Abstract
Background:
Satisfactory outcomes have been reported after all-inside meniscus ramp repair with combined anterior cruciate ligament reconstruction (ACLR). However, clinical outcomes after ACLR with inside-out meniscus ramp repair are limited.
Purpose/Hypothesis:
The purpose of this study was to evaluate patient-reported outcomes for patients who underwent ACLR and medial meniscus ramp repair compared with those who underwent isolated ACLR; patients in the 2 groups were matched for age, sex, and sport/activity. The null hypothesis was that there would be no significant differences in clinical outcomes between groups at a minimum of 2 years postoperatively.
Study Design:
Cohort study; Level of evidence 3.
Methods:
Patients who underwent primary ACLR with bone–patellar tendon–bone (BPTB) autograft by a single surgeon were retrospectively identified. A subgroup of patients with combined ACLR and meniscus ramp repair with a minimum 2-year postoperative follow-up were matched to a cohort who underwent isolated ACLR. Subjective patient-reported questionnaires, knee stability, and return to level of activity/sport were collected.
Results:
There were 851 patients who underwent primary ACLR; of these, 158 (18.6%) had medial meniscus ramp lesions confirmed at arthroscopy. The most common clinical characteristics in patients with ramp lesions were chronic injuries (68.4%), contact mechanism (88%), concomitant lateral meniscus tears (63.2%), and concomitant lateral meniscus posterior root tears (22.2%). Further, 50 patients who underwent combined ACLR and meniscus ramp repair with minimum 2-year follow-up were matched to patients who underwent isolated ACLR. Both groups reported significant improvements in subjective outcomes from preoperative to postoperative assessments (P < .001). No significant differences were found in postoperative outcomes for combined ACLR with ramp repair versus isolated ACLR (P > .05). Patients with meniscus ramp repair had increased preoperative knee laxity demonstrated by grade 3 Lachman (44% vs 6%) and pivot-shift (38% vs 12%) test results compared with patients who underwent isolated ACLR (P ≤ .005 for both).
Conclusion:
This study demonstrates similar clinical outcomes, knee stability on postoperative physical examination, and return-to-sport rates for patients who underwent combined ACLR with BPTB autograft and inside-out meniscus ramp repair versus a matched cohort who underwent isolated ACLR. Clinicians should have a high index of suspicion for the presence of ramp lesions in patients with ACL tears who have a contact mechanism of injury, grade 3 Lachman test result, and concomitant lateral meniscal abnormality.
Keywords: meniscal repair, ACL, ACLR, surgical outcomes, return to sport
Meniscus ramp lesions have become increasingly recognized throughout the orthopaedic surgery literature. Ramp lesions are characterized as a continuum of tears located along the posteromedial meniscocapsular junction and/or meniscotibial attachment of the posterior horn of the medial meniscus, associated with anterior cruciate ligament (ACL) tears.6,7,23,24 The collective awareness of such injuries has led to improved diagnostic strategies,3,21 knowledge of tear incidence at the time of ACL reconstruction (ACLR),1,13 and reported risk factors for increased risk of meniscus ramp tear.18,22
Despite this improved awareness, there is a paucity of literature reporting on the results of surgical treatment. Similar results have been reported between surgical repair and nonoperative treatment after stable meniscus ramp tears left in situ at the time of ACLR.14 In contrast, successful outcomes have been reported at a minimum of 2 years postoperatively in patients who underwent concomitant ACLR and medial meniscus ramp repair via an all-inside technique.25 Because the controversy regarding different treatment strategies remains unresolved, comparing a cohort of patients who undergo combined ACLR and repair for unstable medial meniscus ramp tears with patients who undergo isolated ACLR may provide insight for clinicians. Therefore, the purpose of this study was to evaluate patient-reported outcomes in patients who underwent ACLR and medial meniscus ramp repair compared with a matched cohort who underwent isolated ACLR. The null hypothesis was that no significant differences in outcomes would be found between the patient groups at a minimum of 2 years postoperatively.
Methods
Study Design
This study was approved and deemed exempt from review by Vail Health Hospital. Demographic data and clinical outcome scores were collected on all patients who underwent primary ACLR performed by a single board-certified orthopaedic surgeon (R.F.L.) from April 2010 to January 2017. Inclusion criteria included patients who underwent primary ACLR with bone–patellar tendon–bone (BPTB) autograft combined with repair for an unstable medial meniscus ramp lesion and minimum follow-up period of 2 years. These patients were matched according to age, sex, and sport/activity with patients who underwent primary isolated ACLR. Patients were first matched according to sex, followed by age within 12 months. Next, patient charts were reviewed to determine what the patients self-reported as their main sport of participation, including the sport/activity they were participating in during their ACL tear. Because of the retrospective study design and relatively low sample size, matching according to competition level of sport was not possible.
Study exclusion criteria included patients who had undergone multiligament knee reconstruction or previous meniscal surgery, or who displayed any of the following: concomitant lateral meniscal tears, meniscus root tears, meniscal radial tears, concomitant cartilage procedures, concomitant osteotomy procedures, concomitant fractures, bilateral ACLR, revision ACLR, and ACLR with allograft or hamstring tendon.
Surgical Technique
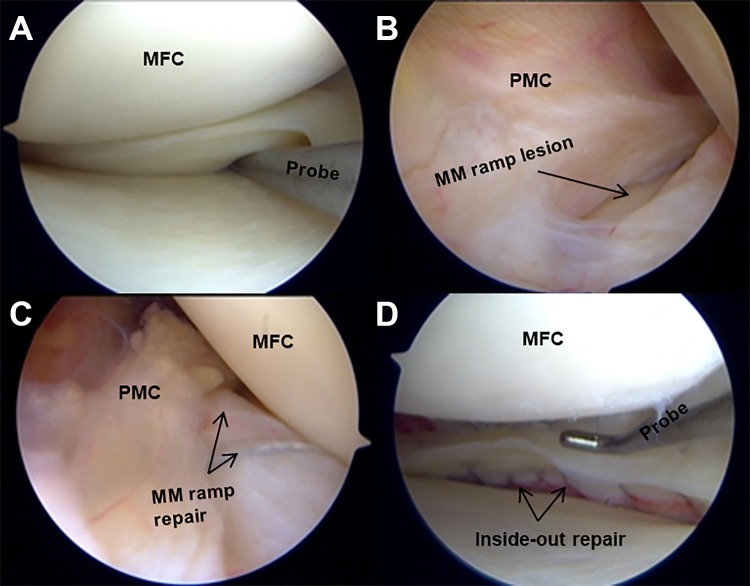
All included patients underwent anatomic, single-bundle, primary ACLR with BPTB autograft according to a previously described and biomechanically validated technique.2,12,27 All of the included patients with unstable meniscus ramp lesions underwent inside-out meniscal repair according to a previously described and biomechanically validated technique.4,6 Sutures were passed through an arthroscopic cannula in a vertical-mattress fashion and tied to the posterior horn of the medial meniscus under direct arthroscopic visualization. We used a systematic approach for the identification and classification of meniscus ramp tears according to a previous study.5 The main subjective grading criteria that were used to constitute a meniscus ramp lesion were (1) extent of the meniscus ramp tear (partial vs full thickness) and (2) meniscal stability upon probing. The size of the tear (eg, ≥2.5 cm) was not a direct indication or contraindication for decision making regarding meniscus ramp repair versus no repair.7 A repairable meniscus ramp lesion was considered a complete tear, located within the meniscocapsular and/or meniscotibial attachment of the posterior horn of the medial meniscus, that was unstable on probing. We evaluated ramp lesions using a modified Gillquist view by placing the arthroscope through the intercondylar notch medial to the posterior cruciate ligament and using a probe above the medial meniscus to push against the posteromedial capsular attachment (Figure 1).
Figure 1.
Arthroscopic images of medial meniscus ramp repair using an inside-out vertical mattress technique. (A) Medial meniscal instability when viewed anteriorly as depicted by increased anterior meniscal translation upon probing. (B) Modified Gillquist view showing complete disruption at the meniscocapsular junction, followed by (C) reapproximation of the meniscocapsular attachment during suture placement through meniscus and posteromedial capsule. (D) Completed inside-out meniscus ramp repair illustrating stability and double-row vertical mattress suture placement. MFC, medial femoral condyle; MM, medial meniscus; PMC, posteromedial capsule.
Postoperative Rehabilitation Protocol
The postoperative rehabilitation protocol was identical for patients who underwent combined ACLR with meniscus ramp repair and those who underwent isolated ACLR. All patients were allowed to bear weight as tolerated upon discharge and were instructed to use crutches until they could ambulate without a limp. Physical therapy commenced within 24 hours after surgery to initiate early range of motion (ROM) and muscle reactivation and to control edema. Rehabilitation included straight-leg raises in an immobilizer until there was no extension lag, at which point patients were transitioned to a functional hinge knee brace (CTi; Ossur Americas). Patients were allowed to begin straight-ahead running exercises at 4 months, with restrictions on pivoting and twisting. Gradual return to play progression was initiated at 6 months after the successful completion of a functional sports test. Return to sports or activity was allowed when the patient achieved normal strength, stability, and knee ROM comparable with the contralateral side, at around 7 to 9 months postoperatively.
Clinical and Patient-Reported Outcomes, Patient Demographics, and Complications/Failures
At a minimum of 2 years after the index surgery, patients were administered an electronic subjective questionnaire that included the following clinical outcome measures: Lysholm knee activity scale, Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), 12-Item Short Form Health Survey (SF-12) physical component summary (PCS), Tegner activity scale, International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, and patient satisfaction with outcome. Patient satisfaction was measured on a 1 to 10 scale, with 10 being very satisfied and 1 being very unsatisfied. Demographic characteristics were recorded and included age, sex, body mass index (BMI), and sport/activity at the time of ACL injury. Data regarding knee ROM and stability on physical examination (Lachman and pivot-shift tests) were collected by a single examiner (R.F.L.) both preoperatively and at a minimum of 2 years postoperatively. Additionally, level of return to sport and preinjury activity level were collected; return to sport was classified as “lower than preinjury level,” “same level as preinjury level,” or “above preinjury level.” Meniscal repair failure was defined as a requirement for any subsequent surgery that required revision meniscal repair or partial meniscectomy of the previous meniscus ramp repair (eg, retear). Complications were recorded, including reintervention surgery requiring partial meniscectomy within a new area of the medial meniscus (eg, secondary tear), ACLR graft failure (ipsilateral and contralateral), deep vein thrombosis, or arthrofibrosis requiring a lysis of adhesions.
Statistical Analysis
For outcome variables comparing preoperative and postoperative scores, a paired t test was used. Because ceiling or floor effects are common in the outcome scales we assessed, we used nonparametric, rank-based statistical methods for group comparisons of postoperative patient-reported outcomes. Specifically, because each patient who underwent ACLR with ramp repair was matched to a patient who underwent isolated ACLR, the Wilcoxon signed-rank test was used for these postoperative group comparisons. Independent t tests were used to compare age and BMI between groups. Chi-square tests and Fisher exact tests were used to compare categorical data including sex, chronicity (acute, <6 weeks from time of injury; chronic, ≥6 weeks from time of injury), knee stability on physical examination, complication rate, and return to preinjury level of activity. All P values were 2-tailed, and an alpha level of less than .05 was considered significant. Unless otherwise noted, medians are reported with first and third quartiles in brackets, and means are reported with ±SDs. All statistical analyses were performed by use of SPSS version 9.4.
Statistical power was considered for the primary study hypothesis in terms of detectable effect size given the planned analysis and the fixed effect size. Assuming a 2-tailed, nonparametric comparison of central tendency of patient-reported outcomes between groups and an alpha level of .05, we determined that 50 patients per group would be sufficient to detect an effect size of d = 0.58 with 80% statistical power. Thus, standardized group mean differences smaller than 0.58 cannot be ruled out by statistically nonsignificant hypothesis tests within this study.
Results
Patient Demographics and Clinical Characteristics
We identified 1176 patients who underwent ACLR during the study period; 851 (72.4%) of these had primary ACLR and 325 (27.6%) had revision ACLR. Of the 851 patients who had primary ACLR, 158 (18.6%) had medial meniscus ramp lesions confirmed at arthroscopy; 84 (53.2%) were male and 74 (46.8%) were female. There were 108 (68.4%) patients with chronic injuries (≥6 weeks from time of injury) and 50 (31.6%) patients with acute injuries (<6 weeks from time of injury). The majority of patients with ramp lesions reported a contact mechanism (n = 139; 88%) at the time of injury compared with a noncontact mechanism (n = 19; 12%). Further, 62% (n = 98) had an isolated ACL injury with a meniscus ramp lesion, whereas 38% (n = 60) had an additional ligamentous knee injury. A concomitant lateral meniscal tear was identified in 100 (63.3%) patients with a ramp lesion, and a concomitant lateral meniscus posterior root tear was identified in 35 (22.2%) patients.
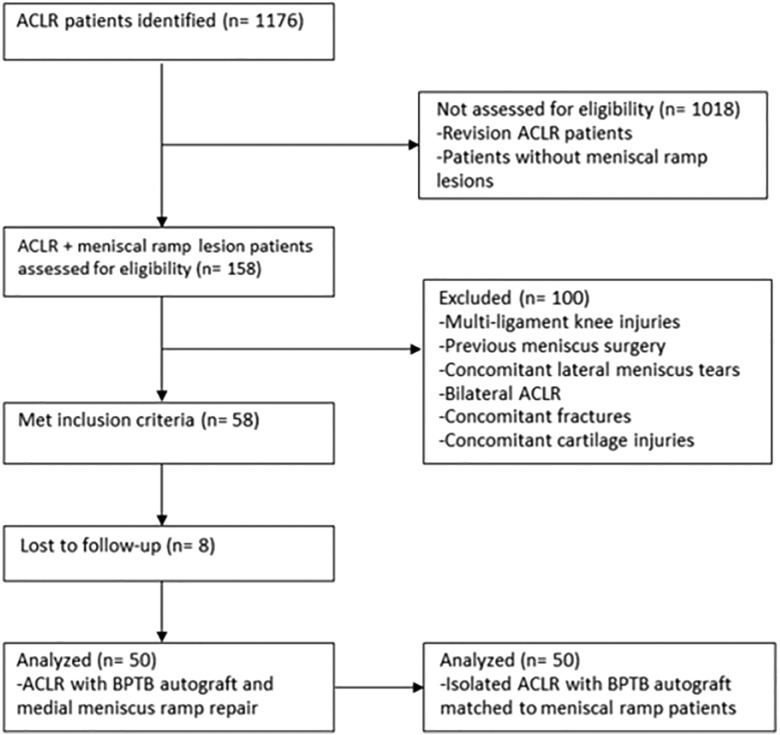
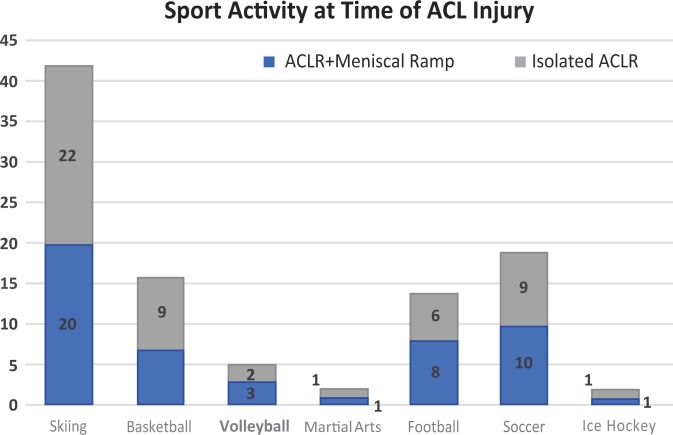
A total of 58 patients met the inclusion criteria for ACLR with combined inside-out repair of unstable medial meniscus ramp lesion. Of these, 50 patients had adequate follow-up during the data collection period, and 8 patients were lost to follow-up (86% retention rate). These patients were evaluated for clinical outcomes and matched to a control group of patients who underwent isolated ACLR (Figure 2). The average follow-up was 2.8 years (range, 2.0-8.0 years). No significant differences were noted in age (P = .667), sex (P ≥. 999), BMI (P = .261), or chronicity of injury (P = .529) between patients in the combined repair group versus control group (Table 1 and Figure 3).
Figure 2.
Flow diagram of patient inclusion according to Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.26 Patients with combined anterior cruciate ligament reconstruction (ACLR) and medial meniscus ramp repair were matched in a 1-to-1 allocation, according to age, sex, and activity level, with patients who underwent primary isolated ACLR. BPTP, bone–patellar tendon–bone.
Table 1.
Demographics for the 2 Groups of Patients: Combined ACLR and Meniscus Ramp Repair (n = 50) and Isolated ACLR (n = 50)a
| Total | Male | Female | |
|---|---|---|---|
| Combined ACLR and meniscus ramp repair | |||
| Patients | 50 | 22 | 28 |
| Age, y | 30.5 ± 11.4 | 31.7 ± 11.8 | 29.5 ± 11.2 |
| BMI | 23.4 ± 2.5 | 25.2 ± 2.6 | 22.5 ± 2.7 |
| Acute injuriesb | 31 | ||
| Chronic injuries | 19 | ||
| Isolated ACLR | |||
| Patients | 50 | 22 | 28 |
| Age, y | 31.4 ± 10.3 | 32.6 ± 10.8 | 28.8 ± 9.3 |
| BMI | 24.2 ± 3.4 | 24.0 ± 3.8 | 23.0 ± 2.8 |
| Acute injuries | 34 | ||
| Chronic injuries | 16 | ||
aValues are reported as number or mean ± SD. ACLR, anterior cruciate ligament reconstruction; BMI, body mass index.
bAcute injuries were considered to occur <6 weeks from the time of injury to surgery, and chronic injuries were considered to occur ≥6 weeks from the time of injury to surgery.
Figure 3.
Sport activity reported at the time of anterior cruciate ligament (ACL) tear in patients with combined ACL reconstruction (ACLR) and medial meniscus ramp repair (n = 50) versus those with isolated ACLR (n = 50).
Patient-Reported Outcomes
The median [first quartile, third quartile] outcome scores significantly improved from preoperative to postoperative assessments for SF-12 (38 [32, 46] to 57 [51, 59]), WOMAC Pain (5 [3, 10] to 0 [0, 1]), WOMAC Stiffness (4 [2, 4] to 1 [0, 2]), WOMAC total (28 [17, 52] to 0 [0, 8]), Lysholm (53 [31, 69] to 86 [80, 95]), Tegner (2 [1, 3] to 8 [6, 9]), and IKDC (66 [62, 72] to 78 [72, 80]) after combined ACLR with meniscus ramp repair (P < .001 for all). Similarly, in isolated ACLR, the median outcome scores significantly improved from preoperative to postoperative assessments for SF-12 PCS (38 [31, 44] to 57 [54, 58]), WOMAC Pain (5 [4, 9] to 0 [0, 2]), WOMAC Stiffness (3 [2, 5] to 0 [0, 2]), WOMAC total (32 [22, 50] to 2 [0, 7]), Lysholm (53 [37, 66] to 85 [80, 94]), Tegner (2 [1, 3] to 7 [6, 8]), and IKDC (65 [55, 69] to 77 [72, 84]) (P < .001 for all). At final follow-up, no significant differences in postoperative subjective outcomes were seen between patients who underwent combined ACLR with meniscus ramp repair and those who underwent isolated ACLR (P > .05 for all) (Table 2).
Table 2.
Patient-Reported Subjective Outcomes Between Patients With Isolated ACLR and Patients With Combined ACLR and Meniscus Ramp Repaira
| Outcome | Isolated ACLR | Combined ACLR and Meniscus Ramp Repair | P Value |
|---|---|---|---|
| SF-12 PCS | 57 [54, 58] | 57 [51, 59] | .330 |
| WOMAC Pain | 0 [0, 2] | 0 [0, 1] | .969 |
| WOMAC Stiffness | 0 [0, 2] | 1 [0, 2] | .903 |
| WOMAC Total | 2 [0, 7] | 0 [0, 8] | .427 |
| Lysholm | 85 [80, 94] | 86 [80, 95] | .842 |
| Tegner | 7 [6, 8] | 8 [6, 9] | .417 |
| IKDC | 77 [72, 84] | 78 [72, 80] | .200 |
| Satisfaction | 9 [8, 10] | 9 [8, 10] | .908 |
aValues are reported as median [first quartile, third quartile]. ACLR, anterior cruciate ligament reconstruction; IKDC, International Knee Documentation Committee questionnaire; SF-12 PCS, 12-item Short Form Health Survey Physical Component Summary; WOMAC, Western Ontario and McMaster Universities Arthritis Index. No significant differences were reported at a mean of 2.8 years postoperatively (P > .05).
Clinical Outcomes and Return to Sport
The mean (±SD) preoperative ROM of the injured knee was –2.2° ± 1.6° of extension to 136.6° ± 2.9° of flexion for ACLR with ramp repair and –2.7° ± 1.8° of extension to 136.1° ± 2.1° of flexion for isolated ACLR (negative degrees indicate hyperextension). The mean postoperative ROM was –1.0° ± 2.8° of extension to 135.2° ± 5.7° of flexion for ACLR with ramp repair and –1.2° ± 1.2° of extension to 135.6° ± 1.9° for isolated ACLR. Patients with meniscus ramp repair had evidence of increased knee laxity preoperatively as demonstrated by grade 3 Lachman (44% vs 6%) and pivot-shift (38% vs 12%) tests compared with patients who had isolated ACLR (P ≤ .005 for both) (Table 3). Patients in both groups demonstrated improved anterior knee stability from preoperative to postoperative status, as reported by grading of the Lachman and pivot-shift tests (Table 3). The majority of patients in the ACLR with ramp repair group (84%) and the isolated ACLR group (90%) returned to the same preinjury level of activity. No significant differences were noted in return to level of activity/sport between patients who underwent ACLR with meniscus ramp repair and those who underwent isolated ACLR (P = .658) (Table 4).
Table 3.
Anterior Knee Stability in Patients With Isolated ACLR and Patients With Combined ACLR and Meniscus Ramp Repaira
| Examination Test | Isolated ACLR | Combined ACLR and Meniscus Ramp Repair | P Value |
|---|---|---|---|
| Lachman Preoperative | |||
| Grade 1 | 1 (2) | 0 (0) | |
| Grade 2 | 46 (92) | 28 (56) | |
| Grade 3 | 3 (6) | 22 (44) | <.001b |
| Postoperative | |||
| Grade 0 | 44 (88) | 45 (90) | .749 |
| Grade 1 | 6 (12) | 5 (10) | |
| Pivot shift Preoperative | |||
| Grade 1 | 2 (4) | 0 (0) | |
| Grade 2 | 42 (84) | 31 (62) | |
| Grade 3 | 6 (12) | 19 (38) | .005b |
| Postoperative | |||
| Grade 0 | 50 (100) | 50 (100) | ≥.999 |
aResults are reported as total number (%). Statistical differences in categorical data between preoperative and postoperative frequencies were computed via a chi-square test. ACLR, anterior cruciate ligament reconstruction.
bStatistically significant at P < .05.
Table 4.
Level of Return to Activity or Sport for Patients With Isolated ACLR and Patients With Combined ACLR and Meniscus Ramp Repaira
| Level of Return to Activity/Sport | Isolated ACLR | Combined ACLR and Meniscus Ramp Repair |
|---|---|---|
| Lower level | 4 (8) | 6 (12) |
| Same level | 45 (90) | 42 (84) |
| Higher level | 1 (2) | 2 (4) |
aResults are reported as total number (%). Return to sport was characterized according to subjectively reported values and measured as a comparison with preinjury activity or sport level. ACLR, anterior cruciate ligament reconstruction.
Complications/Failures
There were 6 reported complications in the ACLR with ramp repair group (12%) and 4 reported complications in the isolated ACLR group (8%), with no significant difference between frequency of complications (P = .505). One patient had a failed inside-out meniscus ramp repair (2%) and underwent a revision medial meniscus ramp repair at 12 months postoperatively from the index surgery. One patient had a partial retear of the meniscus ramp repair and underwent subsequent partial medial meniscectomy (2%). There were no ACLR graft failures in either group at a mean 2.8 years postoperatively; 1 patient (2%) in the isolated ACLR group reported a contralateral ACL tear. Table 5 details the complications in both groups.
TABLE 5.
Complications and Reintervention Surgeries for Patients With Isolated ACLR and Patients With Combined ACLR and Meniscus Ramp Repaira
| Complication | Reintervention | |
|---|---|---|
| Isolated ACLR (4 complications) | ||
| 1 | Arthrofibrosis | Lysis of adhesions |
| 2 | Painful hardware | Deep hardware removal |
| 3 | Contralateral ACL tear | ACLR |
| 4 | Acute injury | Osteochondral allograft transplant |
| Combined ACLR and meniscus ramp repair (6 complications) | ||
| 1 | Cyclops lesion | Debridement of cyclops lesion |
| 2 | Partial retear of medial meniscal repair | Partial medial meniscectomy |
| 3 | Acute injury | ORIF patellar fracture |
| 4 | Arthrofibrosis | Lysis of adhesions |
| 5 | Acute injury | Lateral collateral ligament reconstruction |
| 6 | Arthrofibrosis | Lysis of adhesions |
aACLR, anterior cruciate ligament reconstruction; ORIF, open reduction internal fixation.
Discussion
The main finding of this study was there were no significant differences between patients who underwent combined ACLR with a meniscus ramp repair compared with a matched cohort of patients who underwent isolated ACLR. The incidence of meniscus ramp lesions in all patients who had ACL tear was 18.6% confirmed at the time of arthroscopy. The most common clinical characteristics identified in patients with ramp lesions were chronic injuries, contact mechanism of injury, concomitant lateral meniscal tear, and concomitant lateral meniscus posterior root tear.
Patients who underwent ACLR with BPTB autograft and inside-out meniscus ramp repair for unstable medial meniscus ramp tears reported improved subjective outcomes and knee stability on physical examination, and 88% returned to activity/sport at the same or higher level compared with preoperatively. In a randomized control, Liu et al14 reported similar subjective outcomes and knee stability for patients who underwent all-inside meniscal repair versus those who underwent trephination without repair for stable meniscus ramp lesions at a minimum of 2 years postoperatively (P > .05). Additionally, no significant differences regarding the healing status of meniscus ramp lesions were seen between the 2 groups on follow-up MRI scan (P = .543). Because of the potential for stable ramp lesions to heal without repair, these authors recommended conservative treatment for stable ramp lesions at the time of ACLR.14 Recently, Sonnery-Cottet et al22 reported an 11% rate of meniscectomy at a mean 45.6 months after all-inside meniscus ramp repair. In the current study, the rate of meniscectomy was 2% at a mean 33.6 months after inside-out ramp repair. Therefore, we recommend inside-out repair of all unstable meniscus ramp lesions at the time of ACLR.
In our study, the majority of patients with ACL tears and concomitant meniscus ramp lesions reported chronic injuries (n = 108; 68.4%) and a contact mechanism at time of injury (n = 139; 88%) and were male (n = 84; 53.2%). The most common associated pathologic conditions were concomitant lateral meniscal tears (n = 100; 63.3%) and concomitant lateral meniscus posterior root tears (n = 35; 22.2%). Identification of preoperative risk factors for potential ramp lesions can allow for increased awareness and improved diagnosis at the time of ACLR. Trends in patient characteristics have been previously reported with arthroscopically confirmed meniscus ramp lesions. Specifically, male sex, younger age (<30 years), a concomitant lateral meniscal tear, contact injury mechanism, increased medial meniscal slope, revision ACLR, and chronic injuries have been significantly associated with the presence of meniscus ramp lesions.8,13,18,20,22 The current study further supports these previously identified clinical characteristics of patients with meniscus ramp lesions, with an additional finding of a 22% incidence for concomitant lateral meniscus posterior root tears. This finding may help explain the increased amount of knee instability during the pivot-shift maneuver that has been previously described in biomechanical models.10,11
Meniscal deficiency has been reported as the most significant factor to predict graft failure after ACLR.16 The posterior horn of the medial meniscus is a known secondary stabilizer to anterior tibial translation and thus may help stabilize the ACL-deficient knee.15,19 In contrast, when the ACL is torn in combination with a meniscus ramp lesion, anterior knee translation may increase.6 This finding was described by Sonnery-Cottet et al,22 who reported a preoperative side-to-side laxity difference in anterior knee translation of more than 6 mm. Our results corroborate this finding, as 44% of patients with ACL tears and meniscus ramp lesions demonstrated grade 3 Lachman test result compared with 6% of patients who had isolated ACL tear (P < .001). Therefore, when grade 3 anterior knee instability is noted on physical examination, clinicians should include a posterior horn medial meniscal tear in their differential diagnosis of associated secondary pathologic condition. Despite the known preoperative increase in instability findings, stability on physical examination improved in all patients, and no significant differences were found in clinical knee laxity grading between groups at final follow-up.
Results of the current study demonstrate that inside-out meniscus ramp repair for unstable ramp lesions with concomitant ACLR led to equivalent clinical outcomes to isolated ACLR at a minimum of 2 years postoperatively. Recent biomechanical data suggest that these lesions may result in increased anterior tibial displacement and increased strain on both the native ACL and the ACL reconstructed graft.9,17,23 In the current study, no significant differences were seen in rate of complications between groups (12% ACLR with ramp repair vs 8% isolated ACLR; P = .505). Additionally, the rate of meniscus ramp repair failure after inside-out meniscal repair was 2%, which is lower than previous reports of 11% after all-inside ramp repair.22 Therefore, we recommend inside-out ramp repair at the time of ACLR because of the potential increased knee kinematics associated with ramp tears in ACL-reconstructed knees and equivalence compared with isolated ACLR.6,9
There were some inherent limitations of this study. We reported clinical outcomes for a single surgeon’s patients, who were subject to the same ACLR and meniscus ramp repair technique; thus, our results may not be generalizable. However, this consistency allowed for direct comparisons between patients by use of a 1-to-1 matching study design. There is the inherent possibility of bias with outcomes reported from a single surgeon. However, use of the same ACLR technique offered homogeneity, which allowed for matched comparisons. Additionally, the use of instrumented laxity testing would have offered a more objective assessment of knee stability, but this was not possible because of the retrospective design of this study. Last, we did not evaluate healing rates via second-look arthroscopy, and thus clinical outcomes cannot infer biological healing.
Conclusion
This study demonstrates similar clinical outcomes, postoperative physical examination knee stability, and return-to-sport rates for combined ACLR with BPTB autograft and inside-out meniscus ramp repair compared with isolated ACLR in a matched cohort. Clinicians should have a high index of suspicion for the presence of ramp lesions in patients with ACL tears who report a contact mechanism of injury, grade 3 Lachman test result, and concomitant lateral meniscal abnormality.
Footnotes
Final revision submitted December 16, 2019; accepted December 23, 2019.
One or more of the authors has declared the following potential conflict of interest or source of funding: T.J.D. has received educational support from Smith & Nephew. L.E. has received research support from Arthrex, Biomet, Health Southeast Norway, and Smith & Nephew and royalties from Arthrex and Smith & Nephew, and he has stock/stock options in iBalance. R.F.L. has received educational support from Arthrex, consulting fees from Arthrex and Smith & Nephew, speaking fees from Smith & Nephew, and royalties from Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was waived by Vail Health Hospital Institutional Review Board (protocol No. 2018-59).
References
- 1. Bollen SR. Posteromedial meniscocapsular injury associated with rupture of the anterior cruciate ligament: a previously unrecognised association. J Bone Joint Surg Br. 2010;92(2):222–223. [DOI] [PubMed] [Google Scholar]
- 2. Chahla J, Moatshe G, Cinque ME, Godin J, Mannava S, LaPrade RF. Arthroscopic anatomic single-bundle anterior cruciate ligament reconstruction using bone-patellar tendon-bone autograft: pearls for an accurate reconstruction. Arthrosc Tech. 2017;6(4):e1159–e1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. DePhillipo NN, Cinque ME, Chahla J, Geeslin AG, Engebretsen L, LaPrade RF. Incidence and detection of meniscal ramp lesions on magnetic resonance imaging in patients with anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45(10):2233–2237. [DOI] [PubMed] [Google Scholar]
- 4. DePhillipo NN, Cinque ME, Kennedy NI, et al. Inside-out repair of meniscal ramp lesions. Arthrosc Tech. 2017;6(4):e1315–e1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. DePhillipo NN, Engebretsen L, LaPrade RF. Current trends among US surgeons in the identification, treatment, and time of repair for medial meniscal ramp lesions at the time of ACL surgery. Orthop J Sports Med. 2019;7(2):2325967119827267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. DePhillipo NN, Moatshe G, Brady A, et al. Effect of meniscocapsular and meniscotibial lesions in ACL-deficient and ACL-reconstructed knees: a biomechanical study. Am J Sports Med. 2018;46(10):2422–2431. [DOI] [PubMed] [Google Scholar]
- 7. DePhillipo NN, Moatshe G, Chahla J, et al. Quantitative and qualitative assessment of the posterior medial meniscus anatomy: defining meniscal ramp lesions. Am J Sports Med. 2019;47(2):372–378. [DOI] [PubMed] [Google Scholar]
- 8. Di Vico G, Di Donato SL, Balato G, et al. Correlation between time from injury to surgery and the prevalence of ramp and hidden lesions during anterior cruciate ligament reconstruction: a new diagnostic algorithm. Muscles Ligaments Tendons J. 2017;7(3):491–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Edgar C, Kumar N, Ware JK, et al. Incidence of posteromedial meniscocapsular separation and the biomechanical implications on the anterior cruciate ligament. J Am Acad Orthop Surg. 2019;27(4):e184–e192. [DOI] [PubMed] [Google Scholar]
- 10. Frank JM, Moatshe G, Brady AW, et al. Lateral meniscus posterior root and meniscofemoral ligaments as stabilizing structures in the ACL-deficient knee: a biomechanical study. Orthop J Sports Med. 2017;5(6):2325967117695756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Geeslin AG, Civitarese D, Turnbull TL, Dornan GJ, Fuso FA, LaPrade RF. Influence of lateral meniscal posterior root avulsions and the meniscofemoral ligaments on tibiofemoral contact mechanics. Knee Surg Sports Traumatol Arthrosc. 2016;24(5):1469–1477. [DOI] [PubMed] [Google Scholar]
- 12. Goldsmith MT, Jansson KS, Smith SD, Engebretsen L, LaPrade RF, Wijdicks CA. Biomechanical comparison of anatomic single- and double-bundle anterior cruciate ligament reconstructions: an in vitro study. Am J Sports Med. 2013;41(7):1595–1604. [DOI] [PubMed] [Google Scholar]
- 13. Liu X, Feng H, Zhang H, Hong L, Wang XS, Zhang J. Arthroscopic prevalence of ramp lesion in 868 patients with anterior cruciate ligament injury. Am J Sports Med. 2011;39(4):832–837. [DOI] [PubMed] [Google Scholar]
- 14. Liu X, Zhang H, Feng H, Hong L, Wang XS, Song GY. Is it necessary to repair stable ramp lesions of the medial meniscus during anterior cruciate ligament reconstruction? A prospective randomized controlled trial. Am J Sports Med. 2017;45(5):1004–1011. [DOI] [PubMed] [Google Scholar]
- 15. Papageorgiou CD, Gil JE, Kanamori A, Fenwick JA, Woo SL, Fu FH. The biomechanical interdependence between the anterior cruciate ligament replacement graft and the medial meniscus. Am J Sports Med. 2001;29(2):226–231. [DOI] [PubMed] [Google Scholar]
- 16. Parkinson B, Robb C, Thomas M, Thompson P, Spalding T. Factors that predict failure in anatomic single-bundle anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45(7):1529–1536. [DOI] [PubMed] [Google Scholar]
- 17. Peltier A, Lording T, Maubisson L, Ballis R, Neyret P, Lustig S. The role of the meniscotibial ligament in posteromedial rotational knee stability. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):2967–2973. [DOI] [PubMed] [Google Scholar]
- 18. Seil R, Mouton C, Coquay J, et al. Ramp lesions associated with ACL injuries are more likely to be present in contact injuries and complete ACL tears. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1080–1085. [DOI] [PubMed] [Google Scholar]
- 19. Shoemaker SC, Markolf KL. The role of the meniscus in the anterior-posterior stability of the loaded anterior cruciate-deficient knee: effects of partial versus total excision. J Bone Joint Surg Am. 1986;68(1):71–79. [PubMed] [Google Scholar]
- 20. Song GY, Liu X, Zhang H, et al. Increased medial meniscal slope is associated with greater risk of ramp lesion in noncontact anterior cruciate ligament injury. Am J Sports Med. 2016;44(8):2039–2046. [DOI] [PubMed] [Google Scholar]
- 21. Sonnery-Cottet B, Conteduca J, Thaunat M, Gunepin FX, Seil R. Hidden lesions of the posterior horn of the medial meniscus: a systematic arthroscopic exploration of the concealed portion of the knee. Am J Sports Med. 2014;42(4):921–926. [DOI] [PubMed] [Google Scholar]
- 22. Sonnery-Cottet B, Praz C, Rosenstiel N, et al. Epidemiological evaluation of meniscal ramp lesions in 3214 anterior cruciate ligament-injured knees from the SANTI study group database: a risk factor analysis and study of secondary meniscectomy rates following 769 ramp repairs. Am J Sports Med. 2018;46(13):3189–3197. [DOI] [PubMed] [Google Scholar]
- 23. Stephen JM, Halewood C, Kittl C, Bollen SR, Williams A, Amis AA. Posteromedial meniscocapsular lesions increase tibiofemoral joint laxity with anterior cruciate ligament deficiency, and their repair reduces laxity. Am J Sports Med. 2016;44(2):400–408. [DOI] [PubMed] [Google Scholar]
- 24. Thaunat M, Fayard JM, Guimaraes TM, Jan N, Murphy CG, Sonnery-Cottet B. Classification and surgical repair of ramp lesions of the medial meniscus. Arthrosc Tech. 2016;5(4):e871–e875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Thaunat M, Jan N, Fayard JM, et al. Repair of meniscal ramp lesions through a posteromedial portal during anterior cruciate ligament reconstruction: outcome study with a minimum 2-year follow-up. Arthroscopy. 2016;32(11):2269–2277. [DOI] [PubMed] [Google Scholar]
- 26. Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. PLoS Med. 2007;4(10):e297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ziegler CG, Pietrini SD, Westerhaus BD, et al. Arthroscopically pertinent landmarks for tunnel positioning in single-bundle and double-bundle anterior cruciate ligament reconstructions. Am J Sports Med. 2011;39(4):743–752. [DOI] [PubMed] [Google Scholar]