior stability after ACL reconstruction compared to younger patients. Knee Surg Sports Traumatol Arthrosc. 2019;27(1):230–238. [DOI] [PubMed] [Google Scholar]
- 21. Kim KT, Kim HJ, Lee HI, et al. A comparison of results after anterior cruciate ligament reconstruction in over 40 and under 40 years of age: a meta-analysis. Knee Surg Relat Res. 2018;30(2):95–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lai CCH, Ardern CL, Feller JA, Webster KE. Eighty-three per cent of elite athletes return to preinjury sport after anterior cruciate ligament reconstruction: a systematic review with meta-analysis of return to sport rates, graft rupture rates and performance outcomes. Br J Sports Med. 2018;52(2):128–138. [DOI] [PubMed] [Google Scholar]
- 23. Mall NA, Frank RM, Saltzman BM, Cole BJ, Bach BR., Jr Results after anterior cruciate ligament reconstruction in patients older than 40 years: how do they compare with younger patients? A systematic review and comparison with younger populations. Sports Health. 2016;8(2):177–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Marquass B, Hepp P, Engel T, Dusing T, Lill H, Josten C. The use of hamstrings in anterior cruciate ligament reconstruction in patients over 40 years. Arch Orthop Trauma Surg. 2007;127(9):835–843. [DOI] [PubMed] [Google Scholar]
- 25. Mather RC III, Koenig L, Kocher MS, et al. Societal and economic impact of anterior cruciate ligament tears. J Bone Joint Surg Am. 2013;95(19):1751–1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mehl J, Otto A, Baldino JB, et al. The ACL-deficient knee and the prevalence of meniscus and cartilage lesions: a systematic review and meta-analysis (CRD42017076897). Arch Orthop Trauma Surg. 2019;139(6):819–841. [DOI] [PubMed] [Google Scholar]
- 27. Michalitsis S, Vlychou M, Malizos KN, Thriskos P, Hantes ME. Meniscal and articular cartilage lesions in the anterior cruciate ligament-deficient knee: correlation between time from injury and knee scores. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):232–239. [DOI] [PubMed] [Google Scholar]
- 28. Miller SL, Gladstone JN. Graft selection in anterior cruciate ligament reconstruction. Orthop Clin North Am. 2002;33(4):675–683. [DOI] [PubMed] [Google Scholar]
- 29. Mitchell M, Muftakhidinov B, Winchen T, et al. Engauge Digitizer Software. Available at: http://markummitchell.github.io/engauge-digitizer. Accessed December 11, 2018.
- 30. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Nwachukwu BU, Anthony SG, Lin KM, Wang T, Altchek DW, Allen AA. Return to play and performance after anterior cruciate ligament reconstruction in the National Basketball Association: surgeon case series and literature review. Phys Sportsmed. 2017;45(3):303–308. [DOI] [PubMed] [Google Scholar]
- 32. Osti L, Papalia R, Del Buono A, Leonardi F, Denaro V, Maffulli N. Surgery for ACL deficiency in patients over 50. Knee Surg Sports Traumatol Arthrosc. 2011;19(3):412–417. [DOI] [PubMed] [Google Scholar]
- 33. Sajovic M, Stropnik D, Skaza K. Long-term comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: a 17-year follow-up of a randomized controlled trial. Am J Sports Med. 2018;46(8):1800–1808. [DOI] [PubMed] [Google Scholar]
- 34. Sanders TL, Maradit Kremers H, Bryan AJ, et al. Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. Am J Sports Med. 2016;44(6):1502–1507. [DOI] [PubMed] [Google Scholar]
- 35. Sarraj M, Coughlin RP, Solow M, et al. Anterior cruciate ligament reconstruction with concomitant meniscal surgery: a systematic review and meta-analysis of outcomes. Knee Surg Sports Traumatol Arthrosc. 2019;27(11):3441–3452. [DOI] [PubMed] [Google Scholar]
- 36. Schünemann H, Brożek J, Guyatt G, Oxman A, eds. GRADE Handbook for Grading Quality of Evidence and Strength of Recommendations. Updated October 2013 Hamilton: GRADE Working Group; 2013. Available at: guidelinedevelopment.org/handbook. Accessed December 15, 2018. [Google Scholar]
- 37. Seng K, Appleby D, Lubowitz JH. Operative versus nonoperative treatment of anterior cruciate ligament rupture in patients aged 40 years or older: an expected-value decision analysis. Arthroscopy. 2008;24(8):914–920. [DOI] [PubMed] [Google Scholar]
- 38. Singh A, Wei DT, Lin CTP, et al. Concomitant meniscal injury in anterior cruciate ligament reconstruction does not lead to poorer short-term post-operative outcomes. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1266–1272. [DOI] [PubMed] [Google Scholar]
- 39. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological Index for Non-randomized Studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. [DOI] [PubMed] [Google Scholar]
- 40. Sommerfeldt M, Raheem A, Whittaker J, Hui C, Otto D. Recurrent instability episodes and meniscal or cartilage damage after anterior cruciate ligament injury: a systematic review. Orthop J Sports Med. 2018;6(7):2325967118786507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Toanen C, Demey G, Ntagiopoulos PG, Ferrua P, Dejour D. Is there any benefit in anterior cruciate ligament reconstruction in patients older than 60 years? Am J Sports Med. 2017;45(4):832–837. [DOI] [PubMed] [Google Scholar]
- 42. Wada O, Gamada K, Aoyama N, Mizuno K, Iwasaki Y. A difference in rotational alignment of the tibio-femoral joint after anterior cruciate ligament reconstruction between the bone-patellar tendon-bone and semitendinosus-gracilis grafts. Clin Biomech (Bristol, Avon). 2019;65:45–50. [DOI] [PubMed] [Google Scholar]
- 43. Zeng C, Gao SG, Li H, et al. Autograft versus allograft in anterior cruciate ligament reconstruction: a meta-analysis of randomized controlled trials and systematic review of overlapping systematic reviews. Arthroscopy. 2016;32(1):153–163. [DOI] [PubMed] [Google Scholar]