Abstract
More than 70% of zoonotic diseases are wildlife associated putting wildlife professionals at increased risk of occupational exposure. In 2008 and 2018, the Arizona Department of Health Services surveyed Arizona wildlife professionals from multiple agencies to assess the risk of disease exposure, rabies pre-exposure prophylaxis (PrEP) history, personal protective equipment (PPE) use, and zoonoses knowledge. In 2008, a 12-question survey was distributed at a state wildlife professional meeting using an anonymous email link. In 2018, a 20-question survey was distributed using an anonymous email link to wildlife agency employees. We received 164 and 81 complete responses in the 2008 and 2018 surveys, respectively. Bites from rabies reservoir or spillover species were higher in 2008 (42%) than in 2018 (16%). More respondents received PrEP in 2018 (53%) than in 2008 (45%). Among 43 respondents who performed necropsies or collected animal samples within the past 5 years (2014–2018), only 60% always wore latex or nitrile gloves, and 79% never wore a facemask. Respondents indicated lower awareness of certain zoonoses, including brucellosis (72%) and leptospirosis (60%). Results on zoonoses awareness and reasons for non-use of PPE highlighted targets for education to improve practices, including facilitation of PPE training to prevent future disease transmission.
Keywords: Personal protective equipment, Rabies, Risk, Wildlife, Zoonosis, Zoonotic disease
Introduction
Over half of all emerging infectious diseases are zoonotic, and over 70% of those are associated with wildlife (Jones et al. 2008). Professionals who work with animals are at increased risk of disease exposure through their occupation as compared to the general population, and this risk varies depending upon the type of work performed and the species contacted (Baker and Gray 2009; Bosch et al. 2013; Vitek et al. 1996). In Arizona, multiple zoonotic or vector-borne diseases are present in the wildlife populations including rabies, plague, tularemia, Hantavirus, and others. The major routes of disease transmission are direct and indirect contact with bodily secretions, vector-borne infections, and aerosol or respiratory transmission. Transmission of these zoonotic diseases to people can be pre vented by having policies in place and trainings for staff on the appropriate use of personal protective equipment (PPE) and other preventive measures, and appropriate rabies pre-exposure prophylaxis (PrEP) for at-risk personnel (CDC 2011).
Rabies is a preventable zoonotic disease through appropriate pre-exposure vaccination and/or post-exposure prophylaxis and correct wound care. The Advisory Committee on Immunization Practices and CDC recommend rabies PrEP based on categories of risk. Wildlife workers working in areas where rabies is uncommon to rare are categorized as at ‘infrequent risk’, while those who handle bats or work in rabies-enzootic areas are categorized as at ‘frequent risk’; both risk groups are recommended to complete a three-dose rabies pre-exposure vaccination series (CDC 2011; Rupprecht et al. 2010). Rabies PrEP does not eliminate the need for additional rabies vaccinations following a known or suspect rabies virus exposure, however, it simplifies the rabies post-exposure treatment, and might be protective in cases of unrecognized rabies exposure or when post-exposure treatment is delayed (Williams et al. 2015).
In 2008, the death of a National Park Service (NPS) wildlife biologist in Arizona from pneumonic plague after he conducted a necropsy on an infected mountain lion without adequate PPE (Wong et al. 2009) prompted a national survey of NPS wildlife professionals. Results from the national survey found variability in training on PPE and zoonotic disease awareness among wildlife professionals specifically within the NPS (Bosch et al. 2013). However, there had been no evaluation of wildlife professionals from other agencies within Arizona, such as universities and wildlife control agencies; this prompted coauthors J.G. and E.L. with the Arizona Department of Health Services (ADHS) to conduct a survey among wildlife professionals specifically within Arizona in 2008. The two staff who administered the 2008 survey left the agency shortly after and were unable to implement any activities to promote behavior change. A revised version of the 2008 Arizona survey was created and distributed in 2018 to further describe practice and culture in the intervening period and address additional targets of interest identified in 2008. The results of both surveys are discussed here. The purpose of these survey evaluations was to characterize the frequency and type of animal exposures of wildlife professionals, characterize their rabies PrEP history and PPE use, and assess knowledge of zoonotic or vector-borne diseases carried by wildlife.
Materials and Methods
In 2008, a 12-question survey was distributed in-person at a professional wildlife meeting with approximately 300 attendees from state and federal agencies and also using an anonymous email link to 230 Arizona wildlife agency employees. The email link directed respondents to an online version of the survey by SurveyMonkey®. Paper responses were manually entered into a Microsoft Excel® database.
In 2018, email was the sole distribution method of the revised 20-question survey; there was no comparable wildlife professional meeting taking place and we were unable to recreate the same distribution method as in 2008. The survey was distributed to all 250 AZ-based employees working at state and federal wildlife agencies (e.g., Arizona Game and Fish Department, United States Department of Agriculture Wildlife Services, National Park Service), licensed wildlife rehabilitators, and nuisance or other wildlife control groups through their own list serves. The 2018 survey was created using Qualtrics® and distributed using an anonymous email link. Copies of the surveys are available upon request.
Both surveys included questions on the types of animals contacted as part of respondents’ occupation (birds, reptiles or amphibians, fish, mammals, or invertebrates), history of bites or scratches, PPE use, rabies vaccination status, and demographics. PPE use was defined as wearing appropriate personal protective equipment (latex or nitrile gloves, leather gloves, eye protection such as goggles or glasses, painter’s mark or surgical mask, N95 or higher respirator, face shield, or coveralls, smock, or lab coat); we asked whether each item is worn during certain procedures performed (if they cut into an animal, cut into animal tissue for head removal, collected specimens including tooth removal, assisted in a necropsy, or performed skin collection or removal). Animal species and geography were taken into consideration when analyzing rabies risk assessments; for example, the raccoon variant is not present in Arizona, therefore we considered contact with raccoons to be contact with a rabies spillover species in Arizona rather than a rabies reservoir. Respondents who reported contact with mammals were asked about which types of mammals to determine exposure to Arizona-specific rabies reservoir species (bats, skunks, and foxes) and rabies spillover species (bobcats, coyotes, javelina, wolves, mountain lions, raccoons, and bears), and risk of exposure to other zoonotic diseases. General contact was defined as handling or touching of the animal with PPE use, while direct contact was defined as unprotected handling or touching of the animal without PPE use (e.g., no gloves). The 2018 survey included additional questions that asked about barriers to PPE use (cost, difficulty of use, availability, etc.) and awareness of diseases that wildlife or wildlife-associated arthropods carry. Respondents were able to write-in comments and explanations for some questions with an ‘other’ option; these responses were not formally analyzed but were used to clarify additional animal species worked with or reasons for PPE non-use not already provided as an option. Questions regarding practices performed within the previous 5 years refer to the years 2004–2008 in the 2008 survey and 2014–2018 in the 2018 survey. Prior to distribution, the 2018 survey was piloted with wildlife professionals to ensure question suitability for the intended audience. Descriptive statistics were calculated in Microsoft Excel®. Surveys were anonymous and respondents could not be matched across surveys, resulting in the additional potential differences between the survey administered in 2008 and 2018. We performed Chi-square tests and calculated P values to assess the differences using statistical analysis software SAS® version 9.4 (SAS Institute Incorporated, Cary, North Carolina). A P value < 0.05 was considered significant.
Both surveys offered gift card incentives for participation. Participants were assigned a unique identification number and a random number generator was utilized to select the card recipients. The Centers for Disease Control and Prevention (CDC) reviewed this project for human subjects protection and determined it to be nonresearch, and data were approved for collection in compliance with the Paperwork Reduction Act.
Results
Demographics
In the 2008 survey, responses from 164 Arizona wildlife workers were received for an approximate 31% response rate. Over half of the respondents (n = 87, 54%) reported working in the field for over 10 years (Table 1). Two-thirds of respondents (67%) identified with job titles that indicate high levels of experience, such as senior Wildlife Specialists, Wildlife Biologists, or Supervisors. Nearly three quarters of respondents were employed by a state agency in Arizona (for example, Arizona Game and Fish Department), 19% of respondents were employed by a federal agency working in Arizona (for example, U.S. Department of Agriculture), and the remaining 7% worked for universities, tribal jurisdictions, or other agencies in Arizona.
Table 1.
Demographics of Arizona wildlife professional respondents, 2008 and 2018.
| 2008a (N = 164), no. (%) | 2018 (N = 82), no. (%) | |
|---|---|---|
| Genderb | ||
| Male | - | 41 (50.6%) |
| Female | - | 40 (49.4%) |
| Age (in years) | ||
| 20–29 | - | 16 (19.5%) |
| 30–39 | - | 15 (18.3%) |
| 40–49 | - | 21 (25.6%) |
| 50–59 | - | 21 (25.6%) |
| 60–69 | - | 9 (10.9%) |
| Employer categoryb | ||
| State | 119 (73.5%) | 46 (56.8%) |
| Federal | 31 (19.1%) | 17 (21.0%) |
| College/university | - | 7 (8.6%) |
| Wildlife rehabilitation | - | 3 (3.7%) |
| Other | 12 (7.4%) | 8 (9.9%) |
| Years of experience | ||
| <1 | - | 1 (1.2%) |
| 1–5 | - | 14 (17.1%) |
| 6–10 | - | 19 (23.2%) |
| > 10 | 87 (53.7%) | 48 (58.5%) |
| Formal education (highest) | ||
| Some college | - | 6 (7.3%) |
| Bachelor’s degree | - | 37 (45.1%) |
| Master’s degree | - | 29 (35.4%) |
| PhD or equivalent | - | 10 (12.2%) |
Demographic information (e.g., gender, age, education) was not asked in the 2008 survey, therefore is represented in the table with “–”
One respondent did not answer the gender or employer category question in the 2018 survey, therefore N = 81 in those categories.
In the 2018 survey, responses from 83 Arizona wildlife workers were received; two surveys lacked complete demographic information, resulting in 81 surveys completed including demographic data. The two surveys that lacked complete demographic information (one survey was only missing 2 demographic responses, and the other survey was missing all demographic information) were still included in the majority of the analysis because all other questions asked were complete. Of these completed surveys, 57% of respondents reported being employed by a state agency in Arizona, 21% were employed by a federal agency working in Arizona, and the remaining 22% were employed by universities, wildlife rehabilitation, wildlife control or other agencies in Arizona (Table 1). Forty-eight respondents (59%) had over 10 years of experience. Gender distribution was effectively equal; and respondents had collectively worked in every county in Arizona.
Exposure Risk and Pre-exposure Prophylaxis for Rabies
In 2008, all 164 respondents reported having direct contact with various wild animal species as part of their occupation (Fig. 1). Sixty-one percent of respondents reported having direct contact with bats, 42% with rabies spillover species, and 11% with terrestrial rabies reservoir species (foxes and skunks). Twenty-seven percent of respondents reported having been bitten by an animal while on duty within the past 5 years (2004–2008); 42% (18/43) of these reported being bitten by either rabies reservoir species (bats, skunks, and foxes were reported) or rabies spillover species (bobcats, coyotes, and javelina were reported). Approximately one-third (32%) of respondents reported being scratched by an animal within the past 5 years (2004–2008); 25% of these reported being scratched by rabies reservoir species (bats and foxes were reported) or rabies spillover species (bobcats and coyotes reported).
Figure 1.

Percentage of Arizona wildlife professional respondents reporting animal contact, by type, 2008 and 2018. *Indicates a significant difference was calculated (P < 0.05). In the 2008 study, rabies reservoir species (other than bats) were defined as skunks and foxes. Rabies spillover species were defined as bobcats, coyotes, javelina, wolves, mountain lions, raccoons, and bears. Rodents included prairie dogs (which were broken out further in 2018), bovids included bison and bighorn sheep, and cervids included deer and elk. Contact with prairie dogs, bovids, cervids, fish, amphibians, and invertebrates was not asked about in 2008.
In 2008, 55% of 161 respondents reported not receiving PrEP. Among the respondents who reported not receiving PrEP, 51% reported coming into direct contact with bats, 14% with other rabies reservoir species (foxes and skunks), and 42% with rabies spillover species. Several respondents who did not receive PrEP reported direct high-risk exposures (e.g., bite, scratch, cutting [defined as cutting into an animal or animal tissue for head removal, specimen collection (excluding tooth removal)], assisting with a necropsy, or skin collection or removal) to rabies reservoir and rabies spillover species. Two respondents reported being bitten by rabies reservoir species (both bats) and one by rabies spillover species (coyote). Two respondents reported being scratched by rabies reservoir species (both bats) and four by rabies spillover species (bobcats and coyotes reported). Fifteen percent reported cutting into rabies reservoir species and 40% into rabies spillover species.
In 2008, state employees reported lower attainment of PrEP than federal employees. Only 34% of state employees reported receiving PrEP while 81% of federal employees reported receiving PrEP. Acquisition of the rabies vaccine did not appear to differ by years of employment and job title.
In 2018, all 83 respondents reported having direct contact with various wild animal species as part of their occupation. Forty-one percent of respondents reported having direct contact with bats, 43% with rabies spillover species, and 42% with rabies reservoir species (foxes and skunks). Twenty-three percent of respondents reported having been bitten by an animal while on duty within the past 5 years (2014–2018); 16% (3/19) of these reported being bitten by rabies reservoir species (bats were reported) but no rabies spillover species bites were reported). Approximately one-fifth (19%) of respondents reported being scratched by an animal within the past 5 years (2014–2018); none of these reported being scratched by rabies reservoir species or rabies spillover species.
In 2018, 33% of 60 respondents reported not receiving PrEP. Of the respondents who reported not receiving PrEP, 20% reported coming into direct contact with bats, 40% with other rabies reservoir species (foxes and skunks), and 35% with rabies spillover species. Few respondents who did not receive PrEP reported direct high-risk exposures to rabies reservoir and rabies spillover species. No unvaccinated respondents reported being bitten or scratched by rabies reservoir species or rabies spillover species. Only one respondent (5%) reported cutting into rabies reservoir species (skunk reported) while 30% into rabies spillover species (mountain lions, bear, bobcats, and coyote reported). Thirty percent of the unvaccinated respondents reported the reason they had not received PrEP was cost; four of those six respondents reported contact with a rabies reservoir (bats, skunks, and foxes reported) or spillover species (mountain lion reported).
In 2018, state employees reported lower attainment of PrEP than federal employees. Only 41% of 46 state employees reported receiving PrEP while 71% of 17 federal employees reported receiving PrEP. Acquisition of the rabies vaccine did not appear to differ by years of employment and job title.
Personal Protective Equipment Use
In 2008, the majority of respondents (87%) reported cutting into an animal, and 57% reported removing a tooth from an animal. When cutting into an animal, 56% reported always using either latex or leather gloves, and 6% reported always wearing either a face shield or protective glasses and a mask together (Fig. 2).
Figure 2.

Comparison of categories of PPE use among Arizona wildlife professionals that cut or sampled animal tissues, 2008 and 2018. In the 2008 graph, the N95 or higher respirators are not shown because this question was not specifically addressed in 2008.
In 2018, 78% of respondents reported receiving either formal or on-the-job training on how or when to properly utilize PPE. Fifty-eight percent had cut into animals for sample collection or to perform a necropsy as part of their occupation within the previous 5 years (2014–2018). Among those, 60% of 48 respondents always wore latex or nitrile gloves and 33% sometimes wore them (Fig. 2). Seventy-nine percent of respondents reported never wearing a surgical mask or higher level of respiratory protection (e.g., N95 respirator) and 25% never wore eye protection. The primary reason given for PPE non-use was a belief that it was not necessary for the given scenarios (79% of 48 responses). The next most common reason was that PPE was not readily available (27%), followed by practicality (either too difficult to use, transport, or limited by time) (19%), and cost (2%).
Disease Awareness
The majority of respondents in 2018 indicated high levels of awareness of the endemic diseases carried by wildlife or wildlife-associated arthropods in Arizona (e.g., rabies, plague, Rocky Mountain spotted fever) (ADHS 2019). Awareness was assessed as ‘check the following diseases that you were aware could be carried by wildlife or wildlife-associated arthropods (ex. ticks)’. Awareness of plague was highest at 96%, followed by Rocky Mountain spotted fever (93%), and rabies and hantavirus (both 91%) (Fig. 3). Personal pesticide or pest repellent use occurred at least seasonally (sometimes or always) by 75% of respondents.
Figure 3.
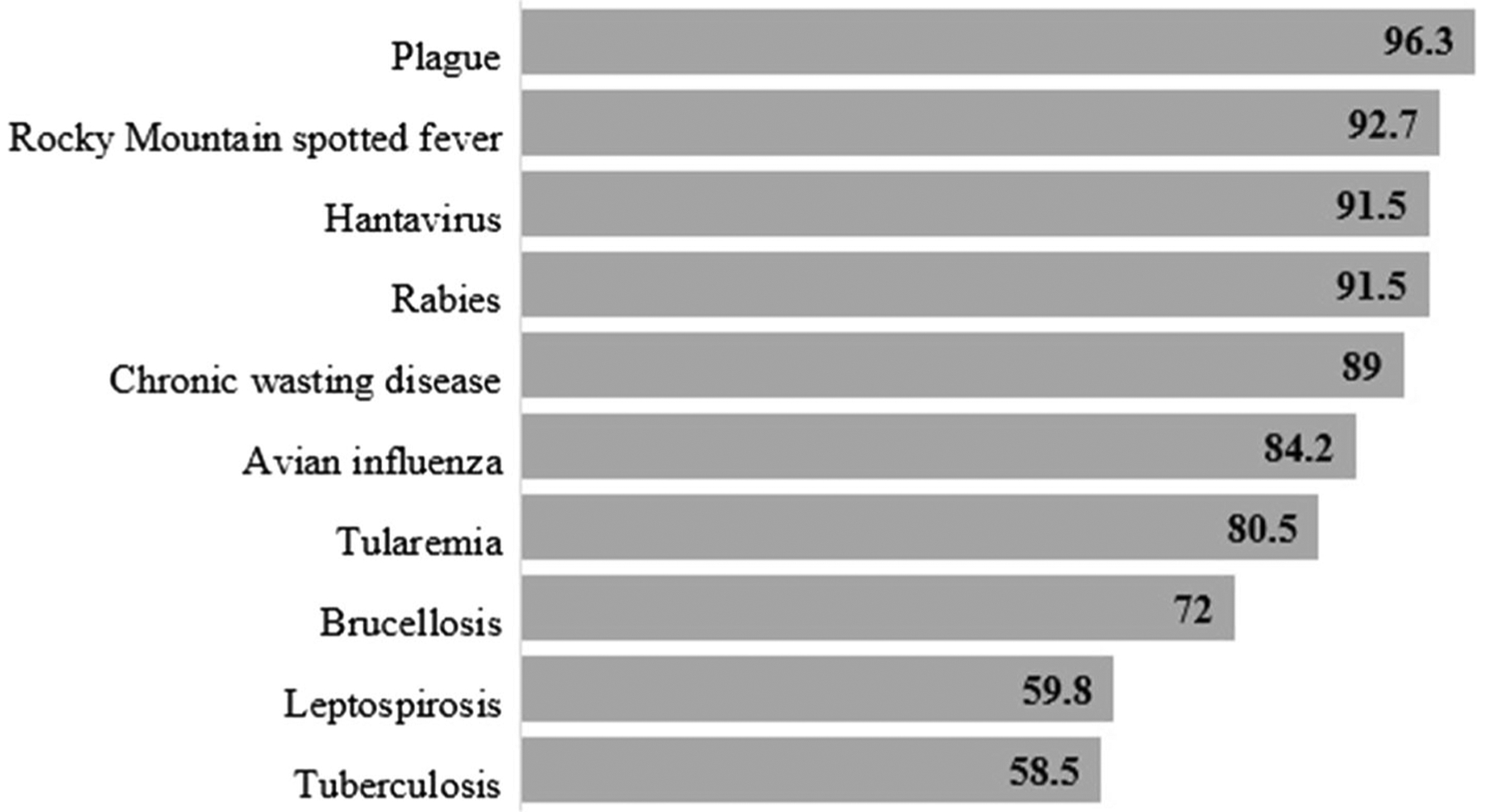
Percent of Arizona wildlife professional respondents aware of zoonotic diseases, 2018.
Comparisons
At a 5% level of significance, from the survey sample data, there is sufficient evidence to conclude that there is a difference in the proportions of wildlife professionals in 2008 and 2018 who had contact with birds (χ2 = 17.9; P < 0.0001), bats (χ2 = 8.9; P = 0.003), and foxes and/or skunks (χ2 = 31.7; P < 0.0001) (Fig. 1, Table 2). Additional significant differences between 2008 and 2018 survey populations are included in Table 2.
Table 2.
Significant differences between wildlife professional survey respondents, 2008 and 2018.
| 2008 (N = 164), no. (%) | 2018 (N = 83), no. (%) | χ2 | P value | |
|---|---|---|---|---|
| Animal contact | ||||
| Birds | 125 (76%) | 41 (49%) | 17.9 | < 0.0001 |
| Bats | 100 (61%) | 34 (41%) | 8.9 | 0.003 |
| Foxes and/or skunks | 18 (11%) | 35 (42%) | 31.7 | < 0.0001 |
| Exposures | ||||
| Being bitten by rabies reservoir/spillover species | 18/43 (42%) | 3/19 (16%) | 3.9 | 0.047 |
| Being scratched by an animal | 52/162 (32%) | 16 (19%) | 4.5 | 0.03 |
| Being scratched by rabies reservoir/spillover species | 13/52 (25%) | 0/16 (0%) | 4.9 | 0.03 |
| Reported cutting into an animal | 141/162 (87%) | 48 (56%) | 26.5 | < 0.0001 |
| Did not receive rabies pre-exposure vaccination | 88/161 (55%) | 20/60 (33%) | 7.9 | 0.005 |
| Had bat contact | 45/88 (51%) | 4/20 (20%) | 6.3 | 0.01 |
| Had fox and/or skunk contact | 12/88 (14%) | 8/20 (40%) | 7.4 | 0.006 |
| Always wore face shield, mask, or goggles while cutting into an animal | 8/141 (6%) | 17/48 (35%) | 27.4 | < 0.0001 |
Denominators are included specifically if different from the column.N
Discussion
Arizona wildlife harbor multiple zoonotic diseases and wildlife professionals are potentially at increased risk of exposure to these diseases due to the nature of their work (Mauldin et al. 2016). Approximately one quarter of our survey respondents reported experiencing wildlife bites in 2008 and 2018, although the frequency of high-risk rabies exposures in 2018 was lower. This study also illustrated similarly low utilization in personal protective practices by wildlife professionals in both 2008 and 2018. Overall low awareness of certain zoonoses and reasons for PPE non-use highlight targets for education to improve practices. Additionally, differences in PPE use or behavior were demonstrated in multiple areas over the 10-year period between the surveys.
Ensuring that wildlife professionals working with animals, especially those who handle bats, receive PrEP is a priority. Bats are the most commonly identified rabies-positive wildlife species in Arizona (ADHS 2018). In addition to multiple bat strains of rabies, other rabies strains endemic in Arizona are the grey fox variant and the south-central skunk variant. Frequent spillover of endemic strains is observed into other species including bobcats, coyotes, and others (ADHS 2018). In scenarios where wildlife professionals do not receive PrEP, if they are bitten or scratched by a rabies reservoir or spillover species, rabies post-exposure prophylaxis (PEP) (human rabies immune globulin and a series of four or five rabies vaccines) is an option; even with PrEP, two boosters of the rabies vaccine are usually recommended as PEP if a potential rabies exposure has occurred (Rupprecht et al. 2010). Eighty percent of 71 wildlife workers from 14 countries in one study reported rabies vaccination (Garland-Lewis et al. 2017), which is higher than our surveys and could be related to differences in local rabies epidemiology and vaccination requirements. In our 2018 survey, when reviewing reasons as to why high-risk respondents with exposure to the common rabies spillover species might have been unvaccinated, one wildlife control professional reportedly was told only veterinarians could receive the vaccine, making it inaccessible. This finding may indicate an ongoing need for responsibility among employing agencies to provide their workers with opportunities to receive PrEP (since private insurance might not cover PrEP), education of wildlife professionals to empower them to pursue appropriate PrEP, and physician education of the risks and need for wildlife professionals to receive PrEP.
The overall percentage of survey respondents bitten by animals (considered a potential rabies exposure) was similar between surveys, but the frequency of bites from rabies reservoir or spillover species was 2.6-fold lower in 2018 compared to 2008 (16% vs 42%). These results might indicate more rabies risk awareness or training among wildlife professionals, fewer people handling difficult-to-handle or more aggressive bats and other rabies spillover species in the later survey, or simply an artifact related to the non-standardized selection of survey respondents. One study of 71 participants in 14 countries found significant lifetime exposures reported of bites from bats and rodents, so bites appear to be a more widespread issue (Garland-Lewis et al. 2017).
Regarding zoonotic disease knowledge, based on the wildlife that respondents have direct contact with, the diseases of highest risk for zoonotic disease exposure in Arizona other than rabies include hantavirus, leptospirosis, plague, tularemia, brucellosis, and tuberculosis. Regarding other vector-related diseases, tick-borne Rocky Mountain spotted fever is endemic on tribal lands in Arizona; Rick-etssia rickettsia transmission is driven by the presence of dogs; however, the burden in and role of coyotes in driving human risk is less known. Therefore, the risk to wildlife professionals is considered low although there are other tick-borne diseases throughout the state such as Rickettsia parkeri rickettsiosis or relapsing fever. There is currently no evidence that chronic wasting disease has infected humans, but the possibility cannot be ruled out. Additionally, although the most common way humans are infected with brucellosis remains eating or drinking contaminated unpasteurized milk products, transmission has also occurred when processing contaminated organs from freshly killed brucellosis infected livestock, wildlife, or feral swine. Lastly, wildlife professionals could be at risk for exposure to other zoonotic and vector-borne diseases not mentioned, including mosquito-borne diseases such as West Nile virus which is endemic in Arizona, due to the nature of their outside work. Risk perception in one national survey found that an index of severity, susceptibility, and dread was greatest for rabies and West Nile virus disease (Hanisch-Kirkbride et al. 2013). The most important variables associated with disease risk perception in that study were gender, education, prior exposure to the disease, and concern for health effects.
For wildlife professionals with animal contact, the NPS recommends a set of standard precautions when working with low-risk healthy animals, and these recommendations change as risk increases (National Park Service 2009). For example, the necropsy of an ill animal necessitates the addition of gloves, protective clothing, eye protection, and “respiratory protection as appropriate to the level of disease risk.” (National Park Service 2009; Miller et al. 2012). Previous literature addressing wildlife professionals’ engagement in prevention practices is limited. However, the national online survey conducted in 2009 of NPS wildlife workers revealed hand hygiene and gloves to be the most frequently reported protective measure used (Bosch et al. 2013). Respondents of the NPS survey reported that having PPE stocked and readily available (92%), having specific PPE kits available during necropsies (91%), and in remote field settings (91%) would facilitate PPE use. Another survey by Garland-Lewis et al. 2017 found that while gloves were used for most tasks, use of N95 respirators and other PPE varied by task.
Consistent and correct PPE use in accordance with the Occupational Safety and Health Administration standard (29 CFR 1910.132) is critical, as protection is only as effective as the materials used and the way they are utilized. Protection for workers should follow the hierarchy of controls that incorporate the following from most to least effective: elimination, substitution, engineering controls, administrative controls, and PPE. Due to the nature of the work wildlife professionals have with animals, many of the more effective controls such as elimination (not having any contact with certain animal species) are not feasible. Administrative controls such as employer policies to guide PrEP; safe handling of animals, tools, and specimens; and PPE use are practical methods to protect wildlife professionals from the occupational hazard of rabies. These controls need to be reinforced through institutional worker safety programs and occupational health.
Diseases other than rabies might carry a higher risk to wildlife professionals due to the absence of PrEP, complacency when handling samples, and gaps in PPE use as a result of forgotten or unknown risk by the user. In our 2018 survey, the most commonly cited reason for PPE non-use in given scenarios was a belief that it was not required. There were no differences observed between the respondents’ PPE use and years of experience, highest education received, or knowledge of diseases carried by wildlife or wildlife-associated arthropods within Arizona. It has previously been shown that perception of risk influences PPE use and risky behavior in a variety of occupational settings (Callahan et al. 2016; Johnston et al. 2014; National Park Service 2009). Poorly fitting or uncomfortable PPE also reduces use and exposes professionals to hazards (Lombardi et al. 2009). Due to the nature of some professionals’ work being outdoors, and the average high temperature in Arizona being 87 °F, comfort as it relates to weather might play a role in the use of certain types of PPE. However, we did not assess if the work with wildlife primarily occurred indoors or outdoors, or if the season or temperature played a role in PPE use.
This study was subject to certain limitations. Due to the distribution method in which multiple partner agencies and organizations dispersed the survey to their employees, an exact response rate could not be calculated. However, we calculated an estimated response rate of 55% in 2008 and 33% in 2018. Furthermore, a specific eligibility question was not included in the survey, so potentially people who do not work with wildlife in Arizona received the survey. This limitation adds to the authors’ challenge of accurately estimating the target population. The groups that received the survey consisted of convenience samples of agencies and organizations with available email addresses, and not all individuals who are exposed to wildlife as part of their profession received the survey, such as animal control workers and zoological facility staff who may have contact with wildlife. Surveys were anonymous and respondents could not be matched across surveys, resulting in the additional potential differences between the survey administered in 2008 and 2018. Direct comparisons in knowledge and practices of respondents were limited since the 2008 and 2018 populations were not the same, therefore independent proportions were used. Periodic surveys using standardized sampling methodologies would therefore be beneficial to compare groups and assess trends.
These survey results have been shared with wildlife agencies in Arizona. In between the two surveys, NPS issued Service-wide guidelines for safe handling of wildlife, including recommendations on the appropriate use of PPE as guided by the local prevalence of disease, potential routes of transmission, and the relative risk of species-specific activities (National Park Service 2009; Wong et al. 2009). Protocols and policies, including active managerial oversight for necropsies and other work conducted by biologists were also developed. The Arizona Department of Health Services agency who provided the Arizona-specific survey in 2008 developed new educational materials to distribute state-wide to all wildlife professionals. Future proposed collaborative (state health department and wildlife agencies) research goals include performing a more-detailed assessment of the scenarios in which professionals are and are not utilizing PPE, and evaluating specific training programs that employees within agencies receive; reviewing institutional policies could also be informative to help establish a culture of safety from the top down. The information gathered from these activities would guide training efforts to areas of highest importance through risk assessment, reduce duplicative or unnecessary training, and save employee and agency resources. Many factors, including peer-pressure and leading by example at the peer and organizational levels, as well as other modes of agency support (e.g., availability of appropriate PPE, requirement of training on and PPE use) have been demonstrated to increase PPE use compliance (Lombardi et al. 2009; Mauldin et al. 2016). Mandating use or requiring employees to follow standard operating procedures could be pursued, and should be pursued to comply with state or local laws as applicable. Appropriate PPE use will best protect workers without being unnecessarily burdensome and costly. Additionally, assessments could be performed to determine what specific agency requirements and options exist for rabies PrEP prior to vaccination among high-risk employees, and to consider if there are sustainable policies within these agencies that support coverage of employees’ pre-vaccination costs. We plan to perform a thorough assessment and evaluate employee rabies vaccination policy changes over time.
Rabies PrEP and serum antibody testing in wildlife personnel at risk is a prudent step, as well as targeted PPE use in risk-based scenarios. Appropriate and frequent continuing education or training for wildlife professionals on these protective measures can help ensure that wildlife professionals are well-equipped to be their own advocates to prevent unnecessary illness or injury as a direct result of their work.
Acknowledgments
We thank Anne Justice-Allen, Chasa O’Briean, Lisa Shender, and the Arizona Game and Fish Department, David Bergman (USDA, APHIS, Wildlife Services), Kenneth Komatsu, Sonya Shannon, Caleb Wiedeman, and the Arizona Department of Health Services, Brant Goode, John Gibbins, Jessica Rinsky, and the Centers for Disease Control and Prevention, and Yue Qui and Arizona State University. This study was funded as part of normal routine activities by the Arizona Department of Health Services and Centers for Disease Control and Prevention.
Footnotes
Publisher's Disclaimer: Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the U.S. Centers for Disease Control and Prevention or the U.S. Department of Health and Human Services.
References
- Arizona Department of Health Services (2018) Rabies—data, publication, and maps. https://www.azdhs.gov/preparedness/epidemiology-disease-control/rabies/#data-publications-maps. Accessed August 15, 2018.
- Arizona Department of Health Services (2019) Infectious disease epidemiology 2010–2015 report. https://www.azdhs.gov/documents/preparedness/epidemiology-disease-control/disease-data-statistics-reports/infectious-disease-epidemiology-report-2010-2015.pdf. Accessed January 17, 2019.
- Baker WS, Gray GC (2009) A review of published reports regarding zoonotic pathogen infection in veterinarians. J Am Vet Med Assoc 234(10):1271–1278 [DOI] [PubMed] [Google Scholar]
- Bosch SA, Musgrave K, Wong D (2013) Zoonotic disease risk and prevention practices among biologists and other wildlife workers–results from a national survey, US National Park Service, 2009. J Wildl Dis 49(3):475–585 [DOI] [PubMed] [Google Scholar]
- Callahan A, Ames NJ, Manning ML, Touchton-Leonard K, Yang L, Wallen R (2016) Factors Influencing Nurses’ Use of Hazardous Drug Safe-Handling Precautions. Oncol Nurs Forum 43(3):342–349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2011) Preexposure vaccinations. https://www.cdc.gov/rabies/specific_groups/travelers/pre-exposure_vaccinations.html. Accessed January 10, 2019.
- Garland-Lewis G, Whittier C, Murray S, Trufan S, Rabinowitz PM (2017) Occupational Risks and Exposures Among Wildlife Health Professionals. Ecohealth 14(1):20–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanisch-Kirkbride SL, Riley SJ, Gore ML (2013) Wildlife Disease and Risk Perception. J of Wildlife Diseases 49(4):841–849 [DOI] [PubMed] [Google Scholar]
- Johnston JD, Eggett D, Johnson MJ, Reading JC (2014) The influence of risk perception on biosafety level-2 laboratory workers’ hand-to-face contact behaviors. J Occup Environ Hyg 11(9):625–632 [DOI] [PubMed] [Google Scholar]
- Jones KE, Patel NG, Levy MA, Storeygard A, Balk D, Gittleman JL, Daszak P (2008) Global trends in emerging infectious diseases. Nature 451(7181):990–993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lombardi DA, Verma SK, Brennan MJ, Perry MJ (2009) Factors influencing worker use of personal protective eyewear. Accid Anal Prev 41(4):755–762 [DOI] [PubMed] [Google Scholar]
- Mauldin MR, Doty JB, Nakazawa Y, Emerson GL, Carroll DS (2016) The importance of mammalogy, infectious disease research, and biosafety in the field. Manter (Linc) 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller JM, Astles R, Baszler T, Chapin K, Carey R, Garcia L, Gray L, Larone D, Pentella M, Pollock A, et al. (2012) Centers for disease control and prevention. Guidelines for safe work practices in human and animal medical diagnostic laboratories. Recommendations of a CDC-convened, Biosafety Blue Ribbon Panel. MMWR Suppl 61(1):1–102 [PubMed] [Google Scholar]
- National Park Service (2009) National park service occupational safety and health program; reference manual 50B. https://www.nps.gov/policy/RM50Bdoclist.htm.
- Rupprecht CE, Briggs D, Brown CM, Franka R, Katz SL, Kerr HD, Lett SM, Levis R, Meltzer MI, Schaffner W, et al. (2010) Use of a reduced (4-dose) vaccine schedule for postexposure prophylaxis to prevent human rabies: recommendations of the advisory committee on immunization practices. Morbidity and Mortality Weekly Report 59(RR-2):1–9 [PubMed] [Google Scholar]
- Vitek CR, Ksiazek TG, Peters CJ, Breiman RF (1996) Evidence against infection with hantaviruses among forest and park workers in the southwestern United States. Clin Infect Dis 23(2):283–285 [DOI] [PubMed] [Google Scholar]
- Williams CJ, Cheftel JM, Elchos BL, Hopkins SG, Levine JF, Association NationalNational Association for State Public Health Veterinarians (2015) Compendium of Veterinary Standard Precautions for Zoonotic Disease Prevention in Veterinary Personnel. J Am Vet Med Assoc 247:1252–1277 [DOI] [PubMed] [Google Scholar]
- Wong D, Wild MA, Walburger MA, Higgins CL, Callahan M, Czarnecki LA, Lawaczeck EW, Levy CE, Patterson JG, Sunen-shine R, et al. (2009) Primary pneumonic plague contracted from a mountain lion carcass. Clin Infect Dis 49(3):e33–e38 [DOI] [PubMed] [Google Scholar]


