Abstract
The leaves of Carica papaya have been used to treat thrombocytopenia in Dengue fever in areas where the virus is endemic. This case series describes the use of C. papaya leaf liquid extract (CPLE) as an adjunctive therapy for four patients receiving standard-of-care treatment for chronic immune thrombocytopenic purpura (ITP). The cases presented here indicate that CPLE may prove beneficial in the management of chronic ITP for patients interested in alternative therapy before progressing to second-line treatments. A larger clinical trial is warranted to evaluate CPLE as an adjunctive therapy in chronic ITP.
Introduction
Immune thrombocytopenic purpura (ITP) is a bleeding disorder defined by an isolated peripheral blood platelet count below 100 x 103/ml that is not otherwise associated with a systemic disease.1 It is characterized by the presence of auto-antibodies against platelet antigens that primarily accelerate platelet clearance but may also interfere with platelet production and function.2 Corticosteroids are the standard first-line therapy for ITP, but the administration of these drugs is limited due to the significant complications associated with long term corticosteroid use including diabetes, osteoporosis, hypertension, gastrointestinal distress, and immunosuppression.3 While 70-80% of patients with ITP may respond to corticosteroid therapy within this time frame, the estimated 10 year disease free survival is only 13-15%.3 Surgical splenectomy is a commonly recommended second-line therapy for low platelet count refractory to initial treatment. Possible complications resulting from splenectomy include bleeding, infection, and thrombosis.4 However, 14% of patients do not respond to splenectomy and 20% of those who do respond relapse in weeks or months.4 In light of the potential challenges associated with standard treatments, new non-invasive therapies are needed to treat ITP.
Carica papaya L. (Caricaceae) is best known in the west as a crop cultivated in tropical and subtropical regions for its fleshy fruit.5 Aside from the use of its fruit as a food source, the leaves of C. papaya have been used in traditional medicine to treat a variety of ailments, most notably Dengue fever. Dengue virus is capable of binding platelets and inducing immune-mediated platelet clearance which manifests as thrombocytopenia ≤100 x 103/ml in the critical phase of the illness.6 Numerous case reports have shown that the administration of C. papaya leaf extract (CPLE) in various doses increases platelet count in Dengue in humans.7-10 Ahmad et al. found that 25 mL of aqueous CPLE administered twice daily for five consecutive days to a patient infected with Dengue was associated with an increase in platelet count from 55 to 168 x 103/ml.7 Another case series of twelve Dengue patients reported that two 5 mL doses of aqueous CPLE administered on the third day of fever was associated with an increased platelet count within 24 hours and full recovery in all patients with no hospital admission.11 Most recently, an open-label randomized controlled trial of 228 patients already receiving standard treatment for Dengue investigated the effect of juice from 50 g of fresh C. papaya leaf daily for three consecutive days and showed a significant increase in mean platelet count at 40 hours and 48 hours in the intervention group compared to standard of care alone.12
Laboratory studies in murine models also support the use of CPLE to increase platelets. In one study, a palm oil suspension of CPLE in a single dose of 15 mg/kg to healthy mice revealed significantly higher mean platelet counts at 1, 2, 4, 8, 10, and 12 hours after dosing compared to the mean count at hour 0.13 A second murine study found that aqueous CPLE administered at 2 g for seven consecutive days showed significantly increased platelet and red blood cell counts compared to controls.14 In rats with cyclophosphamide induced thrombocytopenia, CPLE was found to significantly increase platelet count when given at 400 mg/kg or 800 mg/kg for 15 consecutive days.15 Finally, CPLE has been shown to both protect against and reverse lead acetate-induced damage to the bone marrow in mice by stimulating hematopoiesis of bone marrow cells, particularly megakaryocytes, the precursors to platelets.16
The mechanism by which CPLE increases platelet count is not currently understood. However, one in vitro study by Aziz et al. showed that when applied to peripheral blood leukocytes, CPLE significantly increased secretion of interleukin-6.17 These authors hypothesized that IL-6 may increase platelet count both directly by stimulating proliferation of hematopoietic progenitors and indirectly through its action on thrombopoietin production in liver cells.17
Methods
This case series describes the use of CPLE in the adjunctive care of four patients with chronic immune thrombocytopenic purpura. Patients in this case series were given either 1000 mg TID of 10:1 liquid glycerin extract of C. papaya leaf or 1200 mg TID of dried 10:1 glycerin extract of C. papaya leaf capsules as adjunctive therapy in addition to conventional standard of care. A toxicity study in rats revealed that CPLE extract was safe at a dose of 2 g/kg, 14 times the dose consumed in traditional medicine and 30 times the maximum dose consumed in this case series (0.06 g/kg).18 Hematologic parameters including platelet count and adverse events were recorded for each patient over time.
Results
Case 1
A 67 year old Caucasian male was first diagnosed with ITP on March 9, 1999. His initial presentation revealed a platelet count of 55 x 103/ml and bone marrow biopsy showed numerous megakaryocytes with no abnormal cell infiltration. The patient had no known allergies. Family history was significant for ITP in his mother and one brother. His medical history included a diagnosis of hypothyroid managed with levothyroxine 200 mcg/day and hyperlipidemia managed with gemfibrozil 600 mg BID. His ITP was initially treated with prednisone 100 mg/day. Platelet count increased to 222 x 103/ml by March 18th, 1999. He completed a prednisone taper by May 11th, 1999 and remained in remission for over 10 years.
On June 21st, 2013, after the patient reported increased bruising, platelet count was found to be 61 x 103/ml. He was closely monitored and his platelet count returned to normal spontaneously over the following two weeks. On August 27th, his platelet count dropped again to 5 x 103/ml and a manual differential showed rare large platelets. Prednisone was initiated at 100 mg/day, but as of September 4th, his platelet count had not responded to the steroid treatment. The patient was given an infusion of intravenous immunoglobulin (IVIg) and 250 mg of intravenous methylprednisolone sodium succinate on September 4th and then an additional infusion of IVIg on September 5th. On September 9th, platelet count was below 10 x 103/ml and prednisone was increased to 125 mg/day. A bone marrow biopsy revealed increased megakaryocytes, confirming ITP and ruling out hematolymphoid malignancy. At this time, the patient was diagnosed with steroid refractory ITP and was informed that he should consider splenectomy as he was a good candidate for surgery. He refused splenectomy and against medical advice stated that he wanted to wait for spontaneous remission. His platelet count remained below 5 x 103/ml and on September 13th, he was given a platelet transfusion.
On September 17th, the patient was referred to a naturopathic physician to discuss alternative treatments for low platelet count. The naturopathic physician recommended 1000 mg TID of liquid CPLE in addition to standard conventional medical care as indicated by his hematologist. The patient continued taking prednisone 125 mg/day alone until September 30th and then began taking both prednisone and CPLE as directed. His platelet levels doubled from 33 x 103/ml to 78 x 103/ml over three days beginning on October 1st. By October 8th, his platelet count entered the normal range at 148 x 103/ml and he was able to begin a prednisone taper at that time. He continued taking CPLE 1000 mg TID through the end of November and completed the prednisone taper by December 22nd, after which his platelets remained elevated for four months without intervention.
On March 25th, 2014, the patient relapsed and platelet count fell to 65 x 103/ml. He then initiated CPLE capsules 1200 mg TID alone. On April 4th, his platelets had dropped to 35 x 103/ml so he added prednisone 10 mg/day. His platelet count returned to 310 x 103/ml by April 11th, 2014. He then decreased CPLE to 600 mg TID and his platelet count remained normal for over five months.
The patient reported that he noticed no side effects during the time when he took CPLE. However, over the course of the episode of thrombocytopenia from August 2013 through November 2013, the patient experienced a number of side effects that can be attributed to prednisone treatment. Most notably, his fasting blood glucose increased from a baseline reading of 99 mg/dL on June 21st to a maximum of 309 mg/dL on September 24th. On October 8th, he reported new onset peripheral neuropathy and vision changes. He was diagnosed with corticosteroid-induced diabetes mellitus type II and initiated Metformin 500 mg BID plus insulin. After completing the prednisone taper, his blood glucose returned to normal levels and he was able to discontinue these medications. Finally, the patient reported joint stiffness and pain shortly after the discontinuation of prednisone and C. papaya, and was subsequently diagnosed with rheumatoid arthritis.
Case 2
A 21 year-old female was diagnosed with ITP in September 2011 after diagnostic workup for mild bruising revealed a platelet count of 2 x 103/ml. No other records are available from that time. The patient had no known allergies and no significant medical conditions. She was referred to a hematologist and treated with prednisone and several courses of IVIg during the following year and experienced a moderate, but transient, platelet response. She experienced mood swings and irritability during treatment and elected to discontinue steroid and IVIg treatment in late 2012. The patient’s platelet count remained between 10-15 x 103/ml through September 2013 without any pharmaceutical intervention.
On October 2nd, 2013, the patient was referred to a hematologist at our clinic and received a recommendation to proceed with splenectomy. The splenectomy was performed on November 7th. Her platelet count increased to 188 x 103/ml within four days following the procedure, but over the next four months, her platelet count decreased to between 30-95 x 103/ml. She was not taking any medication during this time.
The patient was referred to a naturopathic physician on April 22nd, 2014 to discuss alternative treatment for ITP. At this visit, her platelet count was 95 x 103/ml, and she was instructed to take CPLE liquid 1000 mg TID. She initiated treatment with CPLE as directed on April 24th, and by May 8th, the patient’s platelet count had increased to 156 x 103/ml. At this time, her naturopathic physician advised her to discontinue CPLE and to have her platelet count retested in one week. On May 15, the patient’s platelet count was reassessed and remained in the normal range at 146 x 103/ml. The patient reported that she noticed no side effects during the time when she took CPLE except possibly improved digestion. The patient was then lost to follow up.
Case 3
A 56 year-old Caucasian male presented with isolated thrombocytopenia of unknown etiology discovered after routine screening prior to coronary angiography performed in December 2011. At the time of diagnosis, his platelet count was 85 x 103/ml with normal WBC (5.0 K/μl) and RBC (5.32 m/μl). The patient had a previous diagnosis of Lyme disease in 1998 and no known allergies. His family history was positive for rheumatoid arthritis in his sister and leukemia in his paternal uncle. On March 28th, 2012, his platelets were 17 x 103/ml and steroid therapy was initiated with prednisone 60 mg/day. The patient’s platelets initially responded to steroid therapy, increasing to 169 x 103/ml by May 8th, 2012. His platelet count remained above 70 x 103/ml with prednisone 10 mg QOD for the next three months.
On September 19th, 2012, the patient’s platelet count dropped to 37 x 103/ml and he was referred to a surgeon for splenectomy, scheduled for November 8th, 2012. The patient was advised to stop taking prednisone at this time, to be reinstituted at a higher dose based on the date of surgery. The patient’s sister advised him to try taking CPLE before surgery and he initiated CPLE liquid 1000 mg TID in late September 2012. The patient reportedly did not initiate high dose prednisone prior to surgery as recommended, but instead remained on low-dose prednisone 10 mg every other day due to patient preference. The patient’s platelet count remained between 25-45 x 103/ml until November 1st, when it increased to 78 x 103/ml. On November 7th, 2012, pre-surgical labs revealed a platelet count of 115 x 103/ml, and the splenectomy was cancelled by the surgeon because platelets were higher than the level of 100 x 103/ml required for the diagnosis of ITP.
The patient’s platelets remained stable over 75 x 103/ml for two months on CPLE 3,000 mg/day and prednisone 10 mg QOD. He was able to discontinue prednisone in January 2013 and his platelet count was maintained above 75 x 103/ml for two additional months on CPLE alone. On March 25th, 2013, his platelet count dropped to 42 x 103/ml. The patient was advised to proceed with a splenectomy if his platelets dropped below 40 x 103/ml. The patient elected to continue CPLE alone and check platelets every two weeks; however, by April 29th, his platelet count dropped to 37 x 103/ml and he agreed to proceed with splenectomy. The patient continued CPLE 3000 mg/day prior to surgery and initiated pre-surgery prednisone taper on May 17th, 2013. Although the patient’s platelets increased to 118 x 103/ml by June 3rd, 2013, the splenectomy proceeded as scheduled on June 7th, 2013. The patient reported no new side effects or adverse events while taking C. papaya extract. He did experience relative lymphopenia throughout this time period that was attributed to prednisone use.
Case 4
A 60 year-old Caucasian female was diagnosed with ITP in 1992 while undergoing routine lab work for hysterectomy and oophorectomy. The patient’s platelet count was reportedly in the range of 30-40 x 103/ml at this time, though exact numbers are not available. A bone marrow biopsy was performed that excluded other causes for thrombocytopenia. The patient was managed by various physicians with low dose prednisone ranging from 5-10 mg/day for more than 20 years. Her medical history included a diagnosis of ulcerative colitis and with total colectomy in 1999 and a subsequent episode of J-pouchitis in March 2014 treated with budesonide 3 mg TID. The patient was referred to a naturopathic physician on May 6th, 2013 after refusing splenectomy as recommended by numerous previous physicians. At the time of referral, the patient’s platelet count was reported at 86 x 103/ml and she was being treated with prednisone 5 mg/day. At the recommendation of the naturopathic physician, the patient initiated treatment CPLE liquid 1000 mg TID in addition to prednisone. On May 12th, the patient’s platelet count had risen to 109 x 103/ml, but subsequently dropped to 98 x 103/ml by May 20th. CPLE was discontinued at this time due to lack of beneficial action on platelet count. The patient denied any adverse effects or new symptoms after starting CPLE.
Discussion
In this case series, patients with chronic ITP refusing second line therapies such as Rituximab or splenectomy received CPLE as an adjunctive treatment to increase platelet count. CPLE was well-tolerated by all four patients with no new symptoms or adverse events reported after administration. In three of the four cases, administration of CPLE was associated with at least one episode of increased platelet count. Most notably, in Case 2, the administration of CPLE liquid 1000 mg TID for two weeks duration was associated with an increase in platelet count from 95 x 103/ml to 156 x 103/ml in a patient with chronic ITP post-splenectomy. However, the association between CPLE and increased platelet count was not observed in all cases. In Case 4, platelet count did not increase after the addition of CPLE 1000 mg TID for two weeks to a chronic low-dose prednisone regimen of 5-10 mg/day. Therefore, prospective and comparative studies are needed to definitively establish CPLE as an adjunctive treatment for chronic ITP and to determine appropriate dose and duration of treatment. Corticosteroids are the standard first-line treatment for ITP. These drugs have a duration of use limited to four consecutive weeks due to significant complications associated with long-term use.3 Even so, corticosteroids are often prescribed for longer periods in patients with chronic ITP whose platelets remain below 30-50 x 103/ml after four weeks of treatment.19 In two of the four cases reported here, the addition of CPLE to oral prednisone therapy was associated with an increase in platelet count. For example, in Case 1, during an episode of thrombocytopenia, the addition of CPLE was associated with an increase in platelet count from 35 to 310 x 103/ml without increasing oral prednisone beyond 10 mg/day. During a previous episode of thrombocytopenia, a four-week course of prednisone of up to 125 mg/day was administered prior to raising the platelet count. As a result of this high-dose prednisone regimen, the patient developed both type 2 diabetes mellitus and white blood cell abnormalities. In Case 3, a combination of low-dose oral prednisone and CPLE was associated with an increased platelet count, allowing the patient to postpone splenectomy for more than six months. Results from these cases suggest that CPLE may reduce the amount of prednisone needed to maintain normal platelet counts in some patients with chronic ITP, thereby reducing the risk of further complications associated with corticosteroid use. However, additional research is needed to determine both the association between CPLE and increased platelet count and the relationship between CPLE and corticosteroid treatment in patients with chronic ITP.
Second-line treatments for patients with chronic ITP who do not respond to corticosteroids include splenectomy as well as several newly developed medical therapies such as Rituximab.20 According to the most recent guidelines from the American Society for Hematology, splenectomy has the highest level of evidence (Grade 1B) for patients with ITP who fail to respond to corticosteroids; however, the rate of remission of ITP at one-year post-splenectomy ranges from 70-80%.20 In Case 2, the use of CPLE 1000 mg TID for two weeks in a patient with a relapse of ITP post-splenectomy was associated with an increase in platelet count from 95 x 103/ml to 156 x 103/ml, suggesting that CPLE may have a role when used alone in patients with refractory ITP. Of note, no cases in this series included the use of Rituximab or other medical second-line therapies. More research is also needed to further evaluate the association between CPLE and increased platelet count in patients with refractory ITP.
While this case series suggests a possible role for C. papaya in the treatment of chronic ITP, it does have several limitations. Primary ITP is now considered to be a heterogeneous condition that can involve a variety of etiologies including infections and immunodeficiency states;2 it is therefore possible that C. papaya is only effective in certain manifestations of ITP. Additionally, epidemiologic research shows that patients with chronic ITP recover spontaneously without intervention at a rate of 11%, so it is impossible to attribute the changes in platelet count observed here to any intervention without a control group.21 Finally, the dose and duration of treatment with C. papaya was not identical in all cases presented here. Studies in patients with Dengue fever have shown therapeutic results with varying doses of C. papaya ranging from one to five days duration,7-12 but patients in this case series used C. papaya for at least two weeks, which may suggest that patients with chronic ITP may require a larger dose or longer duration. Future studies are needed to determine the ideal dose and duration of treatment with C. papaya in humans with ITP.
Conclusion
C. papaya leaf aqueous extract may prove beneficial in the management of chronic ITP for patients interested in alternative therapy before progressing to second-line treatments such as Rituximab or splenectomy. Based on the positive association observed in these cases, a larger clinical study is warranted to evaluate C. papaya as an adjunctive therapy in refractory ITP. This case series indicates that a dose of C. papaya leaf 10:1 glycerin extract at 3000 mg/day for two weeks may be sufficient for a preliminary trial in patients with chronic ITP.
Figure 1.
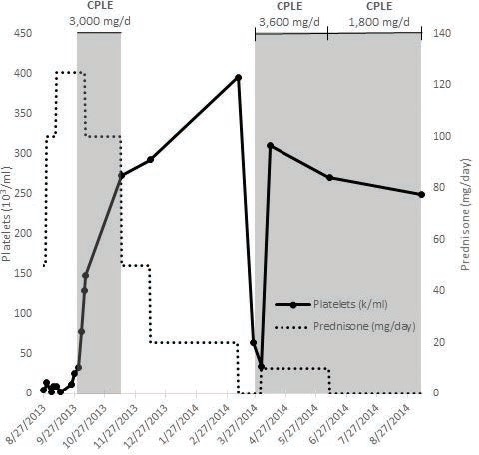
Case 1 platelet count, prednisone dosage, and CPLE dosage over time.
Figure 2.
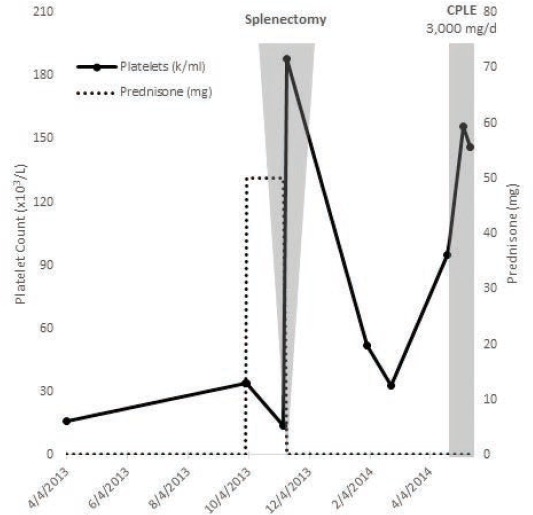
Case 2 platelet count, prednisone dosage, and CPLE dosage over time.
Figure 3.
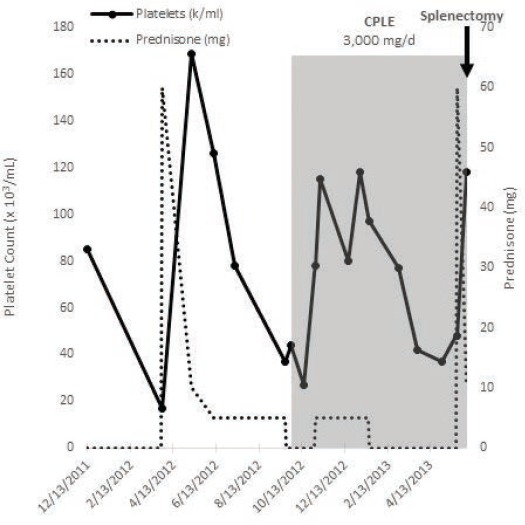
Case 3 platelet count, prednisone dosage, and CPLE dosage over time.
Figure 4.
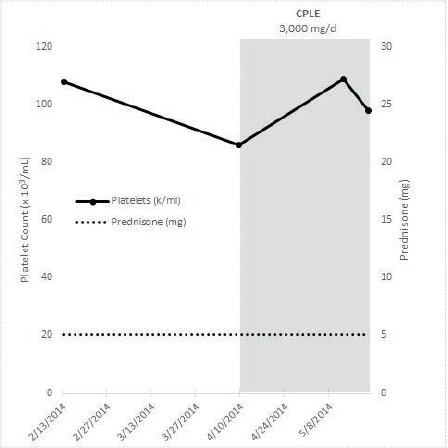
Platelet count, prednisone dosage, and CPLE dosage over time.
References
- 1.Rodeghiero F, Stasi R, Gernsheimer T, et al. Standardization of terminology, definitions and outcome criteria in immune thrombocytopenic purpura of adults and children: report from an international working group. Blood. 2009;113(11):2386-2393. [DOI] [PubMed] [Google Scholar]
- 2.Cines DB, Bussel JB, Liebman HA, Prak ET. The ITP synrome: pathogenic and clinical diversity. Blood. 2009;113(26):5411-6521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Provan D, Stasi R, Newland AC, et al. International consensus report on the investigation and management of primary immune thrombocytopenia. Blood. 2010;115(2):168-186. [DOI] [PubMed] [Google Scholar]
- 4.Schwartz J, Leber MD, Gillis S, et al. Long term follow-up after splenectomy performed for immune thrombocytopenic purpura (ITP). Am J Hematol. 2003;72(2):94-98. [DOI] [PubMed] [Google Scholar]
- 5.Aravind G, Bhownik D, Duraviel S, Harish G. Traditional and medicinal uses of Carica papaya. Journal of Medicinal Plant Studies. 2013;1(1):7-15. [Google Scholar]
- 6.Gan VC. Dengue: moving from current standard of care to state-of-the-art treatment. Current Treatment Options in Infectious Disease. 2014;6:208-226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahmad N, Fazal H, Ayaz M, Abbasi BH, Mohammad I, Fazal L. Dengue fever treatment with Carica papaya leaves extracts. Asian Pac J Trop Biomed. 2011;1(4):330-333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Deepak BS, Grish KJ, Jadhav L. Effect of papaya leaf juice on platelet and WBC count in dengue fever: a case report. JAHM. 2013;1(3):44-47. [Google Scholar]
- 9.Sarala N, Paknikar SS. Papaya extract to treat dengue: A novel therapeutic option? Ann Med Health Sci Res. 2014;4:320-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Siddique O, Sundus A, Ibrahim MF. Effects of papaya leaves on thrombocyte counts in dengue—a case report. J Pak Med Assoc. 2014;64(3):364-6. [PubMed] [Google Scholar]
- 11.Hettige S. Salutary effects of Carica papaya leaf extract in dengue fever patients—a pilot study. Sri Lankan Family Physician. 2008;29(1):17-19. [Google Scholar]
- 12.Subenthiran S, Choon TC, Cheong KC, Thayan R, Teck MB, Muniandy PK, Afzan A, Abdullah NR, Ismail Z. Carica papaya leaves juice significantly accelerates the rate of increase in platelet count among patients with dengue fever and dengue hemorrhagic fever. Evid Based Complement Alternat Med. 2013;1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sathasivam K, Ramanathan S, Mansor SM, Haris MR, Wernsdorfer WH. Thrombocyte counts in mice after the administration of papaya leaf suspension. Wien Klin Wochenschr. 2009;121(3):19-22. [DOI] [PubMed] [Google Scholar]
- 14.Dharmarathna S, Wickramasinghe S, Waduge RN, Rajapakse R, Kularatne S. Does Carica papaya leaf extract increase the platelet count? An experimental study in a murine model. Asian Pac J Trop Biomed. 2013. 3(9):720-724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Patil S, Shetty S, Bhide R, Narayanan S. Evaluation of platelet augmentation activity of Carica papaya leaf aqueous extract in rats. J Pharmacogn Phytochem. 2013;1(5):57-60. [Google Scholar]
- 16.Tham CS, Chakravarthi S, Haleagrahara N, Alwis R. Morphological study of bone marrow to assess the effects of lead acetate on haemopoiesis and aplasia and the ameliorating role of Carica papaya extract. Exp Ther Med. 2013;5(2):648-652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aziz J, Abu Kassim NL, Abu Kasim NH, Haque N, Rahman MT. Carica papaya induces in vitro thrombopoietic cytokines secretion by mesenchymal stem cells and haematopoietic cells. BMC Complement Altern Med. 2015;15(215): epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Afzan A, Abdullah NR, Halim SZ, Rashid BA, Semail RHR, Abdullah N, Jantan I, Muhammad H, Ismail Z. Repeated dose 28-days oral toxicity study of Carica papaya L. leaf extract is sprague dawley rats. Molecules. 2012;17(4):4326-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.George JN, El-Harake MA, Raskob GE. Chronic idiopathic thrombocytopenic purpura. NEJM 1994;331:1207-1211. [DOI] [PubMed] [Google Scholar]
- 20.Stasi R, Amadori S, Osborn J, Newland AC, Provan D. Long-term outcome of otherwise healthy individuals with incidentally discovered borderline thrombocytopenia. PLoS Med. 2006;3: e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Neunert C, Lim W, Crowther M, Cohen A, Solberg L, Jr., Crowther MA. The American Society of Hematology 2011 evidence-based practice guideline for immune thrombocytopenia. Blood. 2011;117(16):4190-4207. [DOI] [PubMed] [Google Scholar]


