Abstract
Background
An ongoing outbreak of coronavirus disease 2019 (COVID-19) has spread around the world. It is debatable whether asymptomatic COVID-19 virus carriers are contagious. We report here a case of the asymptomatic patient and present clinical characteristics of 455 contacts, which aims to study the infectivity of asymptomatic carriers.
Material and methods
455 contacts who were exposed to the asymptomatic COVID-19 virus carrier became the subjects of our research. They were divided into three groups: 35 patients, 196 family members and 224 hospital staffs. We extracted their epidemiological information, clinical records, auxiliary examination results and therapeutic schedules.
Results
The median contact time for patients was four days and that for family members was five days. Cardiovascular disease accounted for 25% among original diseases of patients. Apart from hospital staffs, both patients and family members were isolated medically. During the quarantine, seven patients plus one family member appeared new respiratory symptoms, where fever was the most common one. The blood counts in most contacts were within a normal range. All CT images showed no sign of COVID-19 infection. No severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections was detected in 455 contacts by nucleic acid test.
Conclusion
In summary, all the 455 contacts were excluded from SARS-CoV-2 infection and we conclude that the infectivity of some asymptomatic SARS-CoV-2 carriers might be weak.
Keywords: SARS-CoV-2, Asymptomatic carrier, Contacts, Infectivity
Abbreviations: COVID-19, Coronavirus disease 2019; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; CHD, congenital heart disease; EDOU, emergency department observation unit; ED, emergency department; CT, computed tomography; RT-PCR, Reverse Transcription-Polymerase Chain Reaction; GCDC, Guangzhou Center for Disease Control and Prevention; CDC, Chinese Center for Disease Control and Prevention; IQR, interquartile ranges; PPE, personal protective equipment
1. Introdution
The emergence of the coronavirus disease 2019 (COVID-19) since early December 2019, has spread to many countries recently and sparked world pandemic via mass gathering [[1], [2], [3]]. As of March 24, 2020, there have been 334981 confirmed cases and 14652 deaths globally [4].
It has been proved that the pathogen of COVID-19 is severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which has high homology with SARS-CoV [5]. Similar to SARS-CoV, the dominant SARS-CoV-2 transmission mode is human-to-human transmission [6]. Differently, the reproductive number (R0) (the expected number of secondary cases produced by a single infected person in a susceptible population) is estimated between two and three, which is higher than SARS [6,7]. Furthermore, the transmission of SARS occurs during the symptomatic period [8]. For COVID-19, numerous asymptomatic infections were found among close contacts of confirmed patients, like the report on “Diamond Princess” [9]. However, the epidemiological significance of asymptomatic infections is unclear until now. Recent studies indicated that transmission of COVID-19 could also occur from these individuals with no symptoms [10,11]. However, for now, whether asymptomatic SARS-CoV-2 carriers are contagious still remain controversial.
Here, we report a case of an asymptomatic SARS-CoV-2 carrier with nosocomial infection, as shown below, and describe the clinical characteristics of 455 contacts. Our purpose is to analyze the infectivity of asymptomatic carriers.
Case A was a 22-year-old female patient who had a medical history of congenital heart disease (CHD) presented to the emergency room of Guangdong Provincial People's Hospital (Guangzhou, Guangdong province, China) on January 13, 2020. She complained of shortness of breath for 16 years, and the symptom worsened for one month. The accompanied symptom was chest distress, without cough, sputum production and fever. Apart from CHD, she had no other diseases and had no smoking habit. Her temperature was normal, and laboratory measurements showed no apparent abnormalities (Table 1 ). Echocardiography displayed atrial septal defect and severe pulmonary hypertension. The diagnosis was congenital heart disease, atrial septal defect and pulmonary hypertension.
Table 1.
Laboratory measurements of Case A.
| Jan, 13 | Feb, 12 | Feb, 19 | Feb, 27 | Normal range | |
|---|---|---|---|---|---|
| Blood count, × 10⁹/L | |||||
| White blood cell count | 7.70 | 7.78 | 7.41 | 7.92 | 3.50–9.50 |
| Neutrophil count | 4.97 | 4.14 | 4.16 | 4.44 | 1.80–6.30 |
| Lymphocyte count | 2.13 | 2.91 | 2.13 | 2.63 | 1.10–3.20 |
| Serological variables | |||||
| C-reactive protein, mg/L | 0.6 | 5.89 | NT | NT | <5.0 |
| Procalcitonin, ng/ml | Normal | Normal | NT | NT | <0.05 |
NT = not tested.
Case A was mainly given to oxygen therapy, diuretic treatment, plus pharmacotherapy of pulmonary hypertension. On January 16, as Case A's condition improved and vital signs became stable, she was transferred to emergency department observation unit (EDOU). Owing to the Spring Festival and COVID-19 outbreak, she had been hospitalized in EDOU along with her brother until February 11. Before admission, she underwent a serious of examinations according to hospital-formulated guidance during epidemic period. Nevertheless, the patient's nasopharyngeal swab tested positive for SARS-CoV-2 by real-time Reverse Transcription-Polymerase Chain Reaction (RT-PCR). She was immediately admitted to quarantine ward in infectious department.
Case A and her brother both denied visiting Wuhan (the epidemic area in China) and any contact with COVID-19 patients. They wore masks all the time except at meals and drinking. How she became infected was unknown.
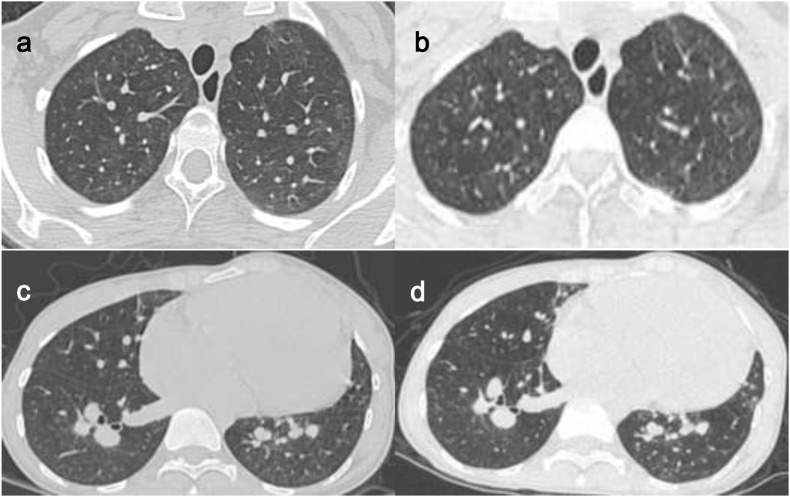
Notably, in isolation, the patient had never fever, sore throat, myalgia or other symptoms associated with virus infection [12]. Shortness of breath and chest distress, without further aggravation than before, were thought to be caused by CHD. Laboratory measurements reflected that white blood cells, lymphocytes, C-reactive protein and procalcitonin were within a normal range (Table 1). Upon admission, chest computed tomography (CT) scan showed non- COVID-19 imaging feature (Fig. 1 . a, c). In the time of hospitalization, the patient received antiviral and interferon therapy. 11 days after the treatment (February 22), chest CT scan indicated no significant differences in comparison with before (Fig. 1. b, d).
Fig. 1.
Chest CT images of Case A. Figure a and c were taken on February 11, which showed non- COVID-19 imaging feature. Case A underwent a CT scan again on February 22. Figure b and d, the follow-up images, showed no significant differences than before.
Meanwhile, nucleic acid tests by real-time RT-PCR assay were performed repeatedly. Nucleic acid tests were positive for five consecutive days from February 11 to 15. The results of the test on quarantine day 16 (February 26) turned negative, subsequently, on quarantine day 18 and 20, which were also negative. She was then released from quarantine on day 21 (March 2, 2020). Due to only laboratory-confirmed positive, case A was diagnosed as an asymptomatic carrier, manifested by Guangzhou Center for Disease Control and Prevention (GCDC).
2. Materials and methods
2.1. Study design and subjects
In our study, asymptomatic COVID-19 carrier was defined as a patient without related clinical symptoms, but whose SARS-CoV-2 test was positive. Since Case A was diagnosed, all contacts, including hospital staffs, family members and patients, were routinely screened. Amounting to 455 contacts – 224 hospital staffs, 196 family members and 35 patients – who had been exposed to case A in EDOU or circulated area of it became the subjects of study. Contacts were defined as individuals in the same ward with Case A. EDOU plus the circulated area of it covers 60 square meters where there are 14 patients' beds placed at least 1.2 m apart. The study was approved by the Medical Ethical Committee of Guangdong Provincial People's Hospital.
2.2. Data collection
Isolated individuals’ detailed information during the emergency department (ED) and hospitalization were retrospectively collected from electronic medical records, while other data were reviewed from documents recorded by related departments. Emphatically, we gathered their contact history, consisting of the date when they went to the emergency, the reason why they came to the emergency, and the time how long they were exposed to the case A. Demographics characteristics were also collected.
Any new symptoms on each person were taken down, both in ED and quarantine, including fever, cough, sputum production, sore throat, etc.
Meanwhile, we obtained imaging and laboratory data from hospital staffs and patients, which of family members were not noted. Each of patients had undergone a CT scan prior to admission because of the outbreak. It had been reviewed after the medical isolation began. Hospital staffs were examined one time. For laboratory test, a complete blood count was focus of attention. Nasopharyngeal swab specimens had been collected at least one time in whole people. All samples were processed at clinical laboratory of hospital and sent to GCDC simultaneously.
Patients and family members were quarantined for medical observation and hospital staffs were not quarantined because of standard protection, in principle.
2.3. Laboratory nucleic acid test
In accordance with the protocol announced previously by the WHO, RT-PCR can be considered in the assessment of individuals who have had contact with a COVID-19 case [13]. Consequently, whether the patients were infected with the SARS-CoV-2 was detected by real-time RT-PCR. Chinese Center for Disease Control and Prevention (CDC) published the sequences of primers and probe targeted to envelope gene of SARS-CoV-2, in January 21, 2020, which were as follows: forward primer 5′-TCAGAATGCCAATCTCCCCAAC-3′; reverse primer 5′-AAAGGTCCACCCGATACATTGA-3′; and probe 5′CY5CTAGTTACACTAGC-CATCCTTACTGC-3′BHQ1.
2.4. Statistical analysis
All research objects employed fundamental descriptive analysis. Continuous variables were expressed as the medians and interquartile ranges (IQR). Categorical variables in each category were summarized as counts and percentages. All statistical analyses were conducted with IBM SPSS statistics 24.0.
3. Results
3.1. Patients
The statistics of 35 patients are displayed in Table 2 . All patients also wore masks except for eating or drinking and were admitted to infectious department for medical isolation. The median contact time was four days (interquartile range, 1.0 to 6.0), whereas the longest among them reached 21 days. The median age of the patients was 62 years (interquartile range, 50.0 to 84.0). A total of 57.1% were males. All individuals had been to ED of our hospital for various diseases. Undoubtedly, acute cardiovascular event and digestive diseases were common, accounting for 25.7% and 22.9%, respectively.
Table 2.
Clinical characteristics of 35 patients.
| Clinical characteristics | Patients (n = 35) |
|---|---|
| Demographics characteristics | |
| Age, median (IQR), years. Male, sex, No. (%) |
62 (50.0–84.0) 20 (57.1) |
| Times of contact with Case A, median (IQR), days Protopathy, No. (%) |
4 (1.0–6.0) |
| Cardiovascular disease | 9 (25.7) |
| Digestive diseases | 8 (22.9) |
| Cerebrovascular disease | 5 (14.3) |
| Orthopedic disease | 4 (11.4) |
| Hematological disease Renal disease Cancer |
2 (5.7) 2 (5.7) 3 (8.6) |
| Others1 | 2 (5.7) |
| Respiratory symptoms | |
| None, No. (%) Any, No. (%) Fever Newly emerged fever |
16 (45.7) 19 (54.3) 11 (31.4) 7 (20.0) |
| Cough | 8 (22.9) |
| Sputum | 4 (11.4) |
| Dyspnea | 7 (20.0) |
| Newly emerged dyspnea | 1 (2.9) |
| Laboratory findings | |
| Leukocyte count ( × 109/L, normal range 4.0–10.0), No. (%) | |
| Increased Decreased Normal |
14 (40.0) 3 (8.6) 18 (51.4) |
| Lymphocyte count ( × 109/L, normal range 1.5–3.5), No. (%) | |
| Increased Decreased Normal |
1 (2.9) 12 (34.3) 22 (62.9) |
| Nucleic acid test negative, No. (%) | 35 (100.0) |
| Radiologic findings | |
| Normal on chest CT, No. (%) | 11 (31.4) |
| Abnormalities on chest CT, No. (%) | 24 (68.6) |
| Inflammatory change | 12 (34.3) |
| Pleural effusion | 16 (45.7) |
| Interstitial change Pulmonary edema |
2 (5.7) 1 (2.9) |
| Pulmonary nodule | 1 (2.9) |
| Clinical outcome | |
| Transfer to specialized department, No. (%) | 25 (71.4) |
| Discharge from hospital, No. (%) | 8 (22.9) |
| Death, No. (%) | 2 (5.7) |
Others include urologic diseases and rheumatic disease.
In terms of clinical symptoms, 16 (45.7%) patients were free of respiratory symptoms, which more than half of them (19 [54.3%]) appeared inversely. The respiratory symptoms involved fever (11 [31.4%]), cough (8 [22.9%]), dyspnea (7 [20.0%]) and sputum (4 [11.4%]). Among patients with fever, hyperthermia (body temperature >39 °C) occurred in one patient with chills after chemotherapy. Three individuals presented slight fever (body temperature between 37.3 °C and 38.0 °C), of whom temperature could return to normal without therapy. Two individuals were diagnosed with infective endocarditis and acute pancreatitis severally with the cause of their symptoms including fever plus dyspnea and stomachache. Another five patients developed fever was consider as complication of the original disease, mostly pulmonary infection, whether the symptom was new or persistent. Last but not least, all dyspnea was associated with heart failure.
The blood counts in most patients were within normal range. Lymphocytopenia (<1.5 × 109 cells/L) had appeared in 34.3% of the patients and leukopenia (<4.0 × 109 cells/L) in 8.6%. One patient was also accompanied with neutropenia (<1.8 × 109 cells/L) on account of myelosuppression after chemotherapy. On the contrary, lymphocytosis (>3.5 × 109 cells/L) was observed in a patient with acute lymphoblastic leukemia. Besides one patient, died on quarantine 4-day, 34 patients underwent multiple nucleic acid tests of SARS-CoV-2. All the results were negative, including first time of the dead. Of 35 patients that had more than once chest CT scan, CT abnormalities were reported in 68.6%. The most common manifestations were inflammatory change (34.3%) and pleural effusion (45.7%). The interstitial change was detected less. Pulmonary edema and nodule were seen in persons with heart failure and lung cancer, respectively. Of particular concern, all CT findings were non-viral infection discussed professionally by radiologists. Normal CT image was found in 11 of 35 patients (31.4%).
According to evaluation from physicians, there were 19 infected patients (54.3%). Of these 19 patients, 15 (42.9%) had pneumonia, which was bacterial (37.1%), followed by pendulous (2.9%) and aspiration (2.9%). Mediastina inflammatory and abdominal infection arose from two patients with fistula. Other two patients had suffered from infection due to protopathy on admission. Above infected patients were administered for empirical antibiotic treatment. Four (11.4%) patients needed emergency surgery for their condition. The rest of them (34.3%) were received to heteropathy.
It totally took 14 days from the last contact with Case A to the end of medical observation. As of Feb 26, 2020, none of 35 patients was diagnosed with SARS-CoV-2 infection. Among whom eight (22.9%) were discharged from the hospital while 25 (71.4%) were transferred to the specialized department for further treatments. The remaining two individuals both died for severe heart failure judged by the clinical expert panel during the period of quarantine.
3.2. Family members
In total, 196 family members were enrolled. The situation on wearing masks was the same as that in patients. Local CDC took charge of following up 172 among them, who were ruled out SARS-CoV-2 infection after 14-days medical isolation, as far as we know. The rest of the escorts were placed in designated locations by GCDC for quarantine. Of these 24 escorts, 11 were male and 13 were female. They aged from 24 to 86 years old and the median age was 47.5 years old (interquartile range, 34.0 to 57.0). The median contact time was five days (interquartile range, 1.0 to 11.0). Regarding examinations, at least two nucleic acid tests were negative. All the attendants except a family member had no respiratory symptoms in the time of quarantine. Details as below.
A 37-year-old woman, who had stayed in EDOU (February 7) for 10 h as relative, developed slight fever (the highest temperature was 37.5 °C), dry cough and sore throat after six days (February 13). Then she was presented to our hospital immediately. According to the investigation, she had worn a mask during the hospital visit and had a history of recurrent acute tonsillitis. After admission, her CT images and laboratory measurements were normal. Additionally, she experienced four SARS-CoV-2 nucleic acid tests successively, all of which were negative. The case was given empirical antibiotic treatment since admission, and her symptoms disappeared afterwards. Based on clinical symptoms as well as auxiliary examination results, she received a diagnosis of acute tonsillitis finally. On Fberuray 25, she recovered and was discharged from the hospital.
3.3. Hospital staffs
To ensure safety, 224 hospital staffs who had come into contact with Case A were screened. As is clearly shown in Table 3 , their identities were mainly composed of doctors (59 [26.3%]) and nurses (101 [45.1%]). Others coexisted in the same room with Case A for work, such as security guards, cleaners, transportation personnel, etc. Of these 224 staffs, 103 were male and 121 were female, with ages ranging 21–60 years old. The median age was 35 years old (interquartile range, 28.0 to 42.0). Most of them were emergency workers so that they had long exposure to confirmed case. Oppositely, some doctors in other departments had a brief stay, approximately one to 2 h, because of emergency consultation. It is noteworthy that all personnel working in ED must take medical protection – namely, using N95 mask, putting on isolation gown and wearing goggle.
Table 3.
Clinical characteristics of 224 hospital staffs.
| Clinical characteristics | Hospital staffs (n = 224) |
|---|---|
| Demographics characteristics | |
| Identity, No. (%) | |
| Doctor | 59 (26.3) |
| Nurse | 101 (45.1) |
| Others1 | 64 (28.6) |
| Age, median (IQR), yr. Male, sex, No. (%) |
35 (28.0–42.0) 103 (46.0) |
| Respiratory symptoms | |
| None, No. (%) | 224 (100.0) |
| Laboratory findings | |
| Leukocyte count ( × 109/L, normal range 4.0–10.0), No. (%) | |
| Increased Decreased Normal |
29 (12.9) 0 (0.0) 195 (87.1) |
| Lymphocyte count ( × 109/L, normal range 1.5–3.5), No. (%) | |
| Increased Decreased Normal |
5 (2.2) 3 (1.3) 216 (96.5) |
| Nucleic acid test negative, No. (%) | 224 (100.0) |
| Radiologic findings | |
| Normal on chest CT, No./total No. (%) | 171/223 (76.7) |
| Abnormalities on chest CT, No./total No. (%) | 52/223 (23.3) |
| Pulmonary nodule | 29/223 (13.0) |
| Pulmonary fibrosis focus | 18/223 (8.1) |
| Pulmonary emphysema | 5/223 (2.2) |
| Quarantine personnel, No. (%) | 0 (0.0) |
Others include security guards, cleaners, transportation personnel, support crew.
No respiratory symptoms were observed, either existing or emerging. Blood test results revealed normal leukocyte count in 87.1% and lymphocyte count in 96.5%. Lymphocyte counts were decreased in three staffs (1.3%) without leukopenia (<4.0 × 109 cells/L). A pregnant nurse failed to accept a CT scan. A minority of hospital staffs (52 [23.3%]) found abnormalities in CT, where pulmonary nodule, fibrosis focus and emphysema were seen. All hospital staffs were tested twice for SARS-CoV-2 nucleic acid, and the results were negative, which was identical with the two groups mentioned above. In contrast to them, none of 224 hospital staffs required medical observation.
4. Dissusion
In this study, we recorded in detail the hospitalized situation, diagnostic procedure, inspection results, treatment plans and clinical outcome of an asymptomatic SARS-CoV-2 carrier who was laboratory confirmation by RT-PCR assay, but without related symptoms and imaging changes in concert with previous reports [12,14]. Also, we analyzed epidemiological and clinical data from 455 contacts who had been exposed to the asymptomatic patient. All the 455 contacts were excluded from SARS-CoV-2 infection. Of the 231 quarantined people (196 family members and 35 patients), 229 were removed from medical observation successfully and two died for severe heart failure. New or existing respiratory symptoms were almost appeared in patients, which were considered to be associated with their original disease or complications. A family member complaining of fever was diagnosed as acute tonsillitis ultimately. Unlike COVID-19, normal blood count was found in most contacts [12,15]. All CT images showed no sign of COVID-19 infection. Unquestionably, all cases tested negative for SARS-CoV-2 nucleic acid. This fact illustrated that there had been no cases of infection in a relatively dense space.
Since the outbreak, our hospital has taken a series of effective prevention and control measures, which made a considerable effect on preventing the spread in this case. Above all, medical staffs abide by the principle of graded protection strictly. For patients and attendants, each patient can only be accompanied by one attendant, and both need to wear personal protective equipment (PPE). Nevertheless, there is still a risk of transmission of COVID-19 under stringent measures. Primarily, shortages of PPE were common in the early stages. Medical resources were supplied to healthcare workers priorly. Due to these factors, patients and attendants can only wear one mask for a long time, resulting in its ineffective. Besides, we noticed that some patients and relatives wore PPE incorrectly due to the lack of adequate training, which was also possible for hospital staffs. Last but not least, it is unavoidable to take off mask while eating or drinking, which provides an opportunity to spread the virus.
Considering all the mentioned factors, we suggest that there are more important reasons for achieving “Zero infection”. As is well-known, person-to-person transmission through respiratory droplets is the main route of COVID-19 transmission [6]. Earlier research revealed that the viral load of respiratory tract samples in an asymptomatic patient was similar to that in the symptomatic patients [11]. However, a single sample is difficult to be representative. In the light of “Zero infection” for this case, we venture to guess that the viral load of respiratory tract samples in the asymptomatic patient might not be high. Moreover, although pathogenic nucleic acids can be detected in respiratory tract samples from asymptomatic carriers, the opportunity of transmission is less than that in symptomatic patient owing to the absence of the way expelling pathogen via cough and sneezing.
Based on the foregoing discussion, we conclude that the infectivity of some asymptomatic SARS-CoV-2 carriers might be weak. This finding implicates that there is not needful to worry unduly for asymptomatic or mild patients during the ongoing COVID-19 pandemic. Furthermore, excessive virus nucleic acid detection is unnecessary, which can relieve the pressure on public health resources. Under the development of epidemic circumstance, more and more public concerns on the increasing number of asymptomatic or mild patients hid in the community. However, combined with our results and the defense measures currently completed, we hope such worries are misplaced and we also believe the world will win this battle certainly.
The limitation of our study is that there is only one case and lack of detailed information on family members quarantined locally. Large-scale multicenter studies are needed to verify our conclusion. However, both asymptomatic carrier and 455 contacts were admitted to and treated in designated places. Hence, the study results are representative to some extent.
5. Conlusions
Infectivity of some asymptomatic SARS-CoV-2 carriers might be weak. Effective prevention and control measures are helpful to prevent COVID-19 spread of asymptomatic carriers. The result of this study may alleviate parts of the public concern about asymptomatic infected people.
Funding
This work was supported by the Science and Technology Planning Project of Guangdong Province (No. 2020B111111005).
CRediT authorship contribution statement
Ming Gao: Methodology, Data curation, Writing - original draft, Writing - review & editing. Lihui Yang: Investigation, Data curation, Formal analysis, Writing - review & editing. Xuefu Chen: Resources. Yiyu Deng: Writing - review & editing. Shifang Yang: Writing - review & editing. Hanyi Xu: Resources. Zixing Chen: Resources. Xinglin Gao: Conceptualization, Project administration, Supervision, Validation.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We owe thanks to the staffs of Guangdong Provincial People's Hospital for gathering data in our study. We also acknowledge all the objects in this study and their family members.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.rmed.2020.106026.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Lescure F.X., Bouadma L., Nguyen D., et al. Clinical and virological data of the first cases of COVID-19 in Europe: a case series. Lancet Infect. Dis. 2020;20 doi: 10.1016/S1473-3099(20)30200-0. Published Online March 27 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adalja A.A., Toner E., Inglesby T.V. JAMA; 2020. Priorities for the US Health Community Responding to COVID-19. Published Online March 03 2020. Available at: [DOI] [PubMed] [Google Scholar]
- 3.McCloskey B., Zumla A., Ippolito G., et al. Mass gathering events and reducing further global spread of COVID-19: a political and public health dilemma. Lancet. 2020;395:1096–1099. doi: 10.1016/S0140-6736(20)30681-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization . 2020. Coronavirus Disease (COVID-19) Outbreak.https://www.who.int/emergencies/diseases/novel-coronavirus-2019 Available at: [Google Scholar]
- 5.Lu R., Zhao X., Li J., et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395:565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang Y., Wang Y., Yan Chen, et al. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J. Med. Virol. 2020;92(6):568–576. doi: 10.1002/jmv.25748. Published Online March 05 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Del Rio C., Malani P.N. JAMA; 2020. COVID-19-New Insights on a Rapidly Changing Epidemic. Published Online February 28 2020. Available at: [DOI] [PubMed] [Google Scholar]
- 8.Zeng G., Xie S.Y., Li Q., et al. Infectivity of severe acute respiratory syndrome during its incubation period. Biomed. Environ. Sci. 2009;22(6):502–510. doi: 10.1016/S0895-3988(10)60008-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Diamond princess (ship) 2020. https://en.wikipedia.org/wiki/Diamond_Princess_ Available at: (ship)
- 10.Hu Z., Song C., Xu C., et al. Life Sci; 2020. Clinical Characteristics of 24 Asymptomatic Infections with COVID-19 Screened Among Close Contacts in Nanjing, China. Sci China. Published Online March 04 2020. Available at: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zou L., Ruan F., Huang M., et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N. Engl. J. Med. 2020;382:1177–1179. doi: 10.1056/NEJMc2001737. Available at: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guan W.J., Zhong N.S. Clinical characteristics of covid-19 in China. N. Engl. J. Med. 2020:382. doi: 10.1056/NEJMoa2002032. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization Corona-virus disease (COVID-19) technical guidance: laboratory testing for 2019-nCoV in humans. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/laboratory-guidance Available at:
- 14.Salehi S., Abedi A., Balakrishnan S., et al. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. AJR Am. J. Roentgenol. 2020:1–7. doi: 10.2214/AJR.20.23034. [DOI] [PubMed] [Google Scholar]
- 15.Huang C., Wang Y., Li X., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)301847. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.