Abstract
Purpose
Posterior root repair of the medial meniscus (MM) can prevent rapid progression of knee osteoarthritis in patients with a MM posterior root tear (MMPRT). The anatomic reattachment of the MM posterior root is considered to be critical in a transtibial pullout repair. However, tibial tunnel creation at the anatomic attachment is technically difficult. We hypothesized that a newly developed point-contact aiming guide [Unicorn Meniscal Root (UMR) guide] can create the tibial tunnel at a better position rather than a previously designed MMPRT guide. The aim of this study was to compare the position of the created tibial tunnel between the two meniscal root repair guides.
Materials and methods
Thirty-eight patients underwent transtibial pullout repairs. Tibial tunnel creation was performed using the UMR guide (19 cases) or MMPRT guide (19 cases). Three-dimensional computed tomography images of the tibial surface were evaluated using the Tsukada’s measurement method postoperatively. The expected anatomic center of the MM posterior root attachment was defined as the center of three tangential lines referring to three anatomic bony landmarks (anterior border of the posterior cruciate ligament, lateral margin of the medial tibial plateau, and retro-eminence ridge). The expected anatomic center and tibial tunnel center were evaluated using the percentage-based posterolateral location on the tibial surface. The distance between the anatomic center and tunnel center was calculated.
Results
The anatomic center of the MM posterior root footprint was located at a position of 79.2% posterior and 39.5% lateral. The mean of the tunnel center in the UMR guide was similar to that in the MMPRT guide (posterior direction, P = 0.096; lateral direction, P = 0.280). The mean distances between the tunnel center and the anatomic center were 4.06 and 3.99 mm in the UMR and MMPRT guide group, respectively (P = 0.455).
Conclusions
The UMR guide, as well as the MMPRT guide, is a useful device to create favorable tibial tunnels at the MM posterior root attachment for pullout repairs in patients with MMPRTs.
Level of evidence
IV
Keywords: Knee, Medial meniscus, Root tear, Pullout repair, Tibial guide
Introduction
A medial meniscus (MM) acts as a secondary stabilizer against the anterior tibial shift and external rotation of the tibia [1, 2]. MM posterior root attachment has an important role in regulating the meniscal movement and hoop tension during knee motion and load-bearing. MM posterior root tears (MMPRTs) involved in complete radial and/or oblique tears adjacent to the root attachment lead to accelerated degradation of the knee joint cartilage by disrupting meniscal functions [3]. MM posterior root repair can reduce an excessive tibiofemoral contact pressure following the MMPRT by anchoring the MM posterior root and horn [4]. Several arthroscopic repair techniques, such as the transtibial pullout repair and suture anchor-dependent repair, show more favorable clinical outcomes compared with conservative treatments in patients with MMPRTs [5, 6].
In arthroscopic MM posterior root repairs, an accurate positioning of the tibial tunnel aperture seems to be critical in restoring meniscal function following transtibial pullout repair [5]. In a biomechanical study, 3-mm displacement of the meniscal attachment induces cartilage deformation by decreasing the meniscal hoop tension in a porcine meniscus root tear model [6]. A non-anatomic repair of the MM posterior root attachment cannot restore the tibiofemoral contact pressure in human cadaveric knees [4]. Therefore, the anatomic placement of the MM posterior root/horn is considered to be necessary for obtaining good clinical outcomes in patients with MMPRT following MM posterior root repair [7]. The attachment of the MM posterior root is located on a triangular area surrounded by the lateral border of the medial tibial plateau, posterior cruciate ligament (PCL), and retro-eminence ridge [8, 9]. Several studies report that the MM posterior root has its attachment at 9.6 mm posterior and 0.7 mm lateral to the apex of the medial tibial eminence [4, 7, 8]. In a three-dimensional (3D) computed tomography (CT) image analysis, an anatomic center of the MM posterior root attachment is located at a position of 78.5% posterior and 39.4% lateral [10] using Tsukada’s method [11]. However, tibial tunnel creation at the anatomic center of the MM posterior root attachment is technically difficult because of the narrow medial joint space and lack of absolute standard landmarks. A specially designed MMPRT aiming guide for transtibial pullout repair (Smith & Nephew, Andover, MA, USA) has an advantage in creating the tibial tunnel aperture at a more anatomic location compared with a conventional non-anatomically designed multi-use guide (Arthrex, Naples, FL, USA) [10]. The MMPRT guide has a narrow twisting/curving shape adjusted to the medial intercondylar space. However, the MMPRT guide does not have a tip-aiming hook to set a guide wire at an accurate point. In this study, we made a point-contact aiming guide [Unicorn Meniscal Root (UMR) guide, Arthrex] to achieve rigid positioning of the tibial tunnel center for the MM posterior root repair. We hypothesized that a newly developed point-contact UMR guide can create the tibial tunnel at a better position rather than a previously designed MMPRT guide. The aim of this study was to compare the tibial tunnel position between two meniscal root repair guides.
Materials and methods
This study received the approval of our Institutional Review Board, and written informed consent was obtained from all patients. Thirty-eight patients (23 women and 15 men, a mean age of 63.2 years), who underwent transtibial pullout repairs for MMPRT between May 2018 and January 2019, were included (Table 1). All the patients had an episode of a sudden posteromedial painful popping, continuous knee pain, and complete radial/oblique MMPRT (meniscal root tear classification, types 2/4) [7, 12]. Patients who had radiographic knee osteoarthritis involved in Kellgren-Lawrence grade III or more and a previous history of meniscus injury or knee surgery were excluded. All the patients were diagnosed as having MMPRTs with magnetic resonance imaging (MRI) examinations and met operative indications for arthroscopic transtibial pullout repair (a femorotibial angle < 180°, Outerbridge grade I or II, and Kellgren-Lawrence grades 0–II) [13–18]. Duration from painful popping event to surgery was 84.4 ± 68.2 days. The presence of the MMPRT was defined according to characteristic MRI findings such as cleft, giraffe neck, ghost, radial tear, and meniscal extrusion signs of the MM posterior root within 9 mm from the attachment [19–21]. We divided the patients into two groups to compare the tibial tunnel position between the UMR guide (Arthrex) and the MMPRT guide (Smith & Nephew). We allocated 19 patients to each group according to the time period. In a power analysis (α error = 0.05, 1 − β error = 0.80), the required sample size was 16 patients in each group (difference, 2 mm; standard deviation, 2 mm). The types of the MMPRT were determined by careful arthroscopic examinations according to the meniscal root tear classification [22].
Table 1.
Demographics and clinical characteristics
| UMR guide | MMPRT guide | P value | |
|---|---|---|---|
| Number of patients | 19 | 19 | |
| Gender, men/women | 7/12 | 8/11 | |
| Root tear classification | |||
| Types 1/2/3/4/5 | 0/16/0/3/0 | 0/17/0/2/0 | |
| Kellgren-Lawrence grade | |||
| Grades 0/I/II/III/IV | 0/4/15/0/0 | 0/7/12/0/0 | |
| Age, years | 61.8 ± 8.7 | 64.5 ± 9.1 | 0.184 |
| Height, m | 1.58 ± 0.10 | 1.61 ± 0.11 | 0.225 |
| Body weight, kg | 67.7 ± 17.4 | 68.8 ± 17.7 | 0.420 |
| Body mass index, kg/m2 | 26.6 ± 4.2 | 26.1 ± 3.7 | 0.355 |
| Femorotibial angle, ° | 177.6 ± 1.5 | 177.0 ± 1.1 | 0.083 |
| Duration from injury to surgery, days | 79.0 ± 70.4 | 90.1 ± 67.6 | 0.323 |
Data of age, height, body weight, body mass index, and femorotibial angle are displayed as a mean ± standard deviation. UMR Unicorn Meniscal Root, MMPRT medial meniscus posterior root tear
Surgical procedure
Standard anteromedial and anterolateral portals were used for the MM posterior root repairs. An outside-in pie-crusting technique involving a release of the deep medial collateral ligament was usually performed by using a standard 18-gauge needle [18]. The torn end of the MM posterior root/horn was grasped and repaired using the two-simple-stitches configuration [18, 23]. A knee ScorpionTM suture passer (Arthrex) was used to pass No. 2 FiberWire (or FiberStick, Arthrex) sutures vertically through the MM posterior horn. Two FiberWire sutures were retrieved through the anteromedial portal. Tibial tunnel creation was performed using the UMR guide or the MMPRT guide [10]. The UMR guide was a newly developed aiming device that had a narrow/slim curving shape adjusted to the medial intercondylar space and included a push-button locking system for both sides of the knee (Fig. 1a-f). The aiming guides were placed at the MM posterior root attachment from the anteromedial portal with reference to the medial tibial eminence and PCL. A 2.4-mm guide wire was inserted, using the aiming device, at a 50° angle to the articular surface, and a 4.0-mm cannulated reamer was used to create a tibial tunnel. Two sutures were pulled out through the tibial tunnel. Tibial fixation was performed with the knee flexed at 20° and with an initial tension of 30 N using a 5.0 × 20-mm interference screw: ThreadTight (Arthrex) or Biosure RG (Smith & Nephew). The combination of the 4.0-mm tibial tunnel and 5.0-mm interference screw would not break the No. 2 FiberWire in patients with MMPRTs. The bone quality of the proximal tibia would be poor in the middle-aged patients who have MMPRTs. Thus, we used an interference screw instead of a Double Spike Plate (Meira, Aichi, Japan) for tibial fixation. An additional anchor screw (5.0 × 25-mm GTS cancellous screw, Meira) was inserted below the tibial tunnel aperture for stabilizing the sutures safely. All the surgical procedures were performed by a single experienced surgeon.
Fig. 1.
Aiming guides for medial meniscus (MM) posterior root repair. a A conventional meniscal root marking hook (upper, Arthrex). The Unicorn Meniscal Root (UMR) guide (lower). An inlet denotes the difference between each guide in shape, sizing scale, and aiming system. A guide-wire catching point (red arrows) is set at the tip of the UMR guide. The catching point of the conventional guide is set at the neck of the hook. The length of a curving part between a border (dashed lines) and catching point is longer in the UMR guide than in the conventional guide. The UMR guide has a more anatomic design to aim the native MM posterior root attachment compared with the conventional guide. b A push-button locking system for both sides of the knee. c A point-contact aiming system of the UMR guide. d The UMR guide has a narrow/slim curving shape based on an anatomic design. e The UMR and meniscus posterior root tear (MMPRT) guides. f The difference in a guide-wire catching system between the two guides
3D CT-based measurements
All patients underwent CT examination at 1 week postoperatively. CT images were obtained with an Asteion 4 Multislice CT System (Toshiba Medical Systems, Tochigi, Japan) using 120 kVp and 150 mA, and 1-mm slice thickness. CT reconstruction of the tibial condyles in the axial plane [24] was completed using a 3D volume-rendering technique (AZE Virtual Place software, Tokyo, Japan). 3D CT images of the tibial surface were evaluated using a rectangular measurement grid as described [11]. The image was rotated to visualize the superior aspect of the proximal tibia, with the internal/external rotation adjusted until the most posterior articular margins of both the medial and lateral tibial plateaus were placed on the horizontal level (Fig. 2). The location of interested points on the tibial surface was assessed using a percentage-dependent method. The posterolateral location on the tibial surface was expressed as a percentage using Tsukada’s method [11]. The expected anatomic center of the MM posterior root attachment was defined as a center of three tangential lines referring to three anatomic bony landmarks (anterior border of the PCL tibial attachment, lateral margin of the medial tibial plateau, and retro-eminence ridge) of the triangular footprint of the MM posterior root (Fig. 2). On 3D CT images, a virtual perfect circle that contacted these three tangential lines with the minimum radius was used to determine an expected anatomic center. The tangential line referring to each bony landmark was set at the nearest point to each expected anatomic center. Tibial tunnel centers were determined as the central point of the circular or oval tunnel aperture. The distance between the tunnel center and anatomic center was measured on 3D CT images (Table 2).
Fig. 2.

Distance between tibial tunnel center and expected anatomic center. The location on the three-dimensional computed tomography (3D CT)-based tibial surface was expressed as a posterolateral percentage using Tsukada’s method [11]. The anatomic center of the medial meniscus (MM) posterior root attachment was defined by the center of a circle (red dotted circle) that contacted three margins [anterior border of the posterior cruciate ligament (PCL) tibial attachment, lateral margin of the medial tibial plateau, and retro-eminence ridge]. Red dot, expected anatomic center of the MM posterior root attachment (in this example: 77.8% posterior and 38.5% lateral). Blue dot, tibial tunnel center (79.3% posterior and 37.1% lateral). The distance between the tibial tunnel center and anatomic center was 1.58 mm in this patient who underwent MM posterior root repair using the Unicorn Meniscal Root (UMR) guide
Table 2.
Location of tibial tunnel center
| UMR guide | MMPRT guide | P value | |
|---|---|---|---|
| Tibial tunnel center | |||
| Posterior, % | 74.5 ± 5.4 | 72.4 ± 4.0 | 0.096 |
| Lateral, % | 37.6 ± 2.9 | 38.1 ± 2.6 | 0.280 |
| Distance between tunnel center and anatomic position, mm | 4.06 ± 1.61 | 3.99 ± 1.99 | 0.455 |
Data are displayed as a mean ± standard deviation. UMR Unicorn Meniscal Root, MMPRT medial meniscus posterior root tear
Statistical analysis
Data were presented as means ± standard deviations. Differences between groups were compared using the Mann-Whitney U test. Significance was set at P < 0.05. Two orthopaedic surgeons independently measured the location of expected anatomic center and tibial tunnel center. Each observer performed each measurement twice, at least 2 weeks apart. The inter-observer and intra-observer reliabilities were assessed with the intra-class correlation coefficient (ICC). An ICC > 0.80 was considered to represent a reliable measurement.
Results
No significant differences between the UMR and MMPRT guide groups were observed in preoperative age, height, body weight, body mass index, and femorotibial angle (Table 1). The mean anatomic center of the MM posterior root attachment was located at a position of 79.2% posterior and 39.5% lateral (Fig. 3). The MM posterior root anatomic center was similar in each group (UMR guide, 79.8% posterior and 39.6% lateral position; MMPRT guide, 78.6% posterior and 39.4% lateral position). The values of the inter-observer and intra-observer reliabilities were considered high, with mean ICC values of > 0.91 and > 0.93, respectively.
Fig. 3.
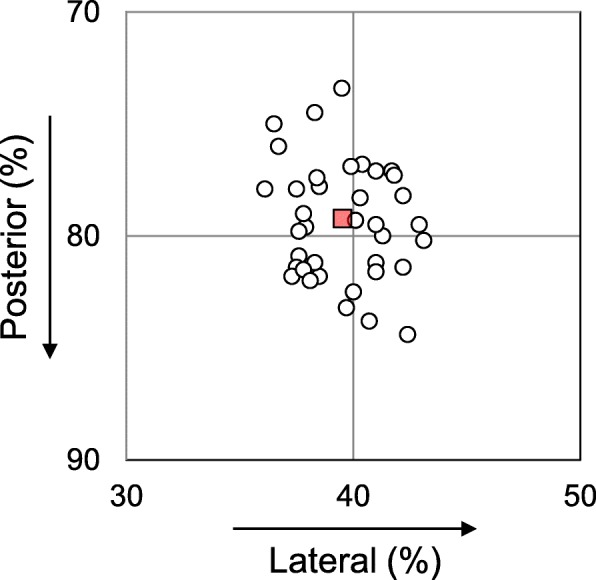
Location of expected anatomic center of the medial meniscus (MM) posterior root attachment (open dots). The mean of the MM posterior root anatomic center was at a position of 78.8% posterior and 39.4% lateral (red square) on a three-dimensional computed tomography (3D CT) image of the tibial surface
The tibial tunnel center of the UMR guide group was located at a position of 74.5% ± 5.4% posterior and 37.6% ± 2.9% lateral (Table 2 and Fig. 4). In the MMPRT guide group, the tibial tunnel center was located at a position of 72.4% ± 4.0% posterior and 38.1% ± 2.6% lateral. Post-hoc power values between the two guide groups were 27.5% and 8.1% in the posterior and lateral directions of tunnel center positions, respectively. The distance between the tunnel center and anatomic center was 4.06 ± 1.61 mm and 3.99 ± 1.99 mm in the UMR and MMPRT guide groups, respectively (a post-hoc power, 3.3%; Table 2). No significant differences in tunnel center position and distance between the
Fig. 4.

Locations of tibial tunnel centers and anatomic center. Red square: the mean anatomic center. Blue triangle: the mean of the tibial tunnel center created by the Unicorn Meniscal Root (UMR) guide (white triangles indicate the location of each case). Orange circle: the mean of the tibial tunnel center in the medial meniscus posterior root tear (MMPRT) guide group (gray dots indicate the location of each case)
two centers were detected between the UMR and MMPRT guide groups (Table 2).
Discussion
This study demonstrated that tibial tunnel centers created using the point-contact UMR guide were similar to those in the MMPRT guide group. Our hypothesis that the UMR guide can create the tibial tunnel at a better position than the MMPRT guide was refuted. The tibial tunnel aperture was located at a favorable position in both groups during arthroscopic MM posterior root repairs. We propose that the newly developed UMR guide system has a high accuracy in creating tibial tunnels at reliable positions during the MM posterior root pullout repairs and does this as well as the MMPRT guide.
In our 3D CT-based measurements, the mean position of the tibial tunnel center in the UMR guide group was similar to that in the MMPRT guide group (Table 2 and Fig. 4). A power analysis did not show a statistical power to achieve the 0.05 level of significance in the tunnel center position towards the posterior direction (a post-hoc power, 27.5%). A more posterior setting of the tibial tunnel may induce a technical difficulty of suture relay. Remaining soft tissues around the posterior root attachment would obstruct an arthroscopic view for suture retrieval. Surgical techniques, such as the outside-in pie-crusting technique or medial collateral ligament release, will be required to obtain the medial joint space widening for accurate tunnel positioning and suture passage during the MM posterior root repair.
MMPRTs lead to abnormal biomechanics of the tibiofemoral joint and the inability to convert axial loads into hoop stresses [25, 26]. Repair of the MMPRT has been shown to reduce the mean tibiofemoral contact pressure by increasing the tibiofemoral contact area in a human cadaveric knee study [27]. Several authors have reported that an anatomic repair of the MM posterior root may be critical for restoring the biomechanical function of the MM [4, 6, 7]. However, there has been no clinical evaluation involved in the relationship between tibial tunnel location and postoperative outcomes following the MM posterior root repair. In addition, patients have their own tibial plateau sizes and their specific MM posterior root attachment. In our study, the distance between the tibial tunnel center and expected anatomic center of the MM posterior root attachment was approximately 4 mm in transtibial pullout repairs using the specially designed UMR and MMPRT guides (Table 2). Previous studies demonstrate that an average attachment area of the MM posterior root is 30.4–47.3 mm2 and the MM posterior root attachment forms an oval or triangular shape [8, 28–30]. We consider that the distance of 4-mm between tunnel center and anatomic center would be acceptable because the radius of the provisional circle to determine the expected anatomic center was 4–5 mm on 3D CT images (Fig. 2).
The MMPRT guide has several advantages in creating a favorable tibial tunnel during pullout repairs in patients with MMPRTs [10]. The narrow and anatomically curving shape of the MMPRT guide can help us to set a guide wire at a more accurate position with high reproducibility compared with previously designed meniscal root guides. The UMR guide has a more anatomic design and longer curving arm to insert the guide into a narrow joint space if the patient has a long anteroposterior distance between the anteromedial portal and the MM posterior root attachment (Fig. 1d-f). In addition, the UMR guide can enable us to set a guide wire more posteriorly because of its point-contact aiming system. On the other hand, the MMPRT guide has a wider safety margin to protect guide wire penetration at the tip of the guide (Fig. 1f). Although the MMPRT guide is separately provided for the left and right knees, the surgeon-friendly UMR guide has an all-in-one and free-aiming system for the medial joint space of both knees. We believe that the UMR guide may have some superiority to the MMPRT guide in tibial bone tunnel creation during the MM posterior toot repair.
There are several limitations to this study. First, the sample size was small. A further study with a larger sample size will be required. Second, the relationship between the tibial tunnel position and postoperative clinical outcome was not evaluated. Third, there was a possibility that an ideal point of the tibial tunnel might be different from the expected anatomic center on 3D CT images. In addition, the CT-image-dependent anatomic center is not validated as a real anatomic center of the MM posterior root attachment. A biomechanical study using cadaveric knees will be required to determine the optimum position of the tibial tunnel in MM posterior root repair. However, the MM condition in patients with symptomatic MMPRTs may be different from that in cadaveric knees. Fourth, the aiming guide setting and tibial tunnel creation were performed by a single experienced orthopaedic surgeon (TF). The usability of these two guides was not scientifically verified by the other surgeons. Finally, there was no significant difference in the accuracy of tibial tunnel creation between these two guides.
Conclusions
The newly developed point-contact UMR guide can enable us to create tibial tunnels for MM posterior root repairs at a favorable position as well as the MMPRT guide can. We conclude that the newly developed UMR guide system has a high accuracy in creating tibial tunnels at reliable positions during MM posterior root repairs.
Acknowledgements
We thank Drs. Shinichi Miyazawa, Takaaki Tanaka, Masataka Fujii, and Tomohito Hino for their clinical support. We also appreciate Drs. Ken Nakata, Nobuo Adachi, and Hideyuki Koga for their great contribution to developing the UMR guide system.
Informed consent
Informed consent was obtained from all patients being included in this study.
Abbreviations
- 3D
Three-dimensional
- CT
Computed tomography
- ICC
Intra-class correlation coefficient
- MM
Medial meniscus
- MMPRT
Medial meniscus posterior root tear
- PCL
Posterior cruciate ligament
- UMR
Unicorn Meniscal Root
Authors’ contributions
TF designed this study and prepared the manuscript. TF performed the operative treatments. YuO, YuyK, YoO, YusK, SM, TH, and TO performed the measurements. All authors contributed to preparing the tables and figures. All authors read and approved the final manuscript.
Funding
No funding sources were provided for this study.
Availability of data and materials
Data sharing was not applicable to this article as no data sets were generated or analyzed during the current study.
Ethics approval
This study received the approval of our Institutional Review Board (Okayama University, No. 1857).
Consent for publication
Consent for publication was obtained from the patients being included in this study.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Takayuki Furumatsu, Email: matino@md.okayama-u.ac.jp.
Yuki Okazaki, Email: yokazaki.okayama@gmail.com.
Yuya Kodama, Email: ykodama314@gmail.com.
Yoshiki Okazaki, Email: yokazaki218@gmail.com.
Yusuke Kamatsuki, Email: fufu9youfu@yahoo.co.jp.
Shin Masuda, Email: me18066@s.okayama-u.ac.jp.
Takaaki Hiranaka, Email: koumei.01.13@gmail.com.
Toshifumi Ozaki, Email: tozaki@md.okayama-u.ac.jp.
References
- 1.Inoue H, Furumatsu T, Miyazawa S, Fujii M, Kodama Y, Ozaki T. Improvement in the medial meniscus posterior shift following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26:434–441. doi: 10.1007/s00167-017-4729-x. [DOI] [PubMed] [Google Scholar]
- 2.Okazaki Y, Furumatsu T, Kodama Y, Hino T, Kamatsuki Y, Okazaki Y, Masuda S, Miyazawa S, Endo H, Tetsunaga T, Yamada K, Ozaki T. Transtibial pullout repair of medial meniscus posterior root tear restores physiological rotation of the tibia in the knee-flexed position. Orthop Traumatol Surg Res. 2019;105:113–117. doi: 10.1016/j.otsr.2018.10.005. [DOI] [PubMed] [Google Scholar]
- 3.Bhatia S, LaPrade CM, Ellman MB, LaPrade RF. Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med. 2014;42:3016–3030. doi: 10.1177/0363546514524162. [DOI] [PubMed] [Google Scholar]
- 4.Ahn JH, Jeong HJ, Lee YS, Park JH, Lee JW, Park JH, Ko TS. Comparison between conservative treatment and arthroscopic pull-out repair of the medial meniscus root tear and analysis of prognostic factors for the determination of repair indication. Arch Orthop Trauma Surg. 2015;135:1265–1276. doi: 10.1007/s00402-015-2269-8. [DOI] [PubMed] [Google Scholar]
- 5.Bonasia DE, Pellegrino P, D'Amelio A, Cottino U, Rossi R. Meniscal root tear repair: why, when and how? Orthop Rev (Pavia) 2015;7:5792. doi: 10.4081/or.2015.5792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stärke C, Kopf S, Gröbel KH, Becker R. The effect of a nonanatomic repair of the meniscal horn attachment on meniscal tension: a biomechanical study. Arthroscopy. 2010;26:358–365. doi: 10.1016/j.arthro.2009.08.013. [DOI] [PubMed] [Google Scholar]
- 7.Moatshe G, Chahla J, Slette E, Engebretsen L, LaPrade RF. Posterior meniscal root injuries. Acta Orthop. 2016;87:452–458. doi: 10.1080/17453674.2016.1202945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johannsen AM, Civitarese DM, Padalecki JR, Goldsmith MT, Wijdicks CA, LaPrade RF. Qualitative and quantitative anatomic analysis of the posterior root attachments of the medial and lateral menisci. Am J Sports Med. 2012;40:2342–2347. doi: 10.1177/0363546512457642. [DOI] [PubMed] [Google Scholar]
- 9.Fujii M, Furumatsu T, Miyazawa S, Kodama Y, Hino T, Kamatsuki Y, Ozaki T. Bony landmark between the attachment of the medial meniscus posterior root and the posterior cruciate ligament: CT and MR imaging assessment. Skelet Radiol. 2017;46:1041–1045. doi: 10.1007/s00256-017-2625-6. [DOI] [PubMed] [Google Scholar]
- 10.Furumatsu T, Kodama Y, Fujii M, Tanaka T, Hino T, Kamatsuki Y, Yamada K, Miyazawa S, Ozaki T. A new aiming guide can create the tibial tunnel at favorable position in transtibial pullout repair for the medial meniscus posterior root tear. Orthop Traumatol Surg Res. 2017;103:367–371. doi: 10.1016/j.otsr.2017.01.005. [DOI] [PubMed] [Google Scholar]
- 11.Tsukada H, Ishibashi Y, Tsuda E, Fukuda A, Toh S. Anatomical analysis of the anterior cruciate ligament femoral and tibial footprints. J Orthop Sci. 2008;13:122–129. doi: 10.1007/s00776-007-1203-5. [DOI] [PubMed] [Google Scholar]
- 12.Furumatsu T, Okazaki Y, Okazaki Y, Hino T, Kamatsuki Y, Masuda S, Miyazawa S, Nakata E, Hasei J, Kunisada T, Ozaki T. Injury patterns of medial meniscus posterior root tears. Orthop Traumatol Surg Res. 2019;105:107–111. doi: 10.1016/j.otsr.2018.10.001. [DOI] [PubMed] [Google Scholar]
- 13.Furumatsu T, Kodama Y, Kamatsuki Y, Hino T, Okazaki Y, Ozaki T. Meniscal extrusion progresses shortly after the medial meniscus posterior root tear. Knee Surg Relat Res. 2017;29:295–301. doi: 10.5792/ksrr.17.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Furumatsu T, Kamatsuki Y, Fujii M, Kodama Y, Okazaki Y, Masuda S, Ozaki T. Medial meniscus extrusion correlates with disease duration of the sudden symptomatic medial meniscus posterior root tear. Orthop Traumatol Surg Res. 2017;103:1179–1182. doi: 10.1016/j.otsr.2017.07.022. [DOI] [PubMed] [Google Scholar]
- 15.Kodama Y, Furumatsu T, Fujii M, Tanaka T, Miyazawa S, Ozaki T. Pullout repair of a medial meniscus posterior root tear using a FasT-Fix all-inside suture technique. Orthop Traumatol Surg Res. 2016;102:951–954. doi: 10.1016/j.otsr.2016.06.013. [DOI] [PubMed] [Google Scholar]
- 16.Fujii M, Furumatsu T, Kodama Y, Miyazawa S, Hino T, Kamatsuki Y, Yamada K, Ozaki T. A novel suture technique using the FasT-Fix combined with Ultrabraid for pullout repair of the medial meniscus posterior root tear. Eur J Orthop Surg Traumatol. 2017;27:559–562. doi: 10.1007/s00590-017-1930-z. [DOI] [PubMed] [Google Scholar]
- 17.Fujii M, Furumatsu T, Xue H, Miyazawa S, Kodama Y, Hino T, Kamatsuki Y, Ozaki T. Tensile strength of the pullout repair technique for the medial meniscus posterior root tear: a porcine study. Int Orthop. 2017;41:2113–2118. doi: 10.1007/s00264-017-3561-8. [DOI] [PubMed] [Google Scholar]
- 18.Okazaki Y, Furumatsu T, Kodama Y, Kamatsuki Y, Masuda S, Ozaki T. Description of a surgical technique of medial meniscus root repair: a fixation technique with two simple stitches under an expected initial tension. Eur J Orthop Surg Traumatol. 2019;29:705–709. doi: 10.1007/s00590-018-2347-z. [DOI] [PubMed] [Google Scholar]
- 19.Furumatsu T, Fujii M, Kodama Y, Ozaki T. A giraffe neck sign of the medial meniscus: a characteristic finding of the medial meniscus posterior root tear on magnetic resonance imaging. J Orthop Sci. 2017;22:731–736. doi: 10.1016/j.jos.2017.03.013. [DOI] [PubMed] [Google Scholar]
- 20.Masuda S, Furumatsu T, Okazaki Y, Kodama Y, Hino T, Kamatsuki Y, Miyazawa S, Ozaki T. Medial meniscus posterior root tear induces pathological posterior extrusion of the meniscus in the knee-flexed position: an open magnetic resonance imaging analysis. Orthop Traumatol Surg Res. 2018;104:485–489. doi: 10.1016/j.otsr.2018.02.012. [DOI] [PubMed] [Google Scholar]
- 21.Okazaki Y, Furumatsu T, Masuda S, Miyazawa S, Kodama Y, Kamatsuki Y, Hino T, Okazaki Y, Ozaki T. Pullout repair of the medial meniscus posterior root tear reduces proton density-weighted imaging signal intensity of the medial meniscus. Acta Med Okayama. 2018;72:493–498. doi: 10.18926/AMO/56247. [DOI] [PubMed] [Google Scholar]
- 22.LaPrade CM, James EW, Cram TR, Feagin JA, Engebretsen L, LaPrade RF. Meniscal root tears: a classification system based on tear morphology. Am J Sports Med. 2015;43:363–369. doi: 10.1177/0363546514559684. [DOI] [PubMed] [Google Scholar]
- 23.Furumatsu T, Miyazawa S, Fujii M, Tanaka T, Kodama Y, Ozaki T. Arthroscopic scoring system of meniscal healing following medial meniscus posterior root repair. Int Orthop. 2019;43:1239–1245. doi: 10.1007/s00264-018-4071-z. [DOI] [PubMed] [Google Scholar]
- 24.Kodama Y, Furumatsu T, Miyazawa S, Fujii M, Tanaka T, Inoue H, Ozaki T. Location of the tibial tunnel aperture affects extrusion of the lateral meniscus following reconstruction of the anterior cruciate ligament. J Orthop Res. 2017;35:1625–1633. doi: 10.1002/jor.23450. [DOI] [PubMed] [Google Scholar]
- 25.Padalecki JR, Jansson KS, Smith SD, Dornan GJ, Pierce CM, Wijdicks CA, LaPrade RF. Biomechanical consequences of a complete radial tear adjacent to the medial meniscus posterior root attachment site: in situ pull-out repair restores derangement of joint mechanics. Am J Sports Med. 2014;42:699–707. doi: 10.1177/0363546513499314. [DOI] [PubMed] [Google Scholar]
- 26.Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am. 2008;90:1922–1931. doi: 10.2106/JBJS.G.00748. [DOI] [PubMed] [Google Scholar]
- 27.LaPrade CM, Foad A, Smith SD, Turnbull TL, Dornan GJ, Engebretsen L, Wijdicks CA, LaPrade RF. Biomechanical consequences of a nonanatomic posterior medial meniscal root repair. Am J Sports Med. 2015;43:912–920. doi: 10.1177/0363546514566191. [DOI] [PubMed] [Google Scholar]
- 28.Johnson DL, Swenson TM, Livesay GA, Aizawa H, Fu FH, Harner CD. Insertion-site anatomy of the human menisci: gross, arthroscopic, and topographical anatomy as a basis for meniscal transplantation. Arthroscopy. 1995;11:386–394. doi: 10.1016/0749-8063(95)90188-4. [DOI] [PubMed] [Google Scholar]
- 29.Hauch KN, Villegas DF, Haut Donahue TL. Geometry, time-dependent and failure properties of human meniscal attachments. J Biomech. 2010;43:463–468. doi: 10.1016/j.jbiomech.2009.09.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zheng L, Harner CD, Zhang X. The morphometry of soft tissue insertions on the tibial plateau: data acquisition and statistical shape analysis. PLoS One. 2014;9:e96515. doi: 10.1371/journal.pone.0096515. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing was not applicable to this article as no data sets were generated or analyzed during the current study.



