Abstract
Introduction:
Osteoporosis is a chronic progressive bone disease where the bone tissue resorption exceeds its regenerative capacities. Such a process leads to the reduction of bone mineral density (BMD), and distortion of trabecular microarchitectonics, which creates the basis for an increased fracture risk on a “low trauma” for osteoporosis patients. The notion of low trauma implies a stressor that will not cause a fracture in a healthy person under normal circumstances. BMD is a strong predictor of future fractures. However, many fractures occur in persons with BMD values beyond the defined osteoporosis threshold, and BMD measurement only partially identifies the part of the population with increased fracture risk. Also, it is known that risk factors are influencing the bone mass reduction as predictors of future fractures, and their association may lead to an increased fracture risk irrespective of the bone mass and T-score.
Aim:
The 10-year individual risk assessment for osteoporotic fracture and the analysis of impact of individual and multiple osteoporosis risk factors on the degree of osteoporotic fracture risk.
Methods:
The research is a retrospective-prospective study which analyzed 120 patients divided into two groups: 1) asymptomatic patients with known risk factors for osteoporosis in the age group of 40-65 (n=60), 2) asymptomatic patients with known risk factors for osteoporosis in the age group of 65-90 (n=60). FRAX® algorithm was used as a tool for the 10-year hip fracture risk assessment, with prior approval of the Centre for Metabolic Bone Diseases, University of Sheffield from the United Kingdom. Fracture risk assessment was calculated using the online FRAX® calculator. High risk is defined as the hip fracture risk higher than 3% or the risk of a “big” osteoporotic fracture higher than 20%. Results are expressed as mean values with a standard deviation. A comparison between tested patient groups was made applying the student T-test.
Results:
32% of patients of average age of 65.8±12.6 years are under high hip fracture risk, 28% of patients are under the hip fracture risk higher than 3%, and the risk for 0.03% patients is higher than 20%. Patients with high fracture risk are of advanced age, female, with lower body weight and height values, lower bone mineral density (BMD) and T score values than patients who are not under a high fracture risk. A positive family anamnesis to osteoporosis and fractures, earlier fractures, smoking, rheumatoid arthritis, and use of glucocorticoids are risk factors that are more represented in patients with high fracture risk and osteoporosis. The impact of the majority of individual risk factors for osteoporosis and fracture is moderate, and their joint effect is significant. The contribution of individual risk factors to the overall 10-year fracture risk depends on the type, number and association of risk factors.
Conclusion:
This research is a contribution to the resolution of polemics among authors, i.e. a dilemma whether persons with multiple clinical risk factors for osteoporosis with T score values beyond the defined threshold for osteoporosis are candidates for therapy with bisphosphonates, and a dilemma whether persons without any clinical risk factors for osteoporosis with T score values within the defined osteoporosis threshold require therapy with bisphosphonates, or only monitoring is sufficient.
Keywords: dual-energy x-way absorptiometry (DEXA), fracture risk assessment (FRAX®), bone mineral density (BMD), T score
1. INTRODUCTION
Osteoporosis is a chronic progressive bone disease where the bone tissue resorption exceeds its regenerative capacities. Such a process leads to the reduction of bone mineral density (BMD), and distortion of trabecular microarchitectonics, which creates the basis for an increased fracture risk on a “low trauma” for osteoporosis patients. The notion of low trauma implies a stressor that will not cause a fracture in a healthy person under normal circumstances (1). BMD is a strong predictor of future fractures. However, many fractures occur in persons with BMD values beyond the defined osteoporosis threshold, and BMD measurement only partially identifies the part of the population with increased fracture risk Also, it is known that risk factors are influencing the bone mass reduction as predictors of future fractures, and their association may lead to an increased fracture risk irrespective of the bone mass and T-score. Considering that the change of bone density does not always match the fracture risk, along with determining the bone metabolism markers, the osteoporosis diagnostics should include the fracture risk assessment based on osteoporosis risk factors, especially if one already experienced a low trauma fracture. Swift osteoporosis identification and management following the first fracture will reduce the risk of the second fracture which is 2-3 times higher (2). As a tool for the assessment of ten-year hip fracture risk or a “big” bone fracture caused by osteoporosis (clinical spine, forearm, hip or shoulder fracture), professor Kanis and associates at the Centre for Metabolic Bone Diseases, University of Sheffield identified fracture risk factors and consolidated them in the Fracture Risk Assessment (FRAX®) algorithm that was applied to the population of the United Kingdom, and its calibration was then implemented in 45 countries (3). The value of FRAX® hip fracture index above 3 % and for other fractures above 20 % is an indication for therapy introduction (4), which is the goal of the FRAX® assessment–to determine if persons with low bone density are candidates for pharmacotherapy or not, based on the individual fracture risk.
2. AIM
The research aim is to conduct the 10-year individual risk assessment for osteoporotic fracture and the analysis of impact of individual and multiple osteoporosis risk factors on the degree of osteoporotic fracture risk.
3. PATIENTS AND METHODS
The research is a retrospective-prospective study which analyzed 120 patients divided into two groups: 1) asymptomatic patients with known risk factors for osteoporosis in the age group of 40-65 (n=60), 2) asymptomatic patients with known risk factors for osteoporosis in the age group of 65-90 (n=60). Both groups were formed using the random sampling method: the first group was formed of the total of 400 patients under the age of 65, and the second group of 600 patients above 65. This study includes only patients who were not previously diagnosed as having primary osteoporosis.
FRAX® questionnaire was used for the osteoporotic fracture risk assessment in all patient groups, with prior approval of the Centre for Metabolic Bone Diseases, University of Sheffield from the United Kingdom.
Fracture risk assessment was calculated using the online FRAX® calculator. High risk is defined as the hip fracture risk higher than 3% or the risk of a “big” osteoporotic fracture higher than 20%. Results are expressed as mean values with a standard deviation. A comparison between tested patient groups was made applying the student T test.
4. RESULTS
The survey covered 120 patients aged ≥ 40 and ≤ 90, of which 92 women, and 28 men.
Table 1. Demographic characteristics .
| Characteristics | Patients (n) | Age in years (mean value and standard deviation) |
|---|---|---|
| Sex | ||
| women | 92 | 66.03±12.71 |
| men | 28 | 65.21±12.64 |
| Age groups by years | ||
| 40-49 | 17 | 46.00±3.25 |
| 50-59 | 25 | 56.36±3.05 |
| 60-69 | 32 | 64.78±2.77 |
| 70-79 | 26 | 74.96±3.05 |
| 80-89 | 20 | 84.40±2.87 |
| Age groups | ||
| 40-64 | 60 | 55.33±7.03 |
| 65-89 | 60 | 76.35±6.98 |
| Total | 120 | 65.84±12.65 |
Figure 1. 10-year fracture risk.
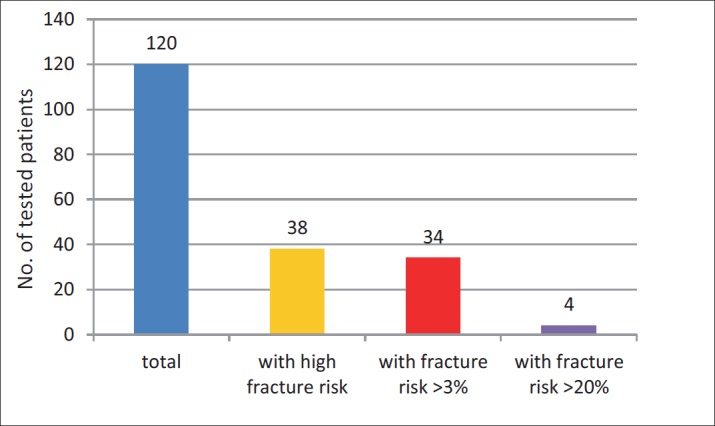
Figure 2. 10-year fracture risk by age.
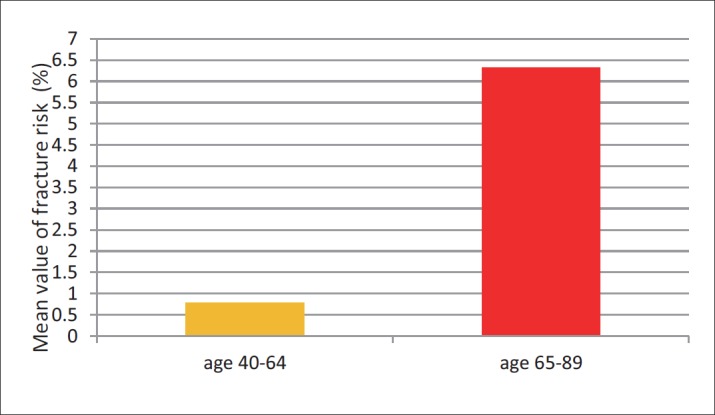
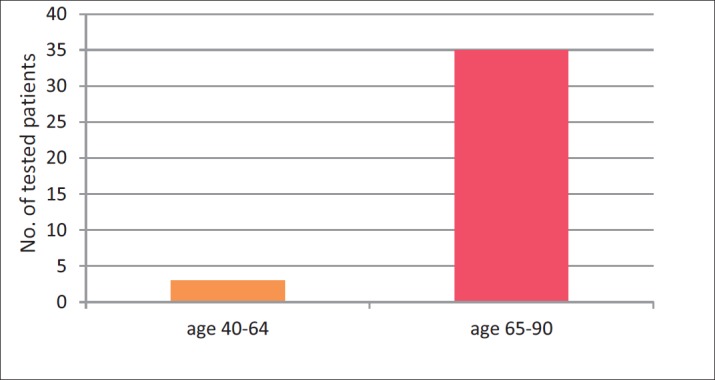
Figure 3. Impact of age on 10-year fracture risk.
It was found in the tested sample that 38 (32%) of patients are under high hip fracture risk, of which 34 (28%) of patients are under the hip fracture risk higher than 3%, and the risk for 4 (0.03%) patients is higher than 20% , (risk of “big” osteoporotic fracture).
Mean value of 10-year hip fracture risk in the group of tested patients aged 40-64 is 0.7%, and 6.3% in the age group of 40-64.
Mean value of 10-year hip fracture risk by age groups is shown in Table 2.
Table 2. 10-year hip fracture risk by age groups .
| % of 10-year hip fracture risk | |||
|---|---|---|---|
| Mean value and standard deviation | p value | ||
| Sex | n | ||
| women | 92 | 4.2±6.7 | |
| men | 28 | 1.1±2.1 | <0.01 |
| Age groups | |||
| 40-64 | 60 | 0.7±1.3 | |
| 65-89 | 60 | 6.3±7.6 | <0.01 |
| Age groups by years | |||
| 40-49 | 17 | 0.2±0.3 | |
| 50-59 | 25 | 0.7±0.9 | |
| 60-69 | 32 | 1.6±1.6 | |
| 70-79 | 26 | 5.1±6.7 | |
| 80-89 | 20 | 10.8±9.0 | <0.01 |
Impact of anthropometric risk factors on 10-year fracture risk
Impact of age
The high fracture risk is statistically more represented among patients in the age group of 65-89, than in the age group of 40-64.
Impact of sex
It was found that the high fracture risk is statistically significantly more represented among women than among men.
Impact of clinical risk factors on 10-year fracture risk
Impact of positive family anamnesis for hip fracture
In the patient group with high fracture risk, there is a statistically significant larger number of patients with a positive anamnesis for hip fracture in parents, compared to patients without high fracture risk.
Impact of previous fractures
Figure 4. Impact of family anamnesis on 10-year fracture risk.
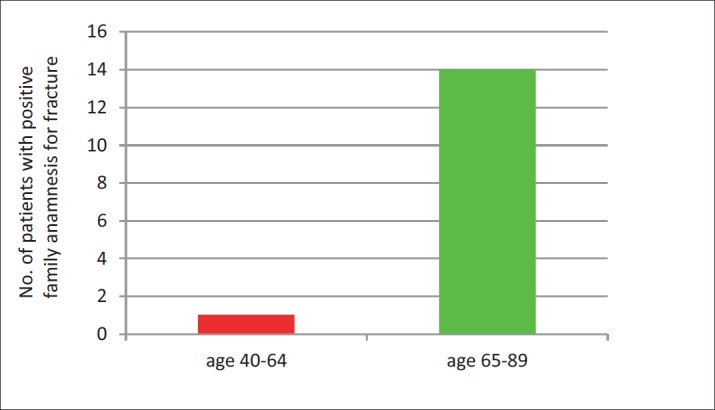
Figure 5. Impact of previous fractures on 10-year fracture risk.
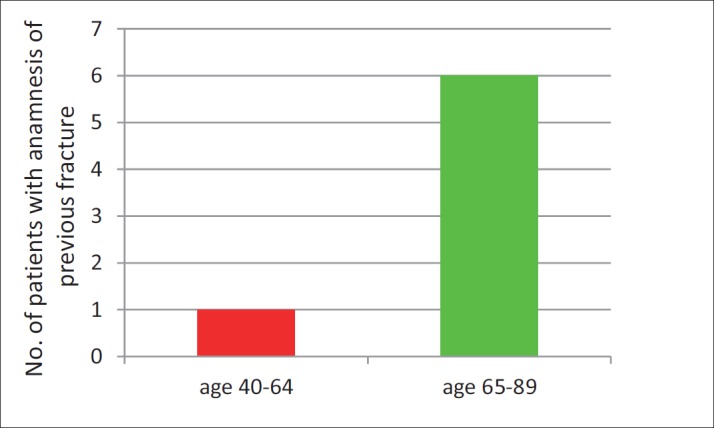
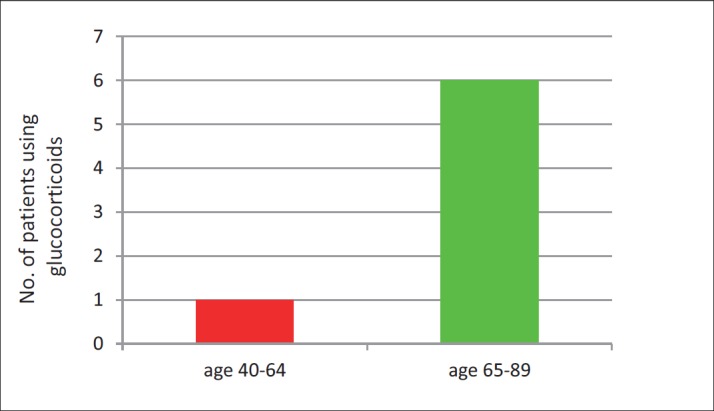
Figure 6. Impact of the use of glucocorticoids on 10-year fracture risk.
Tested patients with high fracture risk had a statistically significant larger number of previous fractures compared to patients without high risk.
Impact of the use of glucocorticoids
The use of glucocorticoids is more represented in patients with high fracture risk, and the difference is statistically significant compared to patients without high risk.
Impact of rheumatoid arthritis
Among patients with high fracture risk, there was a statistically significant larger number of patients with rheumatoid arthritis compared to patients without high fracture risk.
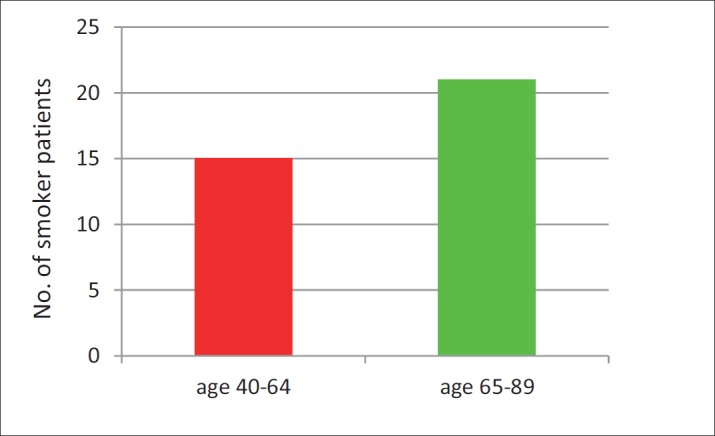
Impact of smoking
Among patients with high fracture risk, there is a statistically significant larger number of smokers compared to patients without high fracture risk.
The contribution of individual risk factors to the overall 10-year fracture risk is different depending on the type, number and association of individual risk factors. A positive family anamnesis for fractures contributes the most to the overall 10-year fracture risk.
Figure 7. Impact of rheumatoid arthritis on 10-year fracture risk.
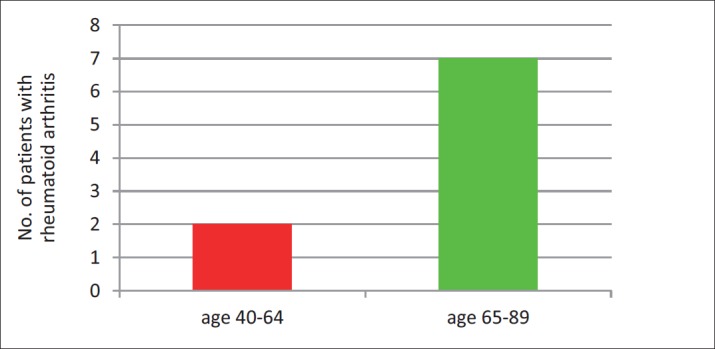
Figure 8. Impact of smoking on 10-year fracture risk.
5. DISCUSSION
Osteoporosis is a systemic skeleton disease characterized by the bone mass decrease and bone structure changes, which results in higher inclination to bone tissue fractures. BMD is a strong predictor of future fractures and osteoporosis is currently defined on BMD (5). However, many fractures occur in persons with BMD values beyond the defined osteoporosis threshold, and BMD measurement only partially identifies the part of the population with increased fracture risk. It is known that, as predictors of future fractures, risk factors are influencing the bone mass reduction by reducing the maximum bone mass developed by the age of 35 and/or accelerate the usually normal process of gradual and mild bone mass reduction which begins after the age of 35, and thereby increase the fracture risk. Also, it is known that some risk factors and their association may lead to an increased fracture risk irrespective of the bone mass and T-score. Apart from determining the bone metabolism markers and BMD value of the spine and hip, the assessment of presence of numerous clinical risk factors for fracture and osteoporosis is necessary for defining the overall fracture risk. Today, it is believed that the existence of osteopenia with previous low trauma fracture represents the first indication for therapy introduction. Also, there is a polemic among authors in the literature on whether the DEXA finding on the low back and hip within the osteoporosis, without the existence of fracture risk factors, represents a therapy indication, or the patient can only be monitored (6). To resolve this disagreement, a group of WHO researchers, in cooperation with the Centre for Metabolic Bone Diseases, University of Sheffield from the United Kingdom developed a fracture risk assessment tool in early 2000s, which is more global than the assessment based on BMD only. Numerous clinical risk factors were identified and validated as fracture predictors independently of BMD. The FRAX® algorithm was developed as a tool for the assessment of 10-year fracture risk and the “big” osteoporotic fracture (spine, forearm, hip or shoulder fracture in persons above the age of 40). It analyses 12 parameters related to osteoporosis risk factors and fracture risk. Age is a separate and dominant risk factor for osteoporosis and fractures (7). Some of the studies point out that women above 65 have 1.5-2 times higher fracture risk than women under the age of 65 (8). Sex also represents a special risk factor for osteoporosis and future fractures. Bodily weight is a strong determinant of bone mineral density. Numerous studies indicate that low body weight represents a bone mass reduction risk factor, and that it can be useful in the selection of women to be referred to the bone density testing (9). Many studies define the positive family anamnesis for fractures as one of the most important risk factors, and numerous authors demonstrated the polymorphism of genes responsible for the genetic predisposition to osteoporosis and increased fracture risk (10). The use of glucocorticoids represents a risk factor for osteoporosis and fracture. Some studies have shown that the fracture incidence increases by 30-50% during three months of therapy administration in patients with rheumatoid arthritis who administer corticosteroid therapy. The first month of therapy administration is deemed the highest-risk-bearing for BMD decrease (11). Smoking of more than 10 cigarettes a day is deemed a fracture risk factor. Nicotine and many other cigarette ingredients together reduce the duration of women’s generative period by decreasing estrogen level, and decrease calcium absorption from small intestine, which additionally leads to osteoporosis (12). Results of our research show that 32% of patients of average age of 65.8±12.6 are under high hip fracture risk, 28% of patients are under the hip fracture risk higher than 3%, and the risk for 0.03% patients is higher than 20% (risk of big fracture). Tested patients with high fracture risk, compared to patients without high risk, had a statistically significant larger number of previous fractures, more of them were smokers and had a positive hip fracture anamnesis in parents, rheumatoid arthritis and use of glucocorticoids, they are advanced age, female, with lower body weight and height, BMD and T score values.
6. CONCLUSION
Apart from determining the BMD and bone metabolism markers, the assessment of presence, number, type and association of clinical fracture risk factors is important for defining the overall fracture risk. The impact of the majority of individual risk factors for osteoporosis and fracture is moderate, and their joint effect is significant. This research is a contribution to the resolution of polemics among authors, i.e. a dilemma whether persons with multiple clinical risk factors for osteoporosis with T score values beyond the defined threshold for osteoporosis are candidates for therapy with bisphosphonates, and a dilemma whether persons without any clinical risk factors for osteoporosis with T score values within the defined osteoporosis threshold require therapy with bisphosphonates, or only monitoring is sufficient. Future research should certainly assess the influence of bone metabolism markers on the osteoporotic fracture risk level, which would complete and improve prevention, diagnostics and treatment of osteoporosis.
Acknowledgments:
The authors would like to acknowledge patients who participated in this study.
Autor’s contributions:
Study conception and design: Alibasic Esad. Acquisition of data: Alibasic Esad, Fazlić Mirsad. Statistical analysis and interpretation: Alibašić Esad, Fazlić Mirsad. Drafting of the manuscript: Fazlić Mirsad, Husic Damir. Critical revision of the manuscript for important intelectual content: Ljuca Farid, Brkić Selmira. Final approval of the version: Alibasic Esad.
Conflict of interest:
None declared.
Financial support:
Nil.
REFERENCES
- 1.Rizzoli R, Boonen S, Brandi ML. The role of calcium and vitamin D in the management of osteoporosis. Bone. 2008;42:246–249. doi: 10.1016/j.bone.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 2.Klotzbuecher CM, Ross PD, Landsman PB. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Mineral Research. 2000;15(4):721–739. doi: 10.1359/jbmr.2000.15.4.721. [DOI] [PubMed] [Google Scholar]
- 3.Collins GS, Mallett S, Altman DG. Predicting risk of osteoporotic and hip fracture in the United Kingdom: prospective independent and external validation of QFractureScores. BMJ. 2011;22:342. doi: 10.1136/bmj.d3651. d3651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leslie WD, Majumdar SR, Lix LM, Johansson H, Oden A, McCloskey E. High fracture probability with FRAX usually indicates densitometric osteoporosis: implications for clinical practice. Osteoporos Int. 2012;23(1):391–397. doi: 10.1007/s00198-011-1592-3. [DOI] [PubMed] [Google Scholar]
- 5.Kanis JA, McCloskey EV, Johansson H, Oden A, Melton LJ, Khaltaev NA. Reference standard for the description of osteoporosis. Bone. 2008;42(3):467–475. doi: 10.1016/j.bone.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 6.Stepán J. Osteoporosis: whom, when and how to treat? Cas Lek Cesk. 2009;148(1):25–33. [PubMed] [Google Scholar]
- 7.Jakobsen A, Laurberg P, Vestergaard P, Andersen S. Clinical risk factors for osteoporosis are common among elderly people in Nuuk, Greenland. Int J Circumpolar Health. 2013;72:195–196. doi: 10.3402/ijch.v72i0.19596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kung AWC, Lee KK, Ho AY, Tang GWK, Luk KD. Ten-year risk of osteoporotic fractures in postmenopausal Chinese women according to clinical risk factors and BMD T-skore: A prospective study. J Bone Miner Res. 2007;22(7):1080–1086. doi: 10.1359/jbmr.070320. [DOI] [PubMed] [Google Scholar]
- 9.Dargent-Molina P, Poitiers F, Breart G. In eldery women weight is the best predictor of a very low bone mineral density: evidence from the EPIDOS study. Osteoporos Int. 2000;11(10):881–888. doi: 10.1007/s001980070048. [DOI] [PubMed] [Google Scholar]
- 10.Falcon-Ramirez E, Casas-Avila L, Miranda A, Diez P, Castro C, Rubio J. Sp 1 polymorphism in collagen I alpha1 gene is associated with osteoporosis in lumbal spine of Mexican women. Mol Biol Rep. 2011;38(5):2987–2992. doi: 10.1007/s11033-010-9963-y. [DOI] [PubMed] [Google Scholar]
- 11.Pereira RM, Carvalho JF, Paula AP, Zerbini C, Domiciano DS, Goncalves H. Guidelines for the prevention and treatment of glucocorticoid-induced osteoporosis. Rev Bras Reumatol. 2012;52(4):580–593. [PubMed] [Google Scholar]
- 12.Demirbag D, Ozdemir F, Ture M. Effects of coffe consumption and smoking habit on bone mineral density. Rheumatol Int. 2006;26(6):530–535. doi: 10.1007/s00296-005-0020-4. [DOI] [PubMed] [Google Scholar]


