Abstract
Polycystic ovarian syndrome (PCOS) is a common cause of menstrual irregularity and hyperandrogenism in women of reproductive age. Conventional treatment is centered around the use of oral contraceptive pills (OCPs) to regulate menstrual cycles, protect against endometrial hyperplasia, and manage clinically evident androgen excess. Many women prefer to avoid OCPs due to concerns about risks and adverse effects, or simply because they desire a non-pharmacologic approach. We present the case of a young woman with a strong preference for a natural approach to her care who presented with PCOS manifesting in menstrual irregularity, acne, and hirsutism. In this case, acupuncture as well as the botanicals Vitex agnus-castus and diindolylmethane were used over a 10-month period. The patient regained menstrual cyclicity, and clinical and biochemical hyperandrogenism normalized. This report underscores the need for an integrative approach to the management of multifactorial disorders such as PCOS and highlights the basic science and clinical data supporting the use of acupuncture, Vitex agnus-castus, and diindolylmethane in patients with this condition.
Introduction
Polycystic ovarian syndrome (PCOS) is one of the most common endocrine disorders in women of reproductive age. Full expression of this disorder can include menstrual irregularity (oligomenorrhea or amenorrhea), androgen excess, insulin resistance, obesity, and polycystic ovarian morphology. The current standard of care for preventing endometrial hyperplasia and treating hyperandrogenism in women with PCOS includes the use of oral contraceptive pills with or without antiandrogens such as spironolactone.1 For women who prefer to avoid these pharmaceutical medications, the ideal therapeutic approach has not been definitively established. This case describes the use of botanical supplements and acupuncture in addressing menstrual irregularity and hyperandrogenism in a young woman with PCOS.
Case Presentation
Our patient is a 21-year-old female with a history of PCOS who presented for an Integrative Medicine consult. She requested a natural approach to balance her hormones and lower her androgen levels. She had a history of abnormal menstrual cycles and was started on oral contraceptive pills (OCPs) at the age of 13 for menstrual regulation. When her irregular cycles persisted after stopping the OCPs at the age of 20, she was evaluated for and diagnosed with PCOS. The diagnosis was based on characteristic findings on transvaginal ultrasound as well as clinical and biochemical evidence of hyperandrogenism. Her predominant symptoms were abnormal menstrual cycles, dysmenorrhea, acne, and hirsutism. Her past medical history was significant for asthma and constipation-predominant irritable bowel syndrome (IBS). Family history was notable only for PCOS in her younger sister. She took no prescription medications but had been taking a botanical supplement containing proanthocyanidins from grape seed and pine bark with the intention of regulating her hormone levels naturally (this was subsequently discontinued). She followed a gluten- and dairy-free diet with low refined sugar intake to control her IBS, and she exercised twice per week, mostly doing weight training.
Timeline.
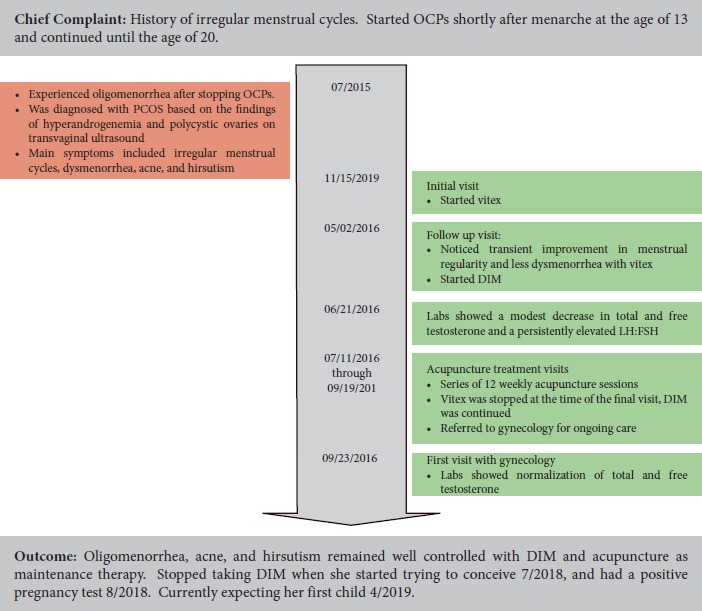
Physical exam was notable for a normal BMI of 20.5 kg/m2 and shaved hair along the linea alba. Baseline labs showed elevated total and free testosterone levels, at 96 ng/dL and 8.4 pg/dL respectively. Sex hormone binding globulin was normal at 78 nmol/L. Luteinizing hormone (LH) to follicle stimulating hormone (FSH) ratio was elevated at almost 3:1. Trans-vaginal ultrasound showed normal sized ovaries with multiple follicles. MRI of the brain showed no pituitary adenoma, and prolactin and TSH were normal. Her lipid panel was normal and hemoglobin A1C was 5.3%.
At her first visit, our patient was started on the herbal supplement Vitex agnus-castus 400 mg twice daily for its progestogenic activity and to aid in menstrual regulation. She was advised to continue to eat a whole foods diet free of gluten, dairy, and refined sugars, and to add yoga to her exercise routine. When she followed up six months later, she reported improved menstrual regularity and less dysmenorrhea with the vitex, but this lasted for only three cycles. In addition, she had noticed increased irritability as well as night sweats. Diindolylmethane (DIM) 100mg daily was added both for its beneficial effects on estrogen metabolism and its antiandrogen effects. Labs done 1 month later showed a modest decrease in total and free testosterone at 86 ng/dL and 5.4 pg/mL, respectively, and a persistently elevated LH to FSH ratio of just under 3:1. At her next follow up visit she complained of persistent hirsutism as well as oligomenorrhea with cycles occurring every 60-65 days. She was advised to continue the vitex and DIM, and she began a series of acupuncture treatments.
Our patient received twelve weekly sessions of acupuncture adapted from a standardized protocol from a clinical trial.2 The following bilateral points were stimulated with electroacupuncture with low frequency (2 Hz): BL 23, Bl 28, SP 6, and SP 9 for 20 minutes. The intensity was adjusted to produce a distinct tapping sensation without discomfort. Needles were inserted to a depth of 10-15 mm without intent to elicit a de qi sensation and without manual stimulation at the following points: PC 6, TW 5, GV 20. In addition to the points described in this protocol, the following body points were stimulated depending on the patient’s presentation at each particular visit: LI 4, LV 3, LI 11 (body points), Shen Men, reproductive point, point zero (auricular points). During two sessions, the SP 6 points were stimulated with electroacupuncture at 10 Hz for 20 minutes. A TDP (Teding Diancibo Pu) heat lamp that provides heat through a mineral plate was placed on the bladder points during the session. Liquid Moxa essence tincture (artemisiae, pericarpium, cinnamomi, fructus piperis capsici, semen sinapsis, zingeberis) was applied to the bladder points after removal of needles.
After the final acupuncture session, androgen levels were rechecked and were found to be in the normal range. Total testosterone was 40ng/dL and free testosterone was 2.8 pg/mL. Our patient’s hirsutism had resolved, and her menstrual cycles had normalized to every 32-34 days. Cycles remained regular and symptoms were well controlled with DIM and acupuncture maintenance therapy.
Discussion
While the exact cause of PCOS is unknown, the predominant theory is that dysregulated steroid hormone production results from the interaction of one of a number of ovarian genetic traits with other hereditary and environmental factors.3 The fact that our patient had a sister with PCOS and that she developed the syndrome herself in the absence of both obesity and insulin resistance highlights the significant role that genetics plays in the development of this syndrome. In fact, in one large twin study, the heritability of PCOS was over 70% among monozygotic twins.4 In addition to genetic inputs, our patient wondered whether or not prolonged use of OCPs could have contributed to her development of PCOS. Some have postulated that polycystic ovaries themselves may develop as a result of chronic anovulation.5 It is a stretch, however, to assert that a persistent anovulatory state can induce the entire syndrome, and to the best of our knowledge, there is no report in the medical literature of a post-pill PCOS.
We used Vitex agnus-castus, DIM, and acupuncture to treat our patient. While there was an improvement in both menstrual regularity and hyperandrogenemia after starting these therapies, a causal relationship is difficult to establish as the three interventions were employed concurrently.
Vitex agnus-castus is an herb that is commonly known for its ability to suppress prolactin release from the pituitary gland. In addition, it has been found to have both estrogen and progesterone activity.6,7 Two randomized placebo controlled trials showed that vitex had beneficial effects in women with oligomenorrhea and amenorrhea.8-10 In one study, women with oligomenorrhea who were given a vitex-containing homeopathic preparation had shorter menstrual cycles, earlier ovulation, and higher mid-luteal progesterone levels than those given placebo.8 In another study, women with irregular menstrual cycles who took a vitex-containing herbal preparation had a statistically significant improvement in menstrual cyclicity compared to those who took a placebo.9
Diindolylmethane (DIM) is a break-down product of indole-3-carbinol, a compound abundant in cruciferous vegetables. While clinical studies on the use of DIM in women with PCOS are lacking, preclinical data suggest that this compound has both estrogenic and anti-androgenic activity.11 The compound’s anti-androgenic properties may be particularly clinically meaningful in women such as our patient with PCOS and hyperandrogenism. Again, the data in this particular population are lacking. DIM’s anti-androgenic effects, however, have been highlighted in other scenarios, such as the suppression of androgen-dependent prostate cancer cell proliferation.12 Whether or not this effect is generalizable remains to be seen.
When studied in women with PCOS, acupuncture was found to improve ovulatory function, increase menstrual frequency, and decrease hyperandrogenicity.13-15 Such improvements have been attributed to acupuncture’s modulation of sympathetic output to target organs and to its modulation of beta-endorphins, which has downstream effects on the release of GnRH and CRH.16 Of note, no difference in ovulation rate or menstrual frequency were reported in women who received true versus sham acupuncture in a randomized, double-blind, sham-controlled clinical trial.2 Although this result casts doubt on the efficacy of acupuncture as an active intervention for PCOS, it has also been argued that the current non-penetrating devices used for placebo/sham control may not be an entirely inert intervention.17 Although point selection for this patient was protocol-based, it was also individually tailored to the patient’s presentation and symptoms (TCM pattern) during each visit. This is consistent with acupuncture as practiced in patient care settings.
In the case presented, the patient stated a clear preference for non-pharmacologic management and was willing to make lifestyle changes to maintain ideal body weight and employ adaptive coping strategies to manage stress. She was able to achieve symptom resolution, menstrual regulation, and correction of the hormonal alteration that drives anovulation. We present this case to highlight the importance of an integrative approach to managing multifactorial conditions such as PCOS.
References
- 1.Goodman NF, Cobin RH, Futterweit W, Glueck JS, Legro RS, Carmina E. American association of clinical endocrinologists, american college of endocrinology, and androgen excess and pcos society disease state clinical review: Guide to the best practices in the evaluation and treatment of polycystic ovary syndrome part 2. Endocrine Practice. 2015;21(12):1415-1426. http://journals.aace.com/doi/abs/10.4158/EP15748.DSCPT2. Accessed Jun 4, 2017. doi: 10.4158/EP15748.DSCPT2. [DOI] [PubMed] [Google Scholar]
- 2.Pastore LM, Williams CD, Jenkins J, Patrie JT. True and sham acupuncture produced similar frequency of ovulation and improved LH to FSH ratios in women with polycystic ovary syndrome. The Journal of Clinical Endocrinology & Metabolism. 2011;96(10):3143-3150. 10.1210/jc.2011-1126. doi: 10.1210/jc.2011-1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ehrman DA, Barnes RB, Rosenfield RL. Polycystic ovary syndrome as a form of functional ovarian hyperandrogenism due to dysregulation of androgen secretion. Endocr Rev. 1995;16(3):322-353. https://academic.oup.com/edrv/article-abstract/16/3/322/2548497/Polycystic-Ovary-Syndrome-as-a-Form-of-Functional. Accessed Jun 4, 2017. doi: 10.1210/edrv-16-3-322. [DOI] [PubMed] [Google Scholar]
- 4.Vink JM, Sadrzadeh S, Lambalk CB, Boomsma DI. Heritability of polycystic ovary syndrome in a dutch twin-family study. J Clin Endocrinol Metab. 2006;91(6):2100-2104. https://academic.oup.com/jcem/article/91/6/2100/2843408/Heritability-of-Polycystic-Ovary-Syndrome-in-a. Accessed Jun 4, 2017. doi: 10.1210/jc.2005-1494. [DOI] [PubMed] [Google Scholar]
- 5.Speroff L, Fritz MA. Clinical gynecologic endocrinology and infertility. Lippincott Williams & Wilkins; 2005. Accessed Jun 4, 2017. [Google Scholar]
- 6.Ibrahim NA, Shalaby AS, Farag RS, Elbaroty GS, Nofal SM, Hassan EM. Gynecological efficacy and chemical investigation of vitex agnus-castus L. fruits growing in egypt. Natural Product Research. 2008;22(6):537-546. 10.1080/14786410701592612. Accessed Jun 4, 2017. doi: 10.1080/14786410701592612. [DOI] [PubMed] [Google Scholar]
- 7.Wuttke W, Jarry H, Christoffel V, Spengler B, Seidlová-Wuttke D. Chaste tree (vitex agnus-castus)--pharmacology and clinical indications. Phytomedicine. 2003;10(4):348-357. Accessed Jun 4, 2017. doi: 10.1078/094471103322004866. [DOI] [PubMed] [Google Scholar]
- 8.Bergmann J, Luft B, Boehmann S, Runnebaum B, Gerhard I. [The efficacy of the complex medication phyto-hypophyson L in female, hormone-related sterility. A randomized, placebo-controlled clinical double-blind study]. Forsch Komplementarmed Klass Naturheilkd. 2000;7(4):190-199. Accessed Jun 4, 2017. doi: 21343. [DOI] [PubMed] [Google Scholar]
- 9.Gerhard N, Patek N, Monga N, Blank N, Gorkow N. Mastodynon(R) bei weiblicher sterilität. Forsch Komplementarmed. 1998;5(6):272-278. Accessed Jun 4, 2017. doi: 21154. [DOI] [PubMed] [Google Scholar]
- 10.Arentz S, Abbott JA, Smith CA, Bensoussan A. Herbal medicine for the management of polycystic ovary syndrome (PCOS) and associated oligo/amenorrhoea and hyperandrogenism; a review of the laboratory evidence for effects with corroborative clinical findings. BMC complementary and alternative medicine. 2014;14(1):511 http://www.ncbi.nlm.nih.gov/pubmed/25524718. doi: 10.1186/1472-6882-14-511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bovee TFH, Schoonen Willem G E J, Hamers ARM, Bento MJ, Peijnenburg Ad A C M. Screening of synthetic and plant-derived compounds for (anti) estrogenic and (anti)androgenic activities. Anal Bioanal Chem. 2008;390(4):1111-1119. https://link.springer.com/article/10.1007/s00216-007-1772-3. Accessed Jun 4, 2017. doi: 10.1007/s00216-007-1772-3. [DOI] [PubMed] [Google Scholar]
- 12.Le HT, Schaldach CM, Firestone GL, Bjeldanes LF. Plant-derived 3,3’-diindolylmethane is a strong androgen antagonist in human prostate cancer cells. The Journal of biological chemistry. 2003;278(23):21136 21145. http://www.ncbi.nlm.nih.gov/pubmed/12665522. doi: 10.1074/jbc.M300588200. [DOI] [PubMed] [Google Scholar]
- 13.Stener-Victorin E, Waldenström U, Tägnfors U, Lundeberg T, Lindstedt G, Janson PO. Effects of electro-acupuncture on anovulation in women with polycystic ovary syndrome. Acta Obstetricia et Gynecologica Scandinavica. 2000;79(3):180-188. http://kipublications.ki.se/Default.aspx?queryparsed=id:1960241. doi: 10.1080/j.1600-0412.2000.079003180.x. [PubMed] [Google Scholar]
- 14.Jedel E, Labrie F, Odén A, et al. Impact of electroacupuncture and exercise on hyperandrogenism and oligo/amenorrhoea in women with polycystic ovary syndrome: A randomized controlled trial. American journal of physiology. Endocrinology and metabolism. 2011;300(1):E37 https://gup.ub.gu.se/ publication/128958. [DOI] [PubMed] [Google Scholar]
- 15.Julia Johansson, Leanne Redman, Paula P., Veldhuis, et al. Acupuncture for ovulation induction in polycystic ovary syndrome: A randomized controlled trial. American Journal of Physiology - Endocrinology and Metabolism. 2013;304(9):934-943. http://ajpendo.physiology.org/content/304/9/E934. doi: 10.1152/ajpendo.00039.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Johansson J, Stener-Victorin E. Polycystic ovary syndrome: Effect and mechanisms of acupuncture for ovulation induction. Evidence-based complementary and alternative medicine : eCAM. 2013;2013:762615 https://www.ncbi.nlm.nih.gov/pubmed/24073009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhu D, Gao Y, Chang J, Kong J. Placebo acupuncture devices: Considerations for acupuncture research. 2013. http://nrs.harvard.edu/urn-3:HUL.InstRepos:11717649. [DOI] [PMC free article] [PubMed]


