In late 2019, there were first reports of an outbreak of unknown-caused pneumonia from Wuhan, Hubei province, China. After a week of investigations, the novel coronavirus, COVID-19, was found as the etiologic factor (1). The virus was a mutated form of Coronaviridae family, which similar to many other respiratory viruses, was comprised of a RNA component covered by viral capsid protein, but acquired a novel genomic mutation, making it resistant to standard medications (2). Highly contagious with droplets and contact transmission, the virus might stay silent for a period of 2.4–15.5 d (3) and then manifests with flu-like symptoms, non-suppurative coughs, fever, diarrhea, myalgia, or even anosmia in some cases. The lungs will be the next victims and in severe cases, after a course of 1–2 weeks, the patients would die due to acute respiratory distress syndrome.
Although primarily reported to be originated from a seafood market in China, it was later reported that human-to-human transmission would play the most crucial role in disease spread (4). It almost took 1.5 month that the outbreak was controlled in China, with a primary increasing trend, steep slope, and then the downtrend. This demonstrates not only the normal trend of an infectious outbreak, but also the role of human interventions to control it. Considering the crowded population of China, health-care preventive and therapeutic interventions were important in restricting the extent of outbreak, as if the natural history of outbreak would have been passed, much more affected patients and deaths were the result.
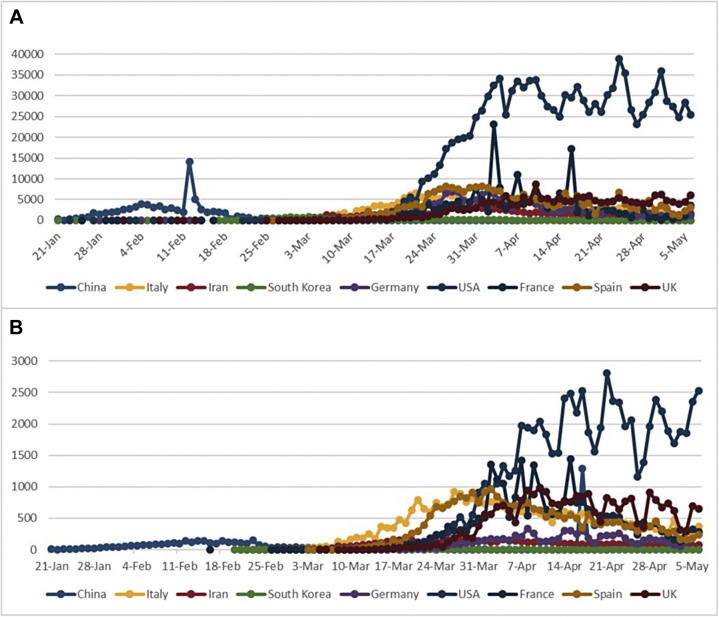
Affecting over 100 patients China, the first reports in other regions came from Thailand, Japan, and South Korea, as the second line affected countries, in which all were infected through transmission from confirmed cases of COVID-19 from China (1). While struggling in the life-and-death battle of COVID-19 outbreak in China, the other countries, were almost in peace, until the second half of February. Interestingly, the beginning of uptrend in other countries was almost simultaneous with beginning of the downtrend in China. This can further be explained by the role of incubation period in estimating the true prevalence of this disease; as although many of the patients were affected in other countries, they were asymptomatic carriers in the incubation period, who could silently infect many others. Therefore, the steep slope of the curves was created when the fist incubation periods were finished.
Moreover, some diagnostic biases could have led underdiagnoses of patients before. In other words, as the symptoms of COVID-19 were similar to other pneumonias, some of mild cases could have been clinically diagnosed with community acquired pneumonia without being tested for COVID-19 until late stages. On the other hands, severe cases, such as those with comorbidities, could cause bias in overestimating viral shedding time and severity of disease symptoms (5).
Eventually, after infecting over 118,000 patients in over 100 countries, and causing more than 4200 deaths, the outbreak was called a “pandemic” by WHO on March 11th 2020 (6).
As one of the neighboring countries of China, South Korea was one of the first countries to be affected by COVID-19. Considering the epidemic curve of South Korea, the outbreak was controlled in less than a month, which may demonstrate timely, efficient actions in prevention and control of this pandemic.
Germany and USA could be representative of facing an outbreak in a developed country. Although the steep slope of both countries started later than some other high-prevalent ones, the reported new cases became quite high considering their population. This could be interpreted as the role of an efficient screening protocol for detecting the patients in mild stages. Also, despite the high frequency, the death rates were not as much high in them. This also demonstrates the efficiency of patient-management in controlling the pandemic.
The first cases of COVID-19 in Italy were reported one month after China, which could be explained based on the incubation period and transmission rate of disease. Despite the disease-controlling actions such as isolation of infected cities, restricting transportations, and therapeutic approaches, they were not efficient enough to restrict the outbreak, and it developed to involve over a hundred thousand people and cause thousands of deaths.
Although the first case of COVID-19 in Spain was reported in early February, there was a 2 week interval until beginning of the steep slope. Therefore, it could be learnt that in the time of an important pandemic, incidence of even one case shall be taken seriously.
France was one of the top 10 countries reporting new cases of COVID-19. The pattern of its epidemic curve is similar to Germany in the matter of new cases. However, it is remarkably different in the matter of deaths, which may demonstrate the difference of these two countries in patient management.
Although no infected cases of COVID-19 were reported from Iran until late February (7), the outbreak quickly raised with a short interval between first report and steep slope. This might be suggestive for misdiagnosis, and unavailability of adequate diagnostic facilities. Besides, inadequate preventive equipment, and transportation restriction could potentially be considered as a cause of increased incidence and death in Iran (Figure 1 ) (8).
Figure 1.
Comparative graphs of daily patients (A) and deaths (B) in some high-prevalent counties. (Update: May 6th, 2020)
The world has encountered several pandemics in the past 2 centuries. Therefore, no matter to which cause, the outbreaks might be inevitable to occur sometimes; but, more important to be considered, is how we approach them to be defined and controlled. First, it should be taken to account that even though some countries, especially the developing ones, might not be marked on the leading board of affected countries, the probability of high prevalence shall not be ignored in them. This is important as low reports in such countries could be a result of inadequate diagnostic tests rather than low prevalence. Second, the approach to control a pandemic would make more sense in case of international collaborations in the matters of disease prevention and treatment. While preventive approaches such as restricting transportation or preventive equipment may be the first lines, research investigations for developing specific medication and vaccines come as the second line of encountering an outbreak.
Acknowledgment
The authors would like to kindly thank all those who have made efforts to control the COVID-19 pandemic. The authors declare to have any conflict of interest. This manuscript was provided with no financial support of any organization.
(ARCMED_2020_579)
Conflict of Interest
The authors declare to have any conflict of interest.
References
- 1.World Health Organization, Novel Coronavirus (2019-nCoV) Situation report-1, 21 January 2020. Geneva, Switzerland. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200121-sitrep-1-2019-ncov.pdf?sfvrsn=20a99c10_4. Accessed March 23, 2020.
- 2.Lu R., Zhao X., Li J. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395:565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Backer J.A., Klinkenberg D., Wallinga J. Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China, 20–28 January 2020. Eurosurveillance. 2020;25 doi: 10.2807/1560-7917.ES.2020.25.5.2000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization, Novel Coronavirus (2019-nCoV) Situation report-3, 23 January 2020. Geneva, Switzerland. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200123-sitrep-3-2019-ncov.pdf?sfvrsn=d6d23643_8. Accessed March 23, 2020.
- 5.de Sousa R., Reusken C., Koopmans M. MERS coronavirus: data gaps for laboratory preparedness. J Clin Virol. 2014;59:4–11. doi: 10.1016/j.jcv.2013.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization, Novel Coronavirus (2019-nCoV) Situation report-51, 11 March 2020. Geneva, Switzerland. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10. Accessed March 23, 2020.
- 7.World Health Organization, Novel Coronavirus (2019-nCoV) Situation report-32, 21 February 2020. Geneva, Switzerland. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200221-sitrep-32-covid-19.pdf?sfvrsn=4802d089_2. Accessed March 23, 2020.
- 8.Worldometer - real time world statistics. COVID-19 Corovavirus Pandemic. 2020. https://www.worldometers.info/coronavirus/