Highlights
-
•
The average SARS-CoV-2 seroprevalence in healthcare workers of a a tertiary hospital, University Hospital Essen, Germany was 1.6 % in the period between March to April 2020.
-
•
The local hygiene standards seem to be effective to prevent patient-to-staff virus transmission at the designated COVID-19 units wards.
-
•
Awareness for COVID-19 infections is crucial even in non−COVID-19 wards.
Abbreviation: SARS-CoV-2, severe acute respiratory syndrome-related coronavirus 2; COVID-19, coronavirus disease 2019; PCR, polymerase chain reaction; FFP, filtering face piece; ELISA, Enzyme-linked Immunosorbent Assay; IgG, Immunoglobulin G; S, spike protein subunit 1; vs., versus; n, number; SD, standard deviation; S/co, signal-to-cut-off ratio
Keywords: SARS-CoV-2, Healthcare workers, COVID-19, Seroprevalence, Antibody detection
Abstract
Background
The novel coronavirus SARS-CoV-2 is associated with a severe respiratory manifestation, COVID-19, and presents a challenge for healthcare systems worldwide. Healthcare workers are a vulnerable cohort for SARS-CoV-2 infection due to frequent and close contact to patients with COVID-19.
Study design
Serum samples from 316 healthcare workers of the University Hospital Essen, Germany were tested for SARS-CoV-2-IgG antibodies. A questionnaire was used to collect demographic and clinical data. Healthcare workers were grouped depending on the frequency of contact to COVID-19 patients in high-risk-group (n = 244) with daily contact to known or suspected SARS-CoV-2 positive patients, intermediated-risk-group (n = 37) with daily contact to patients without known or suspected SARS-CoV-2 infection at admission and low-risk-group (n = 35) without patient contact.
Results
In 5 of 316 (1.6 %) healthcare workers SARS-CoV-2-IgG antibodies could be detected. The seroprevalence was higher in the intermediate-risk-group vs. high-risk-group (2/37 (5.4 %) vs. 3/244 (1.2 %), p = 0.13). Four of the five subject were tested negative for SARS-CoV-2 via PCR. One (20 %) subject was not tested via PCR since he was asymptomatic.
Conclusion
The overall seroprevalence of SARS-CoV-2 in healthcare workers of a tertiary hospital in Germany is low (1.6 %). The data indicate that the local hygiene standard might be effective.
1. Background
In 2019, a novel coronavirus was identified. It first appeared in Wuhan, China and caused a cluster of pneumonia cases. The virus was named severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). The World Health Organization designated the disease COVID-19 (coronavirus disease 2019) [1]. It caused a pandemic, and lead to a challenge for healthcare systems. The number of confirmed cases worldwide increased to 3.3 million and the German public health institute (Robert Koch institute) reported 161,703 cases and 6575 deaths on May 2, 2020 in Germany. In response to the disease spreading, German hospitals started to create capacities by canceling elective admissions. The University Hospital of Essen was designated as hospital of admission for COVID-19 patients for an area of around 5 million residents.
The main route of transmission is person-to-person spread [2]. A vulnerable cohort for infection due to frequent and close contact to COVID-19 patients are healthcare workers [3,4]. To avoid patient-to-staff transmission adherence to strict hygiene standards is important [5] The infection with the SARS-CoV-2 usually leads to seroconversion 11–14 days after the first symptoms [6]. However, due to asymptomatic and oligosymptomatic infections [7,8] testing only symptomatic individuals can lead to a significant underestimation of the SARS-CoV-2 seroprevalence.
2. Objectives
The study presents the results of the first SARS-CoV-2 seroprevalence study in 316 healthcare workers of the University Hospital Essen, Germany. In addition, this study evaluates the local hygiene standards by the rate of infections on the designated COVID-19 units after admission of the first COVID-19 patient at the beginning of March.
3. Study design
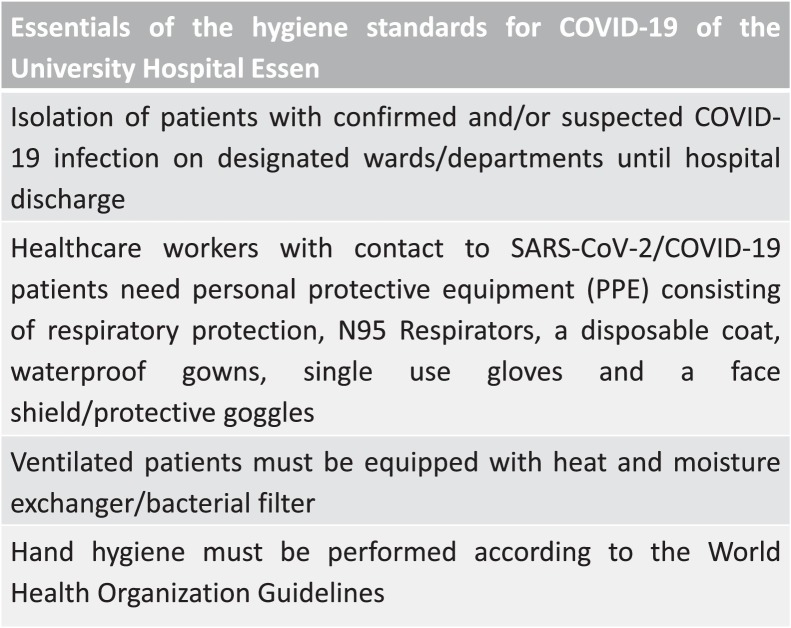
Health care workers of the University Hospital Essen were recruited in this prospective cross-sectional monocentric study. Participants were grouped depending on the frequency of contact to COVID-19 patients: (i) High-risk group with daily contact to COVID-19 patients on the designated wards and on the intensive care units, (ii) intermediated-risk group with daily non−COVID-19 patient contact and as a control (iii) low-risk group without daily patient contact. For staff members of the high-risk group on designated COVID-19 wards a local hygiene standard was prepared (Fig. 1 ). Staff on wards without known or suspected COVID-19 patients (intermediate-risk group) adhere to basic hygiene standards according to the WHO. In addition, all staff members have to wear surgical mask since April 14th. The period of sampling was from March 25th, 2020 until April 21th, 2020. Anti-SARS-CoV-2-IgG antibodies were detected in sera using an semi-quantitative enzyme-linked immunosorbent assay (ELISA) (Euroimmun Medizinische Labordiagnostika, Lübeck, Germany) according to the manufacturer’s instructions.
Fig. 1.
Essentials of the hygiene standard for COVID-19 of the University Hospital Essen.
Fisher’s exact test was used as applicable. Informed consent was obtained from all participants. This study has been approved by the ethics committee of the medical faculty of the University Duisburg- Essen (20−9208-BO).
4. Results
Overall, 317 employees participated in the study. Since one subject was diagnosed for SARS-CoV-2 infection via PCR after a vacation in March 2020 and the comparison between groups was focused on unknown infection of healthcare workers, the subject (intermediate-risk group) was excluded from further analyzes. Subjects characteristics are listed in Table 1 . SARS-CoV-2-IgG antibodies were detected in 5 of 316 (1.6 %) subjects. Out of these, 3 of 244 (1.2 %) subjects belonging to the high-risk group and in 2 of 37 (5.4 %) belonging to the intermediate-risk group. The seroprevalence was higher in the intermediate-risk vs. high-risk group with an odds ratio of 0.22 (confidence interval 95 % 0.04–1.35; p = 0.13). No participant of the control group tested positive for SARS-CoV-2-IgG antibodies. The mean S/CO-value was 2.7 +/- 1.4 and did not differ significantly between groups (Table 1). Four of the five subjects (80 %) with detectable antibodies reported COVID-19 associated symptoms in the past 3 months including headache (40 %) and sneezing (40 %). General malaise, anosmia and fever were observed in just one case each. None of the subjects suffered from cough, sore throat or dyspnea. One of the five subjects (20 %) had no symptoms at all. None of the subjects were hospitalized. The transmission route could not be elucidated in all cases: Three subjects had suspected infection after unprotected professional COVID-19 exposure and in two cases the route of infection is unknown. PCR of a nasopharyngeal swab was performed in 4 out of the 5 cases without SARS-CoV-2 RNA detection.
Table 1.
subject characteristics, SD standard deviation, SARS-CoV-2 severe acute respiratory syndrome coronavirus 2, IgG immunoglobulin G, S/co signal-to-cut-off ratio.
|
high-risk |
intermediate-risk |
low-risk |
overall |
|||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| 244 | 77% | 37 | 12% | 35 | 11% | 316 | 100 % | |
| female | 157 | 64% | 21 | 57% | 26 | 74% | 204 | 65% |
| age (+/- SD) | 36.7 (+/- 10.7) | 42.3 (+/- 13.2) | ||||||
| profession | ||||||||
| nurse | 178 | 73 % | 27 | 73 % | 2 | 6% | 207 | 66% |
| physician | 59 | 24% | 10 | 27% | 9 | 26 % | 78 | 25% |
| lab assistant | 0 | 0% | 0 | 0% | 20 | 57% | 20 | 6% |
| other | 7 | 3% | 0 | 0% | 4 | 11% | 11 | 3% |
| SARS-CoV-2 IgG positive | 3 | 1,2% | 2 | 5,4% | 0 | 0% | 5 | 1,6% |
| SARS-CoV-2 IgG S/co (+/- SD) | 3.0 (+/- 1.8) | 2.2 (+/- 1.1) | 0 | 2.7 (+/- 1.4) | ||||
| symptomatic SARS-CoV-2 infection | ||||||||
| sneeze | 0 | 2 | 0 | 2 | 40 % | |||
| headache | 1 | 1 | 0 | 2 | 40 % | |||
| anosmia | 0 | 1 | 0 | 1 | 20 % | |||
| muscle ache | 1 | 0 | 0 | 1 | 20 % | |||
| general malaise | 1 | 0 | 0 | 1 | 20 % | |||
| diarrhoea | 0 | 1 | 0 | 1 | 20 % | |||
| fever | 1 | 0 | 0 | 1 | 20 % | |||
| cough | 0 | 0 | 0 | 0 | 0% | |||
| shortness of breath | 0 | 0 | 0 | 0 | 0% | |||
| sore throat | 0 | 0 | 0 | 0 | 0% | |||
| asymptomatic | 1 | 0 | 0 | 1 | 20 % | |||
5. Discussion
The aim of this study was to determine the SARS-CoV-2 seroprevalence in healthcare workers of the University Hospital Essen, Germany. In 5 of 316 (1.6 %) healthcare workers antibodies could be detected. The seroprevalence was lower in the high-risk group vs. intermediate-risk group (3/244 (1.2 %) vs. 2/37 (5.4 %), with an odds ratio of 0.22 (confidence interval 95 % 0.04–1.35; p = 0.13). No participant of the low-risk group tested positive for SARS-CoV-2-IgG antibodies. These findings reveal the overall seroprevalence is low, which corresponds to another study from the Santa Clara County, United States with approximately 3500 subjects and a seroprevalence of 1.5 % [9]. Other studies observe higher infection rates in healthcare workers. In a study of 957 employees in another German tertiary hospital 52 (5.4 %) employees tested positive for SARS-CoV-2 PCR. The authors underline the vulnerability of healthcare workers in the ongoing pandemic. Similar findings were observed in a Dutch study of 1353 healthcare workers of whom 86 (6%) were tested positive for SARS-CoV-2 via nasal swab [10]. Interestingly the authors suppose the infection to be community acquired during the early phase of pandemic. An even higher rate of infection of healthcare workers was observed in a study from the United Kingdom by Keeley et al., where 1533 symptomatic healthcare workers were tested for SARS-CoV-2 infection via PCR of whom 282 (18 %) were tested positive [11]. They conclude that early identification of symptomatic staff members is crucial to avoid virus transmission due to staff members and to maximize the available workforce. However, comparison to the current study is restricted since the other studies used nasal swab and PCR to determine the rate of infection, although the nasal swab has a volatile positive rate which depends on the practical application and the onset of infection [12] and the PCR has to be improved [13].
An important approach to prevent patient-to-staff infection is the adherence to hygiene guidelines. The low seroprevalence in the high-risk group might be an indicator that the local hygiene standard is effective (Fig. 1). However, the higher seroprevalence in the intermediate-group suggests that the awareness of COVID-19 patient-to staff transmission must be maintained, even in non−COVID-19 wards. Yet the current study did not evaluate the adherence to local guidelines. To estimate the efficiency of the hygiene standard determination of SARS-CoV-2 seroprevalence might be performed. Furthermore it can provide an overview of the current seroprevalence of the population in the context of missing vaccination and in the context development of herd immunity [14]. Healthcare workers with immunity against SARS-CoV-2 may be less vulnerable for SARS-CoV-2 infection. However antibody detection is no assurance of protective immunity [15].
An interesting finding of the current study underlines the limitation of the nasal swab diagnostic since in four subject the PCR diagnostic was negative though antibody detection was positive. In addition one subject with SARS-CoV-2 antibody detection was asymptomatic. Asymptomatic infections could be observed in other studies in up to 50 % of cases [16,17]. This is another important aspect for the adherence to hygiene standards since asymptomatic infection provide a route of community acquired SARS-CoV-2 infection into hospital care.
In conclusion the seroprevalence of healthcare workers of a tertiary hospital in Germany was 1.6 %. The local hygiene standard might be effective to provide patient-to-staff transmission at the COVID-19 wards. Awareness for COVID-19 infections is crucial even in non−COVID-19 wards.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
Andreas Kribben has received grants for clinical studies, speaker’s fee, honoraria and travel expenses from Actelion, Amgen, Amicus, Alexion, Astellas, Bayer, Baxter, Binding Site, Bristol Myers, Chiesi, CytoSorbents, Fresenius, GlaxoSmithKline, Hexal, Janssen, Kyowa Kirin, MSD, Novartis, Otsuka, Peripal, Pfizer, Roche, Sanofi, Shire, Teva, and Vifor Fresenius Medical. Oliver Witzke has received research grants for clinical studies, speaker’s fees, honoraria and travel expenses from Amgen, Alexion, Astellas, Basilea, Biotest, Bristol-Myers Squibb, Correvio, Chiesi, Gilead, Hexal, Janssen, Dr. F. Köhler Chemie, MSD, Novartis, Roche, Pfizer, Sanofi, TEVA and UCB. Johannes Korth has received grants speaker's fee, honoraria and travel expenses from Astellas, Basilea, Chiesi, Janssen, Novartis and Roche. The other authors declared no conflict of interests.
Author contributions
Johannes Korth: Project administration, Conceptualization, Methodology, Investigation, Writing - Original Draft; Anke Herrmann: Project administration, Investigation, Conceptualization, Methodology, Investigation, Writing - Original Draft; Benjamin, Wilde: Conceptualization, Methodology, Investigation, Writing - Original Draft; Sebastian Dolff: Methodology, Writing - Original Draft; Olympia E. Anastasiou: Conceptualization, Methodology, Writing - Original Draft, Validation; Adalbert Krawczyk: Methodology, Investigation, Validation; Michael Jahn: Resources, Investigation, Writing - Original Draft; Sebastian Cordes: Resources, Investigation, Writing - Original Draft; Birgit Ross: : Methodology, Investigation; Stefan Esser: : Methodology, Investigation, Resources; Monika Lindemann: Methodology, Investigation, Resources; Andreas Kribben: Conceptualization, Methodology, Writing - Original Draft; Ulf Dittmer: Conceptualization, Methodology, Writing - Original Draft, Investigation; Oliver Witzke: Conceptualization, Methodology, Investigation, Writing - Original Draft; All authors approved the final manuscript.
Acknowledgements
The authors would like to thank Hannah Pfeng, Assia Omairatte, Emel Güngör and Dana Haffke for excellent assistance. Oliver Witzke is supported by an unrestricted grant of the Rudolf-Ackermann-Stiftung (Stiftung für Klinische Infektiologie).
References
- 1.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., Zhao X., Huang B., Shi W., Lu R., Niu P., Zhan F., Ma X., Wang D., Xu W., Wu G., Gao G.F., Tan W. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020 doi: 10.1056/nejmoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hoehl S., Berger A., Kortenbusch M., Cinatl J., Bojkova D., Rabenau H., Behrens P., Böddinghaus B., Götsch U., Naujoks F., Neumann P., Schork J., Tiarks-Jungk P., Walczok A., Eickmann M., Vehreschild M.J.G.T., Kann G., Wolf T., Gottschalk R., Ciesek S. Evidence of SARS-CoV-2 infection in returning travelers from Wuhan, China. N. Engl. J. Med. 2020 doi: 10.1056/NEJMc2001899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Luo Y., Trevathan E., Qian Z., Li Y., Li J., Xiao W., Tu N., Zeng Z., Mo P., Xiong Y., Ye G. Asymptomatic SARS-CoV-2 infection in household contacts of a healthcare provider, Wuhan, China. Emerg. Infect. Dis. 2020;26 doi: 10.3201/eid2608.201016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weissman D.N., de Perio M.A., Radonovich L.J. COVID-19 and risks posed to personnel during endotracheal intubation. JAMA. 2020 doi: 10.1001/jama.2020.6627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wong S.C.Y., Kwong R.T.S., Wu T.C., Chan J.W.M., Chu M.Y., Lee S.Y., Wong H.Y., Lung D.C. Risk of nosocomial transmission of coronavirus disease 2019: an experience in a general ward setting in Hong Kong. J. Hosp. Infect. 2020 doi: 10.1016/j.jhin.2020.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Petherick A. Developing antibody tests for SARS-CoV-2. Lancet. 2020;395:1101–1102. doi: 10.1016/S0140-6736(20)30788-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pan X., Chen D., Xia Y., Wu X., Li T., Ou X., Zhou L., Liu J. Asymptomatic cases in a family cluster with SARS-CoV-2 infection. Lancet Infect. Dis. 2020;20:410–411. doi: 10.1016/S1473-3099(20)30114-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu J., Liang J., Zhou H., Peng F., Wang B., Jiang W., Jia B., Luo T. Clinical features and outcomes of asymptomatic cases of SARS-CoV-2 infection. J. Infect. 2020 doi: 10.1016/j.jinf.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bendavid E., Mulaney B., Sood N., Shah S., Ling E., Bromley-Dulfano R., Lai C., Weissberg Z., Saavedra R., Tedrow J., Tversky D., Bogan A., Kupiec T., Eichner D., Gupta R., Ioannidis J., Bhattacharya J. COVID-19 antibody seroprevalence in Santa Clara County, California. MedRxiv. 2020 doi: 10.1101/2020.04.14.20062463. 2020.04.14.20062463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Van Den Bergh M.F.Q.K.- 2020. SARS- CoV- 2 Infection in 86 Healthcare Workers in Two Dutch Hospitals in March; pp. 1–16. [Google Scholar]
- 11.Keeley A.J., Evans C., Colton H., Ankcorn M., Cope A., State A., Bennett T., Giri P., de Silva T.I., Raza M. Roll-out of SARS-CoV-2 testing for healthcare workers at a large NHS Foundation Trust in the United Kingdom, March 2020. Euro Surveill. 2020;25:1–4. doi: 10.2807/1560-7917.ES.2020.25.14.2000433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yang Y., Yang M., Shen C., Wang F., Yuan J., Li J., Zhang M., Wang Z., Xing L., Wei J., Peng L., Wong G., Zheng H., Liao M., Feng K., Li J., Yang Q., Zhao J., Zhang Z., Liu L., Liu Y. Evaluating the accuracy of different respiratory specimens in the laboratory diagnosis and monitoring the viral shedding of 2019-nCoV infections. MedRxiv. 2020 doi: 10.1101/2020.02.11.20021493. 2020.02.11.20021493. [DOI] [Google Scholar]
- 13.Toptan T., Hoehl S., Westhaus S., Bojkova D., Berger A. 2020. Optimized qRT-PCR Approach for the Detection of Intra- and Extra- Cellular SARS-CoV-2 RNAs. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.KWOK K.O., Lai F., Wei W.I., WONG S.Y.S., TANG J. Herd immunity – estimating the level required to halt the COVID-19 epidemics in affected countries. J. Infect. 2020;6:0–1. doi: 10.1016/j.jinf.2020.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Perera R.A.P.M., Mok C.K.P., Tsang O.T.Y., Lv H., Ko R.L.W., Wu N.C., Yuan M., Leung S., Chan J.M.C., Chik T.S.H., Choi C.Y.C., Leung K., Chan K.H., Chan K.C.K., Wu J.T., Wilson I.A., Monto A.S., Poon L.L.M., Peiris M. 2020. Serological Assays for Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), March 2020, 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Day M. Covid-19: identifying and isolating asymptomatic people helped eliminate virus in Italian village. BMJ. 2020;368:m1165. doi: 10.1136/bmj.m1165. [DOI] [PubMed] [Google Scholar]
- 17.Mizumoto K., Kagaya K., Zarebski A., Chowell G. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Eurosurveillance. 2020;25:1–5. doi: 10.2807/1560-7917.es.2020.25.10.2000180. [DOI] [PMC free article] [PubMed] [Google Scholar]