Abstract
Objective
To summarize the cancer burden and trends in China, compare the differences among China, Japan, and South Korea and discuss possible causes of the disparities.
Methods
Incidence and mortality data were extracted from the online cancer database including the GLOBOCAN 2018 and the Global Burden of Disease Study 2017. Trend analysis was conducted using the join-point analysis, and annual percent changes were calculated.
Results
Cancers resulted in approximately 62.9 million disability-adjusted life years (DALYs) in China in 2017. Lung cancer had the greatest contribution, followed by liver cancer, stomach cancer, and esophageal cancer. The trajectory of progress in the reduction of liver and stomach cancers was observed in China. However, China still faced a heavy burden of lung cancer and a growing burden of cancers related to westernized lifestyle such as colorectal cancer, while Japan and South Korea have achieved reductions in colorectal cancer and lung cancer, respectively. Besides, China had a lower age-standardized cancer incidence rate but higher cancer mortality and DALY rates than Japan and South Korea.
Conclusions
China is in the cancer transition stage with a rising burden of colorectal, prostate, and breast cancers along with a heavy burden of lung and upper digestive tract cancers. Taking into consideration the effectiveness of screening and tobacco control in Japan and South Korea, improvement in the current tobacco control policy and cancer screening systems may contribute to cancer control in China.
Keywords: Cancer burden, trend, China, comparison
Introduction
Cancer is the leading cause of death worldwide (1). Distinct geographic disparities exist in cancer burden across the world (2). China, Japan, and South Korea are all located in East Asia. As neighboring countries, Japan and South Korea share similar genetic backgrounds and similar culture with China. Also, in terms of cancer burden, these three countries are all facing a heavy burden of upper digestive tract cancers. But China, Japan, and South Korea are at different stages of socio-economic development. Japan and South Korea are ahead of China in industrialization and urbanization and have higher incidence rates of some westernized lifestyle-related cancers, such as breast cancer and colorectal cancer (3). Besides, Japan and South Korea have a longer history of nationwide cancer control programs than China (4,5). Comparison among these three countries for the cancer burden and trends could be useful to track the effectiveness of national screening programs and to identify modifiable risk factors. The results can serve as a scientific reference for cancer control policy planning.
Thus, we sought to provide an overview of cancer burden and trends in China and to compare them with those in Japan and South Korea. Considering the credibility, availability, and comparability of data, we conducted the analysis based on the online cancer database from the GLOBOCAN 2018 (6) and the Global Burden of Disease Study 2017 (GBD 2017) (7) and we also reviewed cancer survival data from the CONCORD-3 (8), cancer registry reports from China (9,10), Japan (11,12), and South Korea (5,13). We hope that this comparative analysis could contribute to improving measures of cancer control in China.
Materials and methods
Data sources
National estimates of age-standardized incidence and mortality for China, Japan, and South Korea in 2018 were obtained from the GLOBOCAN 2018 (6). The GLOBOCAN project initiated by the International Agency for Research on Cancer (IARC) systematically quantified the incidence, mortality, and prevalence in 185 countries or territories for 36 cancer types. The projected national rates for China in the GLOBOCAN 2018 were based on the recent data from 92 cancer registries. Observed national rates, including incidence and mortality in South Korea, and mortality in Japan, were available and applied to predict the corresponding rates in 2018. Incidence rates in Japan were estimated using mortality-to-incidence ratios derived from cancer registries (14). For the trend analysis, we referred to the cancer incidence in five continents (CI5) series (15). The incidence data in CI5 series were derived from high-quality national population-based registries including five registries in China, five in South Korea and four in Japan. All age-standardized rates of incidence and mortality were calculated using the world standard population. Cancer survival data were retrieved from the CONCORD-3 (8), which provides the largest and latest international cancer survival data. Age-standardized five-year survival rates were calculated using the International Cancer Survival Standard weights (16).
Disability-adjusted life years (DALYs) attributable to cancers for China, Japan, and South Korea in 1990 and 2017 were retrieved from the GBD online results tool (7) engineered by the Institute for Health Metrics and Evaluation (IHME). The GBD annually provides age-sex-specific DALYs for countries across the world. Detailed methods for the GBD 2017 study have been reported in previous studies (17,18). In this study, DALYs per 100,000 population estimates for 29 cancer sites in China, Japan, and South Korea in 2017 were presented by sex and age. To reflect the trends of cancer burden, we also showed the percentage change in all-age and age-standardized DALY rates in China, Japan, and South Korea from 1990 to 2017. The age-standardized DALY rates were based on the GBD reference population (18).
Statistical analysis
Join-point models were used (19) to examine the time trends in age-standardized incidence rates for selected cancer sites in China, Japan, and South Korea. We applied the logarithmic transformation of the rates and a maximum number of two join-points (three line segments) in the models. The annual percent change (APC) was calculated to indicate the direction and magnitude of the trends. The term “increase” or “decrease” was used if the APC was statistically different from zero. P<0.05 was considered statistically significant. The trend analysis was conducted by Joinpoint Regression Program (V.4.7.0.0, National Cancer Institute, 2019).
Results
Current cancer burden in China
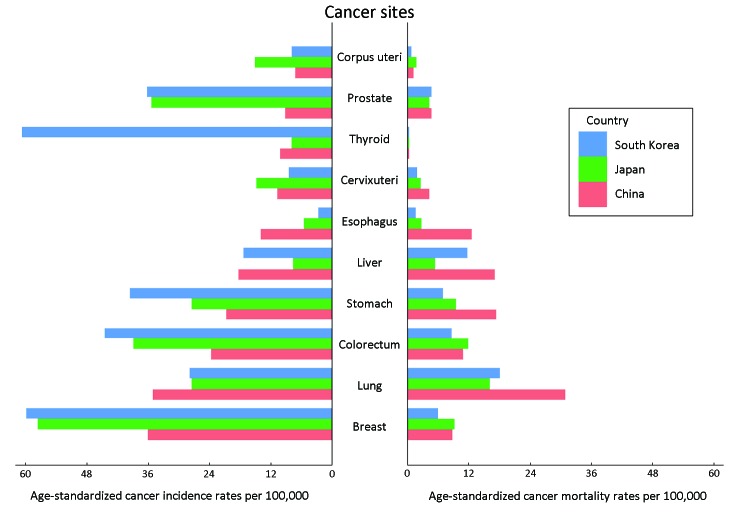
According to the estimates by the GLOBOCAN 2018, about 4,285,033 new cancer cases were diagnosed in China in 2018, which included 2,366,010 males and 1,919,023 females. The crude and age-standardized incidence rates (ASIR) for all cancers were 301.1 and 201.7 per 100,000, respectively. An estimated 2,865,174 cancer deaths occurred in 2018, with 1,791,805 deaths occurring in males and 1,073,369 in females. The crude and age-standardized mortality rates (ASMR) were 201.3 and 130.1 per 100,000, respectively. The incidence and mortality rates were higher in males than in females. Table 1 and Figure 1 show that breast cancer has the highest ASIR in both sexes combined, followed by lung cancer, colorectal cancer, and stomach cancer. Lung cancer was the leading cause of cancer death, followed by stomach cancer, liver cancer, and esophageal cancer.
1. Age-standardized cancer incidence and mortality rates per 100,000 populations by gender in China in 2018.
| Index | Gender | All cancers | Rank | |||||||||
| 1st | 2nd | 3rd | 4th | 5th | 6th | 7th | 8th | 9th | 10th | |||
| CNS, central nervous system; NHL, non-Hodgkin lymphoma. The estimates are from Global Cancer Observatory 2018, IARC, 2018 (6). Age-standardized rates are calculated using the direct method and the world standard population. | ||||||||||||
| Incidence | Both | 201.7 | Breast | Lung | Colorectum | Stomach | Liver | Esophagus | Cervix uteri | Thyroid | Prostate | Corpus uteri |
| 36.1 | 35.1 | 23.7 | 20.7 | 18.3 | 13.9 | 10.7 | 10.1 | 9.1 | 7.1 | |||
| Male | 223.0 | Lung | Stomach | Colorectum | Liver | Esophagus | Prostate | Pancreas | Bladder | Leukemia | NHL | |
| 47.8 | 29.5 | 28.1 | 27.6 | 19.7 | 9.1 | 6.2 | 5.9 | 5.8 | 4.8 | |||
| Female | 182.6 | Breast | Lung | Colorectum | Thyroid | Stomach | Cervix uteri | Liver | Esophagus | Corpus uteri | Ovary | |
| 36.1 | 22.8 | 19.4 | 15.8 | 12.3 | 10.7 | 9.0 | 8.2 | 7.1 | 5.3 | |||
| Mortality | Both | 130.1 | Lung | Stomach | Liver | Esophagus | Colorectum | Breast | Pancreas | Prostate | Cervix uteri | Leukemia |
| 30.9 | 17.5 | 17.1 | 12.7 | 10.9 | 8.8 | 4.9 | 4.7 | 4.4 | 3.5 | |||
| Male | 166.6 | Lung | Liver | Stomach | Esophagus | Colorectum | Pancreas | Prostate | Leukemia | Brain, CNS | NHL | |
| 43.4 | 25.6 | 25.0 | 18.2 | 13.1 | 5.6 | 4.7 | 4.4 | 3.6 | 2.8 | |||
| Female | 95.2 | Lung | Stomach | Colorectum | Breast | Liver | Esophagus | Cervix uteri | Pancreas | Ovary | Brain, CNS | |
| 19.0 | 10.4 | 8.8 | 8.8 | 8.6 | 7.4 | 4.4 | 4.2 | 2.9 | 2.8 | |||
1. Age-standardized incidence and mortality rates per 100,000 populations of selected types of cancers in China (red), Japan (green), and South Korea (blue) in 2018. The data used to generate this figure were from the GLOBOCAN database (6).
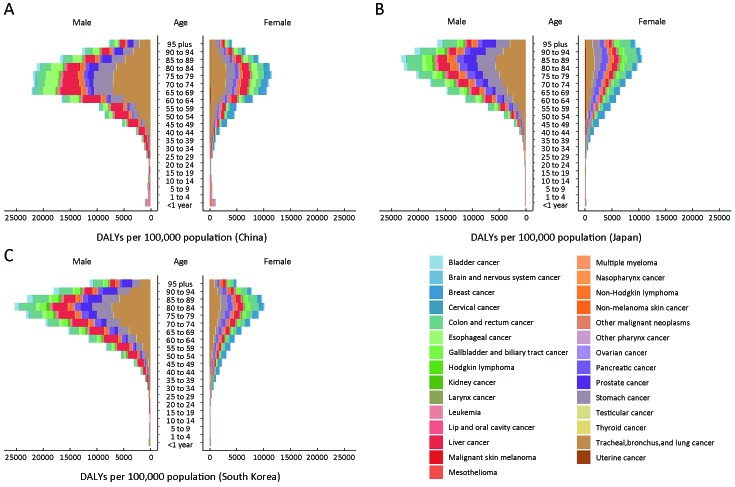
Table 2 shows all age and age-standardized DALYs per 100,000 populations in China in 2017. The GBD 2017 estimated that cancers resulted in approximately 62.9 million DALYs in China. Lung cancer had the greatest contribution (24.3%) to the cancer DALY burden in China in 2017, followed by liver cancer (17.7%), stomach cancer (12.4%), and esophageal cancer (7.1%). These four cancer types accounted for more than 60% of cancer DALYs in China. Figure 2 illustrates the etiologic constituent of DALYs by age and sex. Leukemia dominated among the youth (<20 years), but brain and nervous system cancer was also an important cancer among young age groups. For young and middle-aged adult males, liver cancer and lung cancer were the leading causes of DALYs. Breast cancer resulted in the greatest part of the DALY burden among young and middle-aged adult females. Among elderly adults (>50 years), lung cancer and liver cancer represented the highest disease burden for each sex separately and combined.
2. All age and age-standardized DALYs rates per 100,000 populations by gender in China in 2017.
| Index | Gender | All cancers | Rank | |||||||||
| 1st | 2nd | 3rd | 4th | 5th | 6th | 7th | 8th | 9th | 10th | |||
| DALYs, disability-adjusted life years; CNS, central nervous system; Other, other malignant neoplasms. The estimates are from the Institute for Health Metrics and Evaluation (IHME) website (7). Age-standardized rates are calculated using the GBD reference population (18). | ||||||||||||
| All age rates | Both | 4,450.2 | Lung | Liver | Stomach | Esophagus | Colorectum | Breast | Leukemia | Other | Brain, CNS | Pancreas |
| 1,079.9 | 789.6 | 553.3 | 316.1 | 301.2 | 186.8 | 163.2 | 143.2 | 138.7 | 133.9 | |||
| Male | 5,607.2 | Lung | Liver | Stomach | Esophagus | Colorectum | Leukemia | Brain, CNS | Other | Pancreas | Prostate | |
| 1,479.7 | 1,195.4 | 758.1 | 469.8 | 356.7 | 187.4 | 162.5 | 159.9 | 153.1 | 122.2 | |||
| Female | 3,243.2 | Lung | Breast | Liver | Stomach | Colorectum | Cervical | Esophagus | Leukemia | Other | Brain, CNS | |
| 662.7 | 370.4 | 366.3 | 339.6 | 243.3 | 194.1 | 155.8 | 137.9 | 125.9 | 113.9 | |||
| Age-standardized rates | Both | 3,257.9 | Lung | Liver | Stomach | Esophagus | Colorectum | Leukemia | Breast | Other | Brain, CNS | Pancreas |
| 757.6 | 552.1 | 391.7 | 222.6 | 216.2 | 171.0 | 130.6 | 126.1 | 124.6 | 94.3 | |||
| Male | 4,202.8 | Lung | Liver | Stomach | Esophagus | Colorectum | Leukemia | Brain, CNS | Other | Pancreas | Prostate | |
| 1,075.4 | 852.4 | 553.7 | 341.2 | 265.5 | 194.2 | 146.1 | 136.2 | 111.3 | 101.6 | |||
| Female | 2,344.3 | Lung | Breast | Liver | Stomach | Colorectum | Leukemia | Cervical | Other | Esophagus | Brain, CNS | |
| 451.8 | 253.0 | 251.6 | 235.5 | 168.9 | 146.6 | 132.3 | 117.9 | 107.6 | 102.3 | |||
2. Disability-adjusted life years (DALYs) per 100,000 populations attributable to cancers by age and gender in China (A), Japan (B), and South Korea (C) in 2017. The estimates used to generate this figure were from the Institute for Health Metrics and Evaluation (IHME) website (7).
Time trends in China
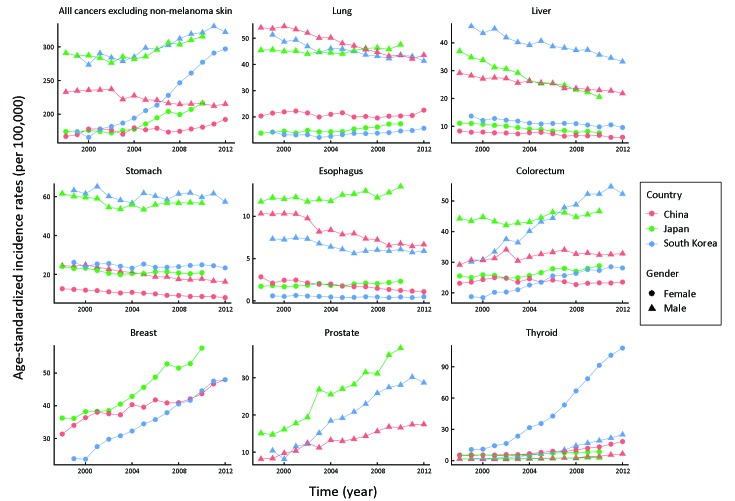
Table 3 shows that the ASIR for all cancers in females was stable from 1998 to 2012 in China. But a significant downward trend was observed in males during this period. As is shown in Figure 3 , the ASIR of lung cancer held steady in both sexes since 2009. Upward trends in the ASIR were observed for colorectal cancer, prostate cancer, and thyroid cancer in males and breast cancer in females. In contrast, the ASIR of stomach cancer, esophageal cancer, and liver cancer showed significant declines for each sex.
3. Trends in age-standardized incidence rates for selected cancers and all cancers combined by gender in China, Japan, and South Korea (%).
| Sites | China | Japan | South Korea | |||||||||||||||||||||||
| Trend 1 | Trend 2 | Trend 3 | Trend 1 | Trend 2 | Trend 3 | Trend 1 | Trend 2 | Trend 3 | ||||||||||||||||||
| Years | APC | Years | APC | Years | APC | Years | APC | Years | APC | Years | APC | Years | APC | Years | APC | Years | APC | |||||||||
| APC, annual percentage change; APC is calculated using age-standardized incidence data based on the world standard population; *, The APC is significantly different from zero (P<0.05);†, All cancers exclude non-melanoma skin. | ||||||||||||||||||||||||||
| Male | ||||||||||||||||||||||||||
| All cancers† | 1998−
2012 |
−0.8* | 1998−
2002 |
−1.3* | 2002−
2010 |
1.6* | 1999−
2012 |
1.3* | ||||||||||||||||||
| Lung | 1998−
2000 |
0.8 | 2000−
2009 |
−2.5* | 2009−
2012 |
−0.3 | 1998−
2005 |
−0.4 | 2005−
2010 |
1.3* | 1999−
2012 |
−1.4* | ||||||||||||||
| Liver | 1998−
2012 |
−1.9* | 1998−
2010 |
−4.6* | 1999−
2012 |
−2.2* | ||||||||||||||||||||
| Stomach | 1998−
2000 |
1.0 | 2000−
2006 |
−4.4* | 2006−
2012 |
−2.5* | 1998−
2003 |
−2.7* | 2003−
2010 |
0.8 | 1999−
2012 |
−0.3 | ||||||||||||||
| Esophagus | 1998−
2012 |
−3.8* | 1998−
2010 |
0.8* | 1999−
2002 |
−0.2 | 2002−
2006 |
−5.6* | 2006−
2012 |
0.5 | ||||||||||||||||
| Colorectum | 1998−
2012 |
0.7* | 1998−
2010 |
0.5* | 1999−
2009 |
5.8* | 2009−
2012 |
0.3 | ||||||||||||||||||
| Prostate | 1998−
2002 |
10.1* | 2002−
2012 |
4.6* | 1998−
2010 |
8.7* | 1999−
2012 |
10.3* | ||||||||||||||||||
| Thyroid | 1998−
2000 |
−7.9 | 2000−
2008 |
9.1* | 2008−
2012 |
22.9* | 1998−
2002 |
−2.3 | 2002−
2010 |
8.2* | 1999−
2001 |
7.6 | 2001−
2009 |
27.9* | 2009−
2012 |
12.9* | ||||||||||
| Female | ||||||||||||||||||||||||||
| All cancers† | 1998−
2000 |
3.1 | 2000−
2009 |
0 | 2009−
2012 |
2.9 | 1998−
2003 |
0.1 | 2003−
2010 |
3.1* | 1999−
2003 |
2.2 | 2003−
2012 |
5.7* | ||||||||||||
| Lung | 1998−
2012 |
−0.2 | 1998−
2005 |
0.5 | 2005−
2010 |
3.8* | 1999−
2003 |
−2.9* | 2003−
2012 |
2.4* | ||||||||||||||||
| Liver | 1998−
2012 |
−2.1* | 1998−
2010 |
−3.3* | 1999−
2012 |
−2.2* | ||||||||||||||||||||
| Stomach | 1998−
2012 |
−3.1* | 1998−
2003 |
−3.4* | 2003−
2010 |
0.4 | 1999−
2012 |
−0.4 | ||||||||||||||||||
| Esophagus | 1998−
2012 |
−6.1* | 1998−
2010 |
2.2* | 1999−
2012 |
−2.5* | ||||||||||||||||||||
| Colorectum | 1998−
2001 |
2.0 | 2001−
2012 |
−0.6* | 1998−
2010 |
1.1* | 1999−
2008 |
4.4* | 2008−
2012 |
1.5 | ||||||||||||||||
| Breast | 1998−
2000 |
8.3 | 2000−
2009 |
1.6* | 2009−
2012 |
4.5* | 1998−
2010 |
4.2* | 1999−
2012 |
5.7* | ||||||||||||||||
| Thyroid | 1998−
2003 |
3.7* | 2003−
2012 |
12.7* | 1998−
2002 |
−4.2* | 2002−
2006 |
11.2* | 2006−
2010 |
4.2 | 1999−
2009 |
23.8* | 2009−
2012 |
10.1 | ||||||||||||
3. Trends in age-standardized incidence rates by cancer site and gender (triangle for male; circle for female) in China (red), Japan (green), and South Korea (blue). The data used to generate this figure were from the Cancer Incidence in Five Continents database (15).
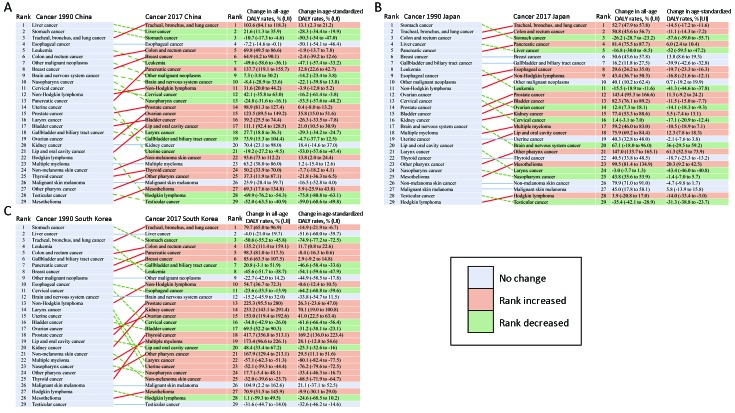
Figure 4A shows the DALYs of 29 cancer types in China, ranked by the number of DALYs in 2017. Lung cancer became the leading cause of DALYs in 2017, replacing liver cancer in 1990. All-age and age-standardized DALY rates of stomach cancer have decreased by 10.7% and 50.3% since 1990, leading to a decrease in its ranking from the second to the third. Esophageal cancer was still the fourth leading cancer for all-cause DALYs, even though the age-standardized DALY rate decreased by 50.1% over the last 27 years. Colorectal cancer and breast cancer both increased in the ranking to become the fifth and sixth leading cancers of all-age DALYs. The all-age DALYs rates increased for colorectal cancer (69.8%) and breast cancer (64.9%) from 1990 to 2017. The all-age and age-standardized DALY rates have increased substantially for pancreatic cancer, ovarian cancer, and lip and oral cavity cancer since 1990. Age-standardized DALY rate of uterine cancer declined by 53% over this period, leading it from 14th in 1990 to fall outside the top 20 causes in 2017.
4. Rank changes in disability-adjusted life years (DALYs) attributable to cancers and percentage change in all age and age-standardized DALY rates in China (A), Japan (B), and South Korea (C) from 1990 to 2017. The estimates used to generate this figure were from the Institute for Health Metrics and Evaluation (IHME) website (7). Age-standardized rates were calculated using the GBD reference population (18).
Comparison with Japan and South Korea in current burden
As estimated by the GLOBOCAN 2018, there was a marked variation in cancer incidence rates among China, Japan, and South Korea, with the incidence in Japan and South Korea being higher than that in China. Overall, the ASIR per 100,000 in South Korea observed among males (332.1) and females (310.6) were nearly 1.5 times higher than the rates among males (223.0) and females (182.6) in China. In contrast to incidence rates, mortality rates in China were nearly 1.5 times higher than those in Japan and South Korea within each sex.
Table 1 and Supplementary Table S1 show the top ten cancer types by the ASIR and ASMR for males, females, and combined in China, Japan, and South Korea. Lung cancer, stomach cancer, and colorectal cancer were listed in the top five common cancers for males in each country. For females, breast cancer, lung cancer, colorectal cancer, stomach cancer, and thyroid cancer were common cancers in the three countries. Figure 1 illustrates the ASIR and ASMR of selected types of cancers in China, Japan, and South Korea in 2018. South Korea had a much higher thyroid cancer incidence than Japan and China. Also, Japan and South Korea had higher incidence rates of breast, colorectal and prostate cancers than China. But the mortality rates of thyroid, breast, colorectal and prostate cancers were similar in these three countries. Another notable aspect was that China had a lower incidence rate but a higher mortality rate of stomach cancer than Japan and South Korea. Correspondingly, Table 4 indicates that Chinese cancer patients had lower 5-year survival rates. Especially for stomach cancer, the survival rate in South Korea has achieved 68.9% but its counterpart was less than 36% in China.
S1. Age-standardized cancer incidence and mortality rates per 100,000 populations by gender in Japan and South Korea in 2018.
| Country | Index | Gender | All cancers | Rank | |||||||||
| 1st | 2nd | 3rd | 4th | 5th | 6th | 7th | 8th | 9th | 10th | ||||
| NHL, non-Hodgkin lymphoma. The estimates are from Global Cancer Observatory 2018, IARC, 2018 (6). Age-standardized rates are calculated using the direct method and the world standard population. | |||||||||||||
| Japan | Incidence | Both | 248.0 | Breast | Colorectum | Prostate | Lung | Stomach | Corpus uteri | Cervix uteri | Pancreas | Ovary | Bladder |
| 57.6 | 38.9 | 35.4 | 27.5 | 27.5 | 15.1 | 14.7 | 9.7 | 9.5 | 8.7 | ||||
| Male | 285.9 | Colorectum | Lung | Stomach | Prostate | Bladder | Liver | Pancreas | Kidney | Esophagus | NHL | ||
| 49.1 | 41.4 | 40.7 | 35.4 | 15.1 | 12.3 | 11.7 | 11.2 | 9.3 | 8.7 | ||||
| Female | 220.5 | Breast | Colorectum | Stomach | Lung | Corpus uteri | Cervix uteri | Thyroid | Ovary | Pancreas | NHL | ||
| 57.6 | 29.6 | 16.0 | 15.6 | 15.1 | 14.7 | 11.2 | 9.5 | 7.7 | 6.1 | ||||
| Mortality | Both | 85.2 | Lung | Colorectum | Stomach | Breast | Pancreas | Liver | Prostate | Gallbladder | Ovary | Esophagus | |
| 16.2 | 12.0 | 9.5 | 9.3 | 7.8 | 5.4 | 4.4 | 3.3 | 3.3 | 2.8 | ||||
| Male | 111.9 | Lung | Colorectum | Stomach | Pancreas | Liver | Esophagus | Prostate | Gallbladder | NHL | Leukemia | ||
| 26.5 | 15.2 | 14.3 | 9.5 | 8.6 | 5.1 | 4.4 | 4.2 | 3.5 | 3.1 | ||||
| Female | 64.3 | Breast | Colorectum | Lung | Pancreas | Stomach | Ovary | Liver | Cervix uteri | Gallbladder | NHL | ||
| 9.3 | 9.2 | 7.8 | 6.2 | 5.6 | 3.3 | 2.7 | 2.7 | 2.5 | 1.9 | ||||
| South Korea | Incidence | Both | 313.5 | Thyroid | Breast | Colorectum | Stomach | Prostate | Lung | Liver | Cervix uteri | NHL | Kidney |
| 60.7 | 59.8 | 44.5 | 39.6 | 36.2 | 27.8 | 17.3 | 8.4 | 8.0 | 7.9 | ||||
| Male | 332.1 | Colorectum | Stomach | Lung | Prostate | Liver | Thyroid | Kidney | NHL | Pancreas | Gallbladder | ||
| 59.5 | 57.8 | 41.7 | 36.2 | 27.7 | 21.8 | 11.5 | 9.0 | 8.7 | 8.4 | ||||
| Female | 310.6 | Thyroid | Breast | Colorectum | Stomach | Lung | Cervix uteri | Liver | Corpus uteri | NHL | Ovary | ||
| 100.5 | 59.8 | 31.3 | 23.5 | 17.2 | 8.4 | 8.2 | 7.8 | 7.1 | 6.5 | ||||
| Mortality | Both | 80.7 | Lung | Liver | Colorectum | Stomach | Pancreas | Breast | Prostate | Gallbladder | Ovary | Leukemia | |
| 18.1 | 11.8 | 8.7 | 7.0 | 6.1 | 6.0 | 4.7 | 4.1 | 2.4 | 2.3 | ||||
| Male | 115.2 | Lung | Liver | Colorectum | Stomach | Pancreas | Gallbladder | Prostate | Esophagus | Leukemia | NHL | ||
| 31.4 | 19.5 | 11.8 | 10.0 | 7.6 | 5.0 | 4.7 | 3.3 | 3.0 | 2.8 | ||||
| Female | 55.0 | Lung | Colorectum | Breast | Liver | Pancreas | Stomach | Gallbladder | Ovary | Cervix uteri | Leukemia | ||
| 8.2 | 6.3 | 6.0 | 5.2 | 4.9 | 4.8 | 3.4 | 2.4 | 2.0 | 1.7 | ||||
4. Age-standardized 5-year survival rates (%) with 95% CI in adults aged 15−99 years from 2000 to 2014 in China, Japan, and South Korea.
| Country | Years | 5-year survival rate (95% CI) | |||||||||
| Lung | Stomach | Liver | Esophagus | Colon | Rectum | Breast | Pancreas | Prostate | Cervix uteri | ||
| 95% CI, 95% confidence interval. The estimates are from the CONCORD-3 (8). Age-standardized rates are calculated using the International Cancer Survival Standard weights (16). | |||||||||||
| China | 2000−2004 | 18.7 (18.0−19.4) | 30.2 (29.3−31.1) | 11.7 (10.9−12.5) | 22.9 (22.0−23.9) | 51.4 (49.6−53.3) | 49.5 (47.5−51.4) | 75.9 (70.9−80.9) | 14.4 (12.8−16.0) | 57.7 (52.3−63.0) | 53.3 (48.1−58.5) |
| 2005−2009 | 17.7 (17.4−18.1) | 33.2 (32.7−33.7) | 11.6 (11.1−12.0) | 27.1 (26.5−27.7) | 55.6 (54.6−56.5) | 52.5 (51.5−53.6) | 80.4 (79.3−81.5) | 10.2 (9.4−11.0) | 62.5 (59.9−65.1) | 63.0 (61.2−64.9) | |
| 2010−2014 | 19.8 (19.4−20.2) | 35.9 (35.3−36.5) | 14.1 (13.6−14.7) | 29.7 (29.0−30.4) | 57.6 (56.6−58.6) | 56.9 (55.8−58.0) | 83.2 (82.1−84.3) | 9.9 (9.1−10.7) | 69.2 (66.4−72.0) | 67.6 (65.8−69.5) | |
| Japan | 2000−2004 | 29.3 (28.1−30.5) | 50.5 (50.0−50.9) | 25.7 (25.1−26.3) | 27.7 (26.4−29.0) | 63.4 (62.7−64.0) | 58.6 (57.6−59.5) | 85.9 (85.2−86.6) | 6.9 (6.4−7.4) | 85.9 (84.9−87.0) | 67.5 (66.3−68.7) |
| 2005−2009 | 29.3 (28.9−29.7) | 57.6 (57.3−57.9) | 28.6 (28.1−29.1) | 33.3 (32.3−34.2) | 66.8 (66.3−67.3) | 64 (63.3−64.6) | 88.9 (88.4−89.3) | 7.6 (7.2−7.9) | 91.4 (90.8−92.0) | 69.2 (68.3−70.1) | |
| 2010−2014 | 32.9 (32.3−33.4) | 60.3 (59.9−60.7) | 30.1 (29.5−30.6) | 36.0 (34.8−37.3) | 67.8 (67.3−68.4) | 64.8 (64.0−65.7) | 89.4 (88.9−89.9) | 8.3 (7.8−8.7) | 93.0 (92.4−93.6) | 71.4 (70.4−72.3) | |
| South Korea | 2000−2004 | 15.3 (15.0−15.6) | 48.6 (48.2−48.9) | 15.3 (15.0−15.7) | 18.6 (17.6−19.6) | 60.5 (59.9−61.2) | 60.8 (60.0−61.6) | 79.5 (78.0−81.0) | 7.6 (7.2−8.1) | 76.0 (74.6−77.5) | 76.0 (75.3−76.7) |
| 2005−2009 | 19.9 (19.6−20.2) | 61.1 (60.8−61.5) | 22.4 (22.1−22.8) | 26.9 (25.8−28.0) | 68.1 (67.6−68.6) | 68.1 (67.5−68.7) | 84.0 (83.0−85.0) | 8.4 (8.0−8.9) | 87.3 (86.5−88.1) | 77.0 (76.4−77.7) | |
| 2010−2014 | 25.1 (24.8−25.4) | 68.9 (68.6−69.2) | 27.2 (26.8−27.6) | 31.3 (30.3−32.4) | 71.8 (71.4−72.2) | 71.1 (70.6−71.7) | 86.6 (85.8−87.5) | 10.5 (10.0−10.9) | 89.9 (89.2−90.5) | 77.3 (76.6−78.0) | |
Supplementary Table S2 shows all age and age-standardized DALYs rates in Japan and South Korea in 2017. Age-standardized DALY per 100,000 populations for all cancers was higher in China when compared with Japan and South Korea. Figure 2 shows DALYs per 100,000 populations by age and gender in China, Japan, and South Korea in 2017. Evaluating DALYs by age, we could see that the population with the highest rates of cancer burden in China were younger than those in Japan and South Korea. Lung cancer represented the highest cancer burden for the three countries, followed by gastrointestinal and liver cancers. In terms of the composition of DALYs by age and sex, leukemia was the highest DALY group among the youth in the three countries, followed by brain and nervous system cancer. For young and middle-aged adult males, the largest contributors to DALYs were liver cancer in China and South Korea and colorectal cancer in Japan, respectively. Breast cancer was the leading cause of DALY among young and middle-aged adult females in the three countries. Among elderly adults (>50 years) in the three countries, lung cancer was the top contributor to cancer burden for males, females, and combined, except being replaced with colorectal cancer in Japanese females.
S2. All age and age-standardized DALYs rates per 100,000 populations by gender in Japan and South Korea in 2017.
| Country | Index | Gender | All cancers | Rank | |||||||||
| 1st | 2nd | 3rd | 4th | 5th | 6th | 7th | 8th | 9th | 10th | ||||
| DALYs, disability-adjusted life years; CNS, central nervous system; NHL, non-Hodgkin lymphoma; Other, other malignant neoplasms; Gallbladder, gallbladder and biliary tract. The estimates are from the Institute for Health Metrics and Evaluation (IHME) website (7). Age-standardized rates are calculated using the GBD reference population (18). | |||||||||||||
| Japan | All age rates | Both | 5,123.6 | Lung | Colorectum | Stomach | Pancreas | Liver | Breast | Gallbladder | Esophagus | Other | Prostate |
| 933.5 | 709.5 | 656.0 | 411.9 | 386.8 | 275.6 | 222.4 | 177.2 | 167.3 | 165.3 | ||||
| Male | 6,404.7 | Lung | Stomach | Colorectum | Liver | Pancreas | Prostate | Esophagus | Gallbladder | Other | NHL | ||
| 1,400.2 | 936.8 | 859.3 | 562.2 | 472.1 | 339.2 | 312.4 | 252.8 | 197.0 | 191.0 | ||||
| Female | 3,906.3 | Colorectum | Breast | Lung | Stomach | Pancreas | Liver | Gallbladder | Ovarian | Other | Cervix | ||
| 567.2 | 534.0 | 490.1 | 389.1 | 354.7 | 220.2 | 193.6 | 171.3 | 139.2 | 137.6 | ||||
| Age-standardized rates | Both | 2,285.5 | Lung | Colorectum | Stomach | Pancreas | Liver | Breast | Other | Leukemia | Gallbladder | Esophagus | |
| 372.7 | 303.9 | 275.3 | 172.2 | 158.6 | 155.4 | 106.7 | 93.0 | 82.5 | 77.8 | ||||
| Male | 2,907.5 | Lung | Stomach | Colorectum | Liver | Pancreas | Esophagus | Other | Prostate | Leukemia | Gallbladder | ||
| 590.2 | 409.1 | 391.8 | 250.4 | 213.5 | 141.1 | 125.9 | 125.5 | 112.1 | 104.4 | ||||
| Female | 1,768.6 | Breast | Colorectum | Lung | Stomach | Pancreas | Ovarian | Other | Cervix | Liver | Leukemia | ||
| 303.8 | 225.9 | 186.5 | 160.6 | 133.9 | 98.5 | 89.6 | 85.1 | 75.3 | 75.1 | ||||
| South Korea | All age rates | Both | 3,727.0 | Lung | Liver | Stomach | Colorectum | Pancreas | Breast | Gallbladder | Leukemia | Other | NHL |
| 689.1 | 605.7 | 473.6 | 388.8 | 227.5 | 201.7 | 165.9 | 116.3 | 106.0 | 90.8 | ||||
| Male | 4,728.6 | Lung | Liver | Stomach | Colorectum | Pancreas | Gallbladder | Prostate | Leukemia | Esophagus | Other | ||
| 1,002.3 | 954.8 | 659.8 | 480.0 | 264.0 | 188.8 | 166.9 | 136.3 | 136.1 | 119.7 | ||||
| Female | 2,710.2 | Breast | Lung | Colorectum | Stomach | Liver | Pancreas | Gallbladder | Ovarian | Cervix | Leukemia | ||
| 404.0 | 371.2 | 296.2 | 284.7 | 251.3 | 190.5 | 142.6 | 112.2 | 109.2 | 95.9 | ||||
| Age-standardized rates | Both | 2,386.1 | Lung | Liver | Stomach | Colorectum | Pancreas | Breast | Gallbladder | Leukemia | Other | Brain, CNS | |
| 421.7 | 371.5 | 297.4 | 242.1 | 139.2 | 128.4 | 102.1 | 101.2 | 83.6 | 65.4 | ||||
| Male | 3,269.5 | Lung | Liver | Stomach | Colorectum | Pancreas | Gallbladder | Prostate | Leukemia | Other | Esophagus | ||
| 688.5 | 614.9 | 444.8 | 329.0 | 174.9 | 130.9 | 128.3 | 121.4 | 97.6 | 89.5 | ||||
| Female | 1,669.7 | Breast | Lung | Stomach | Colorectum | Liver | Pancreas | Leukemia | Gallbladder | Other | Cervix | ||
| 250.1 | 210.6 | 175.1 | 170.8 | 145.2 | 107.3 | 81.9 | 78.8 | 71.2 | 69.9 | ||||
| 451.8 | 253.0 | 251.6 | 235.5 | 168.9 | 146.6 | 132.3 | 117.9 | 107.6 | 102.3 | ||||
Comparison with Japan and South Korea in time trends
Figure 3 shows trends in ASIR by cancer site and gender in China, Japan, and South Korea. In contrast to China, upward trends of ASIR in Japan and South Korea were observed. Rising prostate and female breast cancers contributed the greatest part to the increase of all cancers incidence rates. Lung cancer incidence rate remained generally high in China, Japan, and South Korea. Lung cancer jumped to the first cause of DALYs in 2017, replacing live cancer in China, stomach cancer in Japan and South Korea (Figure 4 ). But Table 3 indicates that the ASIR of lung cancer decreased constantly among males in South Korea. Table 4 shows the age-standardized 5-year cancer survival rates in China, Japan, and South Korea from 2000 to 2014. Survival trends were generally increasing in common types of cancers in the three countries, except for the pancreas cancer survival rate in China.
China, Japan, and South Korea experienced significant downward trends in ASIR and DALYs for liver cancer. As for stomach cancer, declining incidence was also observed in China and Japan, and the incidence decreased but not statistically significant in South Korea (Table 3 ). For Japan and South Korea, stomach cancer declined from being the leading cause of all-age DALYs in 1990 to the third in 2017 (Figure 4B ,C ). The trend analysis indicated that the incidence of esophageal cancer decreased in China and South Korea but increased in Japan. The burden of colorectal cancer in China, Japan, and South Korea has increased over the past several decades. In regard with prostate and thyroid cancers, a constantly growing burden was observed in China, Japan, and South Korea. Besides, there was an alarming trend to increase in breast cancer incidence rates in the three countries.
Discussion
In this study, we performed a comprehensive epidemiological analysis of cancer burden and trends in China and compared the differences between China, Japan and South Korea using high-quality data. We found that China was faced with a rising burden of colorectal, prostate, and breast cancers as well as a heavy burden of lung and upper digestive tract cancers. Compared with Japan and South Korea, China has higher ASMR and DALY rates.
China had a higher ASMR and a relatively lower ASIR for all cancers than Japan and South Korea. Several reasons could explain the seemingly paradoxical situation. Firstly, the significant difference in the composition of incident cancers could result in the higher mortality rate in China. The most common incident cancer was lung cancer in China rather than colorectal cancer, which ranked first for ASIR in Japan and South Korea. The ASIR of lung cancer with a poor prognosis, was higher in China (35.1 per 100,000) than that in Japan (27.5 per 100,000) and South Korea (27.8 per 100,000). In addition, prostate cancer with a low fatality rate ranked fourth in Japanese males and South Korean males, while it fell outside the first five common cancers for ASIR in Chinese males. Secondly, China had lower survival rates of thyroid, breast, colorectal, prostate and stomach cancers. One possible explanation is that higher screening uptake rates in Japan and South Korea may drive the inflation of cancer incidence rates and promote the early detection (4,20). For example, endoscopic screening performed in Japan and South Korea (20,21) may bring about the higher survival rates of stomach cancer. Poor access to cancer care in China also could result in the disparities (4).
Concerning the time trends, similar to previous studies (22,23), we found that China, Japan, and South Korea experienced significant downward trends in the burden of liver and stomach cancers. This trend has been explained by a series of lifestyle changes and public health interventions. For example, the spread of hepatitis B virus vaccination (5,24) and reduced aflatoxin exposure (25) are thought to have contributed to the reduction of liver cancer in China. In Japan, it might be associated with the reduced hepatitis C virus infection (26,27). But the increasing prevalence of obesity and diabetes presents a threat to the favorable trend (28). For stomach cancer, the decreasing prevalence of Helicobacter pylori infection, improved living conditions, and better food preservation practices lead to the declining rates (29). Similar to our analysis, an updated analysis from the National Cancer Center of Japan reported an increase of age-standardized esophageal cancer incidence. But the declining mortality was observed (11). Reasons for this divergent trend have yet to be identified. Endoscopic screening conducted in Japan may have an influence.
Another notable sign for optimism is that lung cancer incidence for males in South Korea has been decreasing constantly in recent years, which reflects a corresponding decline in the smoking prevalence in South Korea. Smoking prevalence among South Korean males dropped from 71.7% in 1992 to 39.7% in 2016 (30). Tobacco control can prevent lung cancer effectively. Nevertheless, though some progress in tobacco control has been made (31,32), China still faces high smoking rates. The National Health Service Survey conducted in 2013 found that more than 45% of Chinese males are current smokers (33). Also, faltering tobacco control policies is criticized in Japan (34). South Korea serves as an example of tobacco control to China and Japan (35). Stronger tobacco control is urgently needed such as increasing tobacco excise taxes and introducing a national smoke-free law.
In our analysis, colorectal, prostate and breast cancers tended to be more common in China, Japan, and South Korea. But according to the latest data from national cancer registries, colorectal cancer incidence and mortality have shown signs of declining in Japan and South Korea (11,12,36). The long-standing national screening programs may have an impact (37-39). Another notable aspect is that Japan and South Korea set up institutions responsible for providing comprehensive cancer information to enhance public awareness (40,41). The rapid rise of prostate cancer incidence could be explained by the widespread prostate-specific antigen testing. Besides, prostate cancer incidence and mortality in Japan and South Korea has seemingly plateaued in recent years (11,36). The rapidly increasing incidence of thyroid cancer in South Korea (42) sounded the alarm that screening also has the potential to promote overdiagnosis. Limited knowledge could explain the rapid increase in female breast cancer. This trend may reflect a collaboration of changed environmental factors, including the delay of childbearing, increases in the levels of obesity, and the spread of breast cancer screening (3).
Our work has several limitations. First, the comparison of estimates in different countries might be compromised because of variations in data collection and reporting systems across countries. Second, our trend analysis was only based on several registries due to insufficient data availability. The observed trends may not represent national profiles. Moreover, trends in the recent ten years could not be evaluated owing to unavailable up-to-date data. It is required to update the analysis based on more contemporary data and use more compressive analysis such as age-period-cohort analysis.
Conclusions
At the transition cancer stage, China still had a heavy burden of lung and upper digestive tract cancers and faced a rising burden of colorectal, prostate, and breast cancers. China, Japan, and South Korea shared similar cancer profiles and time trends. Although the strategies established in Japan and South Korea should be adapted to the specific contexts of China, we could draw some useful lessons. Compared with Japan and South Korea, China had higher age-standardized cancer mortality and DALY rates but lower incidence. Relatively lower mortality and favorable trends of colorectal and lung cancers appeared in Japan or South Korea indicated the effectiveness of screening and tobacco control. Improvement in the current tobacco control policy and cancer screening systems may contribute to cancer control in China. Also, given huge geographic disparities in cancer burden across China, evidence-based approaches are needed for cancer control programs, and tailored to local profile and population risk.
Acknowledgements
This study was supported by the National Key R&D Program of China (No. 2018YFC1313100); Sanming Project of Medicine in Shenzhen (No. SZSM201911015); CAMS Innovation Fund for Medical Sciences (CIFMS) (No.2016-I2M-2-004).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.World Health Organization. Global Health Observatory. 2020. Geneva. Available online: https://www.who.int/data/gho
- 2.Zheng R, Gu X, Li X, et al Analysis on the trend of cancer incidence and age change in cancer registry areas of China, 2000 to 2014. Zhonghua Yu Fang Yi Xue Za Zhi. 2018;52:593–600. doi: 10.3760/cma.j.issn.0253-9624.2018.06.007. [DOI] [PubMed] [Google Scholar]
- 3.Bray F, Ferlay J, Soerjomataram I, et al Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 4.Goss PE, Strasser-Weippl K, Lee-Bychkovsky BL, et al Challenges to effective cancer control in China, India, and Russia. Lancet Oncol. 2014;15:489–538. doi: 10.1016/S1470-2045(14)70029-4. [DOI] [PubMed] [Google Scholar]
- 5.Jun JK, Yoo K-Y. National Cancer Control in Korea. In: Withers M, McCool J, eds. Global Health Leadership: Case Studies From the Asia-Pacific. Cham: Springer International Publishing, 2019.
- 6.Ferlay J, Ervik M, Lam F, et al. Global Cancer Observatory: Cancer Today. 2018. Lyon, France. Available online: https://gco.iarc.fr/today
- 7.Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2017(GBD 2017) Results. 2018. Available online: http://ghdx.healthdata.org/gbd-results-tool
- 8.Allemani C, Matsuda T, Di Carlo V, et al Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391:1023–75. doi: 10.1016/S0140-6736(17)33326-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen W, Zheng R, Baade PD, et al Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115–32. doi: 10.3322/caac.21338. [DOI] [PubMed] [Google Scholar]
- 10.Zheng RS, Sun KX, Zhang SW, et al Report of cancer epidemiology in China, 2015. Zhonghua Zhong Liu Za Zhi. 2019;41:19–28. doi: 10.3760/cma.j.issn.0253-3766.2019.01.005. [DOI] [PubMed] [Google Scholar]
- 11.Katanoda K, Hori M, Matsuda T, et al An updated report on the trends in cancer incidence and mortality in Japan, 1958-2013. Jpn J Clin Oncol. 2015;45:390–401. doi: 10.1093/jjco/hyv002. [DOI] [PubMed] [Google Scholar]
- 12.Center for Cancer Control and Information Services. Cancer Statistics in Japan. 2019. Available online: https://ganjoho.jp/en/professional/statistics/table_download.html
- 13.Ministry of Health and Welfare. Cancer Registration Statistics. 2020. Available online: http://kosis.kr/eng/
- 14.Ferlay J, Colombet M, Soerjomataram I, et al Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 2019;144:1941–53. doi: 10.1002/ijc.31937. [DOI] [PubMed] [Google Scholar]
- 15.Ferlay J, Colombet M, Bray F. Cancer Incidence in Five Continents, CI5plus: IARC CancerBase No. 9. 2018. Lyon, France. Available online: http://ci5.iarc.fr
- 16.Corazziari I, Quinn M, Capocaccia R Standard cancer patient population for age standardising survival ratios. Eur J Cancer. 2004;40:2307–16. doi: 10.1016/j.ejca.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 17.GBD 2017 DALYs and HALE Collaborators Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1859–22. doi: 10.1016/S0140-6736(18)32335-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.GBD 2017 Mortality Collaborators Global, regional, and national age-sex-specific mortality and life expectancy, 1950-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1684–735. doi: 10.1016/S0140-6736(18)31891-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim HJ, Fay MP, Feuer EJ, et al Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19:335–51. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 20.Suh M, Song S, Cho HN, et al Trends in Participation Rates for the National Cancer Screening Program in Korea, 2002-2012. Cancer Res Treat. 2017;49:798–806. doi: 10.4143/crt.2016.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Asaka M, Kato M, Sakamoto N Roadmap to eliminate gastric cancer with Helicobacter pylori eradication and consecutive surveillance in Japan. J Gastroenterol. 2014;49:1–8. doi: 10.1007/s00535-013-0897-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu J, Yang S, Xu K, et al Patterns and Trends of Liver Cancer Incidence Rates in Eastern and Southeastern Asian Countries (1983-2007) and Predictions to 2030. Gastroenterology. 2018;154:1719–28. doi: 10.1053/j.gastro.2018.01.033. [DOI] [PubMed] [Google Scholar]
- 23.Arnold M, Park JY, Camargo MC, et al. Is gastric cancer becoming a rare disease? A global assessment of predicted incidence trends to 2035. Gut 2020 Jan 30. [Epub ahead of print]
- 24.Tanaka M, Katayama F, Kato H, et al Hepatitis B and C virus infection and hepatocellular carcinoma in China: a review of epidemiology and control measures. J Epidemiol. 2011;21:401–16. doi: 10.2188/jea.je20100190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sun Z, Chen T, Thorgeirsson SS, et al Dramatic reduction of liver cancer incidence in young adults: 28 year follow-up of etiological interventions in an endemic area of China. Carcinogenesis. 2013;34:1800–5. doi: 10.1093/carcin/bgt007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tanaka J, Akita T, Ohisa M, et al Trends in the total numbers of HBV and HCV carriers in Japan from 2000 to 2011. J Viral Hepat. 2018;25:363–72. doi: 10.1111/jvh.12828. [DOI] [PubMed] [Google Scholar]
- 27.Park JW, Chen M, Colombo M, et al Global patterns of hepatocellular carcinoma management from diagnosis to death: the BRIDGE Study. Liver Int. 2015;35:2155–66. doi: 10.1111/liv.12818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Valery PC, Laversanne M, Clark PJ, et al Projections of primary liver cancer to 2030 in 30 countries worldwide. Hepatology. 2018;67:600–11. doi: 10.1002/hep.29498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hooi JKY, Lai WY, Ng WK, et al Global Prevalence of Helicobacter pylori Infection: Systematic Review and Meta-Analysis. Gastroenterology. 2017;153:420–9. doi: 10.1053/j.gastro.2017.04.022. [DOI] [PubMed] [Google Scholar]
- 30.Chang Y, Kang HY, Lim D, et al Long-term trends in smoking prevalence and its socioeconomic inequalities in Korea, 1992-2016. Int J Equity Health. 2019;18:148. doi: 10.1186/s12939-019-1051-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lin H, Chang C, Liu Z, et al Subnational smoke-free laws in China. Tob Induc Dis. 2019;17:78. doi: 10.18332/tid/112665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li X, Galea G Healthy China 2030: an opportunity for tobacco control. Lancet. 2019;394:1123–5. doi: 10.1016/S0140-6736(19)32048-3. [DOI] [PubMed] [Google Scholar]
- 33.Wang M, Luo X, Xu S, et al Trends in smoking prevalence and implication for chronic diseases in China: serial national cross-sectional surveys from 2003 to 2013. Lancet Respir Med. 2019;7:35–45. doi: 10.1016/S2213-2600(18)30432-6. [DOI] [PubMed] [Google Scholar]
- 34.Sobue T ED12.05 Tobacco Control Policies in Japan. J Thorac Oncol. 2017;12:S54–S56. doi: 10.1016/j.jtho.2016.11.048. [DOI] [Google Scholar]
- 35.Levy DT, Cho SI, Kim YM, et al SimSmoke model evaluation of the effect of tobacco control policies in Korea: the unknown success story. Am J Public Health. 2010;100:1267–73. doi: 10.2105/AJPH.2009.166900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jung KW, Won YJ, Kong HJ, et al Cancer Statistics in Korea: Incidence, Mortality, Survival, and Prevalence in 2016. Cancer Res Treat. 2019;51:417–30. doi: 10.4143/crt.2019.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Keum N, Giovannucci E Global burden of colorectal cancer: emerging trends, risk factors and prevention strategies. Nat Rev Gastroenterol Hepatol. 2019;16:713–32. doi: 10.1038/s41575-019-0189-8. [DOI] [PubMed] [Google Scholar]
- 38.Schreuders EH, Ruco A, Rabeneck L, et al Colorectal cancer screening: a global overview of existing programmes. Gut. 2015;64:1637–49. doi: 10.1136/gutjnl-2014-309086. [DOI] [PubMed] [Google Scholar]
- 39.Arnold M, Sierra MS, Laversanne M, et al Global patterns and trends in colorectal cancer incidence and mortality. Gut. 2017;66:683. doi: 10.1136/gutjnl-2015-310912. [DOI] [PubMed] [Google Scholar]
- 40.Kye SY, Lee MH, Yoo J, et al Factors affecting satisfaction with cancer information provided through the social networking services of the National Cancer Information Center in Korea. Epidemiol Health. 2017;39:e2017057. doi: 10.4178/epih.e2017057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Okuhara T, Ishikawa H, Urakubo A, et al Cancer information needs according to cancer type: A content analysis of data from Japan’s largest cancer information website. Prev Med Rep. 2018;12:245–52. doi: 10.1016/j.pmedr.2018.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ahn HS, Kim HJ, Welch HG Korea’s thyroid-cancer “epidemic” — screening and overdiagnosis. N Engl J Med. 2014;371:1765–7. doi: 10.1056/NEJMp1409841. [DOI] [PubMed] [Google Scholar]