Abstract
Background:
Procedure-specific opioid-prescribing guidelines have the potential to decrease the number of unused pills in the home without compromising patient satisfaction. However, there is a paucity of data on the minimum necessary quantity to prescribe for outpatient orthopaedic surgeries.
Purpose:
To prospectively record daily opioid use and pain levels after arthroscopic meniscal procedures and anterior cruciate ligament reconstruction (ACLR) at a single institution.
Study Design:
Case series; Level of evidence, 4.
Methods:
A total of 95 adult patients who underwent primary arthroscopic knee surgery (meniscectomy, repair, or ACLR) were enrolled. Patients with a history of opioid dependence were ineligible. Daily opioid consumption and Numeric Rating Scale pain scores were collected through an automated text-messaging platform starting on postoperative day 1 (POD1). At 6 weeks or at patient-reported cessation of opioid use, final survey questions were asked. Patients who failed to complete data collection were excluded. Opioid use was converted into “pills” (oxycodone 5-mg equivalents) to facilitate comparisons and clinical applications. Factors associated with high and low opioid use were compared.
Results:
Of the 95 patients enrolled, 71 (74.7%) were included in the final analysis. Of these, 40 (56.3%) underwent meniscal surgery and 31 (43.7%) underwent ACLR. After outpatient arthroscopic meniscectomy or repair, the total median postdischarge opioid use was 0.3 pills (oxycodone 5-mg equivalents), with 75% of patients consuming 3.3 or fewer pills (range, 0-19 pills). For ACLR, the median postdischarge consumption was 7 pills (75th percentile, 23.3 pills; range, 0-41 pills). Almost one-third of patients (32.3%) took no opioids after surgery (3 ACLR, 20 meniscus). All meniscus patients and 71% of ACLR patients ceased opioid consumption by postoperative day 7.
Conclusion:
Opioids may not be necessary in all patients, particularly after meniscal surgery and in comparison with ACLR. For patients requesting opioids for pain relief, reasonable prescription quantities are 5 oxycodone 5-mg pills after arthroscopic meniscal procedures and 20 5-mg pills after ACLR. Slowing the current opioid epidemic and preventing future crises is dependent on refining prescribing habits. Clinicians should strongly consider patient education regarding expected pain as well as pain management strategies.
Keywords: opioid-prescribing guidelines, meniscectomy, meniscal repair, opioid consumption, anterior cruciate ligament reconstruction
In an effort to ensure functional recovery and adequate pain relief after orthopaedic surgery, providers have tended to overprescribe opioid pain medications.8,18 Past prescribing habits were in part responsible for the current opioid crisis, as patients have been left with significant amounts of leftover medication.8 Unused pills in the home are a risk for diversion for misuse by the patient, family, or friends.1 Patient education on proper disposal and institutional and municipal efforts to increase access to disposal centers are the methods by which the risk of diversion posed by unused pills can be addressed.11 However, source control is also a key aspect of a comprehensive opioid risk reduction strategy. The standardization of prescribing practices through institutional guidelines has been shown to reduce the amount of opioids prescribed at discharge.10,20,21 Unfortunately, there is a lack of data on opioid consumption after discharge for many orthopaedic procedures, precluding the creation of evidence-based as well as procedure- and patient-specific prescribing guidelines.9
There is a particular need for studies on postdischarge opioid use after outpatient surgery, as there is no inpatient consumption data on which to base the discharge prescription, a common recommendation in many narcotic-prescribing guidelines.10,20 Knee arthroscopy and anterior cruciate ligament reconstruction (ACLR) are 2 of the most common outpatient orthopaedic procedures.6 As such, establishing the minimum necessary quantity of opioids to prescribe after these procedures stands to reduce the overall quantity of leftover medication on a broad scale. To our knowledge, only 1 study has investigated patterns of postdischarge opioid use after knee arthroscopy,26 and no studies have been specifically designed to report postdischarge opioid use as a primary outcome after ACLR. The primary purpose of this study was to prospectively record daily opioid use and pain levels after arthroscopic meniscal procedures and ACLR at a single institution. These findings can be used to help establish benchmarks for interventions aiming to decrease opioid use and begin to inform procedure-specific opioid-prescribing guidelines.
Methods
After approval by the institutional review board, a prospective observation study of patients undergoing arthroscopically assisted ACLR or arthroscopic meniscectomy, repair, or debridement was conducted. Exclusion criteria included pediatric patients (skeletally immature), non-English speakers, revision surgery, opioid dependence (defined as daily opioid use in the 6 months prior to surgery), or a diagnosis of chronic pain in the patient’s chart. Chronic pain diagnoses were made by institutional pain specialists after referral by the primary surgeon.19 Research assistants identified and obtained consent from potential patients in the surgeon’s offices or the preoperative holding area. Surgeries were performed under spinal or regional anesthesia (adductor block and sedation) by 1 of 6 fellowship-trained orthopaedic sports surgeons, with the assistance of a fellow, resident, or physician assistant. All surgeries were performed between January 2018 and June 2018 on an outpatient basis at either the main hospital or an ambulatory surgery center associated with the institution. Given the observational nature of the study and to minimize the impact of the Hawthorne effect, surgeons participating in the study were not asked to change their pain- relief strategies, physical therapy regimens, or refill policies in any way. In general, with meniscal repairs being the exception, patients were weightbearing as tolerated after the procedure without range of motion restrictions.
A total of 95 patients consented and were enrolled. At the time of enrollment, patients were asked about their history of substance abuse, psychiatric history, and opioid use. Daily opioid users (6 months preoperatively) were excluded. Those who had taken opioids on a nondaily basis in the 6 months before surgery were classified as “intermittent opioid use” during analyses. Enrolled patients’ cell phone numbers were entered into an automated text messaging–based data collection system, created by 2 of the coauthors (F.L. and A. Premkumar) specifically for use in this study. As an alternative method of recording opioid use, a paper pain diary was available for patients without cell phones; however, no enrolled patients elected to use the pain diary. The platform is hosted by a third party; all technical details were thoroughly reviewed with the hospital’s informational technology department to ensure HIPAA (Health Information Portability and Accountability Act) compliance. The system was initially piloted for use after total joint arthroplasty and has also been used to study opioid use after spine surgery.17 Characteristic, prescription, procedural, and clinical data were extracted from the electronic medical record.
Primary outcomes of interest (opioid use and pain levels) were automatically collected through responses to daily text queries to the patients’ phones, sent at the same time every evening. At the time of enrollment, research assistants counseled patients on what medications could be classified as an opioid. Starting from the time of discharge from the hospital, patients were asked for the number of “opioid pain medication” pills consumed and their average pain level, as measured by the Numeric Rating Scale (NRS), over the prior 24 hours. These daily queries continued until the patient completed 6 weeks of data collection or self-reported opioid cessation. Specifically, patients who reported 4 consecutive days of taking no opioids were asked whether they had stopped taking opioids. Depending on the patient response, the system would automatically continue the daily queries or prompt the final survey questions. Final survey questions included adverse effects, number of remaining pills, and method of handling leftover pills. For those patients who did not respond to the final survey questions via text message, research assistants attempted to contact them through telephone to obtain the answers verbally. Refills were recorded from the state’s electronic prescription monitoring system. In the case that the electronic medical record was unclear regarding an initial prescription, the state’s electronic prescription registry was queried to resolve the discrepancy.
Patients who completed at least 50% of the daily text messages and responded to the final survey questions were included in the final analyses. This response rate has been previously deemed sufficient in electronic survey research.14 Patients whose procedures were misclassified or changed intraoperatively (eg, an open or revision procedure) were excluded from final analyses. Opioid use was converted into oral morphine equivalents (OMEs). To facilitate the comprehension of prescription and consumption quantities, opioid use was also converted into oxycodone 5-mg equivalents; the conversion ratio was 7.5 OME to one 5-mg oxycodone.
Statistical Analysis
All statistical analyses were performed using SPSS (Version 22; IBM). Descriptive statistics, including proportions, medians, and means, are reported for outcomes of interest as appropriate. Categorical variables were compared using chi-square tests (Fischer exact test when appropriate), and continuous variables were compared using Student t tests. Linear regression was utilized to analyze the relationship between the initial opioid prescription and the amount of opioid consumed. The sample was divided into high and low opioid use (top or bottom half of total opioid consumption), and characteristic, prescription, procedural, and clinical factors were compared between the cohorts. To adjust for confounding, a nonparsimonious logistic regression model, including age, body mass index, sex, index procedure, alcohol use, marijuana use, smoking status, psychiatric history, concomitant nonsteroidal anti-inflammatory medication (NSAID) prescription, and type of opioid prescription, was created to identify independent predictors of high or low opioid use. Significance was determined by a type 1 error of P < .05.
Results
Of the 95 patients enrolled, 71 patients (74.7%) were included in the final analysis. Two surgeries were converted to open procedures, 2 patients underwent an unplanned medial collateral ligament repair, 5 were revision procedures, 8 patients did not complete 50% of the daily text messages, and 7 patients did not complete the final survey questions and could not be reached by telephone. Table 1 demonstrates the characteristics of the study sample. The mean age was 39.9 years (range, 17-64 years), with a fairly even distribution of sex (46.5% males vs 53.5% females). No patient met the criteria for intermittent opioid use. A total of 8 patients (11.3%) had a documented psychiatric diagnosis, 7 (9.9%) were recreational marijuana users, 2 (2.8%) were current smokers, and 13 (18.3%) consumed more than 7 alcoholic drinks per week.
Table 1.
Characteristics of Study Samplea
| Age, y, mean ± SD (range) | 39.9 ± 13.1 (17-64) |
| BMI, kg/m2, mean ± SD (range) | 26.6 ± 5.2 (18.3-43.9) |
| Sex | |
| Male | 33 (46.5) |
| Female | 38 (53.5) |
| Smoking | |
| Nonsmoker | 69 (97.2) |
| Current smoker | 2 (2.8) |
| Alcohol use | |
| None | 11 (15.4) |
| 1-6 drinks/week | 47 (66.2) |
| 7-13 drinks/week | 11 (15.5) |
| ≥14 drinks/week | 2 (2.8) |
| Marijuana use | |
| None | 64 (90.1) |
| Current use | 7 (9.9) |
| Surgery | |
| Meniscal procedure | 40 (56.3) |
| ACLR | 31 (43.7) |
| Inpatient stay, d | |
| 0 | 67 (94.4) |
| 1 | 4 (5.6) |
| History of psychiatric disorderb | 8 (11.3) |
| Type of opioid prescribed | |
| Tramadol | 2 (28.8) |
| Oxycodone | 47 (66.2) |
| Hydrocodone | 22 (31.0) |
| Hydromorphone | 1 (1.4) |
| NSAID prescription | |
| Yes | 57 (80.3) |
| No | 14 (19.7) |
| Tylenol prescription | |
| Yes | 7 (9.9) |
| No | 64 (90.1) |
| Adductor blockc | |
| Yes | 24 (77.4) |
| No | 7 (22.6) |
aData are expressed as n (%) unless otherwise indicated. ACLR, anterior cruciate ligament reconstruction; BMI, body mass index; NSAID, nonsteroidal anti-inflammatory drug.
bDefined as medically diagnosed psychiatric disorder, either self-reported or in patient’s medical record.
cReported only for ACLR patients; no adductor blocks were performed for meniscal procedures.
Forty patients (56.3%) underwent a meniscal procedure and 31 (43.7%) underwent ACLR. Of those patients who underwent a meniscal procedure, 5 (12.5%) underwent a repair (4 all-inside, 1 outside-in), and the remainder underwent meniscectomy. In patients undergoing ACLR, the graft choices included ipsilateral hamstring autograft (18; 58.1%), patellar bone-tendon-bone autograft (5; 16.1%), and allograft (8; 25.8%). A total of 57 (80.3%) patients received a prescription for an NSAID while 7 (9.9%) received a prescription for acetaminophen.
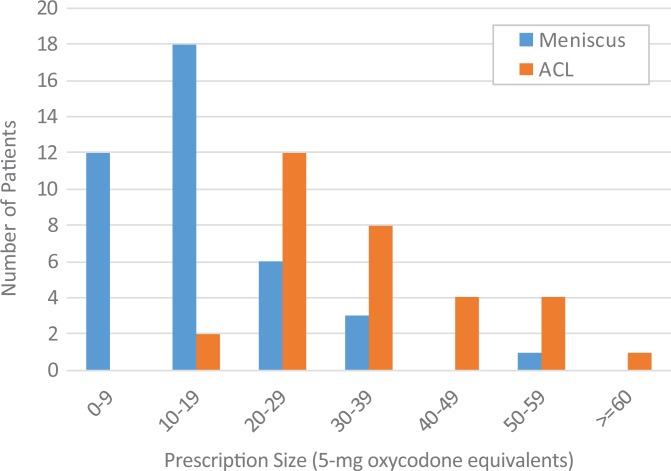
Figures 1 and 2 display initial opioid prescription quantities and total opioid consumption for each patient broken down by procedure. After outpatient arthroscopic meniscectomy or repair, the total median postdischarge opioid use was 0.3 oxycodone 5-mg equivalents, with 75% of patients consuming 3.3 or fewer pill equivalents (range, 0-19 pills). Total postdischarge opioid consumption ranged from 0 to 18.6 pill equivalents (0-140 OME). Of all patients, 20 (50%) took no narcotics after meniscal surgery.
Figure 1.
Distribution of initial opioid prescription size in terms of oxycodone 5-mg equivalents. ACL, anterior cruciate ligament.
Figure 2.
Distribution of total opioid consumed in terms of oxycodone 5-mg equivalents. ACL, anterior cruciate ligament.
For ACLR, the median postdischarge consumption was 7 oxycodone 5-mg equivalents, with 75% of patients consuming 23.3 pill equivalents or fewer. Total postdischarge opioid consumption ranged from 0 to 41 pill equivalents (0-307.5 OME). A total of 3 patients (9.7%) took no narcotics after surgery. Expectedly, patients who underwent ACLR consumed more narcotics compared with those undergoing meniscal procedures (mean, 12.8 ± 13.6 vs 2.5 ± 4.2; P < .001).
Thirteen patients (18.3%) completed their initial prescription, while 3 (4.2%) obtained a refill during the study period (all ACLR) (Table 2). Most patients had narcotics left over (81.7%). The mean quantity of leftover medication was 6.6 pill equivalents (49.2 OME), whereas the maximum number of leftover pill equivalents was 40. One in 4 patients (23.9%) had the equivalent of over 10 oxycodone 5-mg pills left. Half of those with leftover medications answered that they would keep their residual medication (49.0%), whereas only a minority (11.7%) reported appropriate methods of disposal (return to pharmacy, bring to police station/drop-off center).
Table 2.
Opioid Use Dataa
| n | OME | % or Range | |
|---|---|---|---|
| No. of patients completing initial prescription | 13 | — | 18.3 |
| Opioid refills within 6 weeks of surgery | 3 | — | 4.2 |
| Pills consumedb | 6.9 ± 10.6 | 51.9 ± 79.5 | 0-41 |
| Pills left overb | 6.6 ± 8.8 | 49.2 ± 65.9 | 0-40 |
| Method of disposalc | |||
| Destroy/throw away | 20 | — | 39.2 |
| Keep | 25 | — | 49.0 |
| Return to pharmacy or authorities | 6 | — | 11.7 |
aDashes indicate not applicable. OME, oral morphine equivalent.
bReported as mean ± SD and range. “Pill,” 5-mg oxycodone equivalent.
cReported as percentage of 51 patients (13 patients reported no pills remaining, 7 patients did not answer).
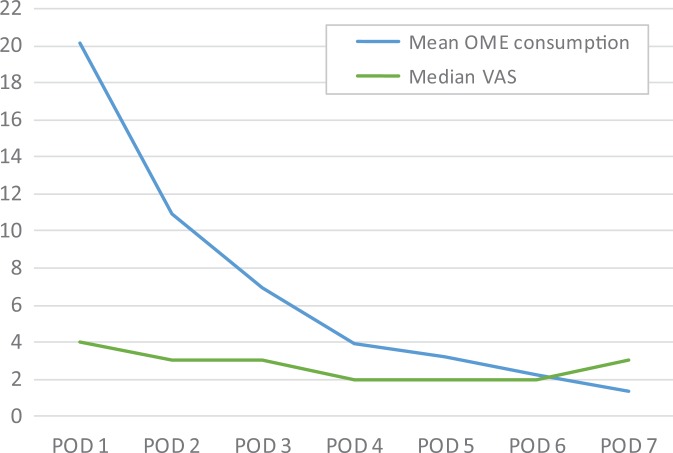
NRS pain scores and daily opioid consumption decreased steadily over the first postoperative week, with pain scores always falling in the mild to moderate range (Figure 3). Only 9 patients (12.7%) took opioids beyond postoperative day 7 (POD7) (all ACLR). The longest period of consumption was 18 days. No patient was taking opioids at the 6-week mark.
Figure 3.
Daily pain scores and opioid consumption per day. Values listed only until POD7, given that 85% of sample ceased opioid use by POD7. OME, oral morphine equivalent; POD, postoperative day; VAS, visual analog scale.
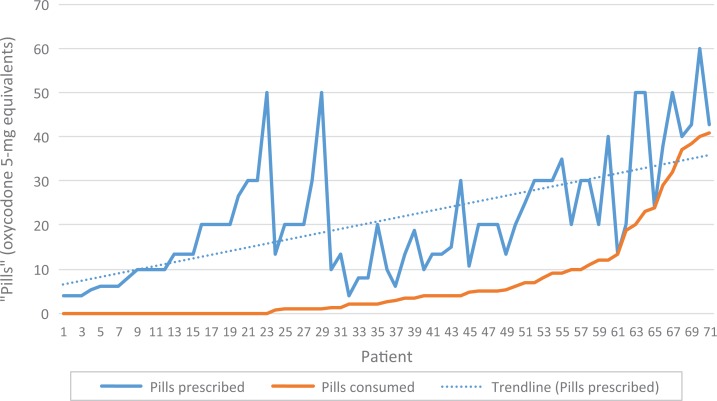
Linear regression was utilized to analyze the relationship between the total oxycodone 5-mg pill equivalents prescribed and consumed for each patient, (R 2 = 0.436) (Figure 4). Univariate comparisons between patients in the top and bottom half of opioid consumption revealed that the only factors associated with opioid use were the type of surgical procedure (high use 67.6% ACLR vs low use 22.2% ACLR; P < .001) and psychiatric diagnoses (high use 20% vs low use 2.8%; P = .022) (Table 3). The multivariate regression was underpowered, precluding meaningful conclusions.16
Figure 4.
Overall amount prescribed (including refills) vs opioid consumed per patient. R 2 = 0.436.
Table 3.
Comparison of Characteristics Between High and Low Opioid Use Patient Cohortsa
| Low Use (n = 36) | High Use (n = 35) | P | |
|---|---|---|---|
| Age, mean ± SD | 41.7 ± 13.9 | 38.1 ± 12.2 | .310 |
| BMI, mean ± SD | 26.6 ± 4.7 | 26.4 ± 5.7 | .864 |
| Sex | |||
| Male | 20 (55.6) | 13 (37.1) | .120 |
| Female | 16 (44.4) | 22 (62.9) | |
| Smoking | |||
| Nonsmoker | 34 (94.4) | 35 (100) | .157 |
| Current smoker | 2 (5.6) | 0 | |
| Alcohol use | |||
| <7 drinks/week | 32 (88.9) | 26 (74.3) | .112 |
| ≥7 drinks/week | 4 (11.1) | 9 (25.7) | |
| Marijuana use | |||
| None | 33 (91.7) | 31 (88.6) | .662 |
| Current use | 3 (8.3) | 4 (11.4) | |
| Surgery | |||
| Meniscal procedure | 28 (77.8) | 12 (34.3) | <.001 |
| ACLR | 8 (22.2) | 23 (65.7) | |
| Inpatient stay, d | |||
| 0 | 35 (97.2) | 32 (91.4) | .290 |
| 1 | 1 (2.8) | 3 (8.6) | |
| History of psychiatric disorder | |||
| No | 35 (97.2) | 28 (80.0) | .022 |
| Yes | 1 (2.8) | 7 (20.0) | |
| Type of opioid prescribed | |||
| Tramadol | 1 (2.8) | 1 (2.9) | .697 |
| Oxycodone | 23 (63.9) | 24 (68.5) | |
| Hydrocodone | 12 (33.3) | 9 (25.7) | |
| Hydromorphone | 0 | 1 (2.9) | |
| NSAID prescription | |||
| No | 5 (13.9) | 9 (25.7) | .211 |
| Yes | 31 (86.1) | 26 (74.3) | |
| Tylenol prescription | |||
| No | 32 (88.9) | 32 (91.4) | .720 |
| Yes | 4 (11.1) | 3 (8.6) | |
| Adductor blockb | |||
| Yes | 7 (87.5) | 17 (73.9) | .429 |
| No | 1 (12.5) | 6 (26.1) | |
aDefined as above or below the median use (3 oxycodone 5-mg pills, 22.5 OME). Data are expressed as n (%), unless otherwise indicated. ACLR, anterior cruciate ligament reconstruction; BMI, body mass index; NSAID, nonsteroidal anti-inflammatory medication.
bReported only for ACL patients.
Discussion
After outpatient arthroscopic meniscectomy or repair, the median postdischarge opioid use was 0.3 oxycodone 5-mg pill equivalents, with 75% of patients consuming 3.3 or fewer pill equivalents. With regard to ACLR, the median postdischarge consumption was 7 pill equivalents, with 75% of patients consuming 23.3 of fewer. Almost one-third of patients (32.3%) took no opioids after surgery. All patients undergoing meniscal procedures and 77% of ACLR patients ceased opioid use after the first week. While only 1 in 6 patients finished their prescriptions, a mere 1 in 20 obtained a refill.
These findings have several implications regarding the minimum necessary quantity of opioid that should be recommended by opioid-prescribing guidelines after outpatient meniscal procedures or ACLR. A prescription for 5 oxycodone 5-mg pills is a reasonable prescription amount after all meniscal procedures, which should account for opioid consumption of over 75% of patients, without leaving patients with excessive amounts of unused pills. With regard to ACLR, a guideline sanctioning a low amount as an initial prescription should theoretically increase refill requests; however, the true increase is likely overestimated, given that less than one-third of those patients who completed their prescription acquired a refill. The discrepancy between completing initial prescriptions and requesting refills has been noted in prior investigations on opioid use after knee and shoulder arthroscopy.8,26 Furthermore, a recent randomized trial of opioid prescriptions after arthroplasty found that larger prescriptions were associated with higher consumption, without affecting patient satisfaction.4 Thus, we believe 20 oxycodone 5-mg pills is a reasonable initial prescription quantity. Given that the opioid consumed increased dramatically beyond 20 pills (see Figure 2), targeting a higher percentile of use in the initial prescription would likely leave many patients with large numbers of unused pills without substantially decreasing refill requests or affecting satisfaction.
The opioid use figures reported in our study are slightly lower than those reported in a similar prospective observational study of 221 patients who underwent outpatient knee arthroscopy (76.9% meniscectomy, 5.9% meniscal repair, 8.6% chondroplasty, 6.3% loose body removal, and 2.3% debridement).26 Patients recorded postoperative opioid use in a pain diary, which was collected by study staff on their first postoperative visit. The median postoperative use was 7 hydrocodone 5-mg equivalents, equal to 4.67 oxycodone 5-mg equivalents (75th percentile, approximately 7 oxycodone 5-mg pills). Differences in consumption may be explained by the initial prescription quantity. While 68.5% of the patients in our study received a prescription of <30 oxycodone 5-mg pill equivalents, 66.9% of patients in the study by Wojahn et al26 received 40 or more pill equivalents at discharge. First, our linear regression suggested an association between prescription quantities and overall use, an association corroborated in past research.4 Second, geographical variation between the studies may also have played a role in opioid consumption.15 Third, our study was performed almost 1.5 years later (began May 2016 vs January 2018), during a time in which public awareness of the dangers of opioids rapidly increased. Regardless of this, both studies support the notion that many patients take very few pills—43% of study patients in the study by Wojahn et al26 consumed fewer than 3.3 oxycodone 5 mg. Thus, while the actual numbers were slightly variable, the clinical difference in opioid consumption of 2 to 3 pills is small and the 2 studies are similar in their conclusions.
This study also presents several key findings regarding the content of educational components that should be considered in any prescribing guideline. First, patients may be counseled that postoperative opioid use is likely to cease within the first few days, 1 week at a maximum—findings similar to previous research.26 Second, there is a great need for education on pill disposal and access to medication disposal centers. Half of the patients with leftover pills reported that they would keep their leftover medications, putting the medication at high risk for diversion to friends or family or for later use by the patient in dangerous scenarios. Lack of access or knowledge regarding pill disposal methods is a common theme in the literature.8,18 For institutions that wish to minimize refill requests by increasing initial prescription sizes, guidelines that provide clear, easy-to-understand instructions on pill destruction methods and pill disposal centers are essential to mitigate the increased risk of diversion of leftover medication. Third, given that multimodal analgesia is the standard of care, patients should be counseled on the role of opioids within multimodal analgesia, the possible adverse effects, and the emergence of dependency with long-term use. Last, the wide variety of opioid use seen among the population sample suggests that blind adherence to a prescribing guideline can be potentially harmful. Almost one-third of patients (half of meniscus patients) took no narcotics after surgery, suggesting that patients should not be universally prescribed narcotics after meniscectomy or ACLR. In many countries outside of the United States, opioids are not routinely prescribed after procedures such as ankle fracture fixation or hip replacement.2,5 In the United States, previous investigations have also shown a contingent of patients who take no to very few opioids after procedures such as 1-level spine surgery or total joint replacement.4,9 Providers may consider asking patients if they would like an opioid prescription at discharge instead of prescribing narcotics after every case.
Deciphering the predictors of increased use within this spectrum is likely to remain challenging. Individualized prescriptions for postoperative opioid use, based on predictive modeling of known influential factors, could help us to better define expected use, potentially eliminating leftover medication and refill requests. However, our findings corroborate past research,3,4,26 concluding that postoperative opioid consumption is difficult to predict. While there is substantial evidence12,23 behind factors associated with the development of chronic opioid consumption or long-term use, these factors (male sex, depression, chronic back pain, and preoperative opioid use) have not been consistently borne out as risk factors for increased immediate postoperative consumption.4,26 While the development of chronic opioid consumption is a greater health hazard for the patients themselves, understanding the factors associated with short-term use is essential to individualizing prescriptions that can reduce the number of leftover pills available for diversion. Despite testing a variety of factors for associations, very few have been found to be associated with increased opioid use in the acute postoperative period. Two studies found that male sex and postoperative pain levels were associated with narcotic consumption (of note, 1 study was in a pediatric population), whereas another study reported associations with smoking and preoperative opioid use in the month before surgery.3,4,26 Notably, ours is the first to report a significant association with history of a psychiatric disorder (P = .022), one of the factors most commonly reported in studies on chronic opioid use.12,22 Interestingly, no study, including ours, has found an association between adjunct analgesics (nonsteroidal anti-inflammatory medications, acetaminophen, or gabapentin) and total opioid consumption after discharge.3,4,26
While a lack of power may explain the largely negative findings of ours and others on predictors of increased postoperative opioid use, another potential explanation is that we do not understand, or are not accurately capturing, the drivers behind postoperative opioid consumption. Over the first postoperative week, the median NRS pain scores and opioid consumption both decreased (see Figure 3). However, while pain scores remained in the moderate range, slowly decreasing over time, the mean opioid consumption decreased at a much faster rate. This suggests that there is a complex relationship between a patient’s opioid use and the patient’s level (or experience) of pain, and that pain likely has a nonlinear relationship with opioid consumption. This theory is further supported by the slight uptick in the median reported pain level on POD7, as the small portion of patients who remained on opioids at that point likely had an atypical pain experience. There is a wide body of research showing that side effects, patient-specific knowledge regarding opioids, objective nociception, inherent gene-specific metabolism, and levels of pain catastrophizing are all factors that may influence patient consumption.5,7,13,24,25 Future studies should be specifically directed at targeting these “nontraditional” factors if we are to advance our knowledge about postoperative opioid consumption and the patient-specific pain experience.
There were several limitations of this investigation. First, while the anonymous, automated data collection system was designed to minimize reporting bias through collecting daily data (instead of weekly/monthly reports), opioids are currently a controversial topic, and there may have been underreporting of consumption. However, the effect of this reporting bias was likely minimal; Wojahn et al26 verified patient-reported pill counts with counts made by research assistants, finding identical numbers in 85% of cases. Second, while this was not the primary purpose of the investigation, the study was underpowered to detect independent associations with opioid use, as evidenced by the failure of the multivariate analysis to reach significance for any tested factor. Furthermore, as discussed, there are likely several factors that influence opioid use that were not measured or accounted for in this study.5,7,13,24,25 Third, given that attitudes and prescribing patterns have been shown to vary by state, the findings of this study may be limited in their nationwide applicability.15 International applications of these findings are precluded by marked differences in the use of opioids for pain relief.2,5,27 Fourth, we were unable to account for surgical variability or differences in invasiveness between the procedures. The surgical technique of ACLR and meniscectomy was no doubt slightly different among the surgeons in this study. Regardless of this, any procedure-specific prescribing guideline must make assumptions of surgical consistency in order to be clinically useful. We would encourage providers to specifically examine opioid use within their own patients to help further refine prescription quantities in the setting of identical surgical techniques. Fifth, because of the study power, we were not able to draw meaningful conclusions regarding opioid consumption based on the ACL graft choice or the type of meniscal procedure. Sixth, given that we could not control for over-the-counter medication taken by study participants, we cannot draw strong conclusions regarding the effect of NSAIDs or acetaminophen. Given that modern postsurgical pain relief is standardized to include a component of multimodal analgesia (cryotherapy, anti-inflammatory medications, adjunct analgesics, etc),19 any guideline for opioid prescriptions should include a modern multimodal analgesia concept as a component. Last, we did not control the initial prescription amounts, potentially influencing average opioid consumption and the conclusions of this investigation.4
Conclusion
We present several important findings that should be incorporated into the creation of opioid-prescribing guidelines after arthroscopic meniscal procedures and ACLR. Given that almost one-third of patients did not take opioids after surgery, opioids should be offered on an as-needed basis and not universally prescribed. After meniscal procedures, 75% of patients consumed 3.3 or fewer oxycodone 5-mg equivalents. After ACLR, the median postoperative consumption was 7 oxycodone 5-mg equivalents, with 75% of patients consuming 23.3 pill equivalents or fewer. Considering these numbers, for those patients who are prescribed opioids, 5 oxycodone 5-mg pills after meniscectomy and 20 pills after ACLR are reasonable initial prescription quantities that should allow for satisfactory pain relief without leading to excessive numbers of unused pills or refill requests. Prescribing guidelines should include large sections on patient education regarding opioid use and proper medication disposal methods, and institutions must increase access to and awareness of disposal centers. Opioid use is widely variable and difficult to predict, making blind adherence to a quantitative prescribing protocol potentially harmful. Clinical judgment must be utilized in all circumstances, and patients that are taking excessive amounts of opioids (with regard to the benchmarks presented in this study) should be followed closely and frequently. Future research should be directed at validating quantitative, procedure-specific prescribing guidelines, investigating the wide variety of biopsychosocial factors that may affect opioid use, and predictive modeling of postoperative opioid consumption.
Footnotes
Final revision submitted December 11, 2019; accepted December 23, 2019.
One or more of the authors declared the following potential conflict of interest or source of funding: This study was funded in part by a Surgeon in Chief grant from the Hospital for Special Surgery. M.M. has received educational support from Arthrex and Smith & Nephew and speaking fees from Arthrex. B.S.S. has received speaking fees from Arthrex. A.P. has received educational support from Arthrex; consulting fees from Zimmer Biomet, Stryker, and Exactech; speaking fees from Smith & Nephew; and royalties from Zimmer Biomet. S.T. has received educational support from Arthrex and Smith & Nephew, consulting fees from DePuy, hospitality payments from Encore Medical and Exactech, and honoraria from Encore Medical. T.A. has received consulting fees from DePuy and NuVasive and royalties from Zimmer Biomet and DePuy. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Hospital for Special Surgery Institutional Review Board (study No. 2017-0046-CR1).
References
- 1. American Society of Addiction Medicine. Opioid addiction 2016 facts & figures; 2016. https://www.asam.org/docs/default-source/advocacy/opioid-addiction-disease-facts-figures.pdf. Accessed May 5, 2019.
- 2. Devine CA, Yu A, Kasdin RG, et al. Postoperative pain management among Dominican and American health-care providers: a qualitative analysis. J Bone Joint Surg Am. 2016;98(12):e50. [DOI] [PubMed] [Google Scholar]
- 3. Grant DR, Schoenleber SJ, McCarthy AM, et al. Are we prescribing our patients too much pain medication? J Bone Joint Surg Am. 2016;98(18):1555–1562. [DOI] [PubMed] [Google Scholar]
- 4. Hannon C, Calkins T, Li J, et al. The James A. Rand Young Investigator’s Award: large opioid prescriptions are unnecessary after total joint arthroplasty: a randomized controlled trial. J Arthroplasty. 2019;34(7)(suppl):S4–S10. [DOI] [PubMed] [Google Scholar]
- 5. Helmerhorst GTT, Lindenhovius ALC, Vrahas M, Ring D, Kloen P. Satisfaction with pain relief after operative treatment of an ankle fracture. Injury. 2012;43(11):1958–1961. [DOI] [PubMed] [Google Scholar]
- 6. Kim S, Bosque J, Meehan JP, Jamali A, Marder R. Increase in outpatient knee arthroscopy in the United States: a comparison of national surveys of ambulatory surgery, 1996 and 2006. J Bone Joint Surg Am - Ser A. 2011;93(11):994–1000. [DOI] [PubMed] [Google Scholar]
- 7. Kirchheiner J, Keulen JTHA, Bauer S, Roots I, Brockmöller J. Effects of the CYP2D6 gene duplication on the pharmacokinetics and pharmacodynamics of tramadol. J Clin Psychopharmacol. 2008;28(1):78–83. [DOI] [PubMed] [Google Scholar]
- 8. Kumar K, Gulotta LV, Dines JS, et al. Unused opioid pills after outpatient shoulder surgeries given current perioperative prescribing habits. Am J Sports Med. 2017;45(3):636–641. [DOI] [PubMed] [Google Scholar]
- 9. Lovecchio F, Derman P, Stepan J, et al. Support for safer opioid prescribing practices. J Bone Joint Surg Am. 2017;99(22):1945–1955. [DOI] [PubMed] [Google Scholar]
- 10. Lovecchio F, Stepan JG, Premkumar A, et al. An institutional intervention to modify opioid prescribing practices after lumbar spine surgery. J Neurosurg Spine. 2019;30(4):483–490. [DOI] [PubMed] [Google Scholar]
- 11. Lovecchio FC, Premkumar A, Stepan JG, Albert TJ. Fighting back: institutional strategies to combat the opioid epidemic: a systematic review. HSS J. 2019;15(1):66–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mohamadi A, Chan JJ, Lian J, et al. Risk factors and pooled rate of prolonged opioid use following trauma or surgery. J Bone Joint Surg Am. 2018;100(15):1332–1340. [DOI] [PubMed] [Google Scholar]
- 13. Nickel BT, Klement MR, Byrd WA, Attarian DE, Seyler TM, Wellman SS. The James A. Rand Young Investigator’s Award: Battling the opioid epidemic with prospective pain threshold measurement. J Arthroplasty. 2018;33(7)(suppl):S3–S7. [DOI] [PubMed] [Google Scholar]
- 14. Nota SPFT, Strooker JA, Ring D. Differences in response rates between mail, e-mail, and telephone follow-up in hand surgery research. Hand. 2014;9(4):504–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Paulozzi LJ, Mack KA, Hockenberry JM. Variation among states in prescribing of opioid pain relievers and benzodiazepines—United States, 2012. J Safety Res. 2014;51:125–129. [DOI] [PubMed] [Google Scholar]
- 16. Peduzzi P, Concato J, Kemper E, Holford TR, Feinstem AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49(12):1373–1379. [DOI] [PubMed] [Google Scholar]
- 17. Premkumar A, Lovecchio FC, Stepan JG, et al. A novel mobile phone text messaging platform improves collection of patient-reported post-operative pain and opioid use following orthopedic surgery. HSS J. 2019;15(1):37–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sabatino MJ, Kunkel ST, Ramkumar DB, Keeney BJ, Jevsevar DS. Excess opioid medication and variation in prescribing patterns following common orthopaedic procedures. J Bone Joint Surg Am. 2018;100(3):180–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Soffin EM, Waldman SA, Stack RJ, Liguori GA. An evidence-based approach to the prescription opioid epidemic in orthopedic surgery. Anesth Analg. 2017;125(5):1704–1713. [DOI] [PubMed] [Google Scholar]
- 20. Stepan JG, Lovecchio FC, Premkumar A, et al. Development of an institutional opioid prescriber education program and opioid-prescribing guidelines: impact on prescribing practices. J Bone Joint Surg Am. 2019;101(1):5–13. [DOI] [PubMed] [Google Scholar]
- 21. Stepan JG, Sacks HA, Lovecchio FC, et al. Opioid prescriber education and guidelines for ambulatory upper-extremity surgery: evaluation of an institutional protocol. J Hand Surg Am. 2018;44(2):129–136. [DOI] [PubMed] [Google Scholar]
- 22. Sun EC, Darnall B, Baker LC, Mackey S. Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period. JAMA Intern Med. 2016;94305:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sun EC, Darnall BD, Baker LC, MacKey S. Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period. JAMA Intern Med. 2016;176(9):1286–1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Syed UAM, Aleem AW, Wowkanech C, et al. Neer Award 2018: the effect of preoperative education on opioid consumption in patients undergoing arthroscopic rotator cuff repair: a prospective, randomized clinical trial. J Shoulder Elbow Surg. 2018;27(6):962–967. [DOI] [PubMed] [Google Scholar]
- 25. Teunis T, Stoop N, Park CJ, Ring D. What factors are associated with a second opioid prescription after treatment of distal radius fractures with a volar locking plate? Hand. 2015;10(4):639–648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wojahn R, Bogunovic L, Brophy R, et al. Opioid consumption after knee arthroscopy. J Bone Joint Surg Am. 2018;100A(19):1629–1636. [DOI] [PubMed] [Google Scholar]
- 27. Zaslansky R, Meissner W, Chapman CR. Pain after orthopaedic surgery: differences in patient reported outcomes in the United States vs internationally. An observational study from the PAIN OUT dataset. Br J Anaesth. 2018;120(4):790–797. [DOI] [PMC free article] [PubMed] [Google Scholar]