Abstract
Introduction:
COVID-19 is the disease caused by an infection of the SARS-CoV-2 virus, first identified in the city of Wuhan, in China’s Hubei province in December 2019. COVID-19 was previously known as 2019 Novel Coronavirus (2019-nCoV) respiratory disease before the World Health Organization (WHO) declared the official name as COVID-19 in February 2020.
Aim:
The aim of this study is to search scientific literature in the biomedicine and analyzed current results of investigations regarding morbidity and mortality rates as consequences of COVID-19 infection of Cardiovascular diseases (CVD), and other most common chronic diseases which are on the top mortality and morbidity rates in almost all countries in the world. Also, to propose most useful measures how to prevent patients to keep themselves against COVID-19 infection.
Methods:
We used method of descriptive analysis of the published papers with described studies about Corona virus connected with CVD, and, also, Guidelines proposed by World Health Organization (WHO) and European Society of Cardiology (ESC), and some other international associations which are included in global fighting against COVID-19 infection.
Results:
After searching current scientific literature we have acknowledged that not any Evidence Based Medicine (EBM) study in the world during last 5 months from the time when first cases of COVID-10 infection was detected. Also, there is no unique proposed ways of treatments and drugs to protect patients, especially people over 65 years old, who are very risk group to be affected with COVID-19. Expectations that vaccine against COVID-19 will be produced optimal during at least 10 months to 2 years, and in all current Guidelines most important proposed preventive measures are the same like which one described in Strategic documents of WHO, in statements of Declaration of Primary Health Care in Alma Ata in 1978.
Conclusion:
WHO proposed preventive measures can be helpful to everybody. Physicians who work at every level of Health Care Systems, but especially at primary health care level, must follow those recommendations and teach their patients about it. But, the fact is that current focus of COVID-19 epidemic has targeted on protection of physical health of population in global, however, the influence on mental health which will be one of the important consequences of COVID-19 pandemic in the future, and which could be declared as «Post-coronavirus Stress Syndrome„ (PCSS) could be bigger challenge for Global Public Health.
Keywords: COVID-19, CVDs, Chronic diseases, Public health, Post-coronavirus Stress Syndrome - PCSS, WHO Guidelines
1. INTRODUCTION
COVID-19 is the disease caused by an infection of the SARS-CoV-2 virus, first identified in the city of Wuhan, in China›s Hubei province in December 2019. COVID-19 was previously known as 2019 Novel Coronavirus (2019-nCoV) respiratory disease before the World Health Organization (WHO) declared the official name as COVID-19 in February 2020. A new respiratory disease - Coronavirus disease 2019 (COVID-19) - is spreading globally and there have been instances of COVID-19 community spread in the United States. COVID-19 spreads by contact with respiratory droplets that spread when an infected person coughs or sneezes. Respiratory virus infection is a major source of global pandemics as a consequence of swift human-to-human respiratory tract transmission. Within the past two decades, coronaviruses and influenza viruses have hit the world several times, causing significant mortality, economic loss, and global panic. The SARS outbreak in 2002 triggered 916 deaths among more than 8000 patients in 29 countries, followed by the emergence of MERS in 2012, which resulted in at least 800 deaths among 2254 patients in 27 countries (1). Besides coronaviruses, avian and swine influenza remain a concern for global public health in the 2009 H1N1 pandemic alone, there were 18 500 laboratory-confirmed deaths and more than 200.000 deaths from respiratory disease worldwide (2).
In late 2019, a cohort of patients presenting with pneumonia of varying acuity and unknown aetiology in Wuhan, China, heralded the outset of COVID-19. As of 30.03.2020, total of 770,165 confirmed cases (including 36,938 deaths in 152 geographical territories) have been reported to the WHO, and this number is still increasing. Although COVID-19 appears to have greater infectivity and lower mortality than SARS and MERS, many uncertainties (including route of infection, viral evolution, epidemic dynamics, appropriate anti-viral treatment, and strategies for disease control) remain. On March 11, 2020, the WHO declared COVID-19 a pandemic (3). Since there is no cure for this viral disease and a long wait is needed to find a vaccine, a rigorous epidemiological measure was first taken. The largest quarantine in history was made, between 50 and 60 million people in several Chinese cities were quarantined; which included necessary hygiene measures, group meetings were canceled, schools closed, and travel banned. Some believe that a later evaluation of all the more modern epidemiological measures will show whether all of them are justified, as experts point to procedures that curb a Severe Acute Respiratory Syndrome (SARS) caused by another type of virus Corona.
2. CONSEQUENCES OF COVID-19 ON CVD AND OTHER COMMON CHRONIC DISEASES
Cardiovascular complications of influenza infection, including myocarditis, acute myocardial infarction, and exacerbation of heart failure have been well-recognized during previous historical epidemics and make a significant contribution to mortality (4). Likewise, previous corona-virus outbreaks have been associated with a significant burden of cardiovascular comorbidities and complications. Furthermore, the severity of the primary respiratory syndrome and risk of adverse outcomes is increased in patients with pre-existing cardiovascular diseases (5, 6). Hypotension, tachycardia, bradycardia, arrhythmia, or even sudden cardiac death are common in patients with SARS. Electrocardiographic changes and troponin elevation may signal underlying myocarditis, and echocardiography frequently demonstrates subclinical left ventricular diastolic impairment (with a higher likelihood of the need for mechanical ventilation in those with systolic impairment and reduced ejection fraction) (7, 8).
Early COVID-19 case reports suggest that patients with underlying conditions are at higher risk for complications or mortality - up to 50% of hospitalized patients have a chronic medical illness (40% cardiovascular or cerebrovascular disease). In the largest published clinical cohort of COVID-19 to date, acute cardiac injury, shock, and arrhythmia were present in 7.2%, 8.7%, and 16.7% of patients, respectively (9), with higher prevalence amongst patients requiring intensive care. CVDs may become unstable in the setting of viral infection as a consequence of imbalance between infection-induced increase in metabolic demand and reduced cardiac reserve. Patients with coronary artery disease and heart failure may be at particular risk as a result of coronary plaque rupture secondary to virally induced systemic inflammation, and rigorous use of plaque stabilizing agents (aspirin, statins, beta-blockers, and angiotensin-converting enzyme inhibitors) has been suggested as a possible therapeutic strategy. Pro-coagulant effects of systemic inflammation (10) may increase the likelihood of stent thrombosis and assessment of platelet function and intensified anti-platelet therapy should be considered in those with a history of previous coronary intervention.
The clinical effects of pneumonia have been linked to increased risk of CVD up to 10-year follow-up (11) and it is likely that cases infected via respiratory virus outbreaks will experience similar adverse outcomes. Therapeutic use of corticosteroids further augments the possibility of adverse cardiovascular events. However, long-term follow-up data concerning the survivors of respiratory virus epidemics are scarce. Lipid metabolism remained disrupted 12 years after clinical recovery in a metabolomic study amongst 25 SARS survivors (12), whereas cardiac abnormalities observed during hospitalisation in eight patients with H7N9 influenza returned to normal at 1-year follow-up (13). Whilst viral phenotype, baseline clinical characteristics, initial disease severity, and immediate management impact on short-term survival, long-term prognosis following outbreaks of respiratory virus infection may equally depend upon the extra-pulmonary manifestations. Serial follow-up studies amongst the survivors of acute infection are surely needed.
Autopsy findings of deaths due to infection with the new virus (COVID-19) revealed that mortality was lower in pulmonary patients compared to cardiac patients or patients with diabetes, and mortality of hypertensive patients was similar to that in lung patients. Doctors quickly looked to see if any of the existing medicines were leading to an improvement in their condition. First, Chinese experts have shown that the antimalarial drug (chloroquine) is effective in patients. Then, a few days ago, French researchers showed in a very small group of patients that the concomitant administration of hydroxychloroquine and azithromycin (Sumamed) had an even better effect in COVID-19 patients. Although these studies are insufficient (due to small sample size and poor clinical experimental design), they indicate that, despite the adverse effects of Azithromycin (severe diarrhea due to Clostridium difficile and prolonged QT interval on ECG), mortality due to infection with a new virus. It should be noted that in 1980, researchers at the PLIVA drug factory found a macrolide antibiotic, Azithromycin, but sold all distribution rights to the European Community and the US in 1986 to Pfizer (14).
Some pharmacologists believe that because certain growth-inhibiting agents, such as Cepharanthin, Selamectin or Mefloquine hydrochloride, affect replication of coronaviruses in vitro, these agents might be used to treat COVID-19 infection in vivo, but it will first be necessary to check their clinical efficacy of Cepharanthin (an ingredient in the local plant Stephania cephalantha) has been used in Japan since almost 70 years ago for a number of acute and chronic diseases because it has various pharmacological effect including anti-inflamatory, anticancer, and antiviral effects (15). There is a considerable debate among biomedical scientists and physicians as to whether patients should stop taking ACE inhibitors (ACEI: Enalapril, Lisinopril, Ramipril and others) and angiotensin receptor blocking drugs (ARB: Losartan, Eprosartan, Valsartan and others) due to their increase of ACE-2 activity and rise of the ACE-2 receptors (16). These drugs help thousands of patients with high blood pressure, chronic heart failure, diabetic kidney damage and other vascular disorders (17). Discontinuing these medicines could have many serious consequences, although medical opinions remain divided (18). On the one hand, there is an indication that these renin-angiotensin blockers could exacerbate coronavirus disease, but on the other hand, some preliminary data show that they are beneficial (19). Controlled clinical trials will establish whether these drugs should be temporarily discontinued (and in which patients) or whether they should even be given to individuals infected with COVID-19. For now, no one should omit taking any of these medicines.
The European Medicines Agency (EMA) has issued a statement advising that patients continue treatment with angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs), despite widely circulated reports that the agents could worsen coronavirus disease (20). “It is important that patients do not interrupt their treatment with ACE inhibitors or ARBs and there is no need to switch to other medicines”, the agency said today. “There is currently no evidence from clinical or epidemiological studies that establishes a link between ACE inhibitors or ARBs and the worsening of COVID-19”.
The new guidance is in line with that recently issued by the European Society of Cardiology and three American cardiology societies. The medications are commonly used by patients with hypertension, heart failure, and kidney disease. Because the coronavirus infects human cells by binding to ACE2 receptors and because these medicines can increase ACE2, it has been suggested that they could increase virus activity. However, the interactions of the virus with the renin-angiotensin-aldosterone system in the body are complex and are not completely understood, the agency notes. “The speculation that ACE-inhibitors or ARBs treatment can make infections worse in the context of COVID-19 is not supported by clinical evidence”, the EMA reiterated. Although not noted in the statement, other reports have suggested that ACE inhibitors and ARBs may reduce the risk for or severity of viral pneumonia in patients with COVID-19 infection, or may actually have potential as treatments. The EMA is collaborating with stakeholders to generate further evidence in epidemiologic studies on the effects of ACE inhibitors and ARBs in people with COVID-19 (20). In light of circulating reports questioning whether nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, also could worsen COVID-19, the agency also recently issued guidance on the use of NSAIDs during the pandemic.
The EMA highlighted that most ibuprofen-containing medicines in the EU are authorised at national level, as a painkiller and in some countries also as an antipyretic (fever treatment medicine). They are widely available over the counter and on prescription. Oral Ibuprofen (over the counter or with a prescription) is used, depending on the presentation, in adults, children and infants from the age of three months, for the short-term treatment of fever and/or pain such as headaches, flu, dental pain and dysmenorrhoea (period pain). Ibuprofen is also prescribed for the treatment of arthritis and rheumatic conditions. Ketoprofen is a similar medicine, mostly prescribed for use in various painful and inflammatory conditions although in some Member States it is available over the counter. Ibuprofen has also been authorised centrally as Pedea to treat ‘patent ductus arteriosus’ in newborn premature babies (20).
The EMA highlighted the need for future epidemiologic studies and stated: “There is currently no scientific evidence establishing a link between ibuprofen and worsening of COVID-19”. There is currently no scientific evidence establishing a link between ibuprofen and worsening of COVID-19. EMA is monitoring the situation closely and will review any new information that becomes available on this issue in the context of the pandemic (20).
In May 2019, EMA’s safety committee (PRAC) started a review of the non-steroidal anti-inflammatory medicines ibuprofen and ketoprofen following a survey by the French National Agency for Medicines and Health Products Safety (ANSM) which suggested that infection due to chickenpox (varicella) and some bacterial infections could be made worse by these medicines. The product information of many NSAIDs already contains warnings that their anti-inflammatory effects may hide the symptoms of a worsening infection. The PRAC is reviewing all available data to see if any additional measure is required (20). When starting treatment for fever or pain in COVID-19, patients and healthcare professionals should consider all available treatment options including paracetamol and NSAIDs. Each medicine has its own benefits and risks which are reflected in its product information and which should be considered along with EU national treatment guidelines, most of which recommend paracetamol as a first treatment option for fever or pain (20). In line with EU national treatment guidelines, patients and healthcare professionals can continue using NSAIDs (like Ibuprofen) as per the approved product information. Current advice includes that these medicines are used at the lowest effective dose for the shortest possible period.
Further to the ongoing PRAC safety review on Ibuprofen and Ketoprofen, EMA highlights the need for epidemiological studies to be conducted in a timely manner to provide adequate evidence on any effect of NSAIDs on disease prognosis for COVID-19. The Agency is reaching out to its stakeholders and is ready to actively support such studies, which could be useful in guiding any future treatment recommendations. EMA will provide further information as necessary and once the PRAC review is concluded (20).
Public health aspects of protection patients with CVDs and patients with other most common chronic diseases against COVID-19 infection
For most people, the immediate risk of becoming ill with the virus that causes COVID-19 is considered low. Older adults and people of any age who have serious medical conditions may be at increased risk of serious complications from COVID-19 infection. However, the virus poses a particular risk for people over 65 and those with chronic illnesses including: cardiovascular disease, Hypertension, Diabetes, Chronic respiratory illness and Malignancies. According to the recently published COVID-19 Clinical Guidance for the cardiovascular care team, the overall case fatality rate (CFR) of COVID-19 based on published reports remains low at 2.3%, with data indicating lower overall Chinese mortality outside of the outbreak epicenter in Hubei, China. Beyond China, real-time reporting indicates CFRs between 2.7% (Iran) and 0.5% (South Korea); however, this information is provisional and likely to changi.
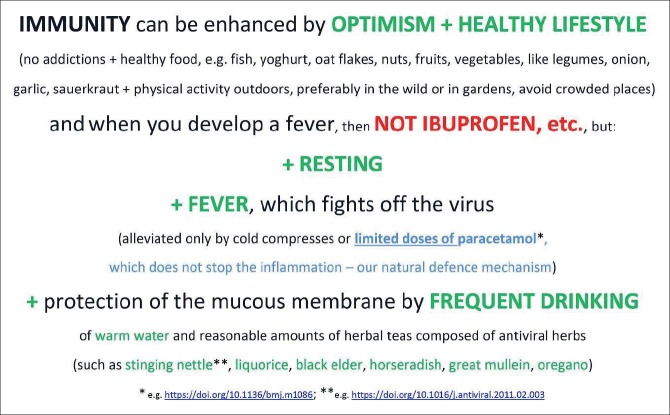
Figure 1. Poster with instructions of necessary hygienic-dietetic and traditional treatments to keep and improve immune system as measures for prevention againts COVID-19 infection. Poster is designed by Sylwia B. Ufnalska, biologist, MSc in Biology, EASE Council members, Editor of EASE Guidelines, Poznan, Poland. Authors thanks to Sylwia for permisson for use this poster in the text.
More than 80% of infected patients experience mild symptoms and recover without intensive medical intervention. However, morbidity and mortality increase significantly with age, rising to 8.0% among patients 70-79 and 14.8% in patients over 80 in large-scale Chinese case reporting. Published case reports from the Chinese Centers for Disease Control indicate patients with underlying comorbid conditions have a heighted risk for contracting COVID-19 and a worse prognosis; depending on the report, between 25% and 50% of COVID-19 patients present with underlying conditions. Case fatality rates for comorbid patients are materially higher than the average population: Cancer: 5.6%, Hypertension: 6.0%, Chronic respiratory disease: 6.3%, Diabetes: 7.3% and CVD: 10.5% (21-25).
During the SARS epidemics in 2003 and the MERS epidemic in 2012 caused by the SARS COV-1 virus, the course of the disease responded to acute respiratory viral infections, but a large number of patients had more severe forms of the disease followed by fatal outcome (26). Mortality was significantly higher in patients with chronic comorbid conditions. Impairment in the immune response to the virus led to severe respiratory failure, which was accompanied by alveo-capillary block due to the diffuse inflammation of the alveolar and vascular structures of the lung, as the body’s immune system activates proinflammatory mediators (cytokines and others) that cause block of the alveolar activation and surfactant inactivation. This condition is known as Acute Respiratory Distress Syndrome (ARDS) and requires the respirator application (26). Death is usually caused by the multiorgan dysfunction.
The current COVID-19 pandemic, also, caused by the Corona virus SARS COV-2, has clinical manifestations as in previous outbreaks, and the virus itself has great genetic similarity to the previous SARS COV-1. The current pandemic, however, has led to dramatic changes in the lives of every inhabitant of this planet, and the greatest challenges for each country public health and health care systems. Despite the genetic similarity, the new virus has other modes of transmission, and appears to have a greater ability to block an adequate immune response, leading to more severe forms of ARDS. After it causes respiratory symptoms, the virus infects all other organ systems (cardiovascular, hematopoietic, digestive, then the kidney, skin, CNS) through the blood (viremia) and can lead to multiorgan failure. The ACE 2 receptors, which are used by the virus to enter the cells of the respiratory system for reproduction, also have other organs, which can be affected at the very beginning of the disease. Such a condition can lead to an overreaction of the immune system with the production of a number of inflammatory mediators such as cytokines, and cause “cytokine storm” (27).
Patients with COVID-19 infection have, in addition to the symptoms of acute respiratory infection, clinical signs of other diseases. Cases with clinical presentation of active gastroenterocolitis with predominance of diarrhea and bleeding have been described. Initial autopsy and biopsy reports of various tissues indicate pathological changes in almost all organ systems. Blood tests of patients with COVID-19 almost always show haematological changes that indicate a disorder of coagulation and immunological status. A large percentage of patients have proven high levels of aminotransferases and it can be assumed that the liver is among the first organs attacked by the virus. The question of the future course of the disease remains unanswered, given the possibility of mutation. Patients with COVID-19 have short-term immunity, but there is the possibility of reinfection and persistent carriers of the virus (similar to B hepatitis positive) (26).
The current major challenge for public health is the comprehensive public health protection at the level of Community and Family Medicine units and their well-educated teams on the features, etiopathogenesis and spreading of COVID-19 infection, as well as all public health measures that have previously been applied in medical history during epidemics and pandemics of varying intensity, and there were many. Experiences from the past are recorded in various educational publications, but unfortunately long unused in the scope and seriousness of approaches and methods of their application, better said, neglected in practice, and the result of all the rapid and intensive application of technologies and pharmacological agents and drugs in the treatment of viral infections such as COVID-19. This global pandemic infection has just shown how dysplosion of the use of diagnostic and therapeutic technologies is relatively powerful to deal with and cope with the effects of a pandemic of this type or another, and how effectively their use can counteract its effects and make them as small and harmful as possible. Štampar’s Principles as well as the Principles of Arab scholars: Hunayin Ibn Ishaq (809-873), Ali Ibn At-Tabari ((808-861), Abdullah Ibn Sina (Avicenna, 980-1037), Ibn Butlan (-1068, philosopher and reformator of Public health), Alauddin Ibn Nafis (1210-1288), and other Arab physicians (40 days quarantine in case of epidemia has been described in Avicenna’s famous book “Canon of Medicine”) (28), as well as numerous other medical manuscripts during Arabic and the Ottoman period, which still exist in many libraries in our areas today, has clearly been the method of choice, as effective vaccines are still pending.
The lessons learned from these books have been passed on for centuries in Bosnia and Herzegovina by attars, scholars and qualified persons, most of them priests of all confessions in these areas. The same experiences are recorded in numerous manuscripts preserved in the auxiliary, but also rich libraries of Franciscan monasteries, mosques, synagogues, churches, and other dedicated objects.
The WHO’s recommendations are largely based on these preventive measures, the experience of which has been around for centuries. Unfortunately, the postulates of the Stampar’s “dispensary method” as screening method of work from the year 1923 (29) and orientation in prevention of epidemic and pandemic type emergence and spread - the effect of which proved to be very effective in Wuhan (China), where trained persons went door to door in flats and houses and sought infected, but also recorded the number of people with chronic diseases, potential for infection and possible lethal outcome. In this case the community and family play a key role in preventing the massive spread of COVID-19 infection demonstrated the importance and value of the public health approach just mentioned in addressing this global pandemic that has occupied the entire planet, and whose consequences in all spheres and forms of life and work are likely to make us think that this approach to organizing the health system and its most important segment - the family and its members, must have a better and more serious approach to health care. Because the question is how many such epidemics or pandemics will happen to us in the future – to us or our descendants.
Unfortunately, within the WHO’s recommendations, there is a somewhat sophisticated current focus on COVID-19 that has neglected, in practice, the appropriate treatment of a large number of patients with massive chronic non-communicable diseases, adhering to the principle of the many times the stated and declared strategic goals of „Health for all“. Twenty years ago, the first author of this article in an earlier article cited the motto – „technologies will dehumanize medicine in the near future“. It seems, as though, this is already happening, but the question is how well those who make decisions in health care systems are aware of this statement.
3. MOST IMPORTANT GUIDELINES FOR PREVENTION COVID-19 ON WEB SITES
The U.S. Centers for Disease Control and Prevention has developed interim guidance for businesses and employers to plan for and respond to COVID-19 (25). The interim guidance is intended to help prevent workplace exposures to acute respiratory illnesses, including COVID-19.
Older adults and those with underlying chronic medical conditions seem to be at higher risk, according to the CDC. As the illness is thought to spread from person to person, experts advise: Wear a mask if you are sick or caring for someone. Frequent hand washing, avoiding crowds and contact with sick people, and cleaning and disinfecting frequently touched surfaces can help prevent coronavirus infections are the main proposal of WHO experts. Those preventive measures at least can help to everybody, including also to patients who have evidenced CVDs in their histories of illness (25).
CDC: Protect yourself and others https://www.cdc.gov/coronavirus/2019-ncov/about/prevention-treatment.html
WHO: Advice for the public https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public
CDC: If you are at higher risk https://www.cdc.gov/coronavirus/2019-ncov/specific-groups/high-risk-complications.html.
WHO: How and when to use masks https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advicefor-public/when-and-how-to-use-masks.
The ESC has made available a resource library and video series on its COVID-19 and Cardiology webpage which is regularly updated. https://www.escardio.org/Education/COVID-19-and-Cardiology?
4. CONCLUSION
It is likely that SARS-CoV-2 will be identified in more communities, including areas where cases have not yet been reported. As such, phisycians who work at primary health care level should assume it could already be in their community and move to restrict all visitors form their home/flats or from the other facilities; cancel group activities and communal dining; and implement active screening of residents for fever and respiratory symptoms, especially older adults often with underlying chronic medical conditions, including patients with CVD, who are at the highest risk of being affected by COVID-19. COVID-19 spreads by contact with respiratory droplets that spread when an infected person coughs or sneezes. Frequent hand washing, avoiding crowds and contact with sick people, and cleaning and disinfecting frequently touched surfaces can help prevent coronavirus infections (22-24). The general strategies CDC recommends to prevent the spread of COVID-19 in LTCF are the same strategies these facilities use every day to detect and prevent the spread of other respiratory viruses like influenza (25). COVID-19 is being increasingly reported in communities across the World.
If they are infected with SARS-CoV-2, the virus that causes COVID-19, highest risk population are at increased risk of serious illness. Ill visitors and healthcare personnel (Epidemilogists, Family phisycians, Patronage nurses, Health care staff for testing risk population, Emergency health care medical professionals, Red Cross staff, etc) are the most likely sources of introduction of COVID-19 into a facility. WHO recommends aggressive visitor restrictions and enforcing sick leave policies for ill HCP, even before COVID-19 is identified in a community or facility. These recommendations are specific for nursing homes, including skilled nursing facilities. Much of this information could also be applied in assisted living facilities. This information complements, but does not replace, the general infection prevention and control recommendations for COVID-19 (25). Current guidance available on web sites (attached up in the text) are based on the currently available information about COVID-19. Probably it will be refined and updated as more information becomes available and as response needs change regarding experiences from almost all countries world wide, covered by WHO rules and recommendations ot the experts in this field. Experts of CDC in US concluded: „It is important to understand transmission dynamics in your community to inform strategies to prevent introduction or spread of COVID-19 in your facility. Consultation with public health authorities can help you better understand if transmission of COVID-19 is occurring in your community.“ (25). Unfortunately, publich health sector in our country is still limited to be effective like it was in previously organized Health Care System in former Yugoslavia with centralized „red and green“ lines of making decissions for every prevention tasks and measures from local communities to higest (national) level. Decision makers in healthcare sector of Bosnia and Herzegovina are „separated“ and very much influenced on the same way as political system, which has not definitely useful for common people - potenital patents or murderes of COVID-19 consequences in the future. Probaly we will stay on main goals for everybody: „stay at home and keep yourself“ and follow instructions how to use proposed and recommended preventive measures from public health experts, besides main act till now - testing of risk people and stay at home and improve your immunity system. Especially patients registered with CVD, Diabetes mellitus, cancers, and respiratory diseases.
But, the fact is that current focus of COVID-19 epidemic has targeted on protection of physical health of population in global, however, the influence on mental health which will be one of the important consequences of COVID-19 pandemic in the future, and which could be declared as «Post-coronavirus Stress Syndrome„ (PCSS) could be bigger challenge for Global Public Health.
Author’s contribution:
All authors contributed in the preparation of the manuscript and they were overseeing this contents of the article, had full access and responsibility of the data. Final proof reading was made by the first author.
Conflict of interest:
None declared.
Financial support and sponsorship:
Nil.
REFERENCES
- 1.Song Z, Xu Y, Bao L, Zhang L, Yu P, Qu Y, Zhu H, Zhao W, Han Y, Qin C. From SARS to MERS, thrusting coronaviruses into the spotlight. Viruses. 2019;11:E59. doi: 10.3390/v11010059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dawood FS, Iuliano AD, Reed C, Meltzer MI, Shay DK, Cheng PY, et al. Estimated global mortality associated with the first 12 months of 2009 pandemic influenza A H1N1 virus circulation: a modelling study. Lancet Infect Dis. 2012;12:687–695. doi: 10.1016/S1473-3099(12)70121-4. [DOI] [PubMed] [Google Scholar]
- 3.Xiong Tian-Yuan, Redwood Simon, Prendergast Bernard, Chen Mao. Coronaviruses and the cardiovascular system: acute and long-term implications. European Heart Journal. 2020;1:1–3. doi: 10.1093/eurheartj/ehaa231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nguyen JL, Yang W, Ito K, Matte TD, Shaman J, Kinney PL. Seasonal influenza infections and cardiovascular disease mortality. JAMA Cardiol. 2016;1:274. doi: 10.1001/jamacardio.2016.0433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khot WY, Nadkar MY. The 2019 Novel Coronavirus Outbreak–A Global Threat. J Assoc Physicians India. 2020;68:67–71. [PubMed] [Google Scholar]
- 6.Badawi A, Ryoo SG. Prevalence of comorbidities in the Middle East respiratory syndrome coronavirus (MERS-CoV): a systematic review and meta-analysis. Int J Infect Dis. 2016;49:129–133. doi: 10.1016/j.ijid.2016.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li SS, Cheng C, Fu C, Chan Y, Lee M, Chan JW, Yiu S. Left ventricular performance in patients with severe acute respiratory syndrome: a 30-day echocardio-graphic follow-up study. Circulation. 2003;108:1798–1803. doi: 10.1161/01.CIR.0000094737.21775.32. [DOI] [PubMed] [Google Scholar]
- 8.Harris JE, Shah PJ, Korimilli V, Win H. Frequency of troponin elevations in patients with influenza infection during the 2017-2018 influenza season. Int J Cardiol Heart Vasc. 2019;22:145–147. doi: 10.1016/j.ijcha.2018.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020 doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Libby P, Simon DI. Inflammation and thrombosis: the clot thickens. Circulation. 2001;103:1718–1720. doi: 10.1161/01.cir.103.13.1718. [DOI] [PubMed] [Google Scholar]
- 11.Corrales-Medina VF, Alvarez KN, Weissfeld LA, Angus DC, Chirinos JA, Chang CC, Newman A, Loehr L, Folsom AR, Elkind MS, Lyles MF, Kronmal RA, Yende S. Association between hospitalization for pneumonia and subsequent risk of cardiovascular disease. JAMA. 2015;313:264. doi: 10.1001/jama.2014.18229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wu Q, Zhou L, Sun X, Yan Z, Hu C, Wu J, et al. Altered lipid metabolism in recov-ered SARS patients twelve years after infection. Sci Rep. 2017;7:9110. doi: 10.1038/s41598-017-09536-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang J, Xu H, Yang X, Zhao D, Liu S, Sun X, Huang J, Guo Q. Cardiac com-plications associated with the influenza viruses A subtype H7N9 or pandemic H1N1 in critically ill patients under intensive care. Braz J Infect Dis. 2017;21:12–18. doi: 10.1016/j.bjid.2016.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Igić R. Pharmacologist’s view of the new corona virus. Scr Med. 2020;51(1):6–8. [Google Scholar]
- 15.Bailly C. Cepharanthine: An update of its mode of action, pharmacological properties and medical applications. Phytomedicine. 2019 Sep;62:152956. doi: 10.1016/j.phymed.2019.152956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020 Mar 4; doi: 10.1016/j.cell.2020.02.052. pii: S0092-8674(20)30229-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Igić R. Pharmacology of the renin-angiotensin system. Banja Luka: Faculty of Medicine, University of Banja Luka; 2014. [Google Scholar]
- 18.Thomson GA. Where are we now with COVID-19? Int J Clin Pract. 2020 Mar 11;:e13497. doi: 10.1111/ijcp.13497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Patel AB, Verma A. COVID-19 and angiotensin-converting enzyme inhibitors and angiotensin receptor blockers: what is the evidence? JAMA. 2020. Mar 14, [March 10th, 2020]. Available on: https://jamanetwork.com/journals/jama/fullarticle/2763803 . [DOI] [PubMed]
- 20.EMA Says Stay on Angiotensin Drugs During COVID-19 Pandemic – Medscape. 2020. Mar 17, [March 18th, 2020]. Available on: https://www.medscape.com/viewarticle/927646 .
- 21.ACC Clinical Bulltiein COVID-19: Clinical Guidance For the CV Care Team. The American College of Cardiology; 2020. Mar, [March 15th, 2020]. Available on: http://www.acc.org/~/media/665AFA1E710B4B3293138D14BE8D1213.pdf . [Google Scholar]
- 22. [March 15th, 2020]. http://www.drugs.com/condition/covid-19.html .
- 23. [March 15th, 2020]. http://www.cdc.gov/coronavirus/2019-ncov/infection-control/index.html .
- 24. [March 15th, 2020]. https://www.healthline.com/health/coronavirus-covid-19#symptoms .
- 25. [March 15th, 2020]. https://www.bing.com/search?q=prevention+covid-19&form=PREXEN .
- 26.Salihefendic N, Zildzic M, Ahmetagic S. Acute Respiratory Distress Syndrome (ARDS) from Endemic Influenza A/H1N1: Prehospital Management. Med Arh. 2015 Feb;69(1):62–63. doi: 10.5455/medarh.2015.69.62-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hassan S, Jawad JM, Ahjel WS, Sing BR, Sing J, Awad MS, Hadi RN. The Nrf2 Activator (DMF) and Covid-19: Is there a Possible Role? Med Arch. 2020 Apr;74(2):134–138. doi: 10.5455/medarh.2020.74.134-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Masic I. Golden ages of Arabic-Islamic medicine: The first Arabic hospitals and the Public health. In: Masic i, et al., editors. Medieval Arabic Medicine. Sarajevo: Avicena; 2010. pp. 239–262. ISBN: 978-9958-720-40-6. [Google Scholar]
- 29.Masic I. The Most Influential Scientists in the Development of Public Health (4): Andrija Stampar (1888-1958) Mater Sociomed. 2019 Dec;31(4):298–299. doi: 10.5455/msm.2019.31.298-299. [DOI] [PMC free article] [PubMed] [Google Scholar]