Abstract
The novel coronavirus disease (COVID-19) pandemic has had a tremendous impact on various health sectors including residency training programs. The suspension of non-essential health services at many hospitals has led to an increase in the workload for residents in emergency department while there was a sharp decline in the workload of residents in departments like Orthopaedics. In this brief report, we discuss the strategy employed at our institution to effectively redistribute our residents to manage the pandemic, and the measures taken to promote resident training and welfare.
Keywords: Orthopaedic resident, COVID, AIIMS
The novel coronavirus disease (COVID-19) pandemic has led to suspension of non-essential health services in most hospitals leading to an unequal distribution of workload. Many patients who availed health services through routine care are directed to emergency department. As a result, emergency department residents and staff are being overburdened while the workload on other departments like Orthopaedics has seen a sharp decline. Therefore, it becomes important to efficiently utilize the hospital staff to provide patient care, and protect the health workers from COVID-19 and burnout. In this viewpoint, we would like to discuss our strategy in using the Orthopaedic resident workforce at All India Institute of Medical Sciences, New Delhi, during COVID-19.
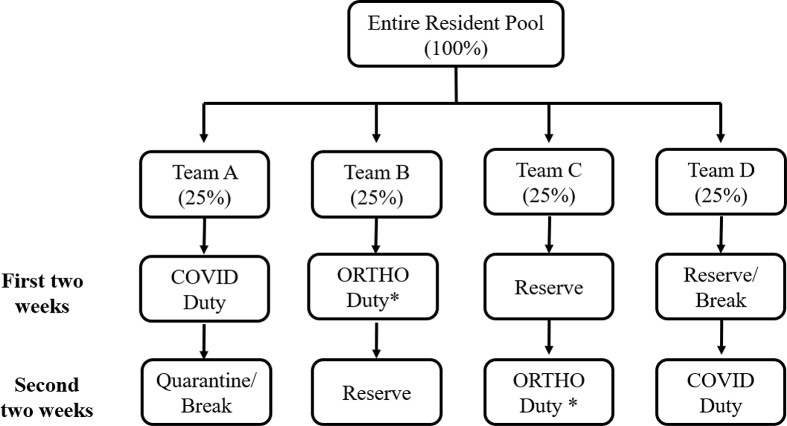
In addition to the cancellation of routine surgeries like joint replacements, sports surgeries and spine surgeries, the decrease in trauma surgeries as a result of reduction in road traffic accidents has led to a significant drop in the volume of surgeries performed by our department. This substantial reduction in the surgeries, and the resulting decline in admitted patients has led to decreased resident requirement. At present, majority of our surgeries are either for oncology patients or for those who experience low energy fractures such as hip fractures. As a result, only one or two operating teams are required per day. Therefore, our residents have been divided into multiple small teams who are assigned duties on a rotational basis (Fig. 1). Each team comprises of senior and junior level residents so that 1–2 operating rooms can be run efficiently every day without overcrowding in the operating rooms. The same team is also sufficient enough to manage patients in ward and emergency department. Apart from this working team, residents in other teams are advised to stay home though they are available 24 × 7.
Fig. 1.
-
•Teams A & D rotate with teams B & C every 4 weeks
-
•25% of the resident strength will be ‘Reserve’ at any point of time so that any escalation of need for COVID duty is met
∗The team of residents in ORTHO duty will manage operative, in-patient and out-patient services.
As part of the hospital policy, currently 25% of our residents are dedicated to serving the COVID-19 patients at any point of time. Since our department does not manage sick patients, our residents are posted with the screening team at our COVID-19 clinics. Other departments which provide critical care such as Anaesthesia, Internal Medicine, Pulmonary Medicine and Emergency Medicine are involved in managing the COVID-19 ward and intensive care units, with assistance from our residents if required. Orthopedic Residents in the COVID-19 team are usually posted for a period of about two weeks after which they are quarantined for 14 days.1 This policy not only restricts resident exposure to COVID-19, but also limits the transmission from residents if they become infected.
AIIMS like many other hospitals has shut down outpatient services. Although this has limited our ability to serve new patients it has not compromised our follow-up care. Patients who have been recently operated and need to have their suture/staple removed or wound inspected are still being seen in our examination rooms in the ward or operating complex as our out-patient blocks are closed. Residents posted in the ward or operating room see the respective patients and discuss with the consultants as required. Moreover, every day residents make telephone calls to patients who already had an appointment with us in the out-patient department. Majority of their concerns could be addressed through telephone, and wherever not addressed, patients were advised to report physically.When feasible and required, patients were also given the opportunity to discuss about their orthopaedic problems using video interaction and images.
Many hospitals across the world are already redistributing their residents to manage the pandemic. Sarpong et al.2 reported the experience of orthopaedic residents and attending physicians posted in the emergency room of their hospital in New York, which had become the epicentre of COVID-19. Rahman et al.3 described how their residents were involved in a prone-positioning protocol to minimize the physical burden on their medical colleagues. Methods have been detailed to regroup the (General surgery) residents into teams to minimize patient contact and prevent transmission between the teams.4 However, the regrouping strategies described by the aforementioned authors do not mention about decreasing the overall resident workforce, and do not involve specific teams for COVID-19 duty. We believe that having a separate team which is involved only in COVID-19 duty prevents transmission between residents, and also protects transmission to orthopaedic patients. Although a national level lockdown at a relatively early stage might have slowed the transmission in India, considering its density of population, an explosive rise in cases post lockdown cannot be ruled out and warrants escalation of preparations. Therefore, we have redistributed residents in a manner that 50% of the residents can be allocated for COVID-19 duty at any time without compromising the orthopaedic care, and safety of patients.
Residents form the major workforce in most teaching hospitals, and take care of both COVID-19 positive and normal patients. However, residency is also a training period, and hospitals have an obligation to continue their educational activities. As part of social distancing measures, lectures, journal clubs, thesis presentations, etc. were suspended. However, we continue to have all our department educational activities through online portals as they were scheduled. Multiple online portals are available which enable live lectures and promote interactions between the participants. These are easy to use and can be implemented anywhere without much technical expertise.
At present, we do not have a universal screening of our patients, and it is possible that some of the orthopaedic patients might be asymptomatic carriers. Moreover, COVID-19 has been reported among a few healthcare workers at AIIMS. Therefore, residents are at risk of contracting COVID-19 even while performing their normal duties. To protect our residents, we have provided N-95 masks to all our residents for use at hospitals even when not seeing a confirmed COVID-19 patient. Additionally, all residents have been provided hydroxychloroquine tablets as the ICMR guidelines have advocated its use for prophylaxis among healthcare workers.5
In summary, we are trying our best to progress in patient care, teaching, and research even during these challenging times (Table 1). Although we hope the current situation to end soon, it is important for orthopaedic departments to find new ways to continue their routine activities instead of waiting for the pandemic to be over. We hope that our experience will provide valuable guidance to other orthopaedic departmentsin managing their residents, and in continuing patient care and learning.
Table 1.
Summary of changes in residency.
| Resident duties |
|---|
| Divided into multiple teams |
| Each team comprise of senior and junior level residents |
| One team is assigned for COVID care |
| 25% residents are kept as reserve |
| Others manage operative, inpatient and outpatient services on rotational basis |
| Resident Education |
| Online lectures, Seminars and Journal Clubs with live streaming and interaction |
| Resident Welfare |
| Universal Hydroxychloroquine prophylaxis |
| Universal N-95 masks |
| Complete personal protective equipment (PPE) for those in COVID team |
Contributor Information
Rajesh Malhotra, Email: rmalhotra62@gmail.com.
Deepak Gautam, Email: cmcdeepak@yahoo.com.
Jaiben George, Email: jaibengeorge@gmail.com.
References
- 1.WHO Considerations for quarantine of individuals in the context of containment for coronavirus disease (COVID-19) 2020. https://www.who.int/publications-detail/considerations-for-quarantine-of-individuals-in-the-context-of-containment-for-coronavirus-disease-(covid-19) [cited 2020 Apr 29];Available from:
- 2.Sarpong N.O., Forrester L.A., Levine W.N. What’s important: redeployment of the orthopaedic surgeon during the COVID-19 pandemic. J Bone Jt Surg. 2020 doi: 10.2106/JBJS.20.00574. Ahead of P:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rahman O.F., Murray D.P., Zbeda R.M. Repurposing orthopaedic residents amid COVID-19. J Bone Jt Surg. 2020 doi: 10.2106/JBJS.OA.20.00058. Ahead of p, In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nassar A.H., Zern N.K., Mcintyre L.K. Emergency restructuring of a general surgery residency program during the coronavirus disease 2019 pandemic: the university of Washington experience. JAMA Surg. 2020 doi: 10.1001/jamasurg.2020.1219. https://jamanetwork.com/ [DOI] [PubMed] [Google Scholar]
- 5.MOHFW Advisory on the use of Hydroxychloroquine prophylaxis for SARSCov2 infection. 2020. https://www.mohfw.gov.in/pdf/AdvisoryontheuseofHydroxychloroquinasprophylaxisforSARSCoV2infection.pdf [cited 2020 Apr 29];Available from: