Abstract
Introduction:
Susceptibility, or openness to smoking, is a predictor of future smoking. This study examines within-gender racial/ethnic differences in smoking susceptibility over historical time (1999–2018) and developmental age (11–18 years).
Methods:
Data were from 205,056 adolescent never smokers in 14 waves of the National Youth Tobacco Survey. Weighted time-varying effect models were used to estimate nonlinear trends in smoking susceptibility among minority (versus white) adolescents. Analyses were conducted in 2019.
Results:
Compared with whites, Latino/a adolescents were consistently more susceptible to smoking, whereas black and Asian adolescents fluctuated between being less and equally susceptible over time. American Indian, Alaska Native, Native Hawaiian, and Pacific Islander adolescents were more susceptible from 2014 to 2017, with differences being larger for girls. Susceptibility peaked at age 14 years. Compared with whites, Latino/a adolescents were more susceptible throughout adolescence. Black adolescents were more susceptible in early adolescence, whereas Asian adolescents were less or equally susceptible to smoking in early to mid-adolescence. American Indian, Alaska Native, Native Hawaiian, and Pacific Islander girls were more susceptible in early and mid-adolescence, but boys were more susceptible in early adolescence only. American Indian, Alaska Native, Native Hawaiian, and Pacific Islander girls were less susceptible than white girls at age 18 years.
Conclusions:
Twenty-year racial/ethnic differences in smoking susceptibility were evident, particularly among girls, but were mostly equivalent between genders over developmental age. Targeting susceptible adolescents with gender-, race/ethnic-, and age-tailored prevention efforts may prevent or delay adolescents’ transition to tobacco use and reduce tobacco-related disparities.
INTRODUCTION
Adolescence is a developmental period critical to smoking susceptibility and initiation.1,2 Susceptibility, or openness to the idea of smoking, is a predictor of future daily smoking.3 Although current smoking among adolescents in the U.S. has decreased in the past 20 years,4 less is known about national rates and trends in smoking susceptibility among never smokers. Given differences in smoking rates by race/ethnicity, gender, and age, research into their association with smoking susceptibility is needed to inform prevention efforts and reduce smoking initiation.1
Between 2014 and 2017, national rates of current smoking were highest among American Indian/Alaska Native (AI/AN) (10.3%) and Native Hawaiian/Pacific Islander (NHPI) (9.5%) adolescents in Grades 6–12.5 Multiracial (6.6%) and white (6.6%) adolescents had the next highest rates, followed by Latino/a (5.7%), black (3.3%), and Asian (2.0%) adolescents.5 Notably, ever use is substantially higher across racial/ethnic groups, ranging from 10.3% among Asian adolescents to 31.4% among AI/AN adolescents.5 In contrast to current use, Latino/a and multiracial adolescents are more likely to have ever smoked than white adolescents.5 Racial/ethnic differences in smoking are also apparent between boys and girls. Generally, boys are more likely to be current smokers, except for Asian and AI/AN boys who are equally likely to be current smokers as girls.5 Of interest is whether noted racial/ethnic and gender differences in current cigarette use are present for smoking susceptibility.
Recent research using the National Youth Tobacco Survey (NYTS) showed racial/ethnic differences in smoking susceptibility.6 Latino/a adolescents were consistently more susceptible to smoking than white adolescents from 1999 to 2014. Conversely, black, Asian, and AI/AN/NHPI adolescents, who were historically less or equally susceptible to white adolescents, became equally or more susceptible starting between 2010 and 2012. Further, smoking susceptibility among girls tends to be equal to or higher than among boys,7,8 potentially attributable to gender-specific risk (e.g., exposure to targeted cigarette advertisements)9 and protective (e.g., parent–child communication)10 factors. Lack of evidence on within-gender racial/ethnic differences in smoking susceptibility may obscure the extent to which specific groups are at risk.11,12
Beyond overall within-gender racial/ethnic differences in smoking susceptibility, understanding the developmental periods in which girls and boys are most susceptible is paramount. During early adolescence, age 10–13 years,13 black and AI/AN/NHPI adolescents are more susceptible to smoking than white adolescents, whereas Asian adolescents are less susceptible.6 Conversely, Latino/a adolescents are more susceptible to smoking than white adolescents throughout adolescence. Stratifying these results by gender can inform optimal delivery times for smoking prevention programs and elucidate pathways to adult smoking among racial/ethnic minority girls and boys.
Building on previous research,6 this study examines gender-stratified racial/ethnic differences in smoking susceptibility over time (1999–2018) and developmental age (11–18 years), providing updated trends in smoking susceptibility beyond 2014 using nationally representative data. Given gender differences in smoking prevalence and smoking susceptibility, it is hypothesized that racial/ethnic disparities in smoking susceptibility will vary by gender. To better target smoking prevention interventions across developmental age, it is necessary to understand gender-specific racial/ethnic disparities in smoking susceptibility.
METHODS
Study Sample
Analyses included data from 14 waves of the publicly available NYTS between 1999 and 2018. NYTS is a nationally representative, cross-sectional, self-report paper survey administered to U.S. middle and high school students to gauge their tobacco-related beliefs, attitudes, and behaviors.14 NYTS is based on a stratified, multistage cluster sample design. Analyses included respondents who reported they never tried cigarettes, even one or two puffs (i.e., never smokers) and were deemed susceptible to smoking based on at least one of three smoking susceptibility questions or were deemed non-susceptible based on all three questions (N=205,056). Ever and current smokers were excluded because they had transitioned out of smoking susceptibility phase of smoking onset3 (Appendix Table 1). Data analysis was conducted in 2019.
Measures
Three questions captured smoking susceptibility: (1) Do you think you will try a cigarette soon? (2) Do you think you will smoke a cigarette in the next year? and (3) If one of your friends were to offer you a cigarette, would you smoke it? Responses to Question 1, from 1999 to 2011, were yes and no. Responses to Question 1 from 2012 to 2018 and to Questions 2 and 3 from 1999 to 2018 were definitely yes, probably yes, probably no, and definitely no. To harmonize response choices, definitely yes, probably yes, and probably no were recoded as yes; definitely no was coded as no.3 Participants who responded no to all three smoking susceptibility questions were considered non-susceptible to smoking, whereas those who responded yes to any of the three questions were considered susceptible to smoking.3
Data on sex, grade, race/ethnicity, and living with a cigarette user were collected. Although NYTS includes self-reported sex, as is common in adolescent health surveys,15 we use the term gender because susceptibility to smoking is more psychological and sociological than biological. From 1999 to 2009, living with a cigarette user was a yes/no question (Does anyone who lives with you now smoke cigarettes?). From 2011 to 2018, participants could report living with cigarette or non-cigarette tobacco product users. Living with cigarette users was coded as yes, and all others as no. Weighted sample characteristics appear in Appendix Tables 2 and 3.
Statistical Analysis
Weighted time-varying effect modeling (TVEM)16 was used to examine within-gender racial/ethnic differences in smoking susceptibility over time (1999–2018) and age (11–18 years) in SAS, version 9.4. TVEM estimates time-varying regression coefficients where a race/ethnicity binary time-varying coefficient represents the odds of being susceptible to smoking with no assumptions of linearity.16 The updated WeightedTVEM macro, not available for the previous publication,6 accommodates complex sampling designs, producing nationally representative estimates of smoking susceptibility.
Within-gender adjusted time-varying ORs of smoking susceptibility of each racial/ethnic group compared to white adolescents are presented.17
Grade and living with a cigarette user were used as time-varying covariates in within-gender racial/ethnic models of smoking susceptibility over historical time.18,19 For age models, survey year was also included as a covariate and grade was excluded because of its high correlation with age (Point Biserial r =0.82).20 Further, age analyses excluded participants aged 9–10 and 19–21 years because of low frequencies (excluded unweighted n=1,220).
As TVEM generates many regression coefficients, results are plotted in curves where significance is evident if a logistic regression curve and its CIs do not cross the non-significance line for the reference group (i.e., white girls/boys). Highest and lowest AORs of smoking susceptibility over time and age are highlighted. TVEM uses listwise deletion. However, weighted missingness was <4% for all variables. Thus, missingness was not expected to impact the results.
RESULTS
Smoking susceptibility among girls was 20%–23% between 1999 and 2011, then increased to 27%–29% between 2014 and 2018 (Appendix Tables 2 and 3). Compared with white girls, Latina girls between 2002 and 2018 (highest AOR=1.81 in 2015) (Figure 1, Panel A) and AI/AN/NHPI girls between 2001 and 2004 (highest AOR=1.62 in 2001) and between 2012 and 2017 (highest AOR=1.76 in 2015) (Figure 1, Panel D) were more susceptible to smoking. Conversely, black girls were less susceptible to smoking between 2001 and 2011 (lowest AOR=0.77 in 2004) and between 2017 and 2018 (lowest AOR=0.71 in 2018) (Figure 1, Panel B, whereas Asian girls were less susceptible to smoking between 2003 and 2009 (lowest AOR=0.74 in 2005) and between 2015 and 2018 (lowest AOR=0.79 in 2018) (Figure 1, Panel C).
Figure 1.
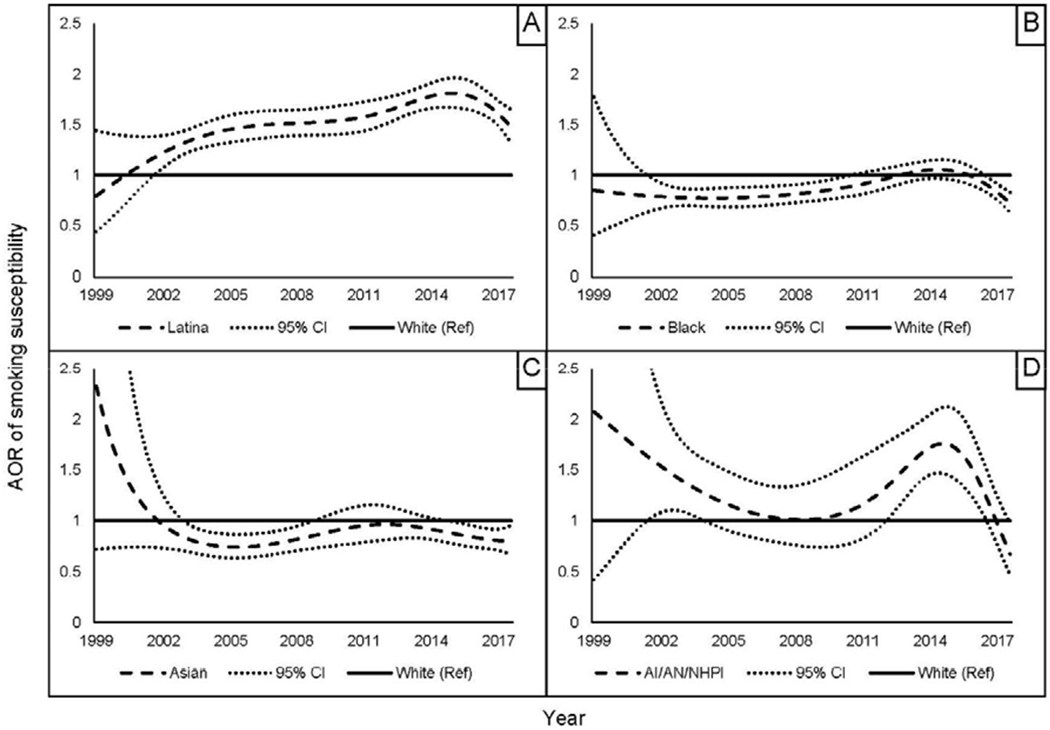
AOR of smoking susceptibility among racial/ethnic minority girls vs white girls over time (1999–2018).
Notes: Panel A: Latina girls vs white girls; Panel B: black girls vs white girls; Panel C: Asian girls vs white girls; Panel D: AI/AN/NHPI girls vs white girls. Models adjusted for grade level and living with a smoker.
AI/AN/NHPI, American Indian, Alaska Native, Native Hawaiian, and Pacific Islander.
Proportions of boys susceptible to smoking were 20%–23% between 1999 and 2011 then increased to 27%–31% between 2014 and 2018 (Appendix Tables 2 and 3). Compared with white boys, Latino boys between 2002 and 2018 (highest AOR=1.42 in 2013) (Figure 2, Panel A), and AI/AN/NHPI boys between 2014 and 2017 (highest AOR=1.34 in 2016) (Figure 2, Panel Dwere more susceptible to smoking. Black boys were less susceptible to smoking between 2002 and 2009 (lowest AOR=0.80 in 2005) and between 2015 and 2018 (lowest AOR=0.78 in 2018) (Figure 2, Panel B). Asian boys were less susceptible to smoking between 2006 and 2010 (lowest AOR=0.82 in 2008) and between 2017 and 2018 (lowest AOR=0.79 in 2018) (Figure 2, Panel C).
Figure 2.
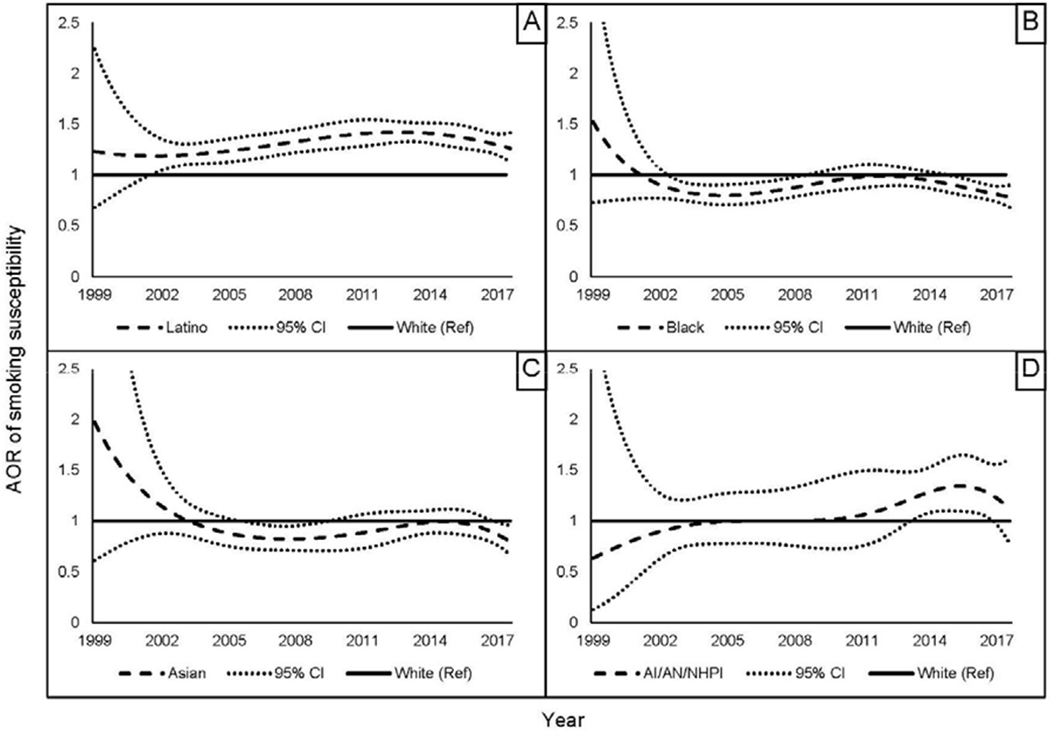
AOR of smoking susceptibility among racial/ethnic minority boys vs white boys over time (1999–2018).
Notes: Panel A: Latino boys vs white boys; Panel B: Black boys vs white boys; Panel C: Asian boys vs white boys; Panel D: AI/AN/NHPI boys vs white boys. Models adjusted for grade level and living with a smoker.
AI/AN/NHPI, American Indian, Alaska Native, Native Hawaiian, and Pacific Islander.
Among adolescents 11 to 18 years, girls’ susceptibility peaked at age 14 years, with 30% susceptible to smoking (Appendix Table 4). Compared with white girls, Latina girls were more susceptible to smoking between ages 11 and 18 years (highest AOR=2.02 at age 12 years) (Figure 3, Panel A). Black girls were more susceptible to smoking between ages 11 and 13 years (highest AOR=1.74 at age 11 years) but were less susceptible between ages 14 and 18 years (lowest AOR=0.59 at age 17 years) (Figure 3, Panel B), whereas Asian girls were less susceptible to smoking between ages 12 and 16 years (lowest AOR=0.78 at age 15 years) (Figure 3, Panel C). AI/AN/NHPI girls were equally or more susceptible to smoking than white girls (highest AOR=1.86 at age 16 years) until age 17 years when they were less susceptible (lowest AOR=0.12 at age 18 years) (Figure 3, Panel D).
Figure 3.
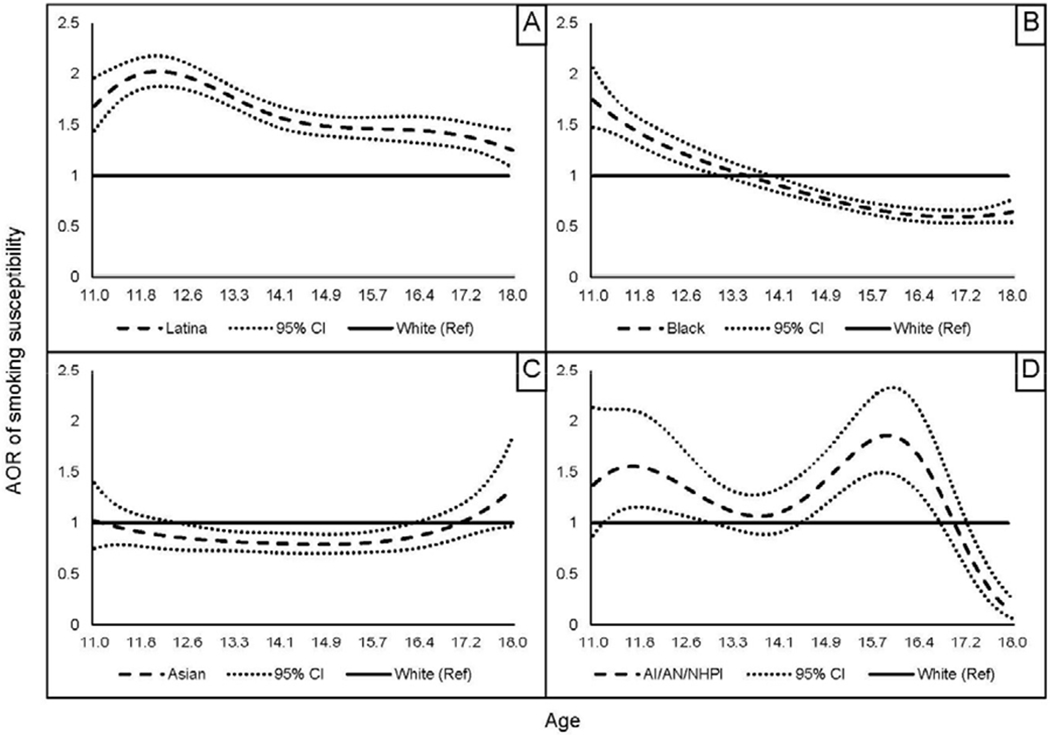
AOR of smoking susceptibility among racial/ethnic minority girls vs white girls over age 11–18 years.
Notes: Panel A: Latina girls vs white girls; Panel B: Black girls vs white girls; Panel C: Asian girls vs white girls; Panel D: AI/AN/NHPI girls vs white girls. Models adjusted for living with a smoker and survey year.
AI/AN/NHPI, American Indian, Alaska Native, Native Hawaiian, and Pacific Islander.
Smoking susceptibility among boys peaked at age 14 years with 29% susceptible (Appendix Table 4). Latino boys were more susceptible than white boys from age 11 to 18 years (highest AOR=1.51 at age 12 years) (Figure 4, Panel A). Black boys were more susceptible to smoking than white boys between age 11 and 13 years (highest AOR=1.29 at age 12 years), after which they were less susceptible between ages 14 and 18 years (lowest AOR=0.64 at age 18 years) (Figure 4, Panel B). Conversely, Asian boys were less susceptible to smoking than white boys from age 11 to 15 years (lowest AOR=0.55 at age 11 years), but were more susceptible from age 17 to 18 years (highest AOR=1.36 at age 18 years) (Figure 4, Panel C). AI/AN/NHPI boys were more susceptible from age 13 to 14 years (highest AOR=1.29 at age 13 years) but were otherwise equally susceptible to smoking as white boys (Figure 4, Panel D).
Figure 4.
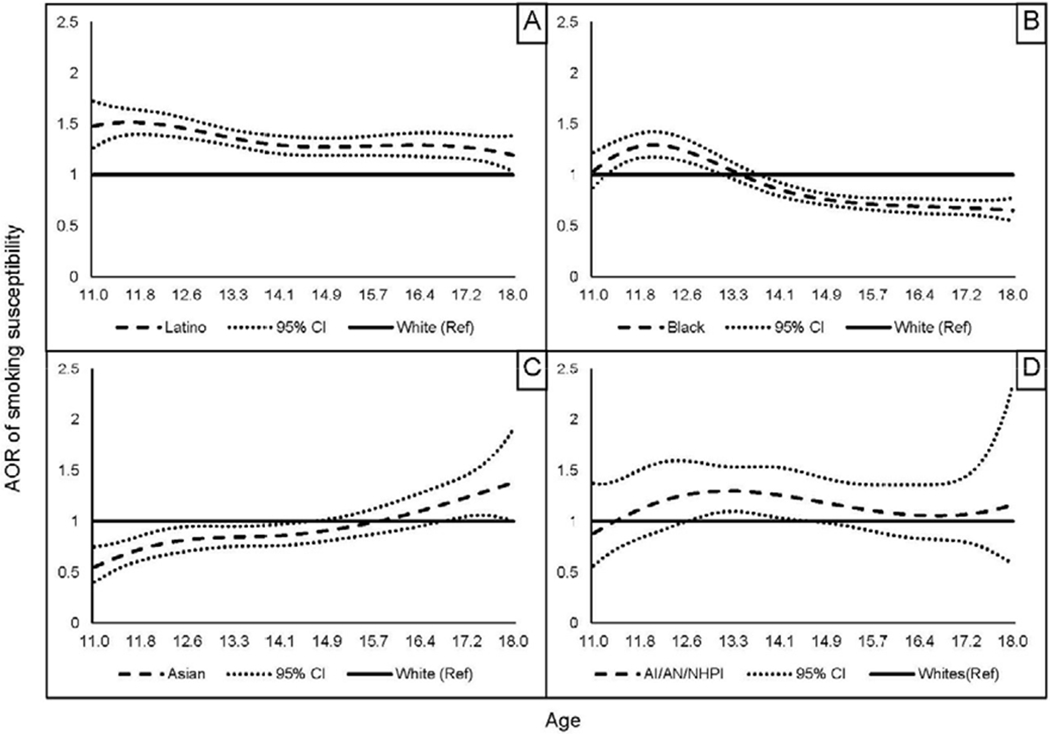
AOR of smoking susceptibility among racial/ethnic minority boys vs white boys over age 11–18 years.
Notes: Panel A: Latino boys vs white boys; Panel B: Black boys vs white boys; Panel C: Asian boys vs white boys; Panel D: AI/AN/NHPI boys vs white boys. Models adjusted for living with a smoker and survey year.
AI/AN/NHPI, American Indian, Alaska Native, Native Hawaiian, and Pacific Islander.
To retain data from all 14 years, susceptibility to and use of e-cigarettes were not included as covariates. Ancillary analyses on data from 2011 to 2018 controlling for e-cigarette use and from 2016 to 2018 controlling for susceptibility to e-cigarettes showed within-gender race and ethnicity patterns of susceptibility to smoking similar to those reported here (data not shown).
DISCUSSION
Despite sharp declines in current and ever smoking among adolescents (Appendix Table 1), smoking susceptibility among never smokers has risen since 2012, peaking between 2014 and 2018 for adolescent girls and boys across racial/ethnic groups. Downward smoking rates are partly attributed to tobacco control policies such as restrictions on tobacco sales and marketing to adolescents, federal and state cigarette taxes, and indoor smoke-free policies that became generalized in the U.S. since 1999. Susceptible adolescents may represent those who did not initiate smoking, partly because of these policies, but are still at risk of future initiation. Addressing this risk of future smoking is a need for tobacco prevention efforts.
The decline in cigarette use has been accompanied by increased marketing of non-cigarette tobacco products, especially e-cigarettes.21 Since 2014, adolescents’ use of these products has reached epidemic proportions,4 prompting a strong response from the U.S. Food and Drug Administration.22 Thus, recent surges in smoking susceptibility could reflect the re-normalization of tobacco use23 or indirect effects of susceptibility to and use of non-cigarette tobacco products on smoking susceptibility.8,24 Of concern is that adolescents susceptible to cigarette smoking may already be non-cigarette tobacco product users or will become non-cigarette tobacco product users or cigarette smokers,25,26 trends that may be observed in forthcoming national surveys of smoking prevalence among adolescents and adults. Research should examine whether smoking susceptibility is attributable to susceptibility to or use of non-cigarette tobacco products, particularly e-cigarettes. Cohort studies are needed to examine transitions from susceptibility/use of non-cigarette tobacco products to susceptibility/use of cigarettes (or vice versa).
Racial/ethnic differences in smoking susceptibility6 were driven in part by gender. Compared with their white counterparts, black and Asian girls were less susceptible to smoking, whereas Latina and AI/AN/NHPI girls were more susceptible. These differences were absent or smaller in magnitude among boys. Although Latino/a adolescents were consistently more susceptible to smoking than white adolescents between 2002 and 2018, these differences grew larger over time between Latina and white girls compared with differences between Latino and white boys.
Findings suggest girls’ susceptibility to smoking is overlooked, corroborating concerns that substance use prevention programs do not target girls or are ineffective among adolescent girls and highlighting a need to develop and implement gender-specific tobacco prevention strategies.27 Lack of major differences in smoking susceptibility rates between girls and boys raises concerns that, over time, lower smoking rates for adult women compared with men will disappear.28 Furthermore, the observation that more than a third of Latino/a adolescent never smokers reported susceptibility in 2018 raises concerns about future smoking risks in this population.
Juxtaposing smoking susceptibility with smoking prevalence data reveals a need for research into the transition from smoking susceptibility to cigarette use, particularly among populations overlooked in prevention efforts.29 Despite lower levels of current smoking at the national level,4,5 Latino/a adolescents had consistently higher susceptibility to smoking compared with white adolescents.6 Latino/a adolescents’ transition to smoking may be reduced through ethnicity-specific protective factors such as familismo, a cultural value emphasizing the importance of family, and ethnic pride, both found to reduce smoking initiation risk among Latino/a adolescents, especially girls.30,31 Indeed, Latinas who are more acculturated to U.S. culture are more likely to smoke than those who are less acculturated.32 Notably, Asian adolescents’ susceptibility is also at odds with their smoking prevalence. Asian adolescents have the lowest rates of smoking but girls were less susceptible to smoking than whites for longer periods of time than boys. These results suggest a need for research into racial/ethnic- and gender-specific protective and risk factors for smoking susceptibility and the transition from susceptibility to cigarette use among Latino/a and Asian adolescents, especially as they become increasingly U.S.-born.33,34 Conversely, smoking susceptibility among black and AI/AN/NHPI adolescents was fairly consistent with smoking prevalence,4,5 which may suggest direct pathways from susceptibility to cigarette use among these populations. Findings regarding AI/AN/NHPI adolescents reaffirm their disproportionate risk of smoking and highlight the need for research with this population.
Research into race/ethnicity- and gender-specific risk factors may elucidate disparities between susceptibility and smoking behavior from initiation and experimentation to regular/daily cigarette use.1,11 For example, tobacco marketing disproportionally is present in low-income and minority neighborhoods, perpetuated by lack of policy enforcement and zoning.35 Adolescents in these communities are also less likely to receive tobacco prevention education in school.36 For gender-specific factors, the desire to lose or maintain weight is a greater predictor of continued smoking among girls than boys (except among black adolescents).37 Another risk factor among adolescent girls is lower (higher) levels of self-reported positive (negative) affect.38 Importantly, although discrepancies between smoking susceptibility and smoking behavior are present at the national level, these rates are influenced by state-level tobacco control policies and regional characteristics.39
Susceptibility to smoking develops relatively uniformly over developmental age for girls and boys. Compared with their white counterparts, smoking susceptibility peaked between ages 11 and 13 for black and Latino/a adolescents. These results contextualize susceptibility as a precursor to smoking, with increases in transition to smoking occurring around age 14–15 years.19 AI/AN/NHPI girls and Asian boys had later ages of peak susceptibly, at 16 and 18 years, respectively. Research is needed to understand risk and protective factors for smoking susceptibility during early (age 10–13 years), middle (age 14–16 years), and late (age 17–19 years) adolescence,13 with early and middle adolescence being critical for tobacco prevention efforts. Further, research is needed to understand the discrepant trajectories of susceptible girls versus boys to explicate reasons for boys’ tendency to initiate smoking earlier than girls.40 Tobacco control efforts should reflect variability in development and behavior throughout adolescence and strategize tobacco prevention efforts that address these milestones.2,41 For example, susceptibility peaks in middle adolescence, a period when peer influence outweighs parental influence in predicting adolescent smoking behavior.41 Higher susceptibility among younger adolescents may also be a result of their social media use, often a platform for disseminating tobacco-related descriptive norms.42
Disaggregating smoking susceptibility revealed notable racial/ethnic differences over developmental age considering known ages of smoking initiation. Despite research showing that black and Latino/a adolescents initiate smoking later than white adolescents, black adolescents were more susceptible to smoking in early adolescence and Latino/a adolescents were consistently more susceptible to smoking until age 18 years compared with white adolescents.43 Conversely, smoking susceptibility among Asian boys and AI/AN/NHPI girls peaked in middle and late adolescence, consistent with their greater likelihood of initiating smoking in late adolescence and young adulthood compared with white adolescents.43,44 Discrepancies in age of smoking susceptibility and initiation highlight a need to understand mediating risk and protective factors for smoking initiation and how these relate to continued or increased smoking uptake throughout the lifespan. These results pinpoint the optimal developmental ages to target at-risk girls and boys from all racial/ethnic groups. In addition to macro-level prevention efforts,1 effective interventions targeting adolescents susceptible to smoking are needed. Prevention efforts targeting at-risk populations produce better and cost-effective outcomes than universal methods.41 The availability and use of digital platforms allow interventions to be tailored to address overlapping and evolving identities, including gender and race/ethnicity over developmental age.45
Limitations
Results are not generalizable to out-of-school adolescents. Although smoking susceptibility was self-reported, the measure has been validated and found predictive of future smoking in a nationally representative longitudinal study.3 Unmeasured and inconsistently measured variables could not be included as covariates. For example, exposure to tobacco advertising online and in stores was omitted in 2016. Because of small sample sizes, AI/AN and NHPI adolescents were collapsed into one group despite differences in their smoking behaviors.5 Limitations on variables collected prevented disaggregating smoking susceptibility by Latino/a national background. Although nationally representative, small sample sizes of some racial and ethnic groups limited the power to detect differences in smoking susceptibility if differences indeed existed. Oversampling of minorities, particularly Asian and AI/AN/NHPI adolescents, is necessary to replicate these findings or reveal associations masked by sample heterogeneity or low power. The coding of susceptibility for Question 1 in 2012–2018 was a departure from previous work.6 However, it is consistent with the default coding of Questions 2 and 3 and parallels established susceptibility definitions that were shown to predict smoking initiation.3 This harmonization approach might have resulted in overestimated proportions of susceptible adolescents starting in 2012.3
CONCLUSIONS
Susceptible adolescents represent a reserve of potential future cigarette smokers and current/future non-cigarette tobacco users. Prevention efforts should target racial/ethnic adolescents who are highly susceptible to smoking, primarily Latino/a and AI/AN/NHPI adolescents. Targeting adolescent girls is needed as they exhibit unique smoking susceptibility patterns over time. Prevention efforts should target adolescents at peak developmental times for smoking susceptibility, which, although different by race/ethnicity, are largely uniform for boys and girls within each racial/ethnic group. Race/ethnicity-, gender-, and age-specific tailored programs for susceptible adolescents can prevent smoking initiation, delay smoking onset, and eliminate tobacco-related disparities.
Supplementary Material
ACKNOWLEDGMENTS
The research presented in this paper is that of the authors and does not reflect the official policy of HHS, NIH, the National Institute on Minority Health and Health Disparities, or the National Heart, Lung, and Blood Institute. The efforts of Drs. Kamke and El-Toukhy were supported by Division of Intramural Research of the National Institute on Minority Health and Health Disparities, NIH. The efforts of Drs. Rodriquez and Perez-Stable were supported by the Division of Intramural Research of the National Heart, Lung, and Blood Institute, NIH. Dr. Pérez-Stable is also supported by the Office of the Director, National Institute on Minority Health and Health Disparities, NIH. Dr. Sabado-Liwag has no funding sources to report. The funding sources had no role in study conceptualization or data analysis. This project only involved the use of de- identified data, which is considered “not human subjects research.” “Not human subjects research” requires no IRB review or approval per NIH policy and 45 CFR 46.
KK drafted the manuscript and analyzed the data; MS-L merged the data; MS-L, EJR, and SEl-T conceptualized the study; EJP-S and SEl-T critically edited and reviewed the manuscript for intellectual content; all authors approved the manuscript. The results of this manuscript have not previously been reported elsewhere. The authors have no financial disclosures to report.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.HHS. Preventing tobacco use among youth and young adults: a report of the Surgeon General. Atlanta, GA: HHS, CDC, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2012. www.ncbi.nlm.nih.gov/books/NBK99237/. Accessed December 2, 2019. [Google Scholar]
- 2.Sawyer SM, Afifi RA, Bearinger LH, et al. Adolescence: a foundation for future health. Lancet. 2012;379(9826):1630–1640. 10.1016/s0140-6736(12)60072-5. [DOI] [PubMed] [Google Scholar]
- 3.Pierce JP, Choi WS, Gilpin EA, Farkas AJ, Merritt RK. Validation of susceptibility as a predictor of which adolescents take up smoking in the United States. Health Psychol. 1996; 15(5):355–361. https://doi.Org/10.1037//0278-6133.15.5.355. [DOI] [PubMed] [Google Scholar]
- 4.Gentzke AS, Creamer M, Cullen KA, et al. Vital signs: tobacco product use among middle and high school students - United States, 2011–2018. MMWR Morb Mortal Wkly Rep. 2019;68(6):157–164. 10.15585/mmwr.mm6806e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Odani S, Armour BS, Agaku IT. Racial/ethnic disparities in tobacco product use among middle and high school students - United States, 2014–2017. MMWR Morb Mortal Wkly Rep. 2018;67(34):952–957. 10.15585/mmwr.mm6734a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.El-Toukhy S, Sabado M, Choi K. Trends in susceptibility to smoking by race and ethnicity. Pediatrics. 2016;138(5):e20161254 10.1542/peds.2016-1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Veeranki SP, Mamudu HM, Anderson JL, Zheng S. Worldwide never-smoking youth susceptibility to smoking. J Adolesc Health. 2014;54(2): 144–150. 10.1016/j.jadohealth.2013.07.036. [DOI] [PubMed] [Google Scholar]
- 8.Trinidad DR, Pierce JP, Sargent JD, et al. Susceptibility to tobacco product use among youth in wave 1 of the Population Assessment of Tobacco and Health (PATH) study. Prev Med. 2017;101:8–14. 10.1016/j.ypmed.2017.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pierce JP, Messer K, James LE, et al. Camel No. 9 cigarette-marketing campaign targeted young teenage girls. Pediatrics. 2010;125(4):619–626. 10.1542/peds.2009-0607. [DOI] [PubMed] [Google Scholar]
- 10.Luk JW, Farhat T, Iannotti RJ, Simons-Morton BG. Parent-child communication and substance use among adolescents: do father and mother communication play a different role for sons and daughters? Addict Behav. 2010;35(5):426–431. 10.1016/j.addbeh.2009.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ethnicity Mermelstein R., gender and risk factors for smoking initiation: an overview. Nicotine Tob Res. 1999;1(1):39–43. 10.1080/14622299050011791. [DOI] [PubMed] [Google Scholar]
- 12.Bowleg L The problem with the phrase women and minorities: intersectionality—an important theoretical framework for public health. Am J Public Health. 2012;102(7):1267–1273. 10.2105/ajph.2012.300750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.WHO. Adolescence: A period needing special attention. http://apps.who.int/adolescent/second-decade/section2/page2/age-not-the-whole-story.html. Published 2014. Accessed September 9, 2019.
- 14.Office on Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion, CDC. Historical NYTS Data and Documentation. Atlanta, GA: CDC; 2018. www.cdc.gov/tobacco/data_statistics/surveys/nyts/data/index.html. Accessed February 9, 2019. [Google Scholar]
- 15.Conron KJ, Landers SJ, Reisner SL, Sell RL. Sex and gender in the US health surveillance system: A call to action. Am J Public Health. 2014;104(6):970–976. 10.2105/AJPH.2013.301831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dziak JJ, Li R, Wagner AT. Weighted TVEM SAS macro users’ guide (Version 2.6). University Park, PA: The Methodology Center, Penn State; 2017. www.methodology.psu.edu. Accessed December 2, 2019. [Google Scholar]
- 17.National Institute on Minority Health and Health Disparities. NIMHD: Overview; 2019. https://nimhd.nih.gov/about/overview/. Accessed September 9, 2019.
- 18.Albers AB, Biener L, Siegel M, Cheng DM, Rigotti N. Household smoking bans and adolescent antismoking attitudes and smoking initiation: findings from a longitudinal study of a Massachusetts youth cohort. Am J Public Health. 2008;98(10):1886–1893. 10.2105/ajph.2007.129320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Keyes KM, Rutherford C, Miech R. Historical trends in the grade of onset and sequence of cigarette, alcohol, and marijuana use among adolescents from 1976–2016: implications for “gateway” patterns in adolescence. Dmg Alcohol Depend. 2019;194:51–58. 10.1016/j.drugalcdep.2018.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.SAS. Compute biserial, point biseral, and rank biserial correlations. 2.2 ed 2007. http://support.sas.com/kb/24/991.html. Accessed December 12, 2019. [Google Scholar]
- 21.El-Toukhy SM, Choi K. Magazine hyped: trends in tobacco advertising and readership characteristics, 2010–2014. Prev Med. 2016;91:132–137. 10.1016/j.ypmed.2016.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.U.S. Food & Drug Administration. FDA’s deeming regulations for e-cigarettes, cigars, and all other tobacco products. www.fda.gov/TobaccoProducts/Labeling/RulesRegulationsGuidance/ucm394909.htm. Published 2019. Accessed April 23, 2019.
- 23.Fairchild AL, Bayer R, Colgrove J. The renormalization of smoking? E-cigarettes and the tobacco “endgame”. New Engl J Med. 2014;370(4):293–295. 10.1056/nejmp1313940. [DOI] [PubMed] [Google Scholar]
- 24.Sabado M, Perez-Stable E, El-Toukhy S. Adolescent susceptibility to cigarette, e-cigarette and hookah by race and ethnicity. Poster presented at: Society for Nicotine and Tobacco Research 25th Annual Meeting, February 22, 2019; San Francisco, CA. [Google Scholar]
- 25.Soneji S, Barrington-Trimis JL, Wills TA, et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults. JAMA Pediatr. 2017;171(8):788–797. 10.1001/jamapediatrics.2017.1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chaffee BW, Cheng J. Tobacco product initiation is correlated with cross-product changes in tobacco harm perception and susceptibility: longitudinal analysis of the Population Assessment of Tobacco and Health youth cohort. Prev Med. 2018;114:72–78. 10.1016/j.ypmed.2018.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kumpfer KL, Smith P, Summerhays JF. A wakeup call to the prevention field: are prevention programs for substance use effective for girls? Subst Use Misuse. 2008;43(8–9):978–1001. 10.1080/10826080801914261. [DOI] [PubMed] [Google Scholar]
- 28.Wang TW, Asman K, Gentzke AS, et al. Tobacco product use among adults - United States, 2017. MMWR Morb Mortal Wkly Rep. 2018;67(44):1225–1232. 10.15585/mmwr.mm6744a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kong G, Singh N, Krishnan-Sarin S. A review of culturally targeted/tailored tobacco prevention and cessation interventions for minority adolescents. Nicotine Tob Res. 2012; 14( 12):1394–1406. 10.1093/ntr/nts118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rajesh V, Diamond PM, Spitz MR, Wilkinson AV. Smoking initiation among Mexican heritage youth and the roles of family cohesion and conflict. J Adolesc Health. 2015;57(1):24–30. 10.1016/j.jadohealth.2015.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Castro FG, Stein JA, Bentler PM. Ethnic pride, traditional family values, and acculturation in early cigarette and alcohol use among Latino adolescents. J Prim Prev. 2009;30(3–4):265–292. 10.1007/s10935-009-0174-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kaplan RC, Bangdiwala SI, Barnhart JM, et al. Smoking among U.S. Hispanic/Latino adults: the Hispanic Community Health Study/Study of Latinos. Am J Prev Med. 2014;46(5):496–506. https://doi.Org/10.1016/j.amepre.2014.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Flores A Facts on U.S. Latinos, 2015. Washington, DC: Pew Research Center; 2017. www.pewhispanic.org/2017/09/18/facts-on-u-s-latinos/. Accessed December 2, 2019. [Google Scholar]
- 34.Colby S, Ortman J. Projection of the size and composition of the U.S. population: 2014 to 2060. Washington, DC: U.S: Census Bureau; 2015. www.census.gov/content/dam/Census/library/publications/2015/demo/p25-1143.pdf Accessed December 12, 2019. [Google Scholar]
- 35.Lee JG, Henriksen L, Rose SW, Moreland-Russell S, Ribisl KM. A systematic review of neighborhood disparities in point-of-sale tobacco marketing. Am J Public Health. 2015;105(9):e8–el8. 10.2105/ajph.2015.302777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kaestle CE, Wiles BB. Targeting high-risk neighborhoods for tobacco prevention education in schools. Am J Public Health. 2010;100(9):1708–1713. 10.2105/ajph.2008.145557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fulkerson J, French S. Cigarette smoking for weight loss or control among adolescents: gender and racial/ethnic differences. J Adolesc Health. 2003;32(4):306–313. 10.1016/s1054-139x(02)00566-9. [DOI] [PubMed] [Google Scholar]
- 38.Audrain-McGovern J, Rodriguez D, Feventhal AM. Gender differences in the relationship between affect and adolescent smoking uptake. Addiction. 2015;110(3):519–529. 10.1111/add.12797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Farrelly MC, Foomis BR, Han B, et al. A comprehensive examination of the influence of state tobacco control programs and policies on youth smoking. Am J Public Health. 2013; 103(3):549–555. 10.2105/ajph.2012.300948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Okoli C, Greaves F, Fagyas V. Sex differences in smoking initiation among children and adolescents. Public Health. 2013;127(1):3–10. 10.1016/j.puhe.2012.09.015. [DOI] [PubMed] [Google Scholar]
- 41.Stanis JJ, Andersen SF. Reducing substance use during adolescence: a translational framework for prevention. Psychopharmacology (Berl). 2014;231(8):1437–1453. 10.1007/s00213-013-3393-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hebert ET, Case KR, Kelder SH, Delk J, Perry CF, Harrell MB. Exposure and engagement with tobacco- and e-cigarette-related social media. J Adolesc Health. 2017;61 (3):371–377. 10.1016/j.jadohealth.2017.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thompson AB, Mowery PD, Tebes JK, McKee SA. Time trends in smoking onset by sex and race/ethnicity among adolescents and young adults: findings from the 2006–2013 National Survey on Drug Use and Health. Nicotine Tob Res. 2018;20(3):312–320. 10.1093/ntr/ntx010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Patten CA, Koller KR, Flanagan CA, et al. Age of initiation of cigarette smoking and smokeless tobacco use among western Alaska Native people: secondary analysis of the WATCH study. Addict Behav Rep. 2018;9:100143 10.1016/j.abrep.2018.100143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Marsch LA, Borodovsky JT. Technology-based interventions for preventing and treating substance use among youth. Child Adolesc Psychiatr Clin N Am. 2016;25(4):755–768. 10.1016/j.chc.2016.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


