To the Editor:
The coronavirus disease 2019 (COVID-19) pandemic has placed tremendous strain on health care systems worldwide, in terms of both patient care in several geographic areas and, more globally, in planning for its anticipated surge. In preparation for increased numbers of patients with severe respiratory compromise, many hospitals have intentionally reduced nonemergent procedures and hospitalizations to preserve hospital capacity and personal protective equipment. In some places, state directives mandate these actions. Such plans and directives should not influence admissions from the emergency department for acute cardiovascular conditions, including heart failure (HF).
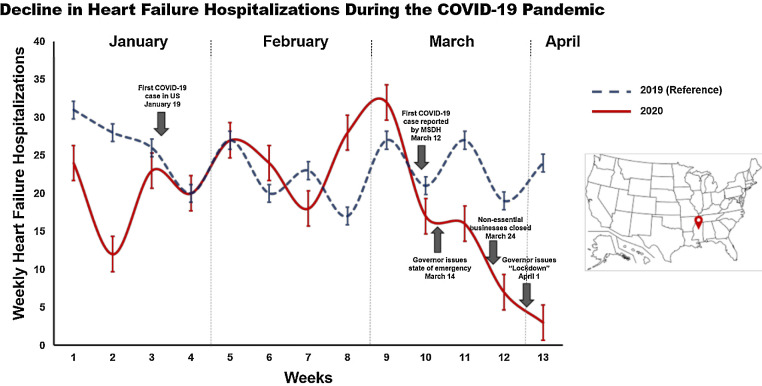
We examined trends in hospitalizations due to HF across a large, tertiary care, academic medical center by using the electronic health record system and hospital discharge database. Hospitalizations with principal diagnoses of HF (acute or acute or chronic, based on ICD-10 codes) were included in this analysis. We examined weekly hospitalizations for HF beginning in January 2020, prior to the first case of COVID-19 in the United States1 through April 11. We also compared trends in hospitalizations for HF from 2019, during the same time period, to account for the potential of residual confounding based on seasonal trends in hospitalizations for HF. All HF subtypes, including HF with reduced ejection fraction (HFrEF), preserved ejection fraction (HFpEF) and midrange ejection fraction (HFmrEF) subtypes were included in this analysis.
Weekly hospitalizations for HF by year (2019 and 2020) are displayed in Fig. 1, along with important events related to the pandemic. In the 2 weeks prior to the first diagnosed case of COVID-19 in Mississippi, cases of HF averaged 30 per week. After the first diagnosed case in Mississippi, mean hospitalizations because of HF declined by 50% to 15 per week. Hospitalizations for HF continued to decline to lower levels after a state of emergency was declared, and they declined even further after the statewide shelter-in-place order was mandated; there were fewer hospitalizations for HF in the last 2 weeks of this analysis. Although we observed week-to-week variability in hospitalizations due to HF in 2019, we did not observe significant and progressive declines similar to those noted during the current COVID-19 pandemic. Before the first case of COVID-19 was identified in the state of Mississippi, 68.1% of cases of HF were of the HFrEF subtype, 22.4% were HFpEF and 9.5% were HFmrEF. We observed a very similar distribution of HF subtypes after March 12, including 65.9% HFrEF, 26.8% HFpEF and 7.3% HFmrEF.
Fig. 1.
Trends of hospitalizations due to heart failure at the University of Mississippi Medical Center from January through April 11, 2020 (red line) and the same time window in 2019 (dashed blue line).
Our observations from a large, tertiary care, academic medical center indicate that there was a marked decline in hospitalizations because of HF during the COVID-19 pandemic. With rare exceptions, most hospitalizations for HF are nonelective and represent worsening congestion that can have significant impacts on patients’ outcomes if the congestion is not treated or delayed. Theoretically, these hospitalizations are not expected to be affected by hospital or health-authority policies. This is particularly true for large, tertiary care referral centers that offer advanced therapies. On the other hand, such centers are likely also to take care of many of the sickest patients with COVID-19. Therefore, it is possible that patients with non-COVID-19-related illnesses may be concerned about the potential of their own risk for nosocomial infection when in the hospital receiving treatment for other, urgent medical conditions such as HF. Importantly, there was no announcement from either the health system or the state health department level to divert patients with certain medical conditions to specific hospitals. To this point, there were similar numbers of transfers because of HF to our institution before and during the COVID-19 pandemic (mean 4.0 ± 2.8 vs 3.0 ± 1.8 transfers per week, respectively).
A major concern is that these declines in hospitalizations because of HF may be due to patients’ fears of medical facilities and the “weathering-the-storm” mentality of patients until the COVID-19 pandemic abates. Further urgent attention to understanding and mitigating these patterns, including plans for alternative monitoring and therapeutic approaches to improve treatment of HF, are warranted during these unprecedented times.
Acknowledgment
The authors thank Mrs. Melissa Stampley for her assistance in the collection of the hospitalization data relating to HF.
Funding
MH is funded by grants from the National Institutes of Health grants 1K08DK099415 (NIDDK) and 5U54GM115428 (NIGMS).
Disclosures
MV is supported by the KL2/Catalyst Medical Research Investigator Training award from Harvard Catalyst (NIH/NCATS Award UL 1TR002541) and serves on advisory boards for Amgen, AstraZeneca, Baxter Healthcare, Bayer AG, Boehringer Ingelheim, Cytokinetics, and Relypsa. JB declares that he serves as a consultant for Abbott, Adrenomed, Amgen, Array, Astra Zeneca, Bayer, Boehringer Ingelheim, Bristol Myers Squib, CVRx, G3 Pharmaceutical, Impulse Dynamics, Innolife, Janssen, LivaNova, Luitpold, Medtronic, Merck, Novartis, NovoNordisk, Relypsa, Roche, V-Wave Limited, and Vifor. All other coauthors have nothing to disclose.
Reference
- 1.Holshue ML. DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, Spitters C, et al.,Washington State 2019-nCoV Case Investigation Team. First case of 2019 novel Coronavirus in the United States. N Engl J Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]