Abstract
We reported a 33-year-old female case with novel coronavirus disease 2019 (COVID-19) accompanied by Acute tubular necrosis (ATN). She had a gestational age of 34 weeks. The patient referred to treatment clinic for COVID-19 in Imam Reza hospital of Tabriz (Iran) after having flu-like symptoms. In radiologic assessment, ground glass opacity (GGO) with consolidation was found in upper right lobe. Lopinavir/ritonavir (200mg/50mg) two tablet tow times, Ribavirin 200mg every 6 h, and Oseltamivir 75mg tow times were given for the treatment of COVID-19. The medications used for treatment of pneumonia were Meropenem, Ciprofloxacin, Vancomycin. All doses of medications were administrated by adjusted dose assuming the patient is anephric. Also, a few supplements were also given after ATN development including daily Rocaltrol and Nephrovit (as a multivitamin appropriate for patients with renal failure), Folic acid and Calcium carbonate. The patient is still under ventilator with a Fraction of inspired oxygen (FiO2) of 60% and Positive end-expiratory pressure (PEEP) of eight. SpO2 is 94% but the patient's ATN problem has been resolved. We started weaning from mechanical ventilator. The patient is conscious with full awareness to time, person and place. The maternal well-being is achieved and her neonate was discharged.
Keywords: Pregnancy, SARS-CoV-2, ATN, Kidney, Infection, Renal involvement
1. Introduction
Coronaviruses are a large family of viruses that were first discovered in 1960. They cause common cold in humans and animals, and are characterized by their crown-like thrones on the wall surfaces of viruses. Such sever diseases emerged in the last 20 years responsible for severe symptoms including SARS-CoV-2 which is the cause of the ongoing pandemic [1,2]. Symptoms of coronavirus appear in the lungs with pneumonia, which is usually associated with mild cold in most people. But there are some types of the virus that are associated with more severe symptoms such as Severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS), and SARS-CoV-2 causing COVID-19 [3]. Finally, on December 2019, for the first time in Wuhan city of China, a new type of coronavirus was identified with a human epidemic after people contracted pneumonia and vaccines and treatments were ineffective, so that named COVID-19 [4]. Depending on the type of coronavirus, symptoms can range from symptoms of common cold to fever, cough, shortness of breath and acute respiratory problems [5,6]. The patient with COVID-19 may also have a few days of apparently unexplained coughs that affect not only the respiratory tract but also other vital organs of the body such as the kidney and liver. Acute gastrointestinal problems such as diarrhea, acute respiratory failure, coagulation disorders and acute renal failure have also been reported that may require hemodialysis [[7], [8], [9]]. We would like to report a case of pregnant woman with COVID-19 who developed acute tubular necrosis (ATN).
2. Case report
A 33-year-old female without comorbidity who had symptoms of the cold a week ago referred to treatment clinic for COVID-19 in Imam Reza hospital of Tabriz, Iran. After Polymerase chain reaction (PCR) test through the nasopharyngeal swab and radiologic examination, she was hospitalized. The symptoms worsened and she was intubated on the second day. The patient was also pregnant with a gestational age of 34 weeks. Lopinavir/ritonavir (200mg/50mg) two tablet tow times, Ribavirin 200mg every 6 h, and Oseltamivir 75mg tow times were given for the treatment of COVID-19. The medications used for treatment of pneumonia were Meropenem, Ciprofloxacin, Vancomycin. All doses of drugs were administrated by adjusted dose assuming the patient is anephric. This study have been approved by the Medical Ethics Committees of Tabriz university of medical sciences before patient enrollment and treatment (Approval ID: IR.TBZMED.REC.1398.1314).
The patient did not receive nephrotoxic drugs such as antibiotics before uremia, and when her BUN and Cr increased, the patient's urine became muddy brown and the volume of urine decreased, and we called it Acute kidney injury (AKI). In our urine sedimentation, there were a lot of granular casts along with cellular debris, which was interpreted as ATN. Due to the presence of urinary sedimentation and the presence of granuloma casts in the urine and muddy brown nature of urine, the diagnosis of ATN was more important than urinary toxicity. In spite of using Furosemide, urine output was 600 cc in 24 hours. After hemoperfusion, urine output reached above 2 L in 24 hours and we entered the polyuria phase.However, Vancomycin was eliminated and Linzolid started for the patient because it is not nephrotoxic.
Also, a few supplements were also prescribed after developing ATN including daily Rocaltrol and Nephrovit (as a multivitamin appropriate for patients with renal failure), Folic acid and Calcium carbonate. Vitamin C 250 mg is administrated by gavage. Hemoglobin and white blood cell at admission time were 11 mg/dl and 2400 per microliter, respectively; so that pancytopenia was diagnosed and suspected of having lupus erythematous. Therefore, rheumatology consultation was asked, all of lupus diagnostic criteria were negative but received Intravenous immunoglobulin (IVIG) 5 gr daily for 5 consecutive days after consultation with hematologist.
The patient did not have peripheral schistocyte in the blood, we did not make diagnoses such as microangiopathy (thrombotic thrombocytopenic purpura-hemolytic uremic syndrome: TTP-HUS) and only Collagen vascular disease (CVO) due to anemia and vascular thrombocytopenia was evaluated. The patient's anemia and thrombocytopenia improved after hemoperfusion and the patient had an increase in hemoglobin and platelets. The patient's electrolytes were regularly monitored. As mentioned, due to the lack of schistocyte in the peripheral blood, microangiopathy was ruled out. Lupus tests including C3, CH50, Cu and Anti-dsDNA were negative. Primary LDH was 1360 that decreased to 380 after hemoperfusion. Serum glutamic oxaloacetic transaminase (SGOT) and Serum glutamic pyruvic transaminase (SGPT) were 78 and 46 units per liter of blood serum, respectively.
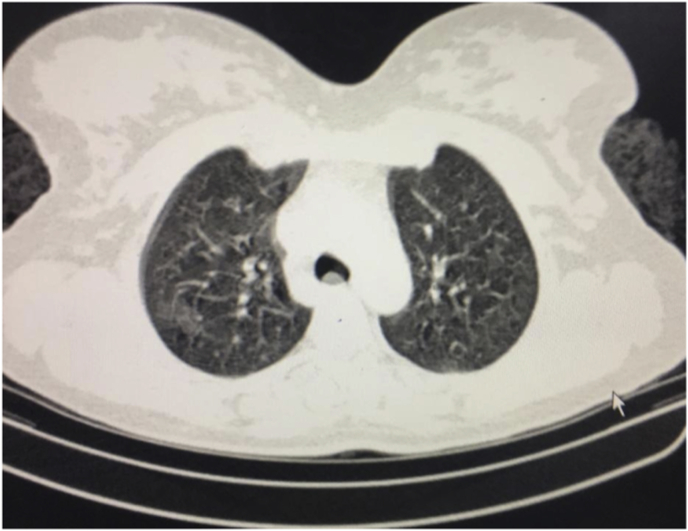
The patient's PCR test was positive, so a CT scan was taken and showed ground glass opacity (GGO) with consolidation in upper right lobe indicating lung involvement. Preoperative CT is presented when the patient was not intubated yet (Fig. 1). After admission, creatinine levels gradually increased up to 6.8 mg/dl accompanied by respiratory and metabolic acidosis in the arterial blood gas (ABG). The patient's respiratory rate increased to 36 breaths/minute and the patient was intubated. She underwent caesarean section after consultation with a gynecologist. he patient had to undergo dialysis 12 hours before caesarean section. The baby was negative for COVID-19 and was in good health. Due to the low platelet count, the patient entered the operating room with 10 platelet injections. Before surgery Hb was 7.25 mg/dl (Blood Pressure = 100/66 mmHg, prothrombin time (PT) = 16s, partial thromboplastin time (PTT) = 36s, Pco2 = 45 mmHg, Hco3 = 18 mEq/L).
Fig. 1.
Perioperative CT scan of intubated patients with COVID-19.
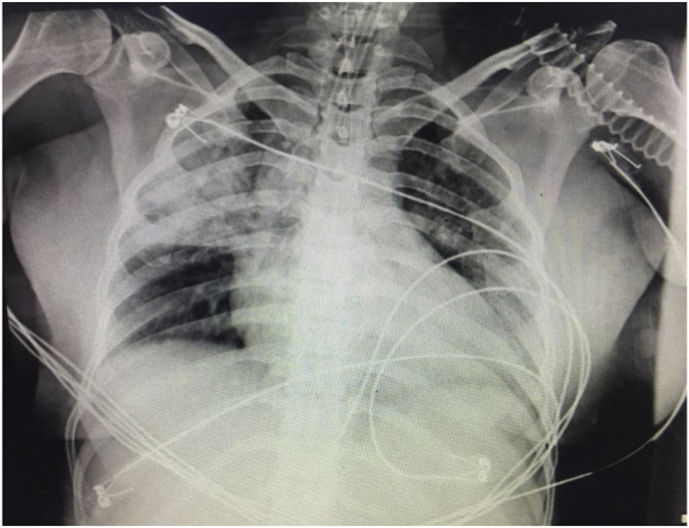
After surgery, hemoglobin had reached 7.8 mg/dl, which inevitably received a unit washed packed cell, and hemoglobin is now 9.5 mg/dl. White blood cell (WBC) increased to 7,400 per microliter. On the sixth day of hospitalization, diuresis was established, and the patient's creatinine declined sharply. The patient's creatinine had reached 3 mg/dl and conservative treatment was launched. The patient is still hospitalized due to COVID-19 and is in the recovery phase with fluid control and does not receive medication for her ATN. The patient is still intubated with a fraction of inspired oxygen (FiO2) of 60% and Positive end-expiratory pressure (PEEP) of eight. SpO2 is 94% but the patient's ATN has been resolved. We started weaning the mechanical ventilation. The patient is conscious with full awareness to time, person and place. The maternal well-being is achieved and her neonate was discharged. Postoperative Chest-x ray is presented (Fig. 2). As shown, pneumonia is clear in the figure that's why the patient is giving Ciprofloxacin, Vancomycin and Meropenem now.
Fig. 2.
Postoperative Chest-x ray of intubated patients with COVID-19.
3. Discussion
We know that COVID-19 involve multiple organs, in such a way that renal failure was reported in two studies [[10], [11], [12], [13], [14]]. Due to low studies in favor of kidney disease and COVID-19, it is hard to make decision in this regard, but what we've seen is the fact that ATN is treated by supportive measure [15]. Maybe routine measures are sufficient, so that kidney replacement therapy is another choice for the treatment of these patients if necessary. Indeed supportive measure can be efficient. So far, no effective antiviral drug was found to treat COVID-19 patients; therefore new drug cannot be named and prescribed without approved results [16]. Various viruses can cause ATN such as Lassa and others [17], and in our case report, SARS-CoV-2 caused ATN. In pregnant women, the manifestation of chest graph does not differ so that the most common finding in corona-positive patients with pneumonia was GGO [18,19]. The reported case had GGO in upper right lobe. The clinical manifestation of pregnant women with COVID-19 is the same other non-pregnant women [[20], [21], [22]]. Given these finding, we did the same and treat like other people. But regarding CT scan, we took it conservatively due to her pregnancy and getting low radiation. Taking chest X-ray was not limited and when it was necessary, we checked it. After delivery and checking the COVID-19 status in the neonate, we found that neonate are resistant to corona virus than of adults because PCR test was negative. Previously, two neonatal cases of COVID-19 have been reported without severe symptoms [23]. The risk of vertical transmission of novel corona virus is low but never reach zero and prevention measure in any levels should be adapted [23,24]. The exact pathology of AKI in patients with COVID-19 was not known but the role of angiotensin-converting enzyme 2 (ACE2) was reported [25]. We know that AKI is happen infrequent in pregnant women. To prevent the development of AKI in patients with mild renal insufficiency such as increase in creatinine potentially can reduce the likelihood of AKI development. In this regard, we made a decision that the patient should undergo hemodialysis to prevent the development of AKI and fortunately we were successful [26]. In a study by Wang et al., SARS-CoV-2 RNA was found in 53 urine sediments through real-time reverse transcription-polymerase chain reaction [27].
4. Conclusion
These case report and other related study indicate the effect of COVID-19 on the development of acute renal failure. Also, AKI is not common in patients with COVID-19. That is why we report this case. The rarity of the AKJ neglects physicians to differentiate this disease in the examination. In conclusion, it is concluded that renal involvement with COVID-19 is the main reason of ATN. We ruled out pre-renal and post-renal reasons to develop ATN. ATN in patients with COVID-19 can be easily treated using supportive-conservative measures. Other differential diagnosis of ATN should be COVID-19.
Declaration of competing interest
The authors report no conflicts of interest.
Acknowledgment
This study was supported by Tabriz University of Medical Sciences, Tabriz, Iran (Grant Number: 65203).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.rmcr.2020.101090.
Contributor Information
Majid Ahmadi, Email: Ahmadi.m@tbzmed.ac.ir.
Hamed Valizadeh, Email: H_valizadeh@yahoo.com.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- 1.Van der Hoek L., Pyrc K., Jebbink M.F., Vermeulen-Oost W., Berkhout R.J., Wolthers K.C., Wertheim-van Dillen P.M., Kaandorp J., Spaargaren J., Berkhout B. Identification of a new human coronavirus. Nat. Med. 2004 Apr;10(4):368–373. doi: 10.1038/nm1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee P.I., Hsueh P.R. Emerging threats from zoonotic coronaviruses-from SARS and MERS to 2019-nCoV. J. Microbiol. Immunol. Infect. 2020 doi: 10.1016/j.jmii.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carlos W.G., Dela Cruz C.S., Cao B., Pasnick S., Jamil S. Novel Wuhan (2019-nCoV) coronavirus. Am. J. Respir. Crit. Care. 2020 Feb 15;201(4):7–8. doi: 10.1164/rccm.2014P7. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization Naming the coronavirus disease (COVID-19) and the virus that causes it. 2019. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it Available at:
- 5.Vabret A., Dina J., Brison E., Brouard J., Freymuth F. Coronavirus humains (HCoV) Human coronaviruses. Pathol. Biol. 2009;57:149–160. doi: 10.1016/j.patbio.2008.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bai Y., Yao L., Wei T. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020 Feb 21;323(14):1406–1407. doi: 10.1001/jama.2020.2565. [published online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C., Liu S., Zhao P., Liu H., Zhu L., Tai Y. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020 Feb 18;8(4):420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mubarak M., Nasri N. COVID-19 nephropathy; an emerging condition caused by novel coronavirus infection. J. Nephropathol. 2020;9(3):e21. doi: 10.34172/jnp.2020.21. [DOI] [Google Scholar]
- 9.Hamidian Jahromi A., Mazloom S., Ballard D.H. What the European and American health care systems can learn from China COVID-19 epidemic; action planning using purpose designed medical telecommunication, courier services, home-based quarantine, and COVID-19 walk-in centers. Immunopathol. Persa. 2020;6:e17. [Google Scholar]
- 10.Anti -2019-nCoV Volunteers, Li Z., Wu M., Yao J., Guo J., Liao X. Caution on kidney dysfunctions of COVID-19 patients. medRxiv. 2020 doi: 10.1101/2020.02.08.20021212. 02.08.20021212. [DOI] [Google Scholar]
- 11.Cheng Y., Luo R., Wang K., Zhang M., Wang Z., Dong L., Li J., Yao Y., Ge S., Xu G. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020;97(5):829–838. doi: 10.1016/j.kint.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Valizadeh R., Baradaran A., Mirzazadeh A., Bhaskar L.V.K.S. Coronavirus-nephropathy; renal involvement in COVID-19. J. Ren. Inj. Prev. 2020;9(2):e18. doi: 10.34172/jrip.2020.18. [DOI] [Google Scholar]
- 13.Dadashzadeh N., Farshid S., Valizadeh R., Nanbakhsh M., Rahimi M.M. Acute respiratory distress syndrome in COVId-19 disease. Immunopathol. Persa. 2020:e16. doi: 10.34172/ipp.2020.16. [DOI] [Google Scholar]
- 14.Valizadeh R., Dadashzadeh N., Zakeri R., James Kellner S., Rahimi M.M. Drug therapy in hospitalized patients with very severe symptoms following COVID-19. J. Nephropharmacol. 2020;9:e21. doi: 10.15171/npj.2020.21. [DOI] [Google Scholar]
- 15.Nazar C.M.J., Bashir F., Izhar S., Anderson J. Overview of management of acute renal failure and its evaluation; a case analysis. J. Nephropharmacol. 2015;4(1):17–22. [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention What to do if you are sick with 2019 Novel Coronavirus (2019-nCoV) 2019. https://www.cdc.gov/coronavirus/2019-ncov/if-you-are-sick/steps-when sick.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fabout%2Fsteps-when-sick.html Available at:
- 17.Micarelli D., Moccia F., Costantini S., Feriozzi S. COVID-19 is a complex disease with wide spectrum of clinical patterns and an emerging problem for nephrologist. J. Nephropathol. 2020;9(4):e33. [Google Scholar]
- 18.Aleebrahim-Dehkordy E., Reyhanian A., Saberianpour S., Hassanpour- Dehkordy H. Acute kidney injury in COVID19. J. Nephropathol. 2020;9:e31. [Google Scholar]
- 19.Qiao J. What are the risks of COVID-19 infection in pregnant women? Lancet. 2020;395(10226):760–762. doi: 10.1016/S0140-6736(20)30365-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y., Qiu Y., Wang J., Liu Y., Wei Y., Yu T. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., Ren R., Leung K.S., Lau E.H., Wong J.Y., Xing X. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N. Engl. J. Med. 2020 doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Forouzesh M., Azadeh Rahimi, Valizadeh R., Dadashzadeh N., Mirzazadeh A. Clinical display, diagnostics and genetic implication of novel coronavirus (COVID-19) Eur. Rev. Med. Pharmacol. Sci. 2020;24(8) doi: 10.26355/eurrev_202004_21047. ahead of print. [DOI] [PubMed] [Google Scholar]
- 23.National Health Commission of the People’s Republic of China Transcript of press conference on Feb 7, 2020. http://www.nhc.gov.cn/xcs/s3574/20200 2/5bc099fc9144445297e8776838e57ddc.shtml accessed. in Chinese.
- 24.Chen H., Guo J., Wang C., Luo F., Yu X., Zhang W., Li J., Zhao D., Xu D., Gong Q., Liao J. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395(10226):809–815. doi: 10.1016/S0140-6736(20)30360-3. published online Feb 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tolouian R., Zununi Vahed S., Ghiyasvand S., Tolouian A., Ardalan M.R. COVID-19 interactions with angiotensin-converting enzyme 2 (ACE2)and the kinin system; looking at a potential treatment. J. Ren. Inj. Prev. 2020;9(2):e19. doi: 10.34172/jrip.2020.19. [DOI] [Google Scholar]
- 26.Van Hook J.W. Acute kidney injury during pregnancy. Clin. Obstet. Gynecol. 2014 Dec;57(4):851–861. doi: 10.1097/GRF.0000000000000069. Review. [DOI] [PubMed] [Google Scholar]
- 27.Wang L., Li X., Chen H., Yan S., Li D., Li Y., Gong Z. Coronavirus disease 19 infection does not result in acute kidney injury: an analysis of 116 hospitalized patients from Wuhan, China. Am. J. Nephrol. 2020 Mar 31:1–6. doi: 10.1159/000507471. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.