To the Editor
We read with interest the articles by Brown et al,1 Lai and Chang,2 Tsai,3 and Babazade et al.4 These articles describe barrier devices for potentially reducing aerosol and droplet transmission in Coronavirus Disease 2019 (COVID-19) patients. Brown et al1 and Babazade et al4 describe the use of plastic drapes, whereas Lai and Chang2 andTsai3 describe rigid box designs.1–4 Although these designs are innovative, they do suffer from some important drawbacks. Rigid box designs significantly limit forearm and hand movements and might require some practice to achieve competence in use.2,3 In addition, the rigid design forces assistants to stand far off to the side of the patient, which limits help with airway management and doesnotoffer them the same protection provided to the laryngoscopist. These designs can require initial elaborate construction, such as Tsai’s3 design. Lai and Chang’s2 design, although less elaborate in construction, lacks transparency of other models, possibly making its use even more challenging.2 Reusable designs of Tsai3 might also have the added issue of having to be decontaminated, which might be a problem in nonmedical grade devices.3 Plastic drape cover designs of Brown et al1 and Babazade et al4 have the advantage of being inexpensive, commonly available, quick to produce, and disposable.1,4 They also have multiple access points for assistance;however, the weight of the plastic drape on proceduralist’s hands still might be an issue when performing procedures under the device. The plastic drape is also quite close to the patient's face and this might not be tolerated by some patients.
To overcome some of these limitations, we constructed a hood to encase the patient’s head during procedures (Figure). It consists of a surgical Mayo stand without the tray and a clear plastic drape allowing clear visualization of the patient’s head and neck. The plastic drape is a C-arm drape cut along a side seam and the bottom, forming a large sheet of clear plastic. This can be draped over the Mayo stand.
Figure.
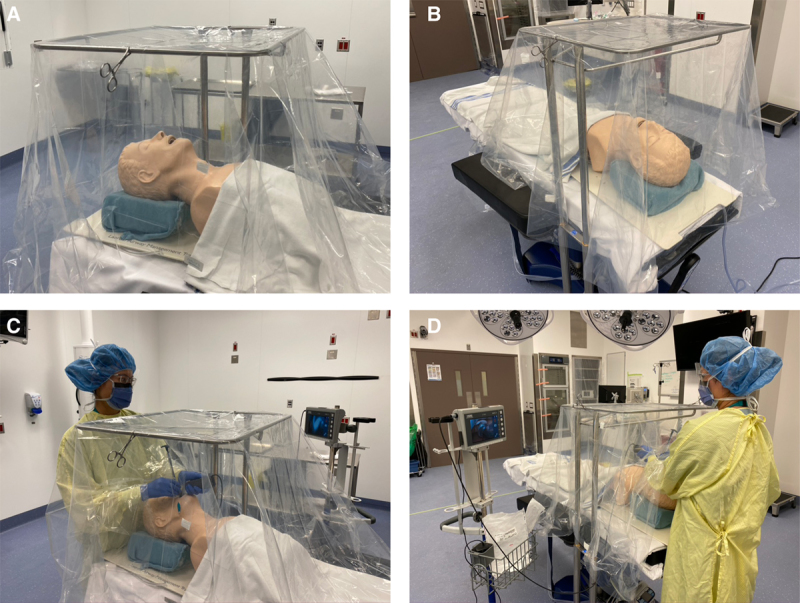
A and B, The hood design from different angles. C and D, The hood design with a clinician performing a simulated intubation.
We tested our device with Glo-Germs administered using a MADgic Laryngo-Tracheal Mucosal Atomization Device to simulate the production of fine droplets and aerosol. When utilizing the hood, visible Glo-Germ spread was confined to the clinician’s hands, forearms, intubating manikin’s head, neck, and the operating table covered by the hood. Without the hood, Glo-Germ could be identified on the laryngoscopist’s hands, entire arms, gown, neck, face, eye protection, mask, and more extended spread around the operating room. As standard masks were used, we also noticed an interesting qualitative difference when the hood was used. Fine droplet Glo-Germ produce a distinctive smell when aerosolized, and this was noticed by the laryngoscopist only when the hood was not used.
We believe our hood maintains the advantages of the barrier design with it offering adequate space around a patient’s head and neck for both the laryngoscopist and assistant to provide effective airway management from preoxygenation to extubation. Additional simulation studies as well as studies involving aerosol behavior in relation to the barrier devices are warranted. Such data will allow more confident approaches to techniques meant at providing protection during airway management.
Ryan Vincent William Endersby, MD, FRCPC
Esther Ching Yee Ho, MD, FRCPC
Adam Oscar Spencer, MD, MSc, FRCPC
David Howard Goldstein, MB, BCh, BAO, MSc FRCPC
Edward Schubert, MD, FRCPC
Department of Anesthesia, Perioperative and Pain Medicine
University of Calgary
South Health Campus
Calgary, Alberta, Canada
ryan.endersby@gmail.com
Footnotes
Conflicts of Interest: Dr R. V. W. Endersby and Dr A. O. Spencer have received an honorarium from Heron Therapeutics for consultant work.
REFERENCES
- 1.Brown S, Patrao F, Verma S, Lean A, Flack S, Polaner D. Barrier system for airway management of COVID-19 patients. Anesth Analg. 2020;xx:xx–xx. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lai Y, Chang C. A carton-made protective shield for suspicious/confirmed COVID-19 intubation and extubation during surgery. Anesth Analg. 2020;xx:xx–xx. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tsai P. Barrier shields. Anesth Analg. 2020;xx:xx–xx. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Babazade R, Khan E, Ibrahim M, Simon M, Vadhera R. Additional barrier to protect healthcare workers during intubation. Anesth Analg. 2020;xx:xx–xx. [DOI] [PMC free article] [PubMed] [Google Scholar]


