Abstract
Objective:
Multiple cognitive risks from different theoretical paradigms (dysfunctional attitudes, negative inferential style, self-criticism, dependency, brooding) predict depression, but may be transdiagnostic vulnerabilities for multiple psychopathologies. Risk factors can be identified as broadly transdiagnostic and relatively specific to psychopathological outcomes by organizing the common and specific aspects of each respective construct using latent bifactor models, and by examining links between dimensions of risk and psychopathology. This study evaluated: (1) whether a bifactor model of cognitive vulnerabilities, including a general cognitive risk dimension (c factor) and several specific dimensions (Schweizer et al., 2018), replicated in early adolescents (Mage=13.50) and extended to younger (Mage=10.46) and older youth (Mage=16.46), and (2) how the general and specific cognitive risk dimensions related to the general psychopathology (p factor) and internalizing- and externalizing-specific dimensions.
Method:
Community youth (N=571; 55% female) reported on cognitive risks; youth and a caregiver reported on psychopathologies (depression, anxiety, aggression, conduct, attention problems).
Results:
The bifactor model of cognitive risk showed good fit and slight advantages over a correlated factors model. The bifactor model exhibited invariance across development and captured key associations that were identified when each individual cognitive risk was related to the bifactor model of psychopathology. C strongly related to the internalizing-specific dimension (β=.86), and moderately to p (β=.33) and the externalizing-specific dimension (β=.42). Specific cognitive risk dimensions (brooding, negative inferential style, dependency) related to all psychopathology dimensions.
Conclusion:
A general cognitive vulnerability (c factor) transdiagnostically associates with a breadth of psychopathologies and most potently to internalizing-specific among youth.
Keywords: cognitive risk, children and adolescents, p factor, internalizing, externalizing
Comorbidity is common across depression, anxiety syndromes, and behavioral and attention problems (Kessler et al., 2005). Latent dimensional bifactor models of psychopathology (Caspi et al., 2014) have emerged as a promising way to reliably, parsimoniously organize the co-occurrence of psychopathological syndromes into general and specific psychopathology dimensions. The general dimension (also called the p factor) accounts for what co-occurs across all measured psychopathological syndromes. After this common variance is accounted for, the remaining variance among certain syndromes is captured in internalizing-specific and externalizing-specific dimensions, which are both independent of p. This bifactor structure of psychopathology has been supported in adults and youth (see Caspi & Moffitt, 2018; Lahey et al., 2017 for reviews).
An important implication of organizing psychopathological symptoms and syndromes via the bifactor model of psychopathology is that multiple psychopathological syndromes may share common underlying risk factors, which can be used to facilitate the identification of transdiagnostic risks for psychopathology (Nolen-Hoeksema & Watkins, 2011). However, relatively little is known about what risk factors and mechanisms predict the latent dimensions of the bifactor model of psychopathology (i.e., p, internalizing-specific, externalizing-specific). An emerging body of work has begun to identify risks for these dimensions, including temperament/personality, chronic stress, genetic, neurobiological and cognitive functioning (Caspi et al., 2014; Castellanos-Ryan et al., 2016; Hankin et al., 2017; Martel, Pan, Hoffman et al., 2017; Olino, Dougherty, Bufferd, Carlson & Klein, 2014; Olino, Dougherty, Bufferd, Carlson & Klein, 2018; Snyder, Hankin, Sandman et al., 2017; Snyder, Young, & Hankin, 2017b; Waldman, Poore, van Hulle, Rathouz, & Lahey, 2016). For instance, higher temperamental negative affectivity (NA), neuroticism and worse self-control are related to p; higher NA and neuroticism relate to the internalizing-specific dimension; and worse effortful control and higher risk-taking associate with the externalizing-specific dimension.
This work suggests that any given transdiagnostic risk may demonstrate varying degrees of breadth (i.e., connection to single or multiple dimensions of psychopathology) and potency (i.e., magnitude of the relationships with dimensions of psychopathology). As such, risks may exhibit general or specific relations with, and have varying degrees of predictive power for, common (p factor) and/or internalizing-specific and -externalizing dimensions of psychopathology. Identifying the breadth and potency of transdiagnostic risks for different psychopathological dimensions could enhance the precision and parsimony of assessment and interventions for psychopathology. A crucial gap concerns what transdiagnostic risks predict p and/or internalizing-specific and externalizing-specific factors of psychopathology as well as understanding the breadth and potency of these associations.
A conceptual framework has been proposed to help researchers clarify the degree to which vulnerabilities exhibit general or specific links to latent dimensional liabilities for psychopathology (Hankin et al., 2016a). When measured at a manifest level, many putatively distinct risk factors likely also exhibit overlap and could be organized more reliably and parsimoniously using latent dimensional models that parse out overlapping and unique aspects of constructs into common and specific factors, respectively (i.e., bifactor models of risk; Hankin et al., 2016a). In contrast to the traditional approach of examining individual manifest risks in relation to individual psychopathological syndromes, Hankin and colleagues (2016a) propose that more parsimonious and clearer relations between risks and psychopathology are revealed when both risk factors and psychopathological outcomes are organized using latent dimensional bifactor models. Then, by linking these two latent dimensional bifactor models of risk and psychopathology together, researchers can better understand transdiagnostic relations between dimensions of risk and psychopathology. This includes elucidating the degree to which different dimensions of risk demonstrate relatively broad or specific connections to different dimensions of psychopathology (i.e., breadth), as well as their predictive power (i.e., potency) for p and/or specific -internalizing and -externalizing dimensions. To date, however, little research has organized risk factors via latent bifactor structural models.
Cognitive Risks to Psychopathology
Cognitive vulnerabilities to psychopathology are a compelling candidate to empirically examine the conceptual model proposed by Hankin and colleagues (2016a). More specifically, latent bifactor models of cognitive risk and psychopathology can be examined jointly to better understand transdiagnostic relations between cognitive risks and psychopathology dimensions. Cognitive risk models of psychopathology propose that individuals with maladaptive thinking tendencies are at increased risk for psychopathology (see Gibb & Coles, 2005; Hankin et al., 2016b for reviews). Several cognitive risks have traditionally been conceptualized as distinct from one another and have originated from different theoretical paradigms. Key cognitive risk constructs from different paradigms include dysfunctional attitudes from Beck’s cognitive model (Beck, 1976), negative inferential style from Hopelessness Theory (Abramson, Metalsky, & Alloy, 1989), two independent maladaptive cognitive-personality dimensions of self-criticism and dependency from Blatt’s model of personality that are distinct factors measured in one singular personality scale (Blatt & Zuroff, 1992), and rumination from Response Styles Theory (Nolen-Hoeksema & Morrow, 1991). Dysfunctional attitudes reflect overly negative schemas including beliefs about the self, world, and others that reflect rigid, excessive standards of perfectionism, performance, contingent self-worth, and needing others’ approval. Negative inferential style reflects individuals’ explanatory style for the causes of aversive events as being stable (i.e., likely to recur) and global (i.e., likely to affect all aspects of life), generating negative self-inferences (e.g., one is worthless), and believing negative consequences will follow. High self-criticism includes an excessive focus on achievement and status to gain approval from others; high dependency includes instability in relationships and self-worth that depends on meeting others’ needs. Lastly, rumination is a passive, repetitive thinking style where one dwells on the potential meaning, causes, and consequences of one’s symptoms of distress.
Historically, these cognitive vulnerabilities were proposed and studied predominantly as risks for depression, yet more recent work suggests that they may be transdiagnostically related across a breadth of psychopathological outcomes. Manifest measures of these cognitive risks predict depression and anxiety, and a smaller body of work suggests that certain cognitive risks relate to externalizing problems (see Hankin et al., 2016b for review). For instance, dysfunctional attitudes have prospectively predicted anxiety among youth (Lee & Hankin, 2009); negative inferential style has been associated with social anxiety in youth (Alloy et al., 2012), and ADHD in youth and adults (Rucklidge et al., 2007); self-criticism has longitudinally predicted externalizing problems in youth (Leadbeater, Kuperminc, Blatt, & Hertzog, 1999), and social anxiety in adults (Cox, Fleet, & Stein, 2004); and rumination has prospectively predicted anxiety in youth and adults (McLaughlin & Nolen-Hoeksema, 2011), and aggression in youth (McLaughlin, Wisco, Aldao, & Hilt, 2014). Overall, these findings suggest that cognitive vulnerabilities may be transdiagnostically related to general psychopathology (p), along with specific internalizing symptoms and perhaps specific externalizing problems. However, extant studies have not adequately and rigorously addressed the extent to which cognitive vulnerabilities relate to p and/or to specific psychopathology dimensions. Empirical work is needed that directly examines how these cognitive risks relate to latent dimensions of psychopathology.
Not only do these prominent cognitive risks relate similarly to various psychopathological outcomes (especially internalizing problems of depression and anxiety), but also these purportedly separate cognitive vulnerabilities themselves are moderately intercorrelated. Given such patterns, it is possible that a more parsimonious structure may organize these cognitive risks. Prior factor analytic work among youth and adults examining subsets of these cognitive risks has found support for both a single factor (Reno & Halaris, 1989; Garber, Weiss, & Shanley, 1993; Hong & Cheung, 2015) and correlated factors structure (Joiner & Rudd, 1996; Gotlib et al., 1993; Hankin et al., 2007; Adams et al., 2007). These two lines of evidence suggest that these cognitive risks likely share something in common and have unique components.
Bifactor Model of Cognitive Risks to Psychopathology & Links to Internalizing Outcomes
A recent study of early adolescents examined three alternative structural models to organize dysfunctional attitudes, negative inferential style, dependency, self-criticism, and rumination—a hierarchical single factor, correlated factors, and a bifactor model (Schweizer et al., 2018). All three models exhibited good fit. The latent bifactor model organized these cognitive vulnerabilities into a common cognitive risk dimension (c factor), reflecting shared variance across all cognitive risk measures, and several specific latent factors representing unique facets of dysfunctional attitudes, negative inferential style, dependency and rumination measures. Supporting the validity of this model, the latent cognitive risk dimensions related to internalizing outcomes. The c factor associated with higher concurrent depressive symptoms, negative affect, and anxious arousal; lower concurrent positive affect; and prospectively predicted depressive episodes over two years. Specific dimensions of cognitive risk also related to validators, though relations were sparser and weaker (e.g., rumination-specific was the only specific dimension that related to higher negative affect).
Moreover, results supported the incremental utility of this bifactor model relative to the alternative structural models. The bifactor model captured links to outcomes that were identified for both the hierarchical single and correlated factors models. In addition, patterns of association with outcomes suggested that c resembled the hierarchical single factor, whereas the specific dimensions of the bifactor model generally resembled the dimensions of the correlated factors model. In summary, and supporting the rationale to continue the investigation of a bifactor model of cognitive risk as an approach to understand transdiagnostic risk, the bifactor model of cognitive risk integrated qualities of both alternative models and succinctly identified key associations with internalizing outcomes. However, as Schweizer and colleagues (2018) focused on examining links between the bifactor model of cognitive risks and individual internalizing outcomes, it is not yet known if dimensions of the bifactor model of cognitive risks relate specifically to internalizing outcomes or if they are more broadly transdiagnostic and relate to externalizing outcomes or general psychopathology (p) as well.
Present Study
Theory has proposed and research has identified numerous individual candidate risks as susceptibilities to various forms of psychopathology, yet it is unlikely that each risk factor is a separate, independent liability to a specific form of psychopathology. Cognitive vulnerabilities represent an ideal group of candidate risks to investigate this broader conceptual issue of transdiagnostic risk as they co-occur with one another and demonstrate similar connections to clinical outcomes, especially internalizing problems. In addition, internalizing and externalizing problems also demonstrate co-occurrence. Taken together, this raises the possibility that cognitive risks may be associated not only with specific internalizing problems, but also more broadly with the general psychopathology liability dimension (p factor) and the externalizing-specific dimension. Yet, to our knowledge, no research has directly examined whether cognitive vulnerabilities are associated transdiagnostically with latent psychopathology dimensions from the bifactor model of psychopathology. Investigating such questions of transdiagnostic breadth (i.e., multitude of relations) and potency (i.e., magnitude of relations) is clarified by assessing multiple manifestations of cognitive risks and psychopathology. Prior work has predominantly focused on examining the links between one form of cognitive risk (e.g., rumination) and one form of psychopathology (e.g., depression) using manifest measures of each. However, this approach is problematic because of the moderate correlations among cognitive risks and high co-occurrence among psychopathologies, which obscures the interpretation of findings (Hankin et al., 2016a).
Basic and translational knowledge in clinical psychology could be advanced by investigating whether there are transdiagnostic risks that could be organized in a simpler structural model, and whether these fewer vulnerability dimensions can be connected to a simpler set of latent dimensions of psychopathology. This is in line with recent theory (Hankin et al., 2016a) suggesting that bifactor models of risk can be linked with a bifactor model of psychopathology to better understand transdiagnostic connections between vulnerabilities and psychopathology. We pursue this line of inquiry in this study. We also replicate and extend initial empirical research supporting a bifactor model of cognitive risks, and validity of this model for predicting internalizing psychopathology outcomes (Schweizer et al., 2018).
We addressed two main questions in a community sample of children and adolescents, as this developmental period is particularly vulnerable for the emergence of many psychopathologies (Kessler et al., 2005) and cognitive vulnerabilities (Abela & Hankin, 2008). First, does a bifactor model of cognitive risk, including a broad cognitive vulnerability dimension (c) and specific dimensions of cognitive risk (e.g., for brooding, negative inferential style, dependency), replicate in early adolescents and extend to younger and older youth? To address this question, we compared the fit of the bifactor model with a correlated factors model. We predicted that the bifactor model of cognitive risk (Schweizer et al., 2018) would replicate in a sample of early adolescents (ages ~12–15) and extend to younger children (ages ~9–11) and older adolescents (ages ~5–17) given that these cognitive risks have been reliably measured and linked to psychopathology from childhood through adolescence (Abela & Hankin, 2008).
Second, what is the pattern of transdiagnostic association (i.e., breadth and potency) between cognitive vulnerabilities, as identified in this bifactor structural model, and the dimensional bifactor model of psychopathology? Are cognitive risk dimensions specifically associated with unique internalizing psychopathology, or are they more broadly transdiagnostic related to the general psychopathology (p) or the externalizing-specific dimensions? Based on prior work linking the common cognitive risk dimension (c) to multiple internalizing outcomes (Schweizer et al., 2018), considerable evidence indicating that these cognitive risks, when measured on a manifest level, demonstrate robust relations to internalizing outcomes and some studies linking certain risks to externalizing outcomes (Hankin et al., 2016b), we hypothesized that the c factor would relate strongly with the internalizing-specific dimension of psychopathology and weakly with the p factor and the externalizing-specific dimension of psychopathology. We also hypothesized that the specific cognitive risk dimensions would relate moderately with the internalizing-specific dimension and weakly with the p factor and externalizing-specific dimension of psychopathology. This prediction was based on prior evidence indicating that c demonstrates stronger links to multiple internalizing outcomes as compared to specific dimensions of cognitive risk (Schweizer et al., 2018).
We also examined the incremental utility of the bifactor modeling approach of cognitive risks relative to the traditional approach of examining each cognitive risk, individually, in relation to psychopathological outcomes. Specifically, we compared patterns of associations that emerged between the two bifactor models of cognitive risk and psychopathology, with patterns of associations for each individual cognitive risk and the bifactor model of psychopathology. Prior work has shown that the bifactor model of cognitive risks captured key links with internalizing outcomes that were identified with alternative models (Schweizer et al., 2018). Thus, we expected that the pattern of transdiagnostic associations (breadth and potency) between the bifactor models of cognitive risks and psychopathology would incorporate the main pattern of associations between each individual cognitive risk and the bifactor model of psychopathology.
Method
Participants and Procedures
The sample for the present study was recruited for a larger longitudinal study on risk to youth depression and co-occurring psychopathology, the Gene, Environment, and Mood (GEM) study (see Hankin et al., 2015 for details on sample and procedures). Brief information letters were sent home directly to the participating school districts of families with a child in 3rd, 6th, or 9th grades. Parent report established that both the parent and child were fluent in English, the child did not have an autism spectrum or psychotic disorder, and the child had an IQ > 70. There was a 60% participation rate of qualified participants (Hankin et al., 2015). The caretaker and youth visited the laboratory for an in-person, initial visit where caretakers provided informed written consent for their child’s participation; youth provided written assent. The institutional review boards approved all procedures.
The current study used data from the 18-month follow-up because the sample was at a comparable stage of development as prior work examining the bifactor model of cognitive risk (Schweizer et al., 2018), and the full set of measures for the current analyses were collected at this timepoint. At this follow-up, 571 youth-parent pairs participated. Participating youth identified their gender as 55% female (45% male); their race as .9% American Indian or Alaskan Native, 8.9% Asian or Pacific Islander, 11.0% Black or African American, 66.1% White, 5.9% multiracial, and 4.7% as other; and their ethnicity as 85% Non-Hispanic or Non-Latinx, and 12.4% as Hispanic or Latinx. On average, youth participants were 13.58 years old (SD=2.37, range=9.27–17.53). Each of the initial 3rd, 6th, and 9th grade cohorts were at the following developmental stages at the 18-month follow-up: late childhood (n=174, M=10.64, SD=0.51, range=9.27–11.73), early adolescence (n=213, M=13.52, SD=0.55, range=12.28–15.77), and middle-late adolescence (n=182, M=16.64, SD=0.50, range=15.15–17.53).
Cognitive Vulnerability Measures
Youth reported on cognitive vulnerabilities. Reliabilities are reported in Table 1.
Table 1.
Descriptive Information and Correlations Among Manifest Measures of Cognitive Risk and Psychopathology
| CDI | MASC PH | MASC SA | MASC SP | CBCL/YSR ODD | CBCL/YSR CD | SNAP Inat. | SNAP Hyp. | EATQ AG | CDAS | ACSQ | CDEQ-SC | CDEQ-Depend. | CRSQ-Brood. | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| c | P | C | P | C | P | C | P | P | C | P | C | P | P | C | P | C | C | C | C | C | ||
| CDI | C | .88 | ||||||||||||||||||||
| P | 0.35 | .88 | ||||||||||||||||||||
| MASCPH | C | 0.51 | 0.18 | .85 | ||||||||||||||||||
| P | 0.23 | 0.53 | 0.28 | .84 | ||||||||||||||||||
| MASC SA | c | 0.43 | 0.13 | 0.52 | 0.10 | .87 | ||||||||||||||||
| P | 0.15 | 0.48 | 0.10 | 0.43 | 0.24 | .88 | ||||||||||||||||
| MASC SP | c | 0.08 | 0.01 | 0.39 | 0.12 | 0.38 | 0.17 | .76 | ||||||||||||||
| P | −0.04 | 0.23 | 0.13 | 0.42 | 0.05 | 0.39 | 0.46 | .79 | ||||||||||||||
| CBCL/YSR ODD | P | 0.14 | 0.52 | 0.08 | 0.40 | −0.01 | 0.37 | −0.01 | 0.21 | .66 | ||||||||||||
| c | 0.48 | 0.29 | 0.32 | 0.20 | 0.25 | 0.09 | −0.01 | −0.06 | 0.30 | .78 | ||||||||||||
| CBCL/YSR CD | P | 0.14 | 0.55 | 0.05 | 0.37 | −0.03 | 0.32 | −0.03 | 0.13 | 0.72 | 0.25 | .70 | ||||||||||
| c | 0.57 | 0.23 | 0.34 | 0.16 | 0.23 | 0.08 | −0.07 | −0.09 | 0.24 | 0.62 | 0.30 | .78 | ||||||||||
| SNAP Inat. | P | 0.21 | 0.53 | 0.07 | 0.33 | 0.00 | 0.36 | −0.01 | 0.16 | 0.49 | 0.20 | 0.46 | 0.19 | .94 | ||||||||
| SNAP Hyp. | P | 0.13 | 0.45 | 0.05 | 0.42 | −0.10 | 0.30 | 0.08 | 0.27 | 0.48 | 0.15 | 0.44 | 0.08 | 0.61 | .90 | |||||||
| EATQ AG | c | 0.43 | 0.20 | 0.31 | 0.15 | 0.26 | 0.08 | 0.03 | −0.03 | 0.21 | 0.55 | 0.20 | 0.63 | 0.13 | 0.09 | .78 | ||||||
| P | 0.17 | 0.47 | 0.09 | 0.39 | 0.00 | 0.39 | 0.04 | 0.19 | 0.64 | 0.21 | 0.62 | 0.25 | 0.43 | 0.47 | 0.26 | .74 | ||||||
| CDAS | c | 0.45 | 0.06 | 0.34 | 0.04 | 0.43 | 0.00 | 0.14 | −0.03 | 0.00 | 0.24 | 0.00 | 0.28 | −0.02 | −0.04 | 0.25 | 0.04 | .85 | ||||
| ACSQ | c | 0.54 | 0.18 | 0.40 | 0.13 | 0.50 | 0.14 | 0.12 | −0.04 | 0.03 | 0.32 | 0.03 | 0.35 | 0.03 | −0.03 | 0.34 | 0.06 | 0.47 | .93 | |||
| CDEQ-SC | c | 0.50 | 0.11 | 0.43 | 0.12 | 0.52 | 0.01 | 0.13 | −0.06 | −0.04 | 0.30 | −0.05 | 0.30 | −0.04 | −0.06 | 0.25 | −0.01 | 0.73 | 0.54 | .84 | ||
| CDEQ-Depend. | c | 0.35 | 0.05 | 0.38 | 0.11 | 0.56 | 0.09 | 0.27 | 0.05 | −0.05 | 0.19 | −0.10 | 0.15 | −0.01 | −0.08 | 0.15 | −0.07 | 0.62 | 0.46 | 0.65 | .83 | |
| CRSQ-Brood. | c | 0.57 | 0.16 | 0.50 | 0.16 | 0.50 | 0.09 | 0.20 | −0.01 | 0.07 | 0.36 | 0.03 | 0.37 | 0.04 | 0.00 | 0.40 | 0.03 | 0.42 | 0.52 | 0.56 | 0.48 | .86 |
| Mean (SD) | 5.27 (5.86) | 3.99 (5.16) | 6.44 (5.73) | 4.78 (4.63) | 7.53 (5.79) | 9.56 (5.44) | 5.23 (4.40) | 5.97 (4.81) | 2.12 (1.89) | 1.80 (2.04) | 2.71 (2.59) | 1.85 (2.53) | 8.12 (6.65) | 4.28 (4.83) | 11.24 (4.08) | 15.14 (4.89) | 33.16 (7.36) | 57.77 (22.03) | 19.04 (4.51) | 20.87 (4.57) | 10.35 (3.88) | |
Note. C=Child report; P=Parent report; CDI=Children’s Depression Inventory; MASC=Manifest Anxiety Scale for Children; SA=social anxiety; PH=physical symptoms; SP =separation/panic symptoms; CBCL/YSR=Child Behavior Checklist/Youth Self Report; ODD=oppositional defiant disorder symptoms; CD=conduct disorder symptoms; EATQ=Early Adolescent Temperament Questionnaire; AG=aggression; SNAP=Swanson, Nolan, and Pelham scale; Inat.=inattention; Hyp.=hyperactivity; CDAS=Children’s Dysfunctional Attitudes Scale; ACSQ=Adolescent Cognitive Style Questionnaire; CDEQ=Children’s Depressive Experiences Questionnaire, SC=Self Criticism subscale, Depend.= Dependency subscale; CRSQ-Brood.=Child Response Styles Questionnaire, brooding items. Correlations within reporter shown in blue for child report and grey for parent report. Alphas are in italics and located on the diagonal. Bold indicates significance at p < .05.
Children’s dysfunctional attitudes scale (CDAS; Abela & Sullivan, 2003).
Youth completed twenty items assessing dysfunctional attitudes (DA) via a 4-point scale. Higher scores reflect greater DA. CDAS shows good reliability and validity for youth (Abela & Sullivan, 2003).
Adolescent cognitive style questionnaires (ACSQ; Hankin & Abramson, 2002).
Youth rated items on a 7-point scale to assess negative inferential style (NIS) subscales (stable, global, consequence, self) via six hypothetical negative event scenarios. Higher scores indicate greater NIS. The ACSQ is reliable and valid (Lakdawalla, Hankin, & Mermelstein, 2007).
Child response styles questionnaire-rumination subscale (CRSQ-RS; Abela, Brozina, & Haigh, 2002).
Brooding was measured with six items from the CRSQ-RS. Youth rate how frequently they respond when feeling sad on a 4-point scale. Higher scores indicate greater brooding. This brooding subscale shows good reliability and validity (Schweizer et al., 2018).
Children’s depressive experiences questionnaire (CDEQ; Abela & Taylor, 2003).
The two distinct constructs of self-criticism and dependency were assessed with two separate scales (12 items each) from the CDEQ using a 3-point scale. Higher scores indicate more self-criticism and dependency. Scales have good reliability and validity (Abela & Taylor, 2003).
Psychopathology Measures
Youth and a caregiver reported on psychopathology. Reliabilities are reported in Table 1.
Children’s depression inventory (CDI; Kovacs, 1985).
The CDI assesses depressive symptoms in children and adolescents and has good reliability and validity (Klein, Dougherty, & Olino, 2005).
Manifest anxiety scale for children (MASC; March, Parker, Sullivan, Stallings, & Conners, 1997).
The MASC assesses anxious symptoms in youth. It contains subscales of Physical Symptoms of Anxiety, Social Anxiety, and Separation Anxiety/Panic. We did not use the Harm Avoidance subscale as it does not assess anxiety but rather risk aversion (Snyder et al., 2015). The MASC has good reliability and validity (March et al., 1997).
Child behavior checklist (CBCL) and youth self-report (YSR) (Achenbach & Rescorla, 2001).
The CBCL and YSR are widely used and validated measures of youth mental health. We used the Oppositional Defiant Disorder (ODD) and Conduct Disorder (CD) DSM-oriented scales, which have good reliability and validity (Achenbach & Rescorla, 2001).
Aggression scale of the early adolescent temperament questionnaire-revised (EATQ-R; Ellis & Rothbart, 2001).
The EATQ-R scale assesses hostile reactivity and aggressive physical and verbal actions in youth; it has good reliability and convergent validity (Snyder et al., 2015).
Multisite multimodal treatment study of children with ADHD (MTA) SNAP-IV (Swanson et al., 2001).
Parents completed the SNAP-IV, including items assessing ADHD (inattention, hyperactivity). It has good reliability and validity (Bussing et al., 2008).
Data Analytic Plan
There were three main steps. First, to examine whether the bifactor model of cognitive risks would replicate in a sample having a similar level of development as prior work (Schweizer et al., 2018), a latent bifactor model of cognitive risks was constructed based on the early adolescent group (ages ~12–15). The bifactor model was compared to an alternative correlated factors model. Second, an examination of model invariance by development (i.e., comparing late childhood, early adolescent, and late adolescent groups) was conducted to examine if the bifactor model of cognitive risks found in early adolescents also extended to younger (i.e., late childhood; ages ~9–12) and older youth (i.e., later adolescence; ages ~15–17). The correlated factors model was also examined for invariance across development and was compared to the bifactor model. Third, the bifactor models of cognitive risk and psychopathology were examined jointly. In addition, each cognitive risk factor, considered individually from the correlated factors model, was associated with the bifactor model of psychopathology. The bifactor model of psychopathology including the full sample of the current study has been published previously (see Snyder, Young, & Hankin, 2017a for details). Each factor of psychopathology (p factor, internalizing-specific, externalizing-specific) was regressed on each factor of cognitive risk in the bifactor model simultaneously (c factor, and specific cognitive risk dimensions that emerged in step one). Each factor of psychopathology (p factor, internalizing-specific, externalizing-specific) was also regressed on each cognitive risk factor, considered individually (dysfunctional attitudes, negative inferential style, dependency, self-criticism, rumination), in separate regression models.
Confirmatory factor analyses (CFA) were conducted with Mplus (L. K. Muthén & Muthén, 2012) using full information maximum likelihood estimation to address missing data. For all models, “good fit” was defined as root mean square error of approximation (RMSEA) ≤ .06, confirmatory fit index (CFI) ≥ .95, and standardized root mean square residual (SRMR) ≤ .08; “acceptable fit” was defined as RMSEA ≤ .08 and CFI ≥ .90 (Hu & Bentler, 1999). We prioritized convergence across fit indices to indicate a good model; researchers regard these as suggested thresholds rather than universal rules (Hu & Bentler, 1999).
Latent dimensional bifactor model for cognitive risks.
Manifest indicators for cognitive risk were created using the same item parceling procedures as in past research (i.e., correlational and facet-representative approaches) (Schweizer et al., 2018) (see supplement for additional details). Model development and testing consisted of two steps. First, the latent factor structure of each cognitive risk construct was examined individually (i.e., dysfunctional attitudes, negative inferential style, etc., were each examined in separate single factor models) (see supplement for additional details). Second, a bifactor model of cognitive risks, including a common factor as well as specific latent factors was examined. We implemented recommended, standard procedures for constructing and evaluating a latent bifactor model (Chen, West, & Sousa, 2006). All indicators were initially loaded directly onto a common factor, which captures the shared variance across all indicators. In addition, all indicators were loaded onto their respective cognitive risk measure factors, which capture the unique variance of each measure of cognitive risk not accounted for by the common factor (Chen et al., 2006). Because the common factor captures the shared variance across these cognitive risk measures, the specific cognitive risk factor correlations were set to zero (Chen et al., 2006; Muthén & Muthén, 2012). The bifactor model including all parcel indicators across all measures of cognitive risks was initially tested and respecified based on the pattern of indicator loadings and the significance of factor variances1. Specific factors were eliminated if: (1) indicator loadings were non-significant or negative for the specific factor and strong for the common factor, or (2) if the specific factor variance was not significantly different from zero. Each of these cases suggests that the variance among the indicators was accounted for by the common factor, so the specific factor should not be considered as separable from the common factor. This same procedure was applied to the respecification of indicator loadings onto the common factor (see supplement for additional details). The correlated factors model included a total of five latent factors, each representing a cognitive risk construct according to its original theoretical conceptualization (i.e., dysfunctional attitudes, negative inferential style, dependency, self-criticism, rumination).
We then conducted measurement invariance testing [configural (model form), metric (factor loadings), and scalar (indicator intercepts)] for the latent models of cognitive risk across age groups (late childhood, early adolescent, late adolescent) using multiple-sample CFA (Kline, 2015). We utilized convergence across difference in fit for CFI and RMSEA such that change in CFI ≤ .01 and change in RMSEA ≤ .015 suggests measurement invariance (Chen, 2007).
The fit of the bifactor and correlated factors models was compared using Akaike information criteria (AIC) and Bayesian information criteria (BIC) because the models were non-nested (lower values indicate better fit; Δ>10 is considered a general cut-off suggesting that models are different; Burnham & Anderson, 2003).
Latent dimensional bifactor model for psychopathology.
We used the same latent dimensional bifactor model of psychopathology that has been demonstrated using this sample, time point and measures (Snyder, Young, & Hankin, 2017a).
Connecting latent dimensional models for cognitive risk and psychopathology.
To examine the degree to which common and specific dimensions of cognitive risk were relatively broadly or uniquely related to different forms of psychopathology, each dimension of psychopathology (p factor, internalizing-specific, externalizing-specific) was regressed on each dimension of cognitive risk (c factor, specific cognitive risk factors) simultaneously within an SEM framework using Mplus (L. K. Muthén & Muthén, 2012). We also examined each dimension of psychopathology (p factor, internalizing-specific, externalizing-specific) regressed on each latent factor of cognitive risk individually (i.e., single factors for dysfunctional attitudes, negative inferential style, self-criticism, dependency, rumination).
Gender was controlled for in all regression analyses. The two-stage False Discovery Rate (FDR) was utilized to constrain the error rate to p=.05 across analyses (Benjamini, Krieger, & Yekutieli, 2006). The aims, method, and data analytic plan for the present study were pre-registered on the Open Science Framework prior to conducting analyses (https://osf.io/ke3jr/).
Results
Descriptive statistics for manifest measures of cognitive risks and psychopathology, internal consistencies in this study, and correlations between manifest measures of cognitive risks and psychopathology are located in Table 1.
Bifactor and Correlated Factors Cognitive Risk Models
All the individual single factor cognitive risk models for dysfunctional attitudes, negative inferential style, self-criticism, dependency, and brooding had good fit by CFI, RMSEA, and SRMR (see S1 in supplement for more details). For the bifactor model including all measures of cognitive risk, there were 18 item parcel indicators total (see supplement for more details). We started by examining if the model from prior work of early adolescents (Schweizer et al., 2018), which included a common cognitive risk (c) factor and four specific factors for dysfunctional attitudes, negative inferential style, dependency and brooding, would replicate within the same developmental group. The initial bifactor model fit was good (SRMR=.06) to acceptable (CFI=.92, RMSEA=.08). Examination of factor loadings revealed that all dysfunctional attitudes, all self-criticism indicators, and two out of four dependency indicators had non-significant or negative loadings for their respective specific factors, but these same loadings were significant and adequate for c. This suggested that variance for all dysfunctional attitudes and self-criticism indicators and two dependency indicators were accounted for by the common cognitive risk factor and not their respective specific factors. Thus, all loadings for the dysfunctional attitudes-specific and the self-criticism-specific factors were removed; this resulted in the elimination of these two specific factors. Additionally, the two non-significant loadings for the dependency-specific factor were removed, and the two remaining loadings for the dependency-specific factor were constrained to be equal for model identification. All remaining loadings and factor variances were significant (see S2 in the supplement for more details). A residual correlation between a self-criticism and dysfunctional attitudes indicator improved model fit. Final model fit for the bifactor model in the early adolescent age group including c and three specific factors for brooding, negative inferential style, and dependency was acceptable (CFI=.92, RMSEA=.08) to good (SRMR=.06) (see Table 2).
Table 2.
Fit Statistics for the Bifactor and Correlated Factors Models for Cognitive Risks and Measurement Invariance Across Age Groups4
| Model | χ2(df) | CFI | RMSEA (90% CI) | SRMR | AIC | BIC |
|---|---|---|---|---|---|---|
| Bifactor Model | ||||||
| Early Adolescent Group | 275.118(124)* | 0.924 | 0.076 (0.064 – 0.088) | 0.059 | 5064.65 | 5283.134 |
| All Age Groups Combined | 509.650 (124)* | 0.933 | 0.074 (0.067 – 0.081) | 0.055 | 13467.177 | 13749.757 |
| Loadings & Intercepts Constrained Across Grade Cohorts (Scalar) | 1023.935 (444)* (3rd=365.957, 6th=307.650, 9th=350.328) | 0.895 | 0.083 (0.076 – 0.090) | 0.092 | 13369.612 | 13904.340 |
| Loadings Constrained Across Grade Cohorts (Metric) | 868.742 (416)* (3rd=294.379, 6th=297.554, 9th=276.809) | 0.918 | 0.076 (0.069 – 0.083) | 0.080 | 13270.418 | 13926.874 |
| Unconstrained Loadings Across Grade Cohorts (Configural) | 806.982 (374)* (3rd=271.083, 6th=275.403, 9th=260.496) | 0.922 | 0.078(0.071 – 0.085) | 0.067 | 13292.659 | 14131.705 |
| Correlated Factors Model | ||||||
| Early Adolescent Group | 287.540 (123)* | 0.917 | 0.079 (0.067 – 0.091) | 0.063 | 5079.075 | 5300.921 |
| All Age Groups Combined | 527.538 (123)* | 0.930 | 0.076 (0.069 – 0.083) | 0.057 | 13487.063 | 13773.991 |
| Loadings & Intercepts Constrained (Scalar) | 1005.175 (421)* (3rd=365.957, 6th=307.650, 9th=350.328) | 0.895 | 0.085 (0.079 – 0.092) | 0.086 | 13369.612 | 13904.34 |
| Loadings Constrained (Metric) | 841.93 (395)* (3rd=284.725, 6th=299.994, 9th=257.214) | 0.919 | 0.077 (0.070 – 0.084) | 0.075 | 13285.609 | 14033.36 |
| Unconstrained Loadings (Configural) | 806.731 (369)* (3rd=270.082, 6th=287.543, 9th=248.369) | 0.921 | 0.079 (0.072 – 0.086) | 0.066 | 13302.407 | 14163.19 |
Note. Early adolescent group (n=213); all age groups combined (late childhood, early adolescent, late adolescent), N=571; CFI = confirmatory fit index; RMSEA = root mean square error of approximation; SRMR = standardized root mean square residual; AIC = akaike information criterion; BIC = bayesian information criterion.
p < .001
The bifactor model was compared to a correlated factors model, which included all manifest indicators across all cognitive risk measures and all five of the latent factors from each of the individual cognitive risk factor models (dysfunctional attitudes, negative inferential style, self-criticism, dependency, brooding). Model fit of the correlated factors model was acceptable (CFI=.92, RMSEA=.08) to good (SRMR=.06) (see Table 2). The two models showed similar fit, although there were slight advantages in favor of the bifactor model relative to the correlated factors model on information criteria (ΔAIC=−14.43, ΔBIC=−17.79) (see Table 2).
Invariance of the bifactor and correlated factors models for cognitive risks by developmental age.
The bifactor and correlated factors models that were identified in the early adolescent group (see preceding section) were then examined for invariance across developmental age (see Table 2). For both the bifactor and correlated factors models, convergence across model fit indices and results of comparisons suggest invariance across developmental stage at the metric level. Across all age groups, model fit for the unconstrained loadings (configural) and the constrained loadings (metric) models was acceptable (CFI, RMSEA) to good (SRMR), but not acceptable for constrained intercepts (scalar). For both the bifactor and correlated factors models change in CFI and RSMEA supported metric invariance (bifactor model: ΔCFI=.004, ΔRMSEA=.002; correlated factors model: ΔCFI=.002, ΔRMSEA=.002).
For our present purposes, only partial metric invariance was required so that we could examine relations between latent factors of cognitive risk and external variables. Partial metric invariance suggests that the same factors are being measured with the same indicators across groups (e.g., developmental stage) (Kline, 2015). Thus, we used the full sample to have maximal statistical power to provide well-estimated effect sizes for relations between the latent factors of cognitive risk and psychopathology.
For the full sample, as seen in Table 2, model fit for the bifactor model was acceptable (CFI=.93, RMSEA=.07) to good (SRMR=.06), and model fit for the correlated factors model was acceptable (CFI=.93, RMSEA=.08) to good (SRMR=.06). Model fit of the bifactor model was better than the correlated factor model (ΔAIC=−19.89, ΔBIC=−24.23).
Examining Associations Between Cognitive Risks and Psychopathology
Linking the latent bifactor models of cognitive risk and psychopathology.
Results are reported in Table 3 and depicted in Figure 1. Higher common cognitive risk was associated with higher general psychopathology (β=.33), and specific internalizing (β=.86) and externalizing (β=.42) (all p’s<.01). Higher brooding-specific was associated with higher general psychopathology (β=.26) and specific internalizing and externalizing (both β’s=.25) (all p’s<.05). Higher negative inferential style-specific was associated with higher specific internalizing (β=.23) and externalizing (β=.12) (all p’s<.05). Dependency-specific was associated with lower general psychopathology (β=−.25) and externalizing-specific (β=−.22) (both p’s<.05).
Table 3.
Regressions for the Bifactor Models of Cognitive Risk and Psychopathology
| DV | IV | β | 95% CI | b | S.E. (b) | Z | Uncorrected P | FDR corrected p |
|---|---|---|---|---|---|---|---|---|
| General Psychopathology (p) | ||||||||
| C.CR | 0.33 | 0.21,0.44 | 0.38 | 0.08 | 4.68 | 0.00 | 0.00 | |
| NIS-Spec. | 0.04 | −0.07,0.16 | 0.05 | 0.07 | 0.74 | 0.46 | 0.13 | |
| Depend.-Spec. | −0.21 | −0.37, −0.06 | −0.25 | 0.10 | −2.58 | 0.01 | 0.00 | |
| Brood.-Spec. | 0.26 | 0.15,0.38 | 0.31 | 0.08 | 3.98 | 0.00 | 0.00 | |
| Gender | −0.19 | −0.29, −0.08 | −0.44 | 0.13 | −3.42 | 0.00 | 0.00 | |
| Internalizing-Specific | ||||||||
| C.CR | 0.86 | 0.78, 0.93 | 2.64 | 0.86 | 3.09 | 0.00 | 0.00 | |
| NIS-Spec. | 0.23 | 0.13,0.32 | 0.69 | 0.27 | 2.60 | 0.01 | 0.00 | |
| Depend.-Spec. | 0.06 | −0.09, 0.20 | 0.17 | 0.23 | 0.75 | 0.45 | 0.13 | |
| Brood.-Spec. | 0.25 | 0.14,0.36 | 0.76 | 0.30 | 2.51 | 0.01 | 0.01 | |
| Gender | 0.21 | 0.11,0.31 | 1.29 | 0.49 | 2.65 | 0.01 | 0.00 | |
| Externalizing-Specific | ||||||||
| C.CR | 0.42 | 0.30, 0.54 | 0.50 | 0.10 | 5.20 | 0.00 | 0.00 | |
| NIS-Spec. | 0.12 | 0.00, 0.25 | 0.15 | 0.08 | 1.93 | 0.05 | 0.02 | |
| Depend.-Spec. | −0.22 | −0.39, −0.04 | −0.26 | 0.11 | −2.26 | 0.02 | 0.01 | |
| Brood.-Spec. | 0.25 | 0.11,0.38 | 0.29 | 0.09 | 3.25 | 0.00 | 0.00 | |
| Gender | 0.08 | −0.04, 0.20 | 0.18 | 0.15 | 1.25 | 0.21 | 0.07 | |
Note. N = 571. C.CR = Common cognitive risk dimension; Spec. = Specific dimension; NIS = Negative inferential style; Depend. = Dependency; Brood. = Brooding.
Figure 1.
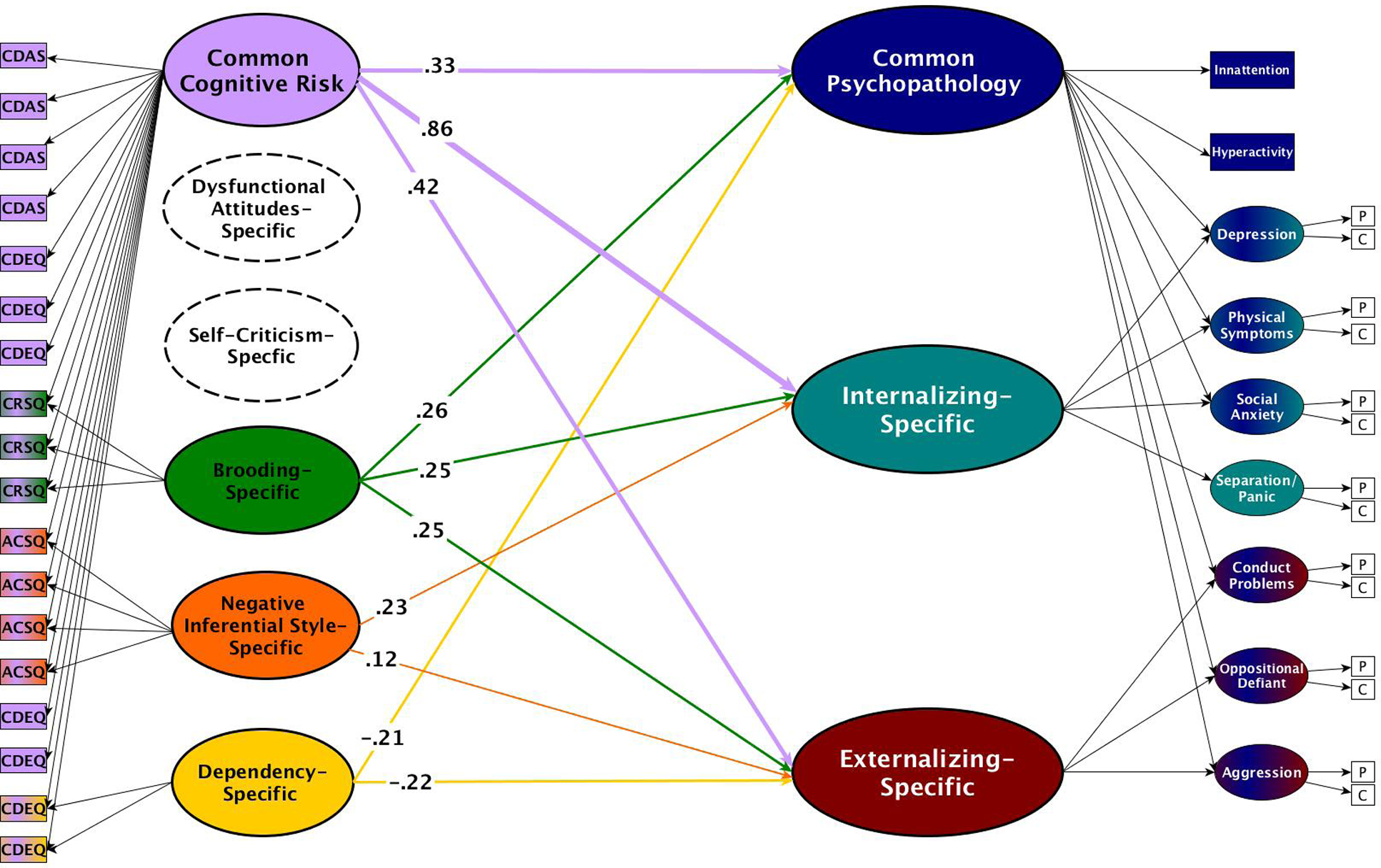
Model depicting associations between bifactor models of cognitive risk and psychopathology controlling for gender. Numbers on lines are standardized regression coefficients (all p’s < .05). The thickness of lines reflects the magnitude of regression coefficients. The specific dysfunctional attitudes and self-criticism factors have a dashed outline because they were both subsumed by the common cognitive risk factor. Cognitive risk measures: ACSQ=Adolescent Cognitive Style Questionnaire; CDAS=Children’s Dysfunctional Attitudes Scale; CDEQ=Children’s Depressive Experiences Questionnaire; CRSQ=Child Response Styles Questionnaire-Brooding items. Psychopathology measures: inattention and hyperactivity were measured via parent report with the National Institute of Mental Health Collaborative MTA version of SNAP-IV; depression was measured with the Children’s Depression Inventory (CDI); anxiety was measured with the physical symptoms of anxiety, social anxiety, and separation/panic subscales of the Manifest Anxiety Scale for Children (MASC); oppositional defiant disorder (ODD) and conduct disorder (CD) were assessed with the DSM-oriented scales of the Child Behavior Checklist (CBCL) and Youth Self Report (YSR); aggression was measured with the aggression scale of the Early Adolescent Temperament Questionnaire Revised (EATQ-R). P=parent report. C=child report. Though not depicted here to improve readability, the bifactor model of psychopathology included reporter method factors and random intercept factors for both parent and child report (for more details, see Snyder et al., 2017a).
Linking each individual cognitive risk and the bifactor model of psychopathology.
Results are reported in Table 4. Higher dysfunctional attitudes, negative inferential style, self-criticism, dependency, and brooding were all associated with higher general psychopathology (average β=.27, range from .14 to .37, all p’s<.05), and specific internalizing (average β=.77, range from .67 to .87, all p’s<.05) (all p’s<.01). All cognitive risks, with the exception of dependency (β=.14, p=.08), were positively associated with specific externalizing (average β=.37, β’s ranging from .25 to .46, all p’s<.05) (all p’s<.05).
Table 4.
Regressions for Each Individual Cognitive Risk Factor and the Bifactor Model of Psychopathology
| DV | IV | β | 95% CI | b | S.E. (b) | z | Uncorrected P | FDR corrected p |
|---|---|---|---|---|---|---|---|---|
| Internalizing-Specific | ||||||||
| Dysfunctional Attitudes | 0.74 | 0.62,0.86 | 1.27 | 0.25 | 5.05 | 0.00 | 0.00 | |
| Gender | 0.34 | 0.22, 0.47 | 1.20 | 0.27 | 4.44 | 0.00 | 0.00 | |
| Externalizing-Specific | ||||||||
| Dysfunctional Attitudes | 0.37 | 0.23,0.52 | 0.41 | 0.09 | 4.31 | 0.00 | 0.00 | |
| Gender | 0.13 | −0.01,0.26 | 0.28 | 0.15 | 1.83 | 0.07 | 0.07 | |
| General Psychopathology (p) | ||||||||
| Dysfunctional Attitudes | 0.26 | 0.14,0.39 | 0.28 | 0.07 | 3.85 | 0.00 | 0.00 | |
| Gender | −0.19 | −0.30, −0.08 | −0.40 | 0.12 | −3.35 | 0.00 | 0.00 | |
| Internalizing-Specific | ||||||||
| Negative Inferential Style | 0.67 | 0.55,0.80 | 1.28 | 0.25 | 5.07 | 0.00 | 0.00 | |
| Gender | 0.38 | 0.25,0.51 | 1.20 | 0.29 | 4.1 | 0.00 | 0.00 | |
| Externalizing-Specific | ||||||||
| Negative Inferential Style | 0.25 | 0.08,0.41 | 0.31 | 0.11 | 2.74 | 0.01 | 0.01 | |
| Gender | 0.15 | 0.03,0.28 | 0.32 | 0.13 | 2.43 | 0.02 | 0.02 | |
| General Psychopathology (p) | ||||||||
| Negative Inferential Style | 0.34 | 0.23, 0.46 | 0.40 | 0.08 | 4.82 | 0.00 | 0.00 | |
| Gender | −0.13 | −0.23, −0.02 | −0.24 | 0.11 | −2.3 | 0.02 | 0.02 | |
| Internalizing-Specific | ||||||||
| Self-Criticism | 0.87 | 0.76,0.99 | 1.99 | 0.62 | 3.23 | 0.00 | 0.00 | |
| Gender | 0.22 | 0.09, 0.34 | 0.99 | 0.37 | 2.69 | 0.01 | 0.01 | |
| Externalizing-Specific | ||||||||
| Self-Criticism | 0.39 | 0.25,0.54 | 0.43 | 0.1 | 4.44 | 0.00 | 0.00 | |
| Gender | 0.08 | −0.06, 0.22 | 0.17 | 0.16 | 1.08 | 0.28 | 0.05 | |
| General Psychopathology (p) | ||||||||
| Self-Criticism | 0.26 | 0.13,0.39 | 0.28 | 0.08 | 3.66 | 0.00 | 0.00 | |
| Gender | −0.24 | −0.34, −0.13 | −0.51 | 0.12 | −4.14 | 0.00 | 0.00 | |
| Internalizing-Specific | ||||||||
| Dependency | 0.78 | 0.66,0.91 | 1.40 | 0.33 | 4.29 | 0.00 | 0.00 | |
| Gender | 0.29 | 0.16,0.41 | 1.03 | 0.3 | 3.49 | 0.00 | 0.00 | |
| Externalizing-Specific | ||||||||
| Dependency | 0.14 | −0.05, 0.32 | 0.14 | 0.1 | 1.46 | 0.15 | 0.08 | |
| Gender | 0.12 | −0.03, 0.27 | 0.25 | 0.16 | 1.57 | 0.12 | 0.07 | |
| General Psychopathology (p) | ||||||||
| Dependency | 0.14 | 0.00, 0.27 | 0.14 | 0.07 | 1.94 | 0.05 | 0.04 | |
| Gender | −0.18 | −0.29, −0.07 | −0.38 | 0.12 | −3.14 | 0.00 | 0.00 | |
| Internalizing-Specific | ||||||||
| Brooding | 0.79 | 0.69,0.89 | 2.34 | 0.43 | 5.47 | 0.00 | 0.00 | |
| Gender | 0.27 | 0.15,0.40 | 1.00 | 0.25 | 3.97 | 0.00 | 0.00 | |
| Externalizing-Specific | ||||||||
| Brooding | 0.46 | 0.32,0.60 | 0.86 | 0.17 | 5.12 | 0.00 | 0.00 | |
| Gender | 0.08 | −0.06,0.21 | 0.17 | 0.15 | 1.13 | 0.26 | 0.05 | |
| General Psychopathology (p) | ||||||||
| Brooding | 0.37 | 0.26, 0.49 | 0.55 | 0.1 | 5.44 | 0.00 | 0.00 | |
| Gender | −0.22 | −0.32, −0.12 | −0.4 | 0.1 | −4.02 | 0.00 | 0.00 | |
Note. N = 571.
Discussion
The present study empirically examined the idea that transdiagnostic relations between risks and psychopathology can be better understood by: (1) organizing both risks and psychopathological outcomes using latent dimensional bifactor models that parse out and organize the common and unique aspects within each construct, and (2) examining patterns of associations (i.e., breadth and potency) between the two latent structural models of risk and psychopathology. Specifically, we examined this notion by studying a bifactor model of cognitive risks, consisting of a common cognitive risk factor (c factor) and several specific cognitive risk dimensions. We evaluated two major propositions: (1) does this bifactor model of cognitive risk replicate (Schweizer et al., 2018), and is the bifactor model invariant across children and adolescents?; and (2) how does the bifactor model of cognitive risk relate to the latent dimensions from the bifactor model of psychopathology? Do dimensions of cognitive risk relate uniquely and strongly to the internalizing-specific dimension, or do they also relate more broadly to the general psychopathology (p factor) and the externalizing-specific dimensions? Does the bifactor modeling approach of cognitive risk add incremental utility over the traditional approach, which is to examine individual cognitive risks in relation to clinical outcomes?
Results showed that a bifactor model of cognitive risks largely replicated in a sample of early adolescents (ages ~12–15) and was invariant across development, such that the model extended to younger (ages ~9–12) and older youth (ages ~15–17). This bifactor model and a correlated factors model both fit the data well, although the bifactor model exhibited slightly better fit on information criteria (AIC, BIC) than a correlated factors model. C and specific latent factors of cognitive risk related to all latent dimensions of psychopathology (i.e., p, internalizing-specific, and externalizing-specific). In particular, c was potently associated (large effect) with what is uniquely shared across internalizing syndromes (internalizing-specific dimension) and related to general psychopathology (p factor) with a small-medium effect and to specific externalizing with a medium effect. Moreover, the bifactor model largely captured the pattern of associations that were identified when each cognitive risk factor was individually associated with all dimensions of psychopathology. This finding supports the incremental utility of the bifactor modeling approach over the traditional approach to conceptualizing and examining risks as distinct constructs. Findings from this research provide insight into how common and specific cognitive vulnerability dimensions confer transdiagnostic risk across the breadth of psychopathology among youth, and illuminate future directions of work for more parsimonious assessment and intervention approaches targeting c.
The present study replicates and extends prior research (Schweizer et al., 2018) showing that a bifactor model organizes cognitive risk constructs across multiple theoretical paradigms into fewer dimensions. A common cognitive risk factor (c) captures the covariance across all measured cognitive risk measures, including self-criticism, rumination (brooding), dysfunctional attitudes, negative inferential style, and dependency. In addition to this general cognitive vulnerability, specific latent cognitive risk dimensions were observed for brooding, negative inferential style, and dependency that are independent of c. No specific factors emerged for self-criticism or dysfunctional attitudes as variance for these indicators was entirely explained and subsumed by c. Stated differently, the self-criticism and dysfunctional attitudes factors correlated so strongly with c that they did not have any remaining variance left over to form specific factors. Thus, it is likely these constructs represent core, defining features of c. Results of the present study, especially in light of replication of prior work (Schweizer et al. 2018)2, lend further support to the notion that although these cognitive risks have been traditionally conceptualized and predominantly studied as independent risks for outcomes, they might be better understood as having both common and distinct components that can be organized by a single unifying model.
The present study also extends our knowledge of cognitive risks across development. The bifactor model of cognitive risks replicated in a community sample of early adolescents (Schweizer et al., 2018) and exhibited metric invariance in both late childhood and late adolescent age groups. Prior work has shown that multiple cognitive risks develop into relatively stable trait-like risks for psychopathology across adolescence (Hankin, 2008), and a single latent factor of several cognitive risks demonstrated stability across middle childhood (Hong, Lee, Tsai, & Tan, 2017). The present study suggests that the bifactor structure of cognitive risks appears to be stable from late childhood through adolescence.
By connecting the latent dimensional bifactor models of cognitive risks and psychopathology together, this study illuminates useful patterns of associations between general cognitive risk and forms of psychopathology. C confers broad transdiagnostic risk, particularly strongly for the internalizing-specific dimension, and also to general psychopathology and externalizing specific problems to a lesser extent. Common cognitive risk (c) strongly related to the internalizing-specific dimension of psychopathology (β=.86). Schweizer and colleagues (2018) similarly showed that c was concurrently associated with depression symptoms, higher negative affect (NA), lower positive affect (PA), and higher anxious arousal symptoms; c also prospectively predicted depression episode onset. The common cognitive risk factor was also moderately associated with both the general psychopathology factor (p factor) and the externalizing-specific dimension (β’s=.33 and .42, respectively). That the general c factor related most potently to internalizing-specific is expected and consistent with the original theories of these cognitive risks. These risks originated theoretically to explain depression, in particular (Beck, 1976; Abramson, et al., 1989; Blatt & Zuroff, 1992; Nolen-Hoeksema & Morrow, 1991), and research on these vulnerabilities then expanded to investigate co-occurring anxiety syndromes as well as broad internalizing problems (Hankin et al., 2016b).
These results add important information about the construct validity of c in terms of relations with important psychopathological outcomes in a nomological network. Of particular interest, findings suggest that c is particularly strongly associated with the internalizing-specific dimension, whereas other studies investigating associations between latent dimensions of the bifactor model of psychopathology and other risks generally find associations of equal or stronger magnitude for p relative to specific psychopathology dimensions (Caspi et al., 2014; Castellanos-Ryan et al., 2016; Hankin, 2019; Hankin et al., 2017; Olino et al., 2014; Snyder, Hankin, Sandman, Head, & Davis, 2017; Snyder, Hankin, & Young, 2017; Hamlat et al., 2018).
The C Factor as General Cognitive Vulnerability: Meaning and Utility
Taken together, these results enhance understanding of the core essence of c. As a latent variable, the general cognitive risk factor (c) represents what is in common across all manifest measures of cognitive vulnerabilities, but this statistical abstraction of a latent variable does not clearly characterize the meaning of c. To advance understanding of the meaning and utility of c, we first consider the factor loadings of measured cognitive risks; later in the Discussion we return to clinical translational implications to further elaborate the potential utility and meaning of c. The strongest factor loadings onto c were for self-criticism followed by dysfunctional attitudes, dependency, negative inferential style and brooding, and nearly all loadings demonstrated comparable strength3. This suggests that a particularly salient feature of c could be a tendency to have negative self-evaluations, perfectionistic standards and contingent self-worth. Other features of c likely include having a pessimistic view of the future, and dwelling on negative content about the self, past experiences, and future expectations. Key themes across loadings reflect a tendency to hold overly negative beliefs about the self, and to experience a pervasive negative self-referential focus. These themes are likely reflected across units of analysis (e.g., genetic, neural, immunological, behavioral), and expanding the knowledge base to illuminate how core cognitive vulnerability relates to other units of analysis remains an important area for future inquiry.
With these cognitive features in mind as markers that characterize the core of c, the utility of this general cognitive vulnerability, and the bifactor modeling approach of cognitive risks, becomes clearer. It is important to consider that the bifactor model of cognitive risks more parsimoniously represented the pattern of associations with latent psychopathology dimensions as compared to the traditional conceptual, analytical approach of examining each individual cognitive risk, separately, in relation to clinical outcomes. More specifically, each individual cognitive risk related strongly with the internalizing-specific dimension (β’s ranging from .67 to .87) and moderately to weakly with the p factor (β’s ranging from .26 to .37) and the externalizing specific dimension (β’s ranging from .25 to .46). The c factor captures the breadth and potency of these “many-to-many” cognitive risk and psychopathology associations in a simpler, more succinct, and coherent model, as seen with the effect sizes between c and the internalizing-specific dimension (β=.86), p factor (β=.33), and externalizing-specific dimension (β=.42).
Thus, the bifactor model of cognitive risk demonstrates incremental utility over the traditional approach to studying cognitive vulnerability. As such, the c factor as a general dimension representing broad cognitive susceptibility to psychopathology holds promise to advance theory and clinical scientific knowledge on cognitive vulnerability models of psychopathology. C focuses attention on central, unifying features across cognitive risks that can confer liability to psychopathology, in a simpler and graded manner (i.e., most potent effects for what is specific to internalizing problems). In addition, the present study highlights that c is most strongly associated with the internalizing-specific dimension, suggesting that an important feature of this dimension includes a confluence of maladaptive thought patterns.
Specific Cognitive Risk Dimensions
After accounting for the general cognitive dimension in the bifactor model, specific latent cognitive risk factors that are independent of c, were identified (for brooding, dependency, negative inferential style). These transdiagnostically associated with all dimensions of psychopathology, and these links varied in terms of breadth and potency depending on the unique cognitive risk and outcome. First, the brooding-specific dimension exhibited comparable links to p and the internalizing-specific and externalizing-specific factors. This finding is consistent with theory and research suggesting that perseverative thinking tendencies are broadly transdiagnostic across many forms of psychopathology (e.g., related to p) and can take different forms depending on the nature of the cognitive and emotional content (e.g., sadness and threat for internalizing; anger in externalizing; Nolen-Hoeksema & Watkins, 2011).
Second, the negative inferential style-specific dimension was associated with the internalizing-specific and externalizing-specific dimensions, but not the p factor. The relation with the internalizing-specific dimension aligns with prior work implicating negative inferential style in internalizing outcomes (e.g., depression, social anxiety, and especially comorbid depression and anxiety; Alloy et al., 2006). Of interest and a novel finding is the association with the externalizing-specific dimension. Past work has shown links between negative cognitive style and conduct problems (Rowe, Maughan, & Eley, 2006). However, the unique association between negative inferential style-specific and the externalizing-specific dimension, after removing the general psychopathology and general cognitive risk covariation (p and c factors), has not been previously investigated. One possible explanation for this finding is that the negative inferential style-specific factor may be tapping a maladapative attributional process that relates specifically to both unique internalizing and externalizing problems. Considerable past research shows that children with a hostile attribution bias, or the tendency to attribute hostile intent to others in ambiguous provocation situations, are more likely to exhibit externalizing behaviors (Dodge, 2006). Alternatively, making negative attributions and inferences (self, consequences) can relate to aggression and externalizing problems within the context of interpersonal disputes (Berg et al., 2019). Individuals who experience frequent, verbal quarrels, such as that tapped by the externalizing-specific dimension, might attribute these interpersonal problems to stable, global causes (“I get into fights all the time”), believe their self is flawed (“There is something wrong with me”), and infer negative consequences for the future (“I will never have healthy relationships”). Future work could examine these possibilities.
Last, the dependency-specific factor exhibited negative associations to p and the externalizing-specific dimensions. Though perhaps initially surprising, this result aligns with prior work showing that the dependency-specific dimension was associated with lower concurrent depressive symptoms (Schweizer et al., 2018) and is consistent with the idea that some psychosocial risks, especially dependency, contain both maladaptive and adaptive elements (Zuroff, Mongrain, & Santor, 2004). On one hand, dependency includes maladaptive elements such as excessive fears of abandonment and loneliness and is associated with depression and interpersonal problems (Fichman et al., 1994). On the other hand, it also includes increased motivation to be close to others and is associated with agreeableness, support seeking, and intimacy in close relationships, which could be adaptive in some contexts (Priel & Shahar, 2000; Fichman et al., 1994). Findings suggest that c subsumes and characterizes the maladaptive aspects of dependency that co-occur with other cognitive risks, whereas the specific-dependency variance may reflect the unique, potentially adaptive aspects of having close relationships and support.
Translational Implications of the C Factor
Findings shed light on the breadth and potency of how transdiagnostic cognitive risks contribute to different psychopathological dimensions, and as such, have implications for enhancing the precision and parsimony of evidence-based assessment and intervention. In terms of assessment, in contrast to the traditional conceptualization and measurement of cognitive risk as distinct constructs that should be measured with separate instruments, results suggest that a bifactor model of cognitive vulnerabilities can integrate these risks into a unified model. The bifactor model could be utilized to help develop a single, unifying instrument that includes the items that best represent the different dimensions of cognitive risk, particularly c. This briefer assessment would be less time-intensive and burdensome for clinicians and clients to complete compared to the present practice of administering several separate measures of cognitive risks (e.g., dysfunctional attitudes, rumination, negative cognitive style, etc.).
Regarding intervention, results showed that the c factor is associated with a breadth of psychopathologies and may be a common element that contributes transdiagnostically to multiple manifestations of psychopathology. Indeed, maladaptive cognitive thinking patterns including overly critical, irrational, distorted cognitions are seen across multiple manifestations of psychopathology (e.g., hopelessness and worthlessness in depression; irrational fears and catastrophizing in some anxiety disorders; altered cognitions about the self and world in PTSD; hostile attributions in aggressive behavior). Interventions targeting c could be particularly helpful in disrupting and correcting these noxious cognitions that commonly contribute to risk across psychopathology. Various psychotherapies have been shown to be effective transdiagnostically for multiple disorders, and these effects may occur because the interventions are targeting common cognitive risk, or the c factor. Explicit transdiagnostic therapies (Harvey & Watkins, 2004) that focus on broader cognitive processes, such as illogical thinking and distorted perceptions likely target c. Transdiagnostic cognitive behavioral therapy programs (TD-cCBT) that focus on reducing several negative cognitions to improve anxiety and depression symptoms provide evidence for improvement in anxiety, depression and quality of life (Newby, Twomey, Li & Andrews, 2016). It is possible that such interventions may be directly targeting c, although future research is needed to study this hypothesis directly.
Limitations and Future Directions
Limitations of the current study point to avenues for future work. First, cognitive risks and psychopathology were examined cross-sectionally. Future work should examine relations using prospective, longitudinal designs to establish temporal ordering. Second, some have proposed that bifactor models overfit data (Bonifay, Lane, & Reise, 2017). To address this concern, we did not solely rely on model fit statistics to evaluate the bifactor model. We compared the bifactor model to an alternative correlated factors model, investigated the construct validity of the bifactor model by examining relations with external validators (i.e., dimensions of psychopathology) (Cronbach & Meehl, 1955), and examined how patterns with outcomes that were identified with the bifactor model compared to patterns with outcomes that were identified for each cognitive risk factor, considered individually, in relation to each dimension of psychopathology. Third, we utilized self-report methods for cognitive risks. However, we used self and caregiver reports to measure psychopathology, which reduces concerns about inflated effects due to mono-informant bias. Self-reports (e.g., cognitive risks) are valid and useful for measuring mental health and risk processes (Samuel, Suzuki, & Griffin, 2016). Even so, future studies should use multiple methods across units of analysis to capture additional information about cognitive risk processes that is not reflected via self-report, and to further examine the construct validity of the bifactor model of cognitive risk. Lastly, the present study utilized a community sample of youth; future work should examine if the same cognitive risk structure and associations with psychopathological outcomes emerge for other samples, including those of different ages and clinical status.
Conclusion
Risks can be better understood as being broadly transdiagnostic and relatively specific to different psychopathologies. By organizing both risks and psychopathological outcomes using latent dimensional bifactor models that parse out and organize the common and unique aspects of both constructs, the patterns of associations between common and specific latent factors of risk and psychopathology can be examined for breadth (i.e., multitude of relations) and potency (i.e., magnitude of relations). This knowledge can advance understanding for transdiagnostic risk, etiology, assessment, and intervention. We replicated a bifactor model that organizes multiple cognitive risks into fewer dimensions, including a common cognitive risk factor (c factor) and multiple specific dimensions in youth. The bifactor model of cognitive risks captured key associations that were identified when each individual cognitive risk was related to the bifactor model of psychopathology. C demonstrated transdiagnostic links to the breadth of psychopathology (connections to the p factor, internalizing-specific, externalizing-specific), with a particularly potent association with what is uniquely shared among internalizing syndromes (internalizing-specific). Transdiagnostic interventions that focus on broader maladaptive cognitive processes, such as overly negative, illogical, distorted perceptions, could help prevent and reduce suffering and distress among youth.
Supplementary Material
Public Health Significance Statement:
A common cognitive vulnerability representing general maladaptive thinking patterns (e.g., overly negative, self-focused beliefs) related to a breadth of mental health problems (depression, anxiety, aggression, conduct, attention issues), and particularly to symptoms that are specific to depression and anxiety among youth. This common cognitive vulnerability may be a transdiagnostic risk that informs transdiagnostic interventions.
Acknowledgments
The research reported in this article was supported by grants from the National Institute of Mental Health to Benjamin L Hankin, R01MH077195, R01MH105501, R01MH109662, and to Jami F. Young, R01MH077178.
Footnotes
The authors declare that they have no conflict of interest.
The significance of item loadings was tested by setting the factor variance to 1. The significance of factor variances were tested by setting the first item loading to 1. Model fit remains constant across both of these parameterizations.
As in the current study, Schweizer and colleagues (2018) also found support for specific dimensions for brooding, negative inferential style and dependency, and did not find evidence for specific self-criticism. One small discrepancy between the current study and this prior study is that a specific dysfunctional attitudes factor was not obtained in the present study; rather, all dysfunctional attitudes indicators were fully subsumed by c. This difference may be due to each study using a different measure of dysfunctional attitudes. Schweizer et al. (2018) utilized 9 items from the Dysfunctional Attitudes Scale (Weissman & Beck, 1978) whereas the present study utilized 20 items from the Children’s Dysfunctional Attitudes Scale (D’Alessandro & Abela, 2000).
Average standardized loadings for each subset of cognitive risk measure indicators onto the c factor were as follows: CDEQ-self-criticism=.73, CDAS=.64, CDEQ-dependency=.59, ACSQ=.56, and CRSQ-brooding =.55.
On average, all youth participants were 13.58 years old (SD=2.37, range=9.27–17.53). Each of the initial 3rd, 6th, and 9th grade cohorts were at the following developmental stages at the 18-month follow-up: late childhood (n=174, M=10.64, SD=0.51, range=9.27–11.73), early adolescence (n=213, M=13.52, SD=0.55, range=12.28–15.77), and late adolescence (n =182, M=16.64, SD=0.50, range=15.15–17.53).
Contributor Information
Tina H. Schweizer, University of Illinois at Urbana-Champaign
Hannah R. Snyder, Brandeis University
Jami F. Young, Children’s Hospital of Philadelphia, University of Pennsylvania Perelman School of Medicine
Benjamin L. Hankin, University of Illinois at Urbana-Champaign
References
- Abela JR, Brozina K, & Haigh EP (2002). An examination of the response styles theory of depression in third-and seventh-grade children: A short-term longitudinal study. Journal of Abnormal Child Psychology, 30(5), 515–527. [DOI] [PubMed] [Google Scholar]
- Abela JR, & Hankin BL (2008). Cognitive vulnerability to depression. Handbook of depression in children and adolescents, 35–78. [Google Scholar]
- Abela JRZ, & Sullivan C (2003). A Test of Beck’s Cognitive Diathesis-Stress Theory of Depression in Early Adolescents. The Journal of Early Adolescence, 23(4), 384–404. [Google Scholar]
- Abela JRZ, & Taylor G (2003). Specific vulnerability to depressive mood reactions in schoolchildren: the moderating role of self-esteem. Journal of Clinical Child and Adolescent Psychology 32(3), 408–418. [DOI] [PubMed] [Google Scholar]
- Abramson LY, Metalsky GI, & Alloy LB (1989). Hopelessness depression: A theory-based subtype of depression. Psychological Review, 96(2), 358–372. [Google Scholar]
- Achenbach T., & Rescorla LA (2001). Manual for the Achenbach system of empirically based assessment school-age forms profiles. Burlington, VT: Aseba. [Google Scholar]
- Adams P, Abela JRZ, & Hankin BL (2007). Factorial categorization of depression-related constructs in early adolescents. Journal of Cognitive Psychotherapy, 21(2), 123–139. [Google Scholar]
- Alloy LB, Abramson LY, Whitehouse WG, Hogan ME, Panzarella C, & Rose DT (2006). Prospective incidence of first onsets and recurrences of depression in individuals at high and low cognitive risk for depression. Journal of abnormal psychology, 115(1), 145. [DOI] [PubMed] [Google Scholar]
- Alloy LB, Black SK, Young ME, Goldstein KE, Shapero BG, Stange JP, … Abramson LY (2012). Cognitive vulnerabilities and depression versus other psychopathology symptoms and diagnoses in early adolescence. Journal of Clinical Child & Adolescent Psychology, 41, 539–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamini Y, Krieger AM, & Yekutieli D (2006). Adaptive Linear Step-up Procedures That Control the False Discovery Rate. Biometrika, 93(3), 491–507. [Google Scholar]
- Berg MT, Rogers EM, Liu W, Mumford EA, & Taylor BG (2019). The interpersonal context of depression and violent behavior: A social psychological interpretation. Aggressive Behavior. [DOI] [PubMed] [Google Scholar]
- Blatt Sidney J., & Zuroff DC (1992). Interpersonal relatedness and self-definition: Two prototypes for depression. Clinical Psychology Review, 12(5), 527–562. [Google Scholar]
- Beck AT (1976). Cognitive therapy and the emotional disorders. New York, NY: International Universities Press. [Google Scholar]
- Bonifay W, Lane SP, & Reise SP (2017). Three concerns with applying a bifactor model as a structure of psychopathology. Clinical Psychological Science, 5(1), 184–186. [Google Scholar]
- Burnham KP, & Anderson DR (2003). Model selection and multimodel inference: A practical information-theoretic approach. New York, NY: Springer. [Google Scholar]
- Bussing R, Fernandez M, Harwood M, Hou W, Garvan CW, Swanson JM, & Eyberg SM (2008). Parent and Teacher SNAP-IV Ratings of Attention Deficit/Hyperactivity Disorder Symptoms: Psychometric Properties and Normative Ratings from a School District Sample. Assessment, 15(3), 317–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, & Moffitt TE (2018). All for one and one for all: Mental disorders in one dimension. American Journal of Psychiatry, 175(9), 831–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H, Israel S, … Moffitt TE (2014). The p Factor: One General Psychopathology Factor in the Structure of Psychiatric Disorders? Clinical Psychological Science : A Journal of the Association for Psychological Science, 2(2), 119–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castellanos-Ryan N, Brière FN, O’Leary-Barrett M, Banaschewski T, Bokde A, … Conrod P (2016). The Structure of Psychopathology in Adolescence and Its Common Personality and Cognitive Correlates. Journal of Abnormal Psychology, 125, 1039–1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen FF, West S, & Sousa K (2006). A Comparison of Bifactor and Second-Order Models of Quality of Life. Multivariate Behavioral Research, 41(2), 189–225. [DOI] [PubMed] [Google Scholar]
- Chen FF (2007). Sensitivity of goodness of fit indexes to lack of measurement invariance. Structural Equation Modeling, 14, 464–504. [Google Scholar]
- Cox BJ, Fleet C, & Stein MB (2004). Self-criticism and social phobia in the US national comorbidity survey. Journal of Affective Disorders, 82, 227–234 [DOI] [PubMed] [Google Scholar]
- Cronbach LJ, & Meehl PE (1955). Construct validity in psychological tests. Psychological Bulletin, 52, 281–302. [DOI] [PubMed] [Google Scholar]
- Dodge KA (2006). Translational science in action: Hostile attributional style and the development of aggressive behavior problems. Development and psychopathology, 18, 791–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis LK, & Rothbart MK (2001, April). Revision of the early adolescent temperament questionnaire. Poster presented at the 2001 SRCD meeting, Minneapolis, Minnesota. [Google Scholar]
- Fichman L, Koestner R, & Zuroff DC (1994). Depressive styles in adolescence: Assessment, relation to social functioning, and developmental trends. Journal of Youth and Adolescence, 23(3), 315–330. [Google Scholar]
- Garber J, Weiss B, & Shanley N (1993). Cognitions, depressive symptoms, and development in adolescents. Journal of Abnormal Psychology, 102, 47–57. [DOI] [PubMed] [Google Scholar]
- Gibb BE, & Coles ME (2005). Cognitive Vulnerability-Stress Models of Psychopathology: A Developmental Perspective In Development of Psychopathology: A Vulnerability-Stress Perspective (pp. 104–135). Thousand Oaks, CA: SAGE Publications, Inc. [Google Scholar]
- Gotlib IH, Lewinsohn PM, Seeley JR, Rohde P, & Redner JE (1993). Negative cognitions and attributional style in depressed adolescents: An examination of stability and specificity. Journal of Abnormal Psychology, 102(4), 607. [DOI] [PubMed] [Google Scholar]
- Hamlat EJ, Snyder HR, Young JF, & Hankin BL (2018). Pubertal Timing as a Transdiagnostic Risk for Psychopathology in Youth. Clinical Psychological Science, 7, 411–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL (2008). Stability of Cognitive Vulnerabilities to Depression: A Short-Term Prospective Multiwave Study. Journal of Abnormal Psychology, 117(2), 324–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL (2019). A choose your own adventure story: Conceptualizing depression in children and adolescents from traditional DSM and alternative latent dimensional approaches. Behaviour Research and Therapy, 118, 94–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL, & Abramson LY (2002). Measuring cognitive vulnerability to depression in adolescence: reliability, validity, and gender differences. Journal of Clinical Child and Adolescent Psychology, 31(4), 491–504. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Davis EP, Snyder H, Young JF, Glynn LM, & Sandman CA (2017). Temperament factors and dimensional, latent bifactor models of child psychopathology: Transdiagnostic and specific associations in two youth samples. Psychiatry Research, 252, 139–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL, Lakdawalla Z, Carter IL, Abela JRZ, & Adams P (2007). Are Neuroticism, Cognitive Vulnerabilities and Self–Esteem Overlapping or Distinct Risks for Depression? Evidence from Exploratory and Confirmatory Factor Analyses. Journal of Social and Clinical Psychology, 26(1), 29–63. [Google Scholar]
- Hankin BL, Snyder HR, Gulley LD, Schweizer TH,… Vasey MW (2016a). Understanding comorbidity among internalizing problems: Integrating latent structural models of psychopathology and risk mechanisms. Development and Psychopathology, 28, 987–1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BH, Snyder HR, & Gulley LD (2016b). Cognitive risks in developmental psychopathology In Cichetti D (Ed.), Developmental psychopathology: Maladaptation and psychopathology (Vol. 3, pp. 312–385). Hoboken, NJ: Wiley. [Google Scholar]
- Hankin BL, Young JF, Abela JR, Smolen A, Jenness JL, Gulley LD, … & Oppenheimer CW (2015). Depression from childhood into late adolescence: influence of gender, development, genetic susceptibility, and peer stress. Journal of Abnormal Psychology, 124(4), 803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey AG, & Watkins E (2004). Cognitive behavioural processes across psychological disorders: A transdiagnostic approach to research and treatment. Oxford University Press, [Google Scholar]
- Hong RY, & Cheung MW-L (2015). The structure of cognitive vulnerabilities to depression and anxiety: Evidence for a common core etiologic process based on a meta-analytic review. Clinical Psychological Science, 3(6), 892–912. [Google Scholar]
- Hong RY, Lee SSM, Tsai FF, & Tan SH (2017). Developmental trajectories and origins of a core cognitive vulnerability to internalizing symptoms in middle childhood. Clinical Psychological Science, 5, 299–315. [Google Scholar]
- Hu Li‐tze, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Joiner TE Jr., & Rudd MD (1996). Toward a categorization of depression-related psychological constructs. Cognitive Therapy and Research, 20, 51–68. [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, & Walters EE (2005). Lifetime Prevalence and Age-of-Onset Distributions of DSM-IV Disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593. [DOI] [PubMed] [Google Scholar]
- Klein DN, Dougherty LR, & Olino TM (2005). Toward Guidelines for Evidence-Based Assessment of Depression in Children and Adolescents. Journal of Clinical Child & Adolescent Psychology, 34(3), 412–432. [DOI] [PubMed] [Google Scholar]
- Kline RB (2010). Promise and pitfalls of structural equation modeling in gifted research In Methodologies for conducting research on giftedness (pp. 147–169). Washington, DC, US: American Psychological Association. [Google Scholar]
- Kline RB (2015). Principles and practice of structural equation modeling. Guilford. [Google Scholar]
- Kovacs M (1985). The children’s depression inventory. Psychopharmacology Bulletin, 21, 995–998. [PubMed] [Google Scholar]
- Lahey BB, Krueger RF, Rathouz PJ, Waldman ID, & Zald DH (2017). A hierarchical causal taxonomy of psychopathology across the life span. Psychological Bulletin, 143, 142–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakdawalla Z, Hankin BL, & Mermelstein R (2007). Cognitive theories of depression in children and adolescents: a conceptual and quantitative review. Clinical Child and Family Psychology Review, 10(1), 1–24. [DOI] [PubMed] [Google Scholar]
- Leadbeater BJ, Kuperminc GP, Blatt SJ, & Hertzog C (1999). A multivariate model of gender differences in adolescents’ internalizing and externalizing problems. Developmental Psychology, 35(5), 1268–1282. [DOI] [PubMed] [Google Scholar]
- Lee A, & Hankin BL (2009). Insecure attachment, dysfunctional attitudes, and low self-esteem predicting prospective symptoms of depression and anxiety during adolescence. Journal of Clinical Child & Adolescent Psychology, 38, 219–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little TD, Rhemtulla M, Gibson K, & Schoemann AM (2013). Why the Items versus Parcels Controversy Needn’t Be One. Psychological Methods, 18(3), 285–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- March JS, Parker JD, Sullivan K, Stallings P, & Conners CK (1997). The Multidimensional Anxiety Scale for Children (MASC): factor structure, reliability, and validity. Journal of the American academy of child & adolescent psychiatry, 36, 554–565. [DOI] [PubMed] [Google Scholar]
- Martel MM, Pan PM, Hoffmann MS, Gadelha A, do Rosário MC, Mari JJ, … Salum GA (2017). A general psychopathology factor (P factor) in children: Structural model analysis and external validation through familial risk and child global executive function. Journal of Abnormal Psychology, 126(1), 137–148. [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, & Nolen-Hoeksema S (2011). Rumination as a Transdiagnostic Factor in Depression and Anxiety. Behaviour Research and Therapy, 49(3), 186–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Wisco BE, Aldao A, & Hilt LM (2014). Rumination as a Transdiagnostic Factor Underlying Transitions Between Internalizing Symptoms and Aggressive Behavior in Early Adolescents. Journal of Abnormal Psychology, 123(1), 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller RO, & Hancock GR (2008). Best Practices in Structural Equation Modeling In Osborne J, Best Practices in Quantitative Methods. SAGE Publications. [Google Scholar]
- Muthén LK, & Muthén BO (2012). Mplus statistical modeling software: Release 7.0. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Newby JM, Twomey C, Li SSY, & Andrews G (2016). Transdiagnostic computerised cognitive behavioural therapy for depression and anxiety: a systematic review and meta-analysis. Journal of Affective Disorders, 199, 30–41. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S (1991). Responses to depression and their effects on the duration of depressive episodes. Journal of Abnormal Psychology, 100(4), 569–582. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, & Watkins ER (2011). A Heuristic for Developing Transdiagnostic Models of Psychopathology: Explaining Multifinality and Divergent Trajectories. Perspectives on Psychological Science, 6(6), 589–609. [DOI] [PubMed] [Google Scholar]
- Olino TM, Bufferd SJ, Dougherty LR, Dyson MW, Carlson GA, & Klein DN (2018). The Development of Latent Dimensions of Psychopathology across Early Childhood: Stability of Dimensions and Moderators of Change. Journal of Abnormal Child Psychology, 46(7), 1373–1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olino TM, Dougherty LR, Bufferd SJ, Carlson GA, & Klein DN (2014). Testing models of psychopathology in preschool-aged children using a structured interview-based assessment. Journal of Abnormal Child Psychology, 42(7), 1201–1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Priel B, & Shahar G (2000). Dependency, self-criticism, social context and distress: comparing moderating and mediating models. Personality and Individual Differences, 28(3), 515–525. [Google Scholar]
- Reno RM, & Halaris AE (1989). Dimensions of depression: A comparative longitudinal study. Cognitive Therapy and Research, 13, 549–563. [Google Scholar]
- Rowe R, Maughan B, & Eley TC (2006). Links between antisocial behavior and depressed mood: The role of life events and attributional style. Journal of Abnormal Child Psychology, 34(3), 283–292. [DOI] [PubMed] [Google Scholar]
- Rucklidge J, Brown D, Crawford S, & Kaplan B (2007). Attributional styles and psychosocial functioning of adults with ADHD: Practice issues and gender differences. Journal of Attention Disorders, 10(3), 288–298. [DOI] [PubMed] [Google Scholar]
- Samuel DB, Suzuki T, & Griffin SA (2016). Clinicians and clients disagree: Five implications for clinical science. Journal of Abnormal Psychology, 125(7), 1001–1010. [DOI] [PubMed] [Google Scholar]
- Schweizer TH, Snyder HR, & Hankin BL (2018). A reformulated architecture of cognitive risks: Common and specific factors and links to internalizing outcomes in adolescence. Assessment. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HR, Gulley LD, Bijttebier P, Hartman CA, Oldehinkel AJ, Mezulis A, … Hankin BL (2015). Adolescent emotionality and effortful control: Core latent constructs and links to psychopathology and functioning. Journal of Personality and Social Psychology, 109(6), 1132–1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HR, Hankin BL, Sandman CA, Head K, & Davis EP (2017). Distinct patterns of reduced prefrontal and limbic grey matter volume in childhood general and internalizing psychopathology. Clinical Psychological Science: A Journal of the Association for Psychological Science, 5(6), 1001–1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HR, Young JF, & Hankin BL (2017a). Strong Homotypic Continuity in Common Psychopathology-, Internalizing-, and Externalizing-Specific Factors Over Time in Adolescents. Clinical Psychological Science, 5(1), 98–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HR, Young JF, & Hankin BL (2017b). Chronic Stress Exposure and Generation Are Related to the P-Factor and Externalizing Specific Psychopathology in Youth. Journal of Clinical Child and Adolescent Psychology, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swanson JM, Kraemer HC, Hinshaw SP, Arnold LE, Conners CK, Abikoff HB, … & Hechtman L (2001). Clinical relevance of the primary findings of the MTA: success rates based on severity of ADHD and ODD symptoms at the end of treatment. Journal of the American Academy of Child & Adolescent Psychiatry, 40(2), 168–179. [DOI] [PubMed] [Google Scholar]
- Waldman ID, Poore HE, van Hulle C, Rathouz PJ, & Lahey BB (2016). External validity of a hierarchical dimensional model of child and adolescent psychopathology: Tests using confirmatory factor analyses and multivariate behavior genetic analyses. Journal of Abnormal Psychology, 125(8), 1053–1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman AN, & Beck AT (1978). Development and Validation of the Dysfunctional Attitude Scale: A Preliminary Investigation. [Google Scholar]
- Zuroff DC, Mongrain M, & Santor DA (2004). Conceptualizing and measuring personality vulnerability to depression: comment on Coyne and Whiffen (1995). Psychological Bulletin, 130(3), 489–511; discussion 512–22. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


