To the Editor
Although the main mechanism of coronavirus disease (COVID-19) transmission is droplet spreading, there are concerns about aerosol-generating procedures such as extubation.1 There are some suggestions from around the world proposing the placement of large transparent plastic sheets over patients’ faces to limit the contamination area.2,3 Therefore, we compared the effectiveness and spreading patterns of acrylic boxes and plastic sheets as protective barriers compared to noncoverage technique under fluorescent condition.
To simulate coughing during tracheal extubation, we intubated the airway of a manikin with an endotracheal tube, size 7.0, with 21 cm depth. We designed a droplet generating device that would simulate a cough with an estimated velocity of 4–10 m/s. A tubing was then connected to the pressure generator and the tip of the nozzle was fixated at the midline in the oral cavity. One milliliter of fluorescent alcohol was then injected through the device as a simulated mass of secretion and droplets. Three different configurations of clear acrylic boxes were used and are illustrated in the Supplemental Digital Content, Figure 1, http://links.lww.com/AA/D105. The transparent plastic sheet used was 115 ×100 cm.
The dispersion of droplets was counted by the number of stained squares only outside the boxes and not as the number of glow spots in each square. We recorded from 3 areas: (a) around the manikin, (b) on the chest of the manikin, and (c) on the anesthesia personnel’s gown and face shield. To systematically document the dispersion outside the boxes, each area was divided differently into columns and rows. A total of 300 measurement squares measuring 5 ×5 cm were created. The incidence of self-contamination was counted and recorded. Each technique was simulated and recorded for 5 consecutive times under fluorescent condition in a darkened research room.
We demonstrated the differences of overall droplet dispersion between 3 acrylic box models (3.3%–19.0%), plastic sheet (2.8%), and noncoverage technique (26.3%) during tracheal extubation. All acrylic boxes showed no contamination on anesthesia personnel. The plastic sheet caused contamination both on the chest and abdomen of anesthesia personnel. Regardless of the technique, the contamination area was more prominent on the right side of the table. Using any box during extubation demonstrated no contamination along the upper border of the table. The spreading pattern of all techniques isshown in theFigure, panels A–E.
Figure.
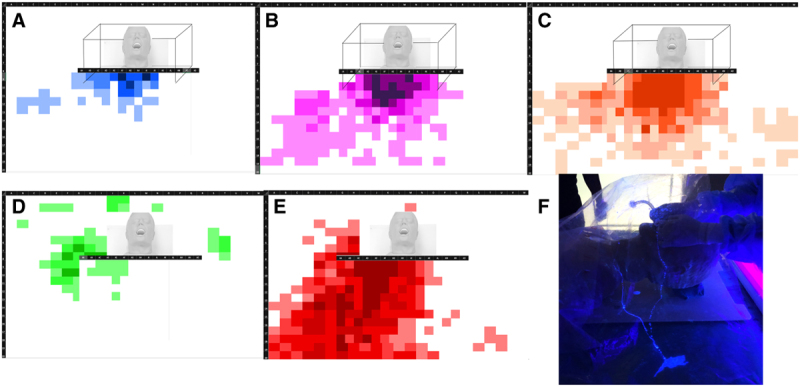
The droplet spreading patterns of panels (A), (B), (C), transparent plastic sheet (D), and noncoverage technique (E). F, The volcano eruption-like effect and the uncontrollable lava flow under the sheet.
The advantages of using an acrylic box to reduce droplet dispersal are the ease of use and its rigid structure which limits the spreading.4 However, higher cost and cleaning procedures can be disadvantageous. Moreover, using different models resulted in different protective outcomes as we proposed. This could be due to the individual design of each box (eg, the top [slope or flat]), the presence of a side-door opening and awning, and hand slots. The height of the box might take part in the contamination area as the droplet dispersion may rebound to the surroundings after striking the top. The slope top can also affect the contamination area. Uncontrollable dispersed flow against the slope top might cause the rebounding of secretion to the hand slots. The side door may cause more contamination if it is opened for airway management assistance. Therefore, we recommend to open the door as necessary for shortest time as possible. Also, if the box is completely wrapped with plastic sheet at both hand slots and around caudal-opening space, the risk of contamination should be diminished as it becomes a nearly closed system.
There are several concerns when using an acrylic box during airway intervention. First, the cleaning methods are still inconclusive, leading to cross-contamination. Second, the hand slots limit hand movement for complicated airway procedures. Thus, suspected difficult airway cases should be evaluated cautiously and personnel should be adequately trained before use. Third, if the patient is agitated or not cooperative, there is a risk of minor trauma.
Using a plastic sheet also resulted in less contamination in the manikin.5 The advantages of a plastic sheet are disposability, lower cost, and less restriction to hand movement.6 However, we demonstrated self-contamination toward the extubator. Although we used only 1 mLof fluorescent fluid, the cough flow spread varied widely under the plastic sheet and toward the opposite side of the extubation attendant which was similar to how lava flows from volcanic eruptions (Figure, panels F). Furthermore, improper discarding of the plastic cover sheet can lead to cross-contamination of the health care workers.
Therefore, the discussed protective tools are helpful in decreasing contamination from droplet dispersion. It is essential to consider all aspects, including limitations, before use, and these barriers do not substitute standard personal protective equipment (PPE) and universal precautions.
ACKNOWLEDGMENTS
We appreciate the contributions to this studyfrom the following: Administrators of Simulation and cardiopulmonary resuscitation center (CPR) center of King Chulalongkorn Memorial Hospital, who gave their time and effort, and Paulo R. C. Dalpian, PhD, for proofreading this document.
Supplementary Material
Prok Laosuwan, MD
Athitarn Earsakul, MD
Patt Pannangpetch, MD
Jariya Sereeyotin, MD
Department of Anesthesiology
King Chulalongkorn Memorial Hospital
Thai Red Cross Society and Faculty of Medicine
Chulalongkorn University
Bangkok, Thailand
jsereeyotin@gmail.com
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website.
REFERENCES
- 1.Chen X, Liu Y, Gong Y, Guo X, Zuo M, Li J, et al. Perioperative management of patients infected with the novel coronavirus: recommendation from the Joint Task Force of the Chinese Society of Anesthesiology and the Chinese Association of Anesthesiologists. Anesthesiology. 2020. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Australian Society of Anaesthetists. Anaesthesia and caring for patients during the COVID-19 outbreak. Available at: https://www.asa.org.au/wordpress/wp-content/uploads/News/eNews/covid-19/ASA_airway_management.pdf. Accessed April 12, 2020.
- 3.Nebraska Medicine and the University of Nebraska Medical Center. Guidelines for Patients with COVID-19 Suspected or Confirmed Infection in the Perioperative Environment. Available at. https://www.nebraskamed.com/sites/default/files/documents/covid-19/guidelines-for-patients-with-covid-in-the-perioperative-environment.pdf. Accessed April 12, 2020.
- 4.Canelli R, Connor CW, Gonzalez M, Nozari A, Ortega R. Barrier Enclosure during endotracheal intubation. N Engl J Med. 2020. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Matava CT, Yu J, Denning S. Clear plastic drapes may be effective at limiting aerosolization and droplet spray during extubation: implications for COVID-19. Can J Anaesth. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brown S, Patrao F, Verma S, Lean A, Flack S, Polaner D. Barrier system for airway management of COVID-19 patients. Anesth Analg. 2020. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


