Abstract
Objective:
To systematically review the symptoms and types of laryngeal injuries resulting from endotracheal intubation in mechanically ventilated patients in the intensive care unit (ICU).
Data Sources:
PubMed, Embase, CINAHL, and Cochrane Library from database inception to September 2017.
Study Selection:
Studies of adult patients who were endotracheally intubated with mechanical ventilation in the ICU and completed post-extubation laryngeal examinations with either direct or indirect visualization.
Data Extraction:
Independent, double-data extraction and risk of bias assessment followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Risk of bias assessment followed the Cochrane Collaboration’s criteria.
Data Synthesis:
Nine studies (7 cohort, 2 cross-sectional) representing 775 patients met eligibility criteria. The mean (standard deviation; 95% confidence interval) duration of intubation was 8.2 (6.0; 7.7–8.7) days. A high prevalence (83%) of laryngeal injury was found. Many of these were mild injuries, although moderate to severe injuries occurred in 13%−31% of patients across studies. The most frequently occurring clinical symptoms reported post-extubation were dysphonia (76%), pain (76%), hoarseness (63%), and dysphagia (49%) across studies.
Conclusions:
Laryngeal injury from intubation is common in the ICU setting. Guidelines for laryngeal assessment and post-extubation surveillance do not exist. A systematic approach to more robust investigations could increase knowledge of the association between particular injuries and corresponding functional impairments, improving understanding of both time course and prognosis for resolution of injury. Our findings identify targets for future research and highlight the long-known, but understudied, clinical outcomes from endotracheal intubation with mechanical ventilation in ICU.
Keywords: endotracheal intubation, intensive care, larynx, voice, deglutition
INTRODUCTION
Globally, there are 13–20 million critically ill patients intubated in intensive care units (ICU) annually.1 Similar to many medical treatments, the iatrogenic effects of intubation have potential for acute and chronic symptoms, and both short- and long-term harms requiring further medical care that extends beyond ICU discharge.
Patient complaints frequently include hoarseness, loss of voice, throat clearing, sore throat, and vocal fatigue post-extubation.2–4 Laryngeal injuries from intubation during surgery are believed to be confined to minor injuries.5–7 By comparison, critically ill patients intubated in ICU generally experience longer intubation resulting in laryngeal injuries that are more prevalent, potentially more severe, frequently overlooked, and often result in voice dysfunction (i.e., dysphonia) and/or swallowing dysfunction (i.e., dysphagia).8–15 Despite potentially serious injury, laryngeal evaluations are often delayed, occurring only if symptoms persist ≥1 week,16–18 sometimes as long as 1–3 months.19–21 This delay results, in part, from the absence of guidelines establishing standard practices for post-extubation assessment. Patients with these injuries, therefore, experience increased risk for both medical sequelae (e.g., post-intubation stenosis with delayed presentation22,23) and prolonged functional handicap (e.g., chronic dysphonia,24 chronic dysphagia25).
The purposes of this systematic review are to: (1) evaluate the nature and severity of laryngeal injury after endotracheal intubation in ICU patients and (2) identify areas of inquiry for mitigation strategies and future intervention. We focused on prospective studies with post-extubation laryngoscopic assessment of laryngeal injury.
MATERIALS AND METHODS
Literature Search
A clinical informationist (C.P.) developed and executed the search strategy in the electronic bibliographic databases PubMed, Embase, CINAHL, and Cochrane Library from inception to April 2016, with two updates in March and September 2017 (eAppendix 1). The searches were limited to the English language and created using controlled vocabulary, such as Medical Subject Headings, Emtree terms, and CINAHL headings, in combination with keywords for the concepts of intubation, visualization techniques, and injury where appropriate. Efforts were made to exclude pediatric-focused research by excluding specific pediatric-related terms from the titles only and a filter was applied to exclude animal-only research. A research filter was applied based on the Cochrane Highly Sensitive Search Strategy for identifying randomized trials in MEDLINE, sensitivity and precision-maximizing version26 with additions for other types of clinical studies.
Selection Criteria
Included studies assessed adult (≥18 years old) patients employing either direct (e.g., line of sight) or indirect (e.g., mirror, flexible endoscopy) visualization of the larynx and reported sufficient laryngeal injury data (e.g., frequencies, nature). Exclusion criteria included: (1) non-English language, (2) case studies and retrospective study designs, (3) patients <18 years old, (4) pre-existing laryngeal injury/disease, (5) patients with surgical interventions that have inherent risk of recurrent laryngeal nerve injury (e.g., neck surgeries, thoracic surgeries), (6) gray literature,27 and (7) non-focal, neurologically impaired patient populations in whom neurologic injury may have made assignment of post-intubation dysphonia and dysphagia to laryngeal injury difficult (e.g., stroke).
Data Extraction/Risk of Bias Assessment
Search strategy results were imported to an online platform (Covidence: www.covidence.org, Melbourne, Australia) for independent review. Two authors (B.B., E.J.) independently screened articles by title, abstract, and full text. Disagreements were refereed by a third author (M.B.B.). Six authors (L.M.A., M.B.B., G.C., E.J., M.J.L., V.P.) completed independent, double-data extraction and risk of bias assessment for accepted articles. Risk of bias assessment followed the Cochrane Collaboration’s criteria,28 with each risk parameter judged as low-, unknown-, or high-risk. Disagreements were settled by consensus. Authors were contacted to provide missing information as needed. A meta-analysis was judged to be inappropriate due to substantial heterogeneity of study methods for the accepted articles.29,30
A 4-point grading rubric was used to classify laryngeal injuries, guided by previous publications.14,31,32 The rubric was developed via consensus by 5 authors: 3 laryngologists (L.M.A., S.R.B., A.T.H.), an emergency physician (M.J.L.), and a speech-language pathologist (M.B.B.). Prevalence was calculated as the total number of patients observed with each injury or symptom divided by the total number of patients analyzed across studies analyzing these outcomes, omitting studies that did not analyze a particular outcome and patients that did not meet criteria. All outcomes were assessed post-extubation. Across studies, terminology describing voice quality was inconsistent. For purposes of prevalence, we report dysphonia and hoarseness separately using the terms relevant to each article, but we group these symptoms of laryngeal injury as “voice dysfunction” in our discussion.
RESULTS
Search Results
There were 4530 publications identified from the 4 databases and other sources as part of a larger systematic review on laryngeal injury. Screening by title and abstract resulted in 126 full-text reviews. Of these, 9 studies from 5 countries were accepted with the focus on laryngeal injury from oral endotracheal intubation in mechanically ventilated ICU patients (Figure 1). These 9 studies comprised 7 cohort studies (663 patients)33–39 and 2 cross-sectional studies (112 patients),40,41 totaling 775 patients (Table 1).
Figure 1.
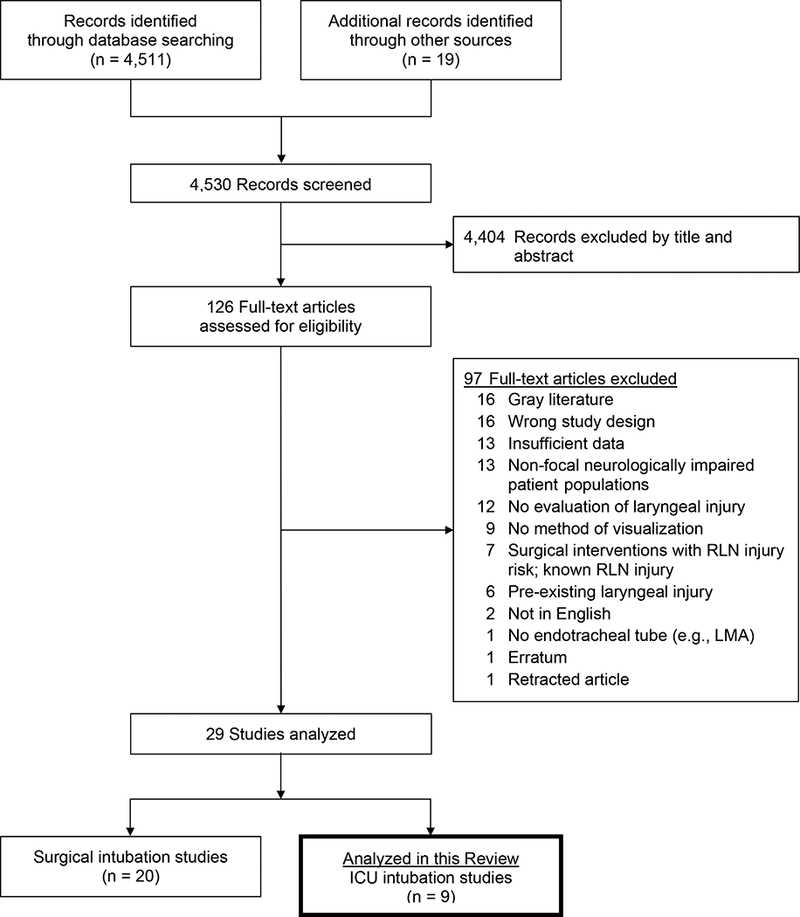
Study selection flowchart.
Table 1.
Methods of included studies.
| Author/Year | Country | Study Design | Number of patients analyzeda |
Mean Patient Age (years) |
ETT size | Method of Visualization |
Duration of Intubation (mean days) |
|---|---|---|---|---|---|---|---|
| Colton House 201140 | United States | Cross-sectional | 61 | 56 | 6.0 – 8.0 | Indirect | 9 |
| Kastonos 198333 | Spain | Cohort | 19 | 59 | 7.0 – 9.0 | Indirect | 6.2 |
| Megarbane 201034 | France | Cohort | 209 | 40 | 6.5 – 8.0 | Indirect | 1.2 |
| Rangachari 200635 | India | Cohort | 51 | 50 | 7.0 – 8.5 | Indirect | 4b |
| Scheel 201641 | United States | Cross-sectional | 51 | 58 | ≤7, ≥8 | Indirect | 9.4 |
| Tadié 201036 | France | Cohort | 136 | 62 | 6.5 – 8.0 | Indirect | 6.9 |
| Van der Meer 201037 | South Africa | Cohort | 32 | 49 | nr | Indirect | 4.5 |
| Volpi 198738 | United States | Cohort | 16 | 53 | nr | Direct | 20.3 |
| Whited 198339 | United States | Cohort | 200 | nr | nr | Direct, Indirect | nr |
Abbreviations: ETT, endotracheal tube; nr, not reported
Reflects the number of patients meeting inclusion/exclusion criteria, and therefore analyzed and reported in this systematic review.
Duration in median days.
Clinical Presentation
Eight studies had laryngeal injury after oral intubation as the primary objective,34–37,40 whereas one study had frequency of dysphagia post-extubation as its primary objective.41 Patients’ mean (SD; 95% confidence interval [95%CI]) age was 53.4 (7.0; 52.8–54.0) years across the 8 (89%) studies reporting age.33–38,40,41 Diagnoses included cardiac,38,41 medical,33,34,36,38–41 mixed medical-surgical,40 oncological,38,41 surgical,39–41 non-neurological trauma,41 and unclear/unstated diagnoses.35,37,41 Whereas 6 (67%) studies reported endotracheal tube (ETT) size,33–36,40,41 only 1 (11%) study distinguished ETT size between the sexes, with most females receiving a 7.0 mm inner diameter (range: 6.5–7.0 mm) compared with most males receiving an 8.0 mm inner diameter (range: 7.5–8 mm).34 Two (22%) studies reported ETT manufacturer.33,36 Across 7 (78%) studies, the calculated mean (SD; 95%CI) duration of intubation was 8.2 (6.0; 7.7–8.7) days.33,34,36–38,40,41 One (11%) study reported median duration of 4 days, but without any measure of variability35 and one study reported 3 groups with ranges of intubation duration without summary statistics39 (Table 1).
Assessment and Diagnosis
Direct visualization via laryngoscope38,39 was used in 2 (22%) studies. Indirect visualization as a laryngeal mirror,39 rigid endoscope35 flexible nasoendoscopy,34,36,37,39–41 and flexible bronchoscopy was used in 8 (89%) studies (Table 1).33 Otolaryngologist interpretation of findings was confirmed in 7 (78%) studies.34–36,38–41 After extubation, assessment was completed within 6 hours,36–38 within 24 hours,34,35,39,40 within 72 hours,41 and at 2 weeks post-extubation.33
Laryngeal Injury – Signs
The prevalence of post-extubation laryngeal injury across all 4 severity grades is summarized in Table 2. Injuries were inconsistently reported across studies, as seen in the raw data presented in Supplementary Table 1. No laryngeal injury was observed in 17% of patients across the 7 (78%) studies reporting this outcome.33–36,38,40,41
Table 2.
Prevalence of laryngeal injury grade by average intubation duration.
| Average Intubation Duration |
||||
|---|---|---|---|---|
| Injury Grade | All Patients (Na = 775)33–41 nb (%) |
<5 Days (Na = 342)34,35,37,39 nb (%) |
5–10 Days (Na = 367)33,36,39–41 nb (%) |
>10 Days (Na = 66)38,39 nb (%) |
| 0 No injury present | 94/543 (17)33–36,38,40,41 | 52/260 (20)34,35 | 42/267 (16)33,36,40,41 | 0/16 (0)38 |
|
1 Self-limited, soft tissue (e.g., edema, erythema, hyperplasia, ecchymosis) |
835/1135 (74)34–37,40,41 | 265/439 (60)34,35,37 | 570/696 (82)36,40,41 | - |
|
2 Hematoma, ulceration, fibrin without glottic narrowing, mass lesion, granulation |
260/842 (31)33–38,40,41 | 70/292 (24)34,35,37 | 174/534 (33)33,36,40,41 | 16/16 (100)38 |
| 3 Stenosis, stenosis with glottic narrowing, hypomobility/ immobility of the vocal folds and/or arytenoids complex) |
137/1048 (13)33,34,36,37,39–41 | 39/500 (8)34,37,39 | 90/498 (18)33,36,39–41 | 7/50 (14)39 |
N: The total number of subjects across studies.
n: The total number of occurrences observed with each injury and within each injury grade divided by the number of possible occurrences. The number of possible occurrences was calculated as the product number of patients evaluated and the number of types of injuries evaluated for each study. Note that each study may not report all injury types. For example, the prevalence of a Grade 1 injury considers all possible injury types (e.g., edema, erythema, hyperplasia, ecchymosis). In the “All Patients” column, the studies reporting each injury type observed 835 occurrences of Grade 1 injury types across 1135 possibilities that they could have occurred, or 74% prevalence of Grade 1 injury.
A high prevalence of minor injury and lower prevalence of more severe injury occurred. Many injuries were self-limiting, Grade 1 injuries. Overall, erythema was most frequent, with a prevalence of 82% (252/307 patients),35,37,40,41 followed closely by edema with a prevalence of 70% (583/828 patients).34–37,40,41 The interarytenoid space, the area through which the ETT passes and remains present in situ, had a 95% (106/112 patients) - 96% (108/112 patients) prevalence of edema and erythema, respectively.40,41 Ulcerations, with a 31% (174/524 patients) prevalence, were the most frequently reported moderate (i.e., Grade 2) injury.33,34,36–38,40,41 Intubation granulomas/granulation tissue, the only other injury type reported, had a 27% (86/318 patients) prevalence.33,35,36,40,41 Vocal fold immobility was the most frequently reported and most common of the severe (i.e., Grade 3) injuries, with a 21% (105/508 patients) prevalence.33,34,36,37,40,41 There was a 6% (12/200 patients) prevalence of glottic stenosis39 and 13% (15/112 patients) prevalence of subglottic stenosis.40,41 A prevalence of 5% or less for both subglottic mucosa edema33 and arytenoid(s) dislocation were reported.34
Laryngeal injury prevalence may change with longer durations of intubation. We further analyzed injury findings based on 3 average durations of intubation identified by data generated from this review: (1) <5 days,34,35,37 (2) 5–10 days,33,36,40,41 and (3) >10 days38,39 (Table 2; Supplementary Table 2). There was increased prevalence and increased severity of injury observed in patients intubated 5–10 days compared with those intubated <5 days. Specifically, there was a 37% and 38% increased prevalence of injury in Grades 1 and 2, respectively. Grade 3 had a 125% increase in prevalence between the same two periods. Two studies with durations >10 days38,39 reported 3 unique injury types and are unable to be summarized.
Delays in post-extubation assessment may also contribute to variability in laryngeal injury prevalence. We identified 4 windows of assessment across studies: (1) ≤6 hours,36–38 (2) ≤24 hours,34,35,39,40 (3) ≤72 hours,41 and (4) 2 weeks33 (Table 3; Supplementary Table 3). Compared with overall prevalence and considering variability in the reporting of data, timing of assessment resulted in little change in laryngeal injury prevalence within grade. This finding suggests that the injuries observed vary little within 3 days post-extubation. One study completed assessments 2-weeks post-extubation and demonstrated 84% prevalence of injury in patients who were intubated a mean of 6.2 days (range: 2–14 days), similar to each of the earlier time points.33
Table 3.
Prevalence of laryngeal injury grade by timing of assessment post-extubation.
| Timing of Assessment Post-extubaiton |
||||
|---|---|---|---|---|
| Injury Grade | ≤6 Hours (Na = 184)36–38 nb (%) |
≤24 Hours (Na = 521)34,35,39,40 nb (%) |
≤72 Hours (Na = 51)41 nb (%) |
2 Weeks (Na = 19)33 nb (%) |
| 0 No injury present | 36/152 (24)36,38 | 52/321 (16)34,35,40 | 3/51 (6)41 | 3/19 (16)33 |
|
1 Self-limited, soft tissue (e.g., edema, erythema, hyperplasia, ecchymosis) |
167/264 (63)36,37 | 441/616 (72)34,35,40 | 227/255 (89)41 | - |
|
2 Hematoma, ulceration, fibrin without glottic narrowing, mass lesion, granulation |
77/320 (24)36–38 | 122/382 (32)34,35,40 | 46/102 (45)41 | 15/38 (39)33 |
|
3 Stenosis, stenosis with glottic narrowing, hypomobility/ immobility of the vocal folds and/or arytenoids complex) |
30/168 (18)36,37 | 79/740 (11)34,39,40 | 26/102 (25)41 | 2/38 (5)33 |
N: The total number of subjects across studies.
n: The total number of occurrences observed with each injury and within each injury grade divided by the number of possible occurrences. The number of possible occurrences was calculated as the product number of patients evaluated and the number of types of injuries evaluated for each study. Note that each study may not report all injury types. For example, the prevalence of a Grade 1 injury considers all possible injury types (e.g., edema, erythema, hyperplasia, ecchymosis). In the “All Patients” column, the studies reporting each injury type observed 835 occurrences of Grade 1 injury types across 1135 possibilities that they could have occurred, or 74% prevalence of Grade 1 injury.
Laryngeal Injury – Symptoms
Symptoms of laryngeal injury identified after extubation were common (Table 4, Supplementary Tables 1–3), with voice dysfunction (i.e., dysphonia), dysphagia, and pain being the most frequent. Both voice dysfunction (197/260 patients)33,34,37 and pain (184/241 patients)34,37 had a 76% prevalence. Dysphagia had a prevalence of 49% (157/319 patients).33,34,37,41 Laryngeal dyspnea and stridor were least frequent with a prevalence of 23% (48/209 patients)34 and 7% (11/155 patients),33,36 respectively.
Table 4.
Prevalence of symptoms reported post-extubation.
| Symptoms | Patients, na (%) |
|---|---|
| Dysphonia (including hoarseness) | 197/260 (76)33,34,37 |
| Pain | 184/241 (76)34,37 |
| Dysphagia | 157/319 (49)33,34,37,41 |
| Laryngeal dyspnea | 48/209 (23)34 |
| Stridor | 11/155 (7)33,36 |
| Overall | 597/1184 (50)33,34,36,37,41 |
Prevalence is reported as the total number observed divided by the total number of patients analyzed for each sign/symptom across studies.
Methodological quality
Methodological quality is summarized as risk of bias (Supplementary Table 4). All studies provided adequate rationale with clear objectives. Most studies included sufficient subject selection criteria (8/9: 89%) and minimized reporting bias (7/9: 78%). Weaknesses included insufficient information for study replication (3/9: 33%) and appropriate controls for sampling (3/9: 67%), in addition to detection (5/9: 56%), attrition (3/9: 33%), and avoidance (3/9: 33%) biases.
DISCUSSION
This systematic review demonstrates that laryngeal injury is a frequent consequence of intubation and is exacerbated with increased duration, despite considerable variability of study methods, patient populations, and outcomes reporting among the accepted articles. Only a small fraction of patients will emerge from intubation injury-free. Although less severe injuries are more common, Grades 2 and Grade 3 injuries occur with a remarkable frequency of 31% and 13%, respectively. On average, more than twice as many patients will sustain moderate or severe injuries that impact airway, voice, and/or swallowing than will have no injury. Assessments completed within 72 hours of extubation appear to have little effect on outcomes, suggesting that resolution of even less severe injuries extends beyond 3 days.
A necessary first step in managing laryngeal injuries is in determining their presence and severity to facilitate appropriate and individualized management. Management could be coordinated by the ICU team and involve a variety of other disciplines. Treatment might include prescribing glucocorticoids42 and anti-reflux medications,43 procedures such as stenosis dilation44 and vocal fold medialization by anesthesiology and otolaryngology,45,46 therapy by speech-language pathology for voice47,48 and swallowing,49,50 and other complementary therapies for improving patient function and quality of life.51,52
One finding worth highlighting is that approximately half of all patients experienced dysphagia after extubation and that 1 in 5 patients had vocal fold immobility. It is well-recognized that intubation duration more than 2 days places patients at high risk for both acute and chronic dysphagia25,34,41,53,54 that may result in aspiration, possibly leading to aspiration pneumonia or pneumonitis.55–59 There are several potential contributing etiologies that might increase aspiration risk in this population, including compromised cognition,60 sensory impairment,17,61 reduced laryngeal adductor reflex,62,63 and reduced strength in muscles involved in swallowing.64 Emerging evidence is linking morphological laryngeal injury to aspiration,41 with an aspiration prevalence of 38%−44% during oral consumption in patients with unilateral vocal fold immobility.65,66 Moreover, the risk of pneumonia doubles in patients with unilateral vocal fold paralysis.67 Early recognition of vocal fold paralysis may mitigate risks for pneumonia or pneumonitis with a timely vocal fold medialization procedure, for example.45,68 Additionally, comprehensive investigation may identify other findings associated with symptoms such as dysphagia, increasing the chances for earlier risk stratification and appropriate management.
Similar ETT inner diameters (i.e., ETT size) were used across studies, but not all studies reported size and/or manufacturer. This presents 2 issues for attribution of laryngeal injury to ETT size. First, there is no standard for assigning ETT size, but size: (1) reflects inner lumen diameter, (2) has no association with outer diameter measurement, (3) is similar across manufacturers, and (4) may be considered with therapeutic value (e.g., air volume, pressure, oxygenation)69 and instruments use via the ETT (e.g., bronchoscope). The ETT outer diameter: (1) contacts anatomical structures, (2) is associated with occupying space within the larynx/trachea, and (3) is, at least partly, responsible for laryngeal injuries and their symptoms. There is minor (≤0.5 mm) variability in outer diameter between manufacturers (i.e., Mallinckrodt,™ Portex, Smiths Medical, Unoflex), each using similar materials. However, Mallinckrodt™ currently produces 2 ETTs (i.e., TaperGuard™ Evac, SealGuard™ Evac) that have outer diameters approximately 1 mm larger than other ETTs across sizes and manufacturers.70 No conclusions can be made concerning laryngeal injury, ETT size, and/or materials/manufacturing due to the large variability within and between studies. Future studies should report these characteristics to address this concern.
Our findings encourage more routine, timely and consistent use of a laryngeal assessment and dysphagia screening post-extubation, especially in the wake of payment reform and a national focus on patient safety. Hospital-acquired conditions represent a multi-dimensional risk with both cost and exposure dimensions. Aspiration pneumonia and pneumonitis are potentially preventable hospital-acquired conditions that require significant resources, including primary care and specialty physicians,71 with prevalence as high as 14% in post-extubated ICU patient populations.54 Hospital-acquired pneumonia can increase length of stay in the ICU by more than 8 days.72 The exposure and costs (financially and in occupancy) associated with such preventable harm represent a strong market, fiscal, and moral case for prevention, or at least early screening, assessment, and treatment. A screening for laryngeal injury is, perhaps, more complicated. Moderate to severe laryngeal injuries may result in more than 2 days and $6000 in costs with readmission for repair.73 Despite frequent complaints of dysphonia and pain after extubation, identifying which patients are at high risk for moderate to severe laryngeal injury and the best time for assessment is less clear. Moreover, there are no screening tools or published guidelines offering direction on this issue, a large gap in critical care patient populations and their long-term outcomes.74
Regardless of which symptom(s) are present, “wait and see” remains the most common approach to identification and management of these injuries,17–19 despite nearly 40 years of evidence and recommendations for more timely evaluations.15,34,41,75–77 Remarkably, there are no published guidelines for post-extubation assessment of laryngeal injury or dysphagia. The only published guideline concerning post-extubation assessment specifically addresses one symptom—hoarseness.21 It states that the laryngoscopic evaluation of patients with both hoarseness and a history of intubation “may [be completed] at any time” (p. S14), but “clinicians should perform laryngoscopy…[with unresolved hoarseness] within 4 weeks or irrespective of duration if a serious underlying cause is suspected” (p. S15).21 Much is left to interpretation from these recommendations because they are made for hoarseness of any etiology, written for ambulatory outpatients instead of at-risk ICU patients, and are not specific to intubation injury. We emphasize that hoarseness may be only one of many symptoms of laryngeal injury. Among the most prevalent symptoms is pain, which may be indicative of serious laryngeal injury. Dysphagia is also highly prevalent with potential for serious consequences soon after extubation.8,33,34,36,37,41 Future studies and screening guidelines should consider these other symptoms.
A high risk of bias was observed in >50% of the rating parameters. These results appear to reflect difficulties controlling experimenter biases, specifically: 1) detection bias, 2) attrition bias, avoidance bias, and reporting bias. The 2 cross-sectional studies (both from one lab) included in this review represent a low risk of bias across all parameters.40,41 The 7 cohort studies all introduced unknown or high risks of bias.33–39 The introduction of these biases may reflect the dynamic, frequently unpredictable ICU setting combined with data collection across multiple time points. Extra care must be taken to reduce biases through methodological controls with these types of study designs. Clarity in writing for study replication is also concerning. Editorial review, and publication guidelines for clinical studies should strive for improvements in writing clarity and reduction of study biases.
Limitations
There are three potential limitations noted. First, our search was limited to the English language. We acknowledge that studies from other languages may provide results that are contrary to our findings and conclusions, but we believe this to be unlikely with the robust agreement between studies accepted for review. Second, our data were limited to ICU. Intubation is also performed routinely in emergency medicine and surgical settings. Although emergency medicine settings were not specifically excluded, we are not aware of any studies using laryngoscopy for post-extubation evaluation of these patients. Studies about intubation trauma and laryngeal injury in surgical settings offer a different patient population and considerable differences in intubation duration and were not the focus of this review. Third, after study acceptance, we observed a ≥19 year gap between three studies published in/before 198733,38,39 and the next study published in 2006.35 Although clinical practice and improved construction of endotracheal tubes during this period may have impacted intubation technique and laryngeal injury, prevalence of injury between these two time periods were similar. Despite these limitations, this systematic review makes a novel contribution toward ongoing research in the area of post-extubation laryngeal injury, and is a call to action for increased awareness of this phenomenon.
CONCLUSIONS
Considering the prevalence of laryngeal injury, dysphonia, and dysphagia and their associated risks for more serious medical complications, practice guidelines are needed for post-extubation screening/assessment in the ICU. Evidence strongly indicates that intubation duration is associated with prevalence and severity of laryngeal injuries. Injuries are frequent and range widely in severity post-extubation. Although mild injuries are more prevalent, moderate to severe injuries occur frequently and require timely clinical attention. Presently, no clinical standards of practice address these potentially serious injuries and there is little evidence in this review to offer direction. Findings suggest new areas for scientific inquiry and highlight long-known and under-identified iatrogenic injury from one of the most common procedures in medicine—endotracheal intubation.
Supplementary Material
ACKNOWLEDGEMENTS
This research was supported by the National Institutes of Health/National Institute on Deafness and Other Communication Disorders (5K23DC013569, Brodsky).
Dr. Brodsky’s institution received funding from National Institutes of Health (NIH)/National Institute on Deafness and Other Communication Disorders, and he received funding from MedBridge. Drs. Brodsky, Pandian, and Hillel received support for article research from the NIH. Dr. Pandian’s institution received funding from Smiths Medical and other consulting work. Dr. Hillel received funding from Olympus USA. Dr. Akst received funding from KayPentax and Olympus, both of which are not related to this work.
Abbreviations:
- LMA
laryngeal mask airway
- RLN
recurrent laryngeal nerve
Footnotes
Copyright form disclosure: The remaining authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Adhikari NKJ, Fowler RA, Bhagwanjee S, Rubenfeld GD. Critical care and the global burden of critical illness in adults. Lancet. 2010;376(9749):1339–1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bishop MJ, Weymuller EA, Fink BR. Laryngeal effects of prolonged intubation. Anesth Analg. 1984;63:335–342. [PubMed] [Google Scholar]
- 3.Santos PM, Afrassiabi A, Weymuller EA Jr. Prospective studies evaluating the standard endotracheal tube and a prototype endotracheal tube. Ann Otol Rhinol Laryngol. 1989;98(12 Pt 1): 935–940. [DOI] [PubMed] [Google Scholar]
- 4.Benjamin B, Holinger LD. Laryngeal complications of endotracheal intubation. Ann Otol Rhinol Laryngol. 2008;117(9 (Suppl 200)):1–20.18254362 [Google Scholar]
- 5.Alexopoulos C, Lindholm CE. Airway complaints and laryngeal pathology after intubation with an anatomically shaped endotracheal tube. Acta Anaesthesiol Scand. 1983;27(4):339–344. [DOI] [PubMed] [Google Scholar]
- 6.Nordang L, Lindholm CE, Larsson J, Linder A. Early laryngeal outcome of prolonged intubation using an anatomical tube: A double blind, randomised study. Eur Arch Otorhinolaryngol. 2016;273(3):703–708. [DOI] [PubMed] [Google Scholar]
- 7.Geraci G, Cupido F, Lo Nigro C, Sciuto A, Sciume C, Modica G. Postoperative laryngeal symptoms in a general surgery setting. Clinical study. Annali italiani di chirurgia. 2013;84(4):377–383. [PubMed] [Google Scholar]
- 8.Donnelly WH. Histopathology of endotracheal intubation. An autopsy study of 99 cases. Arch Pathol. 1969;88(5):511–520. [PubMed] [Google Scholar]
- 9.Dubick MN, Wright BD. Comparison of laryngeal pathology following long-term oral and nasal endotracheal intubations. Anesth Analg. 1978;57(6):663–668. [PubMed] [Google Scholar]
- 10.Brandwein M, Abramson AL, Shikowitz MJ. Bilateral vocal cord paralysis following endotracheal intubation. Archives of Otolaryngology - Head and Neck Surgery. 1986;112(8):877–882. [DOI] [PubMed] [Google Scholar]
- 11.Colice GL, Stukel TA, Dain B. Laryngeal complications of prolonged intubation. Chest. 1989;96(4):877–884. [DOI] [PubMed] [Google Scholar]
- 12.Santos PM, Afrassiabi A, Weymuller EA Jr. Risk factors associated with prolonged intubation and laryngeal injury. Otolaryngol Head Neck Surg. 1994;111(4):453–459. [DOI] [PubMed] [Google Scholar]
- 13.Massard G, Rouge C, Dabbagh A, et al. Tracheobronchial lacerations after intubation and tracheostomy. Ann Thorac Surg. 1996;61(5):1483–1487. [DOI] [PubMed] [Google Scholar]
- 14.Eckerbom B, Lindholm CE, Alexopoulos C. Airway lesions caused by prolonged intubation with standard and with anatomically shaped tracheal tubes. A post-mortem study. Acta Anaesthesiol Scand. 1986;30(5):366–373. [DOI] [PubMed] [Google Scholar]
- 15.Brodsky MB, González-Fernández M, Mendez-Tellez PA, Shanholtz C, Palmer JB, Needham DM. Factors associated with swallowing assessment after oral endotracheal intubation and mechanical ventilation for acute lung injury. Ann Am Thorac Soc. 2014;11(10):1545–1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Benjamin B Prolonged intubation injuries of the larynx: endoscopic diagnosis, classification, and treatment. Ann Otol Rhinol Laryngol Suppl. 1993;160:1–15. [DOI] [PubMed] [Google Scholar]
- 17.Benjamin B, Holinger LD. Laryngeal complications of endotracheal intubation. Ann Oto Rhinol Laryn. 2008;117(9):2–20. [Google Scholar]
- 18.Sadoughi B, Fried MP, Sulica L, Blitzer A. Hoarseness evaluation: a transatlantic survey of laryngeal experts. Laryngoscope. 2014;124(1):221–226. [DOI] [PubMed] [Google Scholar]
- 19.Colice GL. Resolution of laryngeal injury following translaryngeal intubation. Am Rev Respir Dis. 1992;145(2 Pt 1):361–364. [DOI] [PubMed] [Google Scholar]
- 20.Schwartz SR, Cohen SM, Dailey SH, et al. Clinical practice guideline: Hoarseness (dysphonia). Otolaryngol Head Neck Surg. 2009;141(3 Suppl 2):S1–s31. [DOI] [PubMed] [Google Scholar]
- 21.Stachler RJ, Francis DO, Schwartz SR, et al. Clinical practice guideline: Hoarseness (Dysphonia) (Update). Otolaryngol Head Neck Surg. 2018;158(1_suppl):S1–S42. [DOI] [PubMed] [Google Scholar]
- 22.Whited RE. A prospective study of laryngotracheal sequelae in long-term intubation. Laryngoscope. 1984;94(3):367–377. [DOI] [PubMed] [Google Scholar]
- 23.Wain JC. Postintubation tracheal stenosis. Chest Surg Clin N Am. 2003;13(2):231–246. [DOI] [PubMed] [Google Scholar]
- 24.Havas TE, Priestley J, Lowinger DS. A management strategy for vocal process granulomas. Laryngoscope. 1999;109(2 Pt 1):301–306. [DOI] [PubMed] [Google Scholar]
- 25.Brodsky MB, Huang M, Shanholtz C, et al. Recovery from dysphagia symptoms after oral endotracheal intubation in acute respiratory distress syndrome survivors. A 5-year longitudinal study. Ann Am Thorac Soc. 2017;14(3):376–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions: Version 5.1.0 (updated March 2011). Cochrane Collaboration; 2011. [Google Scholar]
- 27.Alberani V, De Castro Pietrangeli P, Mazza AM. The use of grey literature in health sciences: A preliminary survey. Bull Med Libr Assoc. 1990;78(4):358–363. [PMC free article] [PubMed] [Google Scholar]
- 28.Higgins JPT, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1(2):97–111. [DOI] [PubMed] [Google Scholar]
- 30.Moller AM, Myles PS. What makes a good systematic review and meta-analysis? Br J Anaesth. 2016;117(4):428–430. [DOI] [PubMed] [Google Scholar]
- 31.Lindholm C-E. Prolonged Endotracheal Intubation: A clinical investigation with special reference to its consequences for the larynx and trachea and to its place an alternative to intubation through a tracheostomy. Acta Anaesthesiol Scand. 1969;13(s33):1–80.5363891 [Google Scholar]
- 32.Thomas R, Kumar EV, Kameswaran M, et al. Post intubation laryngeal sequelae in an intensive care unit. J Laryngol Otol. 1995;109(4):313–316. [DOI] [PubMed] [Google Scholar]
- 33.Kastanos NM, Miro REM, Perez AMM, Mir AXM, Agusti-Vidal AM. Laryngotracheal injury due to endotracheal intubation: Incidence, evolution, and predisposing factors. A prospective long-term study. Crit Care Med. 1983;11(5):362–367. [DOI] [PubMed] [Google Scholar]
- 34.Megarbane B, Be Hong T, Kania R, Herman P, Baud FJ. Early laryngeal injury and complications because of endotracheal intubation in acutely poisoned patients: a prospective observational study. Clin Toxicol (Phila). 2010;48(4):331–336. [DOI] [PubMed] [Google Scholar]
- 35.Rangachari V, Sundararajan I, Sumathi V, Kumar K. Laryngeal sequelae following prolonged intubation: A prospective study. Indian J Crit Care Med. 2006;10(3):171–175. [Google Scholar]
- 36.Tadié JM, Behm E, Lecuyer L, et al. Post-intubation laryngeal injuries and extubation failure: A fiberoptic endoscopic study. Intensive Care Med. 2010;36(6):991–998. [DOI] [PubMed] [Google Scholar]
- 37.Van der Meer G, Ferreira Y, Loock JW. The S/Z ratio: A simple and reliable clinical method of evaluating laryngeal function in patients after intubation. J Crit Care. 2010;25(3):489–492. [DOI] [PubMed] [Google Scholar]
- 38.Volpi D, Lin PT, Kuriloff DB, Kimmelman CP. Risk factors for intubation injury of the larynx. Ann Otol Rhinol Laryngol. 1987;96(6):684–686. [DOI] [PubMed] [Google Scholar]
- 39.Whited RE. Posterior commissure stenosis post long-term intubation. Laryngoscope. 1983;93(10):1314–1318. [DOI] [PubMed] [Google Scholar]
- 40.Colton House J, Noordzij JP, Murgia B, Langmore S. Laryngeal injury from prolonged intubation: A prospective analysis of contributing factors. Laryngoscope. 2011;121(3):596–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Scheel R, Pisegna JM, McNally E, Noordzij JP, Langmore SE. Endoscopic assessment of swallowing after prolonged intubation in the ICU setting. Ann Otol Rhinol Laryngol. 2016;125(1):43–52. [DOI] [PubMed] [Google Scholar]
- 42.Rafii B, Sridharan S, Taliercio S, et al. Glucocorticoids in laryngology: A review. Laryngoscope. 2014;124(7):1668–1673. [DOI] [PubMed] [Google Scholar]
- 43.Hanson DG, Kamel PL, Kahrilas PJ. Outcomes of antireflux therapy for the treatment of chronic laryngitis. Ann Otol Rhinol Laryngol. 1995;104(7):550–555. [DOI] [PubMed] [Google Scholar]
- 44.Hillel AT, Karatayli-Ozgursoy S, Benke JR, et al. Voice quality in laryngotracheal stenosis: impact of dilation and level of stenosis. Ann Otol Rhinol Laryngol. 2015;124(5):413–418. [DOI] [PubMed] [Google Scholar]
- 45.Bhattacharyya N, Kotz T, Shapiro J. Dysphagia and aspiration with unilateral vocal cord immobility: Incidence, characterization, and response to surgical treatment. Ann Otol Rhinol Laryngol. 2002;111(8):672–679. [DOI] [PubMed] [Google Scholar]
- 46.Rosero EB, Ozayar E, Mau T, Joshi GP. A sequential anesthesia technique for surgical repair of unilateral vocal fold paralysis. J Anesth. 2016;30(6):1078–1081. [DOI] [PubMed] [Google Scholar]
- 47.American Speech-Language-Hearing Association. The use of voice therapy in the treatment of dysphonia [Technical Report]. Available from wwwashaorg/policy. 2005.
- 48.Angadi V, Croake D, Stemple J. Effects of vocal function exercises: A systematic review. J Voice. 2017. [DOI] [PubMed] [Google Scholar]
- 49.Langmore SE. History of fiberoptic endoscopic evaluation of swallowing for evaluation and management of pharyngeal dysphagia: Changes over the years. Dysphagia. 2017;32(1):27–38. [DOI] [PubMed] [Google Scholar]
- 50.Macht M, White SD, Moss M. Swallowing dysfunction after critical illness. Chest. 2014;146(6):1681–1689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cardoso R, Meneses RF, Lumini-Oliveira J. The effectiveness of physiotherapy and complementary therapies on voice disorders: A systematic review of randomized controlled trials. Frontiers in medicine. 2017;4:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rohof WO, Myers JC, Estremera FA, et al. Inter- and intra-rater reproducibility of automated and integrated pressure-flow analysis of esophageal pressure-impedance recordings. Neurogastroenterol Motil. 2014;26(2):168–175. [DOI] [PubMed] [Google Scholar]
- 53.Brodsky MB, Gellar JE, Dinglas VD, et al. Duration of oral endotracheal intubation is associated with dysphagia symptoms in acute lung injury patients. J Crit Care. 2014;29(4):574–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Macht M, Wimbish T, Clark BJ, et al. Postextubation dysphagia is persistent and associated with poor outcomes in survivors of critical illness. Crit Care. 2011;15(5):R231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kozlow JH, Berenholtz SM, Garrett E, Dorman T, Pronovost PJ. Epidemiology and impact of aspiration pneumonia in patients undergoing surgery in Maryland, 1999–2000. Crit Care Med. 2003;31(7):1930–1937. [DOI] [PubMed] [Google Scholar]
- 56.Marik PE. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med. 2001;344(9):665–671. [DOI] [PubMed] [Google Scholar]
- 57.Skoretz SA, Flowers HL, Martino R. The incidence of dysphagia following endotracheal intubation: A systematic review. Chest. 2010;137(3):665–673. [DOI] [PubMed] [Google Scholar]
- 58.Schmidt J, Holas M, Halvorson K, Reding M. Videofluoroscopic evidence of aspiration predicts pneumonia and death but not dehydration following stroke. Dysphagia. 1994;9(1):7–11. [DOI] [PubMed] [Google Scholar]
- 59.Macht M, Wimbish T, Bodine C, Moss M. ICU-acquired swallowing disorders. Crit Care Med. 2013;41(10):2396–2405. [DOI] [PubMed] [Google Scholar]
- 60.Leder S, Suiter D, Lisitano Warner H. Answering orientation questions and following single-step verbal commands: Effect on aspiration status. Dysphagia. 2009;24(3):290–295. [DOI] [PubMed] [Google Scholar]
- 61.Aucott W, Prinsley P, Madden G. Laryngeal anaesthesia with aspiration following intubation. Anaesthesia. 1989;44(3):230–231. [DOI] [PubMed] [Google Scholar]
- 62.Kaneoka A, Pisegna JM, Inokuchi H, et al. Relationship between laryngeal sensory deficits, aspiration, and pneumonia in patients with dysphagia. Dysphagia. 2018;33(2):192–199. [DOI] [PubMed] [Google Scholar]
- 63.Kaneoka A, Pisegna JM, Krisciunas GP, et al. Variability of the pressure measurements exerted by the tip of laryngoscope during laryngeal sensory testing: A clinical demonstration. Am J Speech Lang Pathol. 2017;26(3):729–736. [DOI] [PubMed] [Google Scholar]
- 64.Brodsky MB, De I, Chilukuri K, Huang M, Palmer JB, Needham DM. Coordination of pharyngeal and laryngeal swallowing events during single liquid swallows after oral endotracheal intubation for patients with acute respiratory distress syndrome. Dysphagia. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Leder SB, Ross DA. Incidence of vocal fold immobility in patients with dysphagia. Dysphagia. 2005;20(2):163–167; discussion 168–169. [DOI] [PubMed] [Google Scholar]
- 66.Domer AS, Leonard R, Belafsky PC. Pharyngeal weakness and upper esophageal sphincter opening in patients with unilateral vocal fold immobility. Laryngoscope. 2014;124(10):2371–2374. [DOI] [PubMed] [Google Scholar]
- 67.Tsai MS, Yang YH, Liu CY, et al. Unilateral vocal fold paralysis and risk of pneumonia: A nationwide population-based cohort study. Otolaryngol Head Neck Surg. 2018;158(5):896–903. [DOI] [PubMed] [Google Scholar]
- 68.Cates DJ, Venkatesan NN, Strong B, Kuhn MA, Belafsky PC. Effect of vocal fold medialization on dysphagia in patients with unilateral vocal fold immobility. Otolaryngol Head Neck Surg. 2016;155(3):454–457. [DOI] [PubMed] [Google Scholar]
- 69.Stenqvist O, Sonander H, Nilsson K. Small endotracheal tubes: Ventilator and intratracheal pressures during controlled ventilation. Br J Anaesth. 1979;51(4):375–381. [DOI] [PubMed] [Google Scholar]
- 70.Covidien. Mallinckrodt™ Tracheal Tubes Airway Product Catalogue. UK: Covidien; 2012. [Google Scholar]
- 71.Centers for Medicare and Medicaid Services. Hospital Inpatient PPS for Acute Care Hospitals and the Long-Term Care Hospital PPS & FY 2015 Rates. Health and Human Services;2014. CMS-1607-F. Retrieved 01/10/2018 from: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalAcqCond/HAC-Regulations-and-Notices-Items/CMS-1607-F.html.
- 72.Zimlichman E, Henderson D, Tamir O, et al. Health care-associated infections: a meta-analysis of costs and financial impact on the US health care system. JAMA internal medicine. 2013;173(22):2039–2046. [DOI] [PubMed] [Google Scholar]
- 73.Bhatti NI, Mohyuddin A, Reaven N, et al. Cost analysis of intubation-related tracheal injury using a national database. Otolaryngol Head Neck Surg. 2010;143(1):31–36. [DOI] [PubMed] [Google Scholar]
- 74.Needham DM, Davidson J, Cohen H, et al. Improving long-term outcomes after discharge from intensive care unit: Report from a stakeholders’ conference. Crit Care Med. 2012;40(2):502–509. [DOI] [PubMed] [Google Scholar]
- 75.Kambič V, Radšel Z. Intubation lesions of the larynx. Br J Anaesth. 1978;50(6):587–590. [DOI] [PubMed] [Google Scholar]
- 76.Kastanos N, Estopa Miro R, Marin Perez A, Xaubet Mir A, Agusti-Vidal A. Laryngotracheal injury due to endotracheal intubation: incidence, evolution, and predisposing factors. A prospective long-term study. Crit Care Med. 1983;11(5):362–367. [DOI] [PubMed] [Google Scholar]
- 77.Gallivan GJ, Dawson JA, Robbins LD. Critical care perspective: Videolaryngoscopy after endotracheal intubation: Implications for voice. J Voice. 1989;3(1):76–80. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


