Introduction
As the COVID-19 (coronavirus disease 2019) pandemic spreads globally, our knowledge about its myriad presentations continues to evolve. Here we present a case of a patient with COVID-19 who rapidly succumbed to death after presenting to the emergency room (ER) with apparent acute myocardial infarction (MI).
Case report
A 72-year-old man with history of hypertension presented to the ER in early April of 2020 via ambulance with complaints of chest tightness and a feeling of impending doom. He described shortness of breath, cough, fatigue, and intermittent diarrhea for the preceding few days. He had not sought any prior regular medical care.
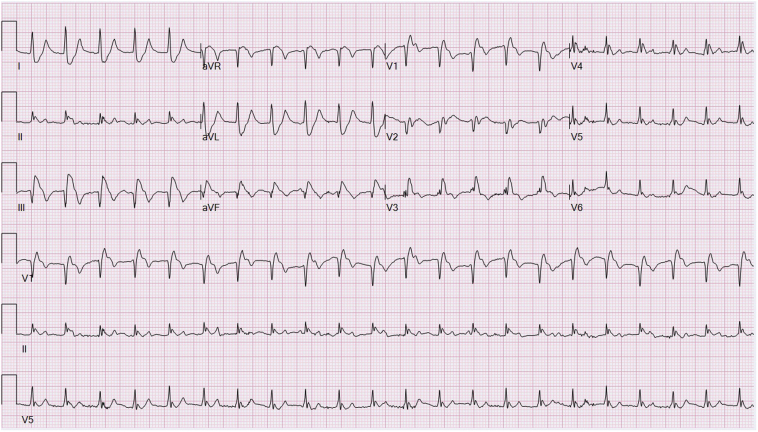
Paramedic evaluation demonstrated an afebrile male in obvious distress with chest pain and shortness of breath. An electrocardiogram (ECG) done in the field was interpreted as acute ST-elevation MI. The initial ECG on arrival in the ER is shown in Figure 1. Blood pressure was 158/110. He was hypoxic and was placed on high-flow oxygen. He was moved to a respiratory isolation room while being prepared for emergent cardiac catheterization.
Figure 1.
Initial electrocardiogram.
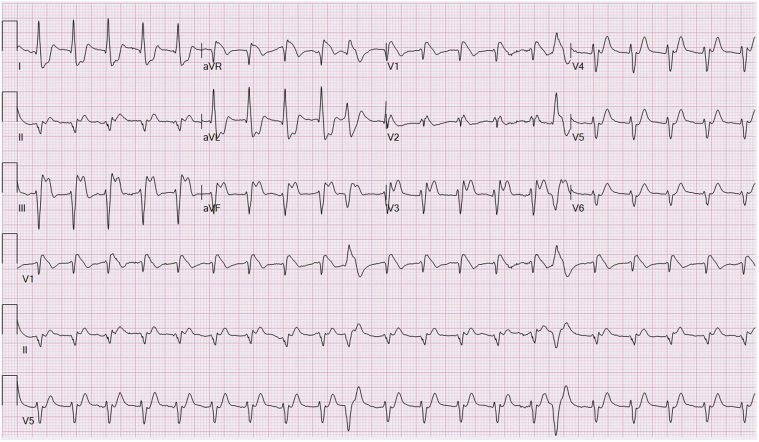
Within a few minutes of arrival in the ER, the patient suddenly became unresponsive and pulseless. Resuscitation was started and the patient was emergently intubated. He had brief return of spontaneous circulation, at which time a second ECG was done (shown in Figure 2). However, he was persistently hypotensive and eventually became pulseless again. After 45 minutes of rigorous efforts, resuscitation was terminated after team discussion and the patient was pronounced dead. At the coroner’s request, a sample for SARS-Cov-2 was sent which subsequently returned positive. Other laboratory tests could not be drawn prior to the patient’s deteriorating hemodynamically. Autopsy was not performed.
Figure 2.
Electrocardiogram after brief return of spontaneous circulation during the resuscitation.
Discussion
This case shows rapid deterioration, sustained ventricular tachycardia (VT), and sudden cardiac death in a COVID-19 patient. It is likely that COVID-19 appears to be a significant factor in the clinical course.
Figure 1 shows a wide-complex tachycardia at rate of 134 beats per minute (bpm) and QRS width of 140 ms. P waves are noted at cycle length of 1200 ms (50 bpm) and AV dissociation is noted. This is consistent with VT and not a supraventricular rhythm with ST-elevation MI. The QRS morphology suggests origin from the inferoseptal left ventricle. A junctional ectopic tachycardia with V-A block is also a less likely possibility. Figure 2 shows a slower tachycardia (123 bpm) with QRS width of 148 ms. There is a significant loss of R wave across precordial leads and no discernible P waves noted. Premature ventricular contractions are noted that appear to reset the tachycardia, which could suggest a reentrant mechanism vs fortuitous cycle length variation. There is no prior history of MI or Q waves in inferior leads. This is likely VT originating from the inferoapical left ventricular septum.
It is noteworthy that during the SARS (sudden acute respiratory syndrome) outbreak of 2002, extrapulmonary manifestations were common, but cardiac manifestation were not very prominent.1 Transient arrhythmias, cardiomegaly, and ventricular dysfunction were reported but were self-limiting or required minimal intervention, and myocarditis was not mentioned.2,3 During the MERS (Middle East respiratory syndrome) outbreak, a case of myocarditis was reported.4 Acute viral myocarditis can be fulminant and may sometimes mimic acute MI and cause arrhythmias.5 Patients with COVID-19 can deteriorate rapidly with shock and multiorgan failure. There are also reports suggesting significant cardiac injury and arrhythmias in COVID-19 patients.6,7 Fulminant myocarditis has been reported in COVID-19 patients.8 Although it is possible that COVID-19 was a mere bystander in this patient, his history of COVID-19-related symptoms, acute respiratory failure, and atypical ECG findings, as well as precipitous course, point towards myocarditis.
Conclusion
Timely recognition and treatment of acute cardiac events in the ER during the COVID-19 pandemic presents a unique challenge. Based on the limited clinical and published data, we suspect that our patient may have had acute cardiac injury and myocarditis masquerading as acute MI, likely owing to COVID-19, leading to malignant VT and, finally, sudden death. Careful attention should be given to COVID-19 as a possible etiology, and prophylactic personal protective equipment should be used in patients presenting with suspected acute MI, acute heart failure, and ventricular arrhythmias.
Key teaching points.
-
•
Acute cardiac injury, ST elevation, and ventricular arrhythmias can occur in myocarditis, especially in association with acute viral illnesses such as COVID-19.
-
•
Acute cardiac presentations like this can lead to very rapid deterioration and death.
-
•
It is important to keep viral myocarditis in the differential diagnosis in critically ill patients, especially during a pandemic such as COVID-19.
Footnotes
Funding: No funding resources/grants were involved.
References
- 1.Sellers S.A., Hagan R.S., Hayden F.G. The hidden burden of influenza: a review of the extra-pulmonary complications of influenza infection. Influenza Other Respir Viruses. 2017;11:372–393. doi: 10.1111/irv.12470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yu C., Wong R.S., Wu E.B. Cardiovascular complications of severe acute respiratory syndrome. Postgrad Med J. 2006;82:140–144. doi: 10.1136/pgmj.2005.037515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xiong T.Y., Redwood S., Prendergast B. Coronaviruses and the cardiovascular system: acute and long-term implications. Eur Heart J. 2020;41:1798–1800. doi: 10.1093/eurheartj/ehaa231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alhogbani T. Acute myocarditis associated with novel Middle East respiratory syndrome coronavirus. Ann Saudi Med. 2016;36:78–80. doi: 10.5144/0256-4947.2016.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cooper L. Myocarditis. N Engl J Med. 2009;360:1526–1538. doi: 10.1056/NEJMra0800028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dawei W., Bo H., Chang H. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen C., Zhou Y., Wang D.W. SARS-CoV-2: a potential novel etiology of fulminant myocarditis. Herz. 2020;45:230–232. doi: 10.1007/s00059-020-04909-z. [DOI] [PMC free article] [PubMed] [Google Scholar]