Abstract
Aims
Type 2 diabetes mellitus (T2DM) and gestational diabetes (GDM) are globally on the rise, accompanied by comorbidities and associated health costs. Increased physical activity, healthy nutrition, and weight loss have shown the potential to prevent T2DM/GDM. Despite this, reaching vulnerable groups remains a key challenge. The aim of this scoping review was to identify barriers and facilitating factors in the prevention of T2DM/GDM in vulnerable groups.
Methods
We conducted a systematic literature search in May 2018, updated in September 2019, in several databases (e.g. PubMed, Embase) to identify barriers and facilitating factors in the prevention of T2DM/GDM in vulnerable groups. Two reviewers independently screened the results. Extracted data was charted, categorized, and summarized.
Results
We included 125 articles. Ninety-eight studies were extracted, and eight categories of barriers and facilitating factors were formed. The most common categories of barriers were limited knowledge, family/friends, and economic factors, and the most common categories of facilitating factors were family/friends, social support, and knowledge.
Conclusion
This scoping review identified various barriers and facilitating factors in vulnerable groups. Preventive interventions should consider these barriers and facilitating factors in developing preventive interventions or in adapting existing ones.
Background
The prevalence of type 2 diabetes mellitus (T2DM) and gestational diabetes (GDM) is rising worldwide, and so are the associated health consequences and healthcare costs [1]. Evidence shows that the prevalence of T2DM/GDM is higher in obese or overweight, physically inactive individuals [2, 3]. Increased physical activity, healthy nutrition, and weight loss may prevent or delay T2DM/GDM manifestation [4]. Lifestyle interventions like the Diabetes Prevention Program (DDP) may reduce the risk of T2DM more effectively than antidiabetic drugs such as metformin [5]. However, these preventive interventions typically target patients mostlyfrom the general population, and it is challenging to reach vulnerable groups, including individuals with a migration background and/or low socio-economic status. Such patients are disproportionally affected by T2DM/GDM and diabetes-related complications [6, 7]. Language, cultural perception, and lower health literacy often play important roles in non-participation [8]. Research suggests that behavioral change is possible, but generally requires comprehensive approaches tailored to specific settings and target groups [9]. Therefore, the development of new T2DM/GDM interventions should be informed by evidence of barriers and facilitating factors. This may enhance the willingness of patients to participate in preventive interventions. The aim of this scoping review was to identify and describe barriers and facilitating factors in the prevention of T2DM/GDM in vulnerable groups.
Methods
This project was commissioned by the Federal Centre for Health Education in Germany as part of the “National education and communication strategy on diabetes mellitus”. Its protocol was published a-priori [10]. Since the International prospective register of systematic reviews (PROSPERO) does not register scoping reviews, this scoping review is not registered.
The scoping review was conducted following the Arksey and O´Malleys framework [11] and the Joanna Briggs Institute Reviewers’ Manual 2015 [12]. It is reported based on the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist [13].
Eligibility criteria
Inclusion criteria
vulnerable patients with, or at risk of, T2DM/GDM
studies present barriers and facilitating factors for implementing a preventive intervention
WHO mortality stratum A countries
publication date ≥ 2008
Exclusion criteria
indigenous people, children, or people with mental disorders
no full texts available
general prevention without any context of T2DM/GDM
patients on antidiabetic medication
Eligibility criteria were categorized using the Population, Concept, Context (PCC) mnemonic (Table 1). All study types were eligible that present barriers to and facilitating factors for implementing preventive interventions in vulnerable patients with, or at risk of, T2DM/GDM. Studies published before January 2008 were excluded, because barriers and facilitators are affected by external factors such as accessibility of care and information. We assume that accessibility has changed substantially compared to 10 years ago due to the increased volume of digital and virtual goods, services, and processes in healthcare. As a result, the barriers and facilitators might have changed, so that there would be a lack of comparability if we chose a longer period.
Table 1. PCC (Population, Concept, Context).
| P | Diabetes mellitus type 2 or gestation diabetes | Type 2 diabetes mellitus |
| Gestational diabetes mellitus | ||
| People at risk of developing diabetes mellitus or gestational diabetes mellitus | ||
| Vulnerable patients/-groups | Elderly, older people, seniors > 65 years | |
| Disabled people | ||
| People in need of care, residents of a nursing home | ||
| Unemployed people | ||
| Refugees/migrants as well as ethnic groups (e.g. African Americans or Hispanics) | ||
| Homeless people | ||
| Drug/substance abusers (excluding nicotine abuse/smoking) | ||
| Low socio-economic status | ||
| C | Prevention | Primary/ secondary/ tertiary prevention |
| Barriers and facilitating factors | Definition of barriers and motivating aspects e.g. language, costs, religion, ethnic background, low income, social and health support | |
| Solutions to exploit barriers and support solutions e.g. materials and manpower, use of media, insurance | ||
| C | >2008; WHO stratum A | |
| Other | all types of studies; all languages; available in full text version | |
The PPC (Population, Concept, Context) mnemonic illustrates the eligibility criteria for the scoping review. Additionally to the classic PPC mnemonic there are other criteria regarding study types, languages and the availability of the full text version.
No language restriction was applied. All full texts published in languages other than English or German were translated by an external agency. We only included studies performed in countries within the low mortality stratum (A) defined by the World Health Organization [14]. By doing so, we ensured that our findings were applicable throughout western industrialized countries. We define vulnerable groups according to Lewis et al. [15], but excluded indigenous people, children, and people with mental disorders. This was done to align our study with the aims of the “National education and communication strategy on diabetes mellitus”. To separate tertiary prevention from therapy, we excluded studies with patients treated with any antidiabetic medication. Furthermore, we excluded studies which could be interpreted as preventing general metabolic risk factors without primary focus on T2DM/GDM prevention, such as studies aiming at weight reduction in obese patients.
Information sources
The following electronic databases were searched: PubMed, EMBASE, PsycINFO, PSYNDEX, Social Science Citation Index, and CINAHL. Grey literature was searched on greylit.org and via the homepages of the WHO and international healthcare or public health departments (e.g. Department of Health & Social Care, UK; Agency for Healthcare Research and Quality (AHRQ); US Preventive Services Task Force). We manually checked the reference lists of all included studies.
Search
The search strategy was developed by the research team in collaboration with an experienced librarian and checked by a referee according to the Peer Review of Electronic Search Strategies (PRESS) guideline [16]. All initial database searches were conducted in May 2018, while grey literature was searched in July 2018. The initial database searches were updated in September 2019. The initial grey literature search was not updated because the original search was very time-consuming and did not yield any relevant references. The search strategy is presented as S1 Appendix.
Data management
The search results were uploaded and managed using Microsoft Excel.
Study selection
Two reviewers independently screened the titles and abstracts of all search results and assessed full texts of potentially relevant articles against the predefined selection criteria. Any disagreement was resolved by discussion and consensus. The reasons for exclusion of full texts were documented.
Data extraction
A standardized extraction form was developed for this review. Using a sample of five articles, the form was piloted, assessed for completeness and applicability, and modified to ensure all data necessary to address the research questions were obtained. Data were extracted by one reviewer and checked by another. Disagreements were resolved through discussion and consensus.
Data items
The preliminary data extraction categories were derived from our overarching research question. The following data were collected:
study characteristics (e.g. country, setting, publication date, number of participants, study design/method)
patient characteristics (e.g. age, gender, allocation to vulnerable group)
inclusion/exclusion criteria
barriers
facilitating factors
Patient allocation to a vulnerable group was made according to the PCC mnemonic. Studies targeting mixed groups were allocated to the new ‘mixed vulnerable group’. We assigned each barrier and facilitating factor to one of the following eight predefined categories: language, economic factors, family and friends, work, social support, religion, culture, and knowledge. We defined these categories based on qualitative thematic analysis. The total number of barriers and facilitating factors within each category is based on the number of identified studies which mentioned this barrier or facilitating factor. We did not analyze how often a barrier or facilitating factor is mentioned within each study.
Risk of bias
As this is a scoping review, risk of bias was not assessed. This is consistent with guidance on the conduct of scoping reviews [11].
Data analysis
We used Arksey and O’Malley’s methods [11] and provide a descriptive analysis of the extent, nature, and distribution of the studies included in the review as well as a narrative thematic summary of the data collected. This was achieved by summarizing the literature according to the types of vulnerable groups, comparators, barriers and prohibitive factors, and outcomes identified. We aimed to map the extent, range, and nature of research in this area using visual representations of the data. Data were charted, categorized, and summarized. We reported quantitative (e.g. frequency) and qualitative results. Furthermore, we sought to explore similarities and differences, both within and between studies, to identify patterns and themes and postulate explanations for findings. We focused on barriers and prohibitive factors for preventive interventions in vulnerable patients with or at risk of T2DM/GDM. We also considered the robustness of the included studies by assessing the overall strength and confidence of the findings. Where possible, we stratified our results by vulnerable groups.
Results
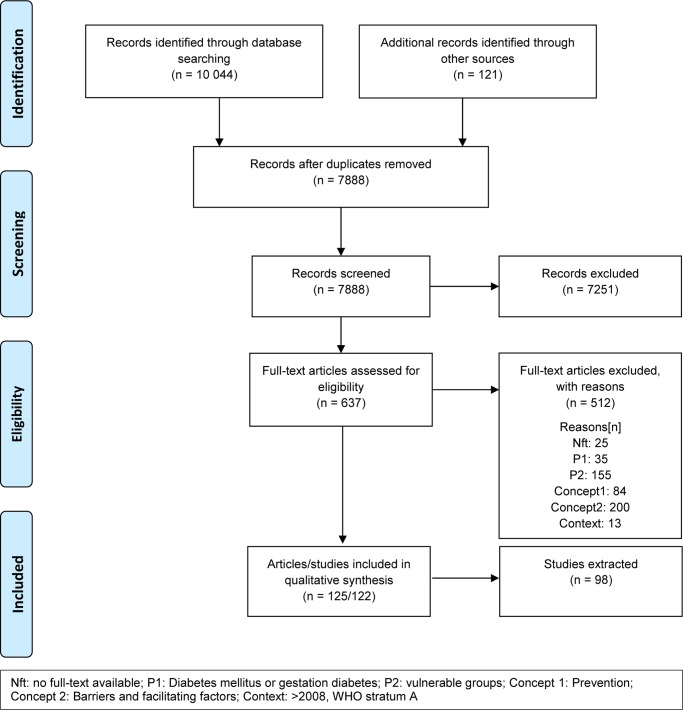
Our database search yielded 10,044 articles. An additional 121 references were identified by searching for grey literature and checking reference lists, which led to 7888 articles after deduplication (see Fig 1). A list of excluded full-text articles is available as S2 Appendix. A total of 125 articles (122 studies) were included. Included reviews (n = 24, e.g. systematic reviews, narrative reviews) were used for reference-checking but no data were extracted. The remaining 101 articles (98 studies) were extracted and analyzed.
Fig 1. Flow chart.
Characteristics of included studies
Among included studies, n = 77 had a qualitative design (focus groups n = 40, interviews n = 37). Most studies were conducted in the US (n = 65), others in Australia (n = 8), Canada (n = 7), and the UK (n = 8). We identified four studies which focused only on GDM [17–20], and three (four articles) which focused on both T2DM and GDM [21–24]. The most prominent vulnerable groups within these studies were migrants (n = 59), ethnic groups (n = 23) such as Afro-Americans, and people with low socio-economic status (n = 6). Other vulnerable groups identified were older migrants (n = 2), migrants/ethnic groups which could not be sharply delineated (n = 2), homeless people (n = 1), a mixed group of people with a low socioeconomic status and homeless people (n = 1), unemployed people (n = 1), migrants with low socio-economic status (n = 1), people with disabilities (n = 1) and older people (n = 1). The characteristics of included studies are listed in S3 Appendix.
Barriers and facilitating factors for implementing a preventive intervention
Various categories of barriers and facilitating factors for implementing a preventive intervention were identified, some of which overlapped within the same study (Table 2). The most common types of barriers are family and friends (44/98), limited knowledge (44/98 studies), and economic factors (40/98). The most widely encountered facilitating factors are family and friends (46/98), social support (27/98), and knowledge (15/98). Family and friends, knowledge, and social support are factors that can influence the implementation of a preventive intervention in either direction. Other barriers could not be assigned to any of the eight categories, and appeared in an insufficient number of studies to justify forming additional categories. These include insufficient time, insufficient skills, insufficient motivation/energy, fear (e.g. of needles) in T2DM management or of injuries while being physical active, and travel/transport issues.
Table 2. Barriers and facilitating factor categories for implementing a preventive intervention for people with or at risk of T2DM/GDM.
| barriers | facilitating factors | both within a study | |
|---|---|---|---|
| Language | 22 | 0 | 0 |
| economic factors | 40 | 0 | 0 |
| family and friends | 44 | 46 | 22 |
| Work | 28 | 0 | 0 |
| social support | 16 | 27 | 8 |
| Religion | 5 | 8 | 1 |
| Culture | 30 | 0 | 0 |
| knowledge | 44 | 15 | 4 |
| other barriers (e.g. insufficient time, problems with travelling, insufficient motivation) | 9 | n.a. | n.a. |
GDM: gestational diabetes; n.a.: not applicable; T2DM: type 2 diabetes mellitus
The total number of barriers and facilitating factors within each category is based on the number of identified studies which mentioned this barrier or facilitating factor.
T2DM/GDM
Most studies were conducted in a T2DM population (88/98), only four studies in the context of GDM. The most common barriers in GDM studies were economic factors (n = 4) and limited knowledge (n = 3). One important facilitating factor for the prevention of GDM is the wellbeing of the unborn child.
Language
We identified 22/98 studies which describe language barriers. All but one study, performed in an ethnic group [25], were within the vulnerable group of migrants. In most studies, language barriers led to difficulties in understanding either written materials or oral information [26]. In addition, anxiety about dealing with native speakers was reported to be a major barrier to health service access for non-native speakers [27].
Economic factors
Economic barriers included not only the cost of preventive interventions (e.g. nutritional/fitness courses or travel costs), but more importantly the cost of healthy food. Lack of health insurance also constituted an economic barrier [28]. Economic factors were identified only as barriers; possible facilitating factors such as incentives for participating or insurance bonus programs were not reported in the identified studies.
Family and friends
Family and friends can act as both barrier and facilitating factor. This depends on whether they act supportively [29] regarding the preventive intervention or obstruct it. For example, family members may not want to change their dietary habits along with the patient, thus making it hard for the patient to stick to their new diet or force them to prepare two different meals [30]. There was also a gender difference in how factors in the family and friends category were perceived. Women often describe family as a barrier because childcare [31] or household chores [32] result in a lack of time to implement preventive interventions.
Work
Work creates a lack of time in which to join preventive courses or tutorials [33]. Shift work leads to variable work hours, making it difficult to join courses on a regular basis. Additionally, patients working shifts [34] or nights [34, 35] find it harder to eat regular meals.
Social support
This category describes social support as both a barrier and facilitating factor. Social support in this category encompasses government support, along with covers any other type of external help. For example, single mothers listed insufficient childcare opportunities while participating in a preventive intervention as a barrier [36].
Religion/culture
Religion and culture were two separate categories of barriers and facilitating factors but overlapped in many ways. For instance, religious festivals often involve a lot of traditional food.
Religious beliefs could be both barrier and facilitating factor. Bhattacharya et al. showed this within the same study [37]. Different options exist on how to interpret God´s will and how to embed T2DM in the religious context. The diagnosis of T2DM could be considered as “God given”, leading believers to “surrender to God´s will” [38, 39]. Another belief was “that not taking care of one´s body goes against (…) self-responsibility” [37]. Some studies demonstrated the importance of rice in many cultures including South Asian, African, and Latino Communities. The preventive diets often referred to western food and therefore gained little acceptance compared to rice-based traditional foods [40].
Limited knowledge
Limited knowledge describes the inability to implement given information, e.g. in the diet. Most information about food and cooking was designed based on western diets, and therefore leaves patients with unanswered questions regarding meal preparation and food choices [26]. Some participants described the amount of information on diabetes prevention as overwhelming and unrealistic for their daily lives [23, 24].
Other barriers
Another overarching barrier across groups was insufficient time, due for example to managing family-owned businesses with long workhours, or to family commitments such as childcare [41]. Furthermore, studies described problems with travel distance, e.g. to prevention courses or “food outlets” [42], or travel issues due to elevated age [41]. Insufficient personal motivation [23, 24, 36] was another common barrier.
Vulnerable groups and gender aspects
Only a single barrier and no facilitating factor was unique for one specific vulnerable group (language barrier for migrants). All other barriers and facilitating factors were identified at least once in each specific vulnerable group. Gender-specific perceptions were identified especially in the category ‘family and friends’. Male T2DM patients see family as a facilitator [43], whereas women more often describe family as a barrier due to childcare issues [36], insufficient diet compliance of the other family members [33], or culturally based reasons like shame of being seen in sportswear or going to the gym [36], or husbands not wanting their wives to go to the gym [44].
Discussion
In this scoping review, we were able to identify and categorize various barriers and facilitating factors in the prevention of T2DM/GDM in vulnerable groups. Most studies targeted only one vulnerable group, but some targeted mixed groups like “older migrants”. The three most common vulnerable groups within the 98 identified studies were “migrants”, “ethnic groups”, and “people with low socio-economic status”.
All eight categories of barriers and facilitating factors were identified within each vulnerable group apart from one (language barrier for migrants). The most common facilitating factors (family/friends, social support) are similar in each vulnerable group. The most common barriers were limited knowledge, family/friends, and economic factors. The differences between vulnerable groups with respect to te most common barriers were minimal. Only one category of barrier could be attributed to a single vulnerable group only (language barrier to migrants). Factors including insufficient motivation, cost of healthy food, or work are similar to those found in T2DM/GDM prevention designed for general high-risk population [45]. However, cultural or religious factors seem to be exclusive to vulnerable groups, and are important especially for migrants and ethnic groups.
It appears that barriers and facilitating factors between the vulnerable groups are similar, which should be taken into account when developing T2DM/GDM preventive interventions targeted at vulnerable groups. Still, the religious and cultural background of each vulnerable group needs to be considered separately, which may lead to different approaches for T2DM/GDM prevention in each vulnerable group.
Gender differences in the direction of certain factors require that women and men be approached in different ways for T2DM/GDM prevention. For families, lack of social support such as childcare could act as a barrier for parents to join preventive interventions. This could be addressed by providing childcare as part of the intervention, or by allowing children to join the intervention. Men could be further motivated e.g. by integrating their partners into the preventive intervention.
All barriers and facilitating factors identified to be relevant to vulnerable groups should be accounted for, either by adapting existing programs, or by developing new interventions specifically for vulnerable groups. Examples where this has already been implemented are the adaption of the National Diabetes Prevention Program (NDPP) to men with a low socio-economic status [46], and a culturally adapted lifestyle intervention among Iraqi immigrants in Sweden [47]. Straightforward options to modify existing interventions are translations, or adaptation to alternative food cultures such as rice-based diets. To address more complex aspects, such as the influence of family/friends or gender differences, it may be necessary to develop new preventive interventions for the target population.
Limitations
The publication date of included studies was limited to the past decade, because of the limited time frame available within the “National awareness and prevention strategy on diabetes in Germany”. The effect of this limitation is likely small, because barriers and facilitating factors reported in older studies are likely outdated in view of growing digitization. The eight categories for barriers and facilitating factors were predetermined. Therefore, some factors that did not fit into any category were classified post-hoc as “other barriers”, but it seems possible that alternative or additional categories, may have been relevant. The richness of the collected data warrants additional analyses (e.g. thematic analysis) that could be undertaken in the future, but were beyond the scope of this scoping review.
Conclusions
We identified various barriers and facilitating factors which should be considered in the development of future preventive interventions and adaption of existing interventions. Some general barriers and facilitating factors should be considered regardless of the presence of vulnerable groups, including economic factors and gender aspects. Religious and cultural factors, in particular, require different approaches for each vulnerable group.
Supporting information
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
We would like to thank Käthe Goossen for copyediting.
Abbreviations
- GDM
Gestational diabetes mellitus
- PPC
Population, Concept, Context
- T2DM
Type 2 diabetes mellitus
- WHO
World Health Organization
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study is funded by the Federal Center for Health Education. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. https://www.bzga.de/
References
- 1.Ogurtsova K, d.R.F J., Huang Y, Linnenkamp U, Guariguata L, Cho NH, et al. IDF Diabetes Atlas: Global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract, 2017. 128: p. 40–50. 10.1016/j.diabres.2017.03.024 [DOI] [PubMed] [Google Scholar]
- 2.Sullivan PW, M E., Ghushchyan V, Wyatt HR, Hill JO, Obesity, inactivity, and the prevalence of diabetes and diabetes-related cardiovascular comorbidities in the U.S., 2000–2002. Diabetes Care, 2005. 28: p. 1599–1603. 10.2337/diacare.28.7.1599 [DOI] [PubMed] [Google Scholar]
- 3.Pu J, Z B., Wang EJ, Nimbal V, Osmundson S, Kunz L, et al. Racial/Ethnic Differences in Gestational Diabetes Prevalence and Contribution of Common Risk Factors. Paediatr Perinat Epidemiol, 2015. 29(5): p. 436–43. 10.1111/ppe.12209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cefalu WT, B J., Tuomilehto J, Fleming GA, Ferrannini E, Gerstein HC, et al. Update and Next Steps for Real-World Translation of Interventions for Type 2 Diabetes Prevention: Reflections From a Diabetes Care Editors’ Expert Forum. Diabetes Care, 2016. 39(7): p. 1186–201. 10.2337/dc16-0873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Knowler W.B.-C E; Fowler SE; Hamman RF; Lachin JM; Walker EA; et al. , Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. The New England Journal of Medicine, 2002. 346(6): p. 393–403. 10.1056/NEJMoa012512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Connolly V, U N, Sherriff P, Bilous R, Kelly W, Diabetes prevalence and socioeconomic status: a population based study showing increased prevalence of type 2 diabetes mellitus in deprived areas. J Epidemiol Community Health, 2000. 54(3): p. 173–177. 10.1136/jech.54.3.173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schwartz N, N Z., Green MS, The prevalence of gestational diabetes mellitus recurrence—effect of ethnicity and parity: a metaanalysis. Am J Obstet Gynecol, 2015. 213(3): p. 310–7. 10.1016/j.ajog.2015.03.011 [DOI] [PubMed] [Google Scholar]
- 8.Patel N., et al. , Barriers and Facilitators to Healthy Lifestyle Changes in Minority Ethnic Populations in the UK: a Narrative Review. J Racial Ethn Health Disparities, 2017. 4(6): p. 1107–1119. 10.1007/s40615-016-0316-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grol R, G J., From best evidence to best practice: effective implementation of change in patients’ care. Lancet, 2003. 11(362(9391)): p. 1225–30. [DOI] [PubMed] [Google Scholar]
- 10.Breuing J.P D; Neuhaus AL; Heß S; Lütkemeier L; Haas F; et al. Barriers and facilitating factors in the prevention of diabetes type II and gestational diabetes in vulnerable groups: protocol for a scoping review. Systematic Review, 2018. 7(245): p. 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arksey H. a.O.M L., Scoping studies: towards a methodological framework. International Journal of Social Research Methodology, 2005. 8(1): p. 19–32. [Google Scholar]
- 12.Institute T.J B Joanna Briggs Institute Reviewers’ Manual: Methodology for JBI Scoping Reviews. 2015. [Google Scholar]
- 13.Tricco A.C.L E; Zarin W; O’Brien K.K; Colquhoun H; Levac D; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Annals of Internal Medicine, 2018. 169(7): p. 467–473. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 14.Organization, W.H. List of Member States by WHO region and mortality stratum. 1999; http://www.who.int/whr/2003/en/member_states_182-184_en.pdf. [Google Scholar]
- 15.Lewis V., K.L B., McClurg A., Goldman Boswell R., and Fisher E.S., The Promise And Peril Of Accountable Care For Vulnerable Populations: A Framework For Overcoming Obstacles. Health Affairs, 2012. 31(8): p. 1777–1785. 10.1377/hlthaff.2012.0490 [DOI] [PubMed] [Google Scholar]
- 16.McGowan J., S M., Salzwedel D.M., Cogo E., Foerster V., Lefebvre C., PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Explanation and Elaboration (PRESS E&E) Journal of Clinical Epidemiology, 2016. 75: p. 40–46. 10.1016/j.jclinepi.2016.01.021 [DOI] [PubMed] [Google Scholar]
- 17.Bandyopadhyay M., et al. , Lived experience of gestational diabetes mellitus among immigrant South Asian women in Australia. Australian and New Zealand Jouranl of Obstetrics and Gynaecology, 2011. 56: p. 360–364. [DOI] [PubMed] [Google Scholar]
- 18.Dayyani I., et al. , A qualitative study about the experiences of ethnic minority pregnant women with gestational diabetes. Scand J Caring Sci, 2019. 33(3): p. 621–631. 10.1111/scs.12655 [DOI] [PubMed] [Google Scholar]
- 19.Marquez D.X., et al. , Perspectives of Latina and non-Latina white women on barriers and facilitators to exercise in pregnancy. Women Health, 2009. 49(6): p. 505–21. 10.1080/03630240903427114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rhoads-Baeza M.E. and Reis J., An exploratory mixed method assessment of low income, pregnant Hispanic women’s understanding of gestational diabetes and dietary change. Health Education Journal, 2010. 71(1): p. 80–89. [Google Scholar]
- 21.Handley M.A., et al. , Applying the COM-B model to creation of an IT-enabled health coaching and resource linkage program for low-income Latina moms with recent gestational diabetes: the STAR MAMA program. Implement Sci, 2016. 11(1): p. 73 10.1186/s13012-016-0426-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oza-Frank R., et al. , Healthcare Experiences of Low-Income Women with Prior Gestational Diabetes. Matern Child Health J, 2018. 22(7): p. 1059–1066. 10.1007/s10995-018-2489-y [DOI] [PubMed] [Google Scholar]
- 23.Yee L.M., et al. , Social and Environmental Barriers to Nutrition Therapy for Diabetes Management Among Underserved Pregnant Women: A Qualitative Analysis. J Nutr Educ Behav, 2016. 48(3): p. 170–80 e1. 10.1016/j.jneb.2015.11.003 [DOI] [PubMed] [Google Scholar]
- 24.Yee L.M., et al. , Factors promoting diabetes self-care among low-income, minority pregnant women. J Perinatol, 2016. 36(1): p. 13–8. 10.1038/jp.2015.134 [DOI] [PubMed] [Google Scholar]
- 25.Patel V. and Iliffe S., An exploratory study into the health beliefs and behaviours of British Indians with type II diabetes. Primary Health Care Research & Development, 2017. 18: p. 97–103. [DOI] [PubMed] [Google Scholar]
- 26.Alzubaidi H., Mc Namara K., and Browning C., Time to question diabetes self-management support for Arabic-speaking migrants: exploring a new model of care. Diabet Med, 2017. 34(3): p. 348–355. 10.1111/dme.13286 [DOI] [PubMed] [Google Scholar]
- 27.Choi S.E., et al. , Spousal support in diabetes self-management among Korean immigrant older adults. Res Gerontol Nurs, 2015. 8(2): p. 94–104. 10.3928/19404921-20141120-01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bernstein A.M., et al. , Beliefs About Preventive Care, Individual Health, and Lifestyle Change Among Low-Income African American Women at Risk for Diabetes. Holist Nurs Pract, 2014. 28(1): p. 24–30. 10.1097/HNP.0000000000000006 [DOI] [PubMed] [Google Scholar]
- 29.Hempler N.F., et al. , Dietary education must fit into everyday life: a qualitative study of people with a Pakistani background and type 2 diabetes. Patient Prefer Adherence, 2015. 9: p. 347–54. 10.2147/PPA.S77380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Murrock C.J., Taylor E., and Marino D., Dietary challenges of managing type 2 diabetes in African-American women. Women Health, 2013. 53(2): p. 173–84. 10.1080/03630242.2012.753979 [DOI] [PubMed] [Google Scholar]
- 31.Gele A.A., et al. , Beyond Culture and Language: Access to Diabetes Preventive Health Services among Somali Women in Norway. J Diabetes Res, 2015. 2015: p. 549795 10.1155/2015/549795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Miller S.T., Marolen K.N., and Beech B.M., Perceptions of physical activity and motivational interviewing among rural African-American women with type 2 diabetes. Womens Health Issues, 2010. 20(1): p. 43–9. 10.1016/j.whi.2009.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Njeru J.W., et al. , Stories for change: development of a diabetes digital storytelling intervention for refugees and immigrants to minnesota using qualitative methods. BMC Public Health, 2015. 15: p. 1311 10.1186/s12889-015-2628-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nam S., et al. , Challenges of diabetes management in immigrant Korean Americans. Diabetes Educ, 2013. 39(2): p. 213–21. 10.1177/0145721713475846 [DOI] [PubMed] [Google Scholar]
- 35.Rosal M.C., et al. , Awareness of diabetes risk factors and prevention strategies among a sample of low-income Latinos with no known diagnosis of diabetes. Diabetes Educ, 2011. 37(1): p. 47–55. 10.1177/0145721710392247 [DOI] [PubMed] [Google Scholar]
- 36.Tang J.W., et al. , Perspectives on prevention of type 2 diabetes after gestational diabetes: a qualitative study of Hispanic, African-American and White women. Matern Child Health J, 2015. 19(7): p. 1526–34. 10.1007/s10995-014-1657-y [DOI] [PubMed] [Google Scholar]
- 37.Bhattacharya G., Spirituality and Type 2 Diabetes Self-Management Among African Americans in the Arkansas Delta. Jouranl of Social Service Research, 2013. 39(4): p. 469–482. [Google Scholar]
- 38.Sohal P.S., Prevention and Management of Diabetes in South Asians. 32, 2008. 3: p. 206–210. [Google Scholar]
- 39.Yilmaz-Aslan Y., et al. , Illness perceptions in Turkish migrants with diabetes: a qualitative study. Chronic Illn, 2014. 10(2): p. 107–21. 10.1177/1742395313501207 [DOI] [PubMed] [Google Scholar]
- 40.Moise R.K., et al. , Diabetes Knowledge, Management, and Prevention Among Haitian Immigrants in Philadelphia. Diabetes Educ, 2017. 43(4): p. 341–347. 10.1177/0145721717715418 [DOI] [PubMed] [Google Scholar]
- 41.Cha E., et al. , Understanding cultural issues in the diabetes self-management behaviors of Korean immigrants. Diabetes Educ, 2012. 38(6): p. 835–44. 10.1177/0145721712460283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chaufan C., Constantino S., and D M., ‘It’s a full time job being poor’: understanding barriers to diabetes prevention in immigrant communities in the USA. Critical Public Health, 2012. 22(2): p. 147–158. [Google Scholar]
- 43.Chlebowy D.O., Hood S., and LaJoie A.S., Facilitators and barriers to self-management of type 2 diabetes among urban African American adults: focus group findings. Diabetes Educ, 2010. 36(6): p. 897–905. 10.1177/0145721710385579 [DOI] [PubMed] [Google Scholar]
- 44.Khanam S., Attitudes towards health and exercise of overweight women. The Journal of The Royal Society for the Promotion of Health, 2008. 128(1): p. 26–30. 10.1177/1466424007085225 [DOI] [PubMed] [Google Scholar]
- 45.Booth A.L C; Dean M; Hunter S.J.; McKinley M.C.;, Diet and physical activity in the self-management of type 2 diabetes: barriers and facilitators identified by patients and health professionals. Primary Health Care Research & Development, 2013. 14: p. 293–306. [DOI] [PubMed] [Google Scholar]
- 46.Gary-Webb T.L., et al. , Translation of the National Diabetes Prevention Program to Engage Men in Disadvantaged Neighborhoods in New York City: A Description of Power Up for Health. Am J Mens Health, 2018. 12(4): p. 998–1006. 10.1177/1557988318758788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Siddiqui F.W V.; Kurbasic A.; Sonestedt E.; Lundgren K.B.; Lindeberg S.; Nilsson P.M.; et al. , Changes in dietary intake following a culturally adapted lifestyle intervention among Iraqi immigrants to Sweden at high risk of type 2 diabetes: a randomised trial. Public Health Nutrition, 2017. 20(15): p. 2827–2838. 10.1017/S136898001700146X [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.