Abstract
Background:
Studies of the novel coronavirus-induced disease COVID-19 in Wuhan, China, have elucidated the epidemiological and clinical characteristics of this disease in the general population. The present investigation summarizes the clinical characteristics and early prognosis of COVID-19 infection in a cohort of patients with fractures.
Methods:
Data on 10 patients with a fracture and COVID-19 were collected from 8 different hospitals located in the Hubei province from January 1, 2020, to February 27, 2020. Analyses of early prognosis were based on clinical outcomes and trends in laboratory results during treatment.
Results:
All 10 patients presented with limited activity related to the fracture. The most common signs were fever, cough, and fatigue at the time of presentation (7 patients each). Other, less common signs included sore throat (4 patients), dyspnea (5 patients), chest pain (1 patient), nasal congestion (1 patient), headache (1 patient), dizziness (3 patients), abdominal pain (1 patient), and vomiting (1 patient). Lymphopenia (<1.0 × 109 cells/L) was identified in 6 of 10 patients, 9 of 9 patients had a high serum level of D-dimer, and 9 of 9 patients had a high level of C-reactive protein. Three patients underwent surgery, whereas the others were managed nonoperatively because of their compromised status. Four patients died on day 8 (3 patients) or day 14 (1 patient) after admission. The clinical outcomes for the surviving patients are not yet determined.
Conclusions:
The clinical characteristics and early prognosis of COVID-19 in patients with fracture tended to be more severe than those reported for adult patients with COVID-19 without fracture. This finding may be related to the duration between the development of symptoms and presentation. Surgical treatment should be carried out cautiously or nonoperative care should be chosen for patients with fracture in COVID-19-affected areas, especially older individuals with intertrochanteric fractures.
Level of Evidence:
Prognostic Level IV. See Instructions for Authors for a complete description of levels of evidence.
Since December 2019, a new coronavirus disease, COVID-19, has been spreading in China, particularly in the city of Wuhan, Hubei province. Several studies have identified common characteristics of COVID-19-associated pneumonia, including epidemiological, demographic, clinical, laboratory, radiographic, and treatment data1-5. The severe acute respiratory syndrome coronavirus (SARS-CoV-2) has been classified as the β-coronavirus 2b lineage and has characteristics typical of the coronavirus family6. A recent study demonstrated that SARS-CoV-2 is very similar to another coronavirus carried by bats, leading to speculation that the novel virus may be hosted in bats7. Current evidence suggests that wild animals illegally traded in the Huanan Seafood Wholesale Market were the likely culprit of the spread of the virus among humans8.
It is well established that patients with fractures are susceptible to pulmonary infection, especially those with lower-limb fracture and limited ambulatory capacity9. It has been reported that COVID-19 infections are clustered within groups of individuals in close contact in places such as supermarkets, public transportation, and hospitals10. Patients with severe fractures often require hospitalization and surgical treatment, making this population susceptible to COVID-19 infection. Thus, the question arises concerning the best medical practices for patients who have both fracture and COVID-19 infection at the time of presentation. There is an urgent need to determine whether patients with fracture who are affected by COVID-19 have a higher risk of mortality because of the infection. The purpose of the present retrospective study was to analyze the clinical data for 10 hospitalized patients with both a fracture and COVID-19 infection and to identify the most appropriate management strategy.
Materials and Methods
Study Design and Participants
A retrospective review of the medical records of 10 patients with both a bone fracture and COVID-19 infection was performed. The patients were admitted to Wuhan Union Hospital, Wuhan General Hospital of Guangzhou Military Command, Hubei Hospital of Traditional Chinese Medicine, Dongxihu District People’s Hospital of Wuhan City, Wuhan Pu’ai Hospital, Hanyang University Hospital, Taihe Hospital of Shiyan City, and Ezhou Central Hospital between January 1, 2020, and February 27, 2020. COVID-19 was diagnosed in accordance with the New Coronavirus Pneumonia Prevention and Control Program, 6th edition, published by the National Health Commission of China11. Importantly, to eliminate the potential missed cases of COVID-19, clinical diagnosis was added in the 5th edition of the New Coronavirus Pneumonia Prevention and Control Program, which stipulated that a suspected case with an evident radiological manifestation should be identified as a confirmed case of COVID-1912. Six of the 10 patients were positive for SARS-CoV-2 on the basis of quantitative reverse transcription polymerase chain reaction (qRT-PCR) of throat swab samples. Of the remaining 4 patients, 3 had a negative result and 1 did not receive the qRT-PCR test during her hospitalization. All patients presented with clear evidence of viral pneumonia on computed tomography (CT) scans. Informed consent was obtained from all participants before enrollment in the study.
Data Collection
Primary data included clinical characteristics, signs and symptoms, results of laboratory tests, evidence of COVID-19 infection, treatment, and clinical outcome. The medical records were provided by the 8 participating hospitals and were analyzed at the Department of Orthopedics, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, with use of a customized data-collection form. Throat swab samples were obtained from patients who were identified as having a suspected COVID-19 infection and were analyzed by qRT-PCR with use of a kit recommended by the Chinese Center for Disease Control and Prevention (CDC) according to the World Health Organization (WHO) guidelines. Total RNA was extracted from throat swabs with use of the RNA isolation kit (Zhongzhi) and was reverse-transcribed with use of the One Step RT-PCR Kit (Takara). Primers were designed on the basis of the Wuhan-Hu-1 sequence (MN908947) to amplify part of the sequence of the S segment (nt 21730-22458). The primer sequences were 5′-CTCAGGACTTGTTCTTACCTT-3′ and 5′-CAAGTGCACAGTCTACAGC-3′. The clinical outcomes were assessed at the follow-up examination on February 27, 2020.
Statistical Analysis
SPSS software (version 23.0; IBM) was used for statistical analysis of primary data. Categorical variables are presented as the median and interquartile range or as the number and percentage. Diagrams of curves were drawn with use of Prism (version 8.3; GraphPad).
Results
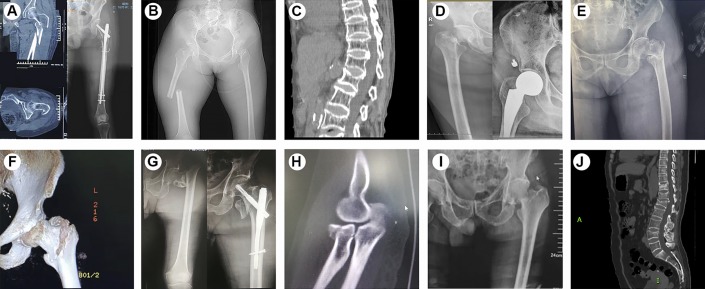
The 10 patients (8 women and 2 men) ranged from 34 to 87 years of age (Table I). All of the fractures had been caused by accidents. Nine of the 10 patients had sustained the fracture in a low-velocity accident, and 1 patient (Case 9) had sustained the fracture as well as a brain injury as the result of a high-velocity (traffic) accident (see Appendix Table I). Seven of the 10 patients had a nosocomial infection, whereas 3 patients had contracted COVID-19 before admission to the hospital for the treatment of the fracture. The orthopaedic diagnosis was based on a radiograph or 3-dimensional CT scan (Fig. 1). Nine of the 10 patients were exposed to SARS-CoV-2 either by contact with an infected individual or by direct exposure in a contagious environment. Three patients had osteoporosis along with an underlying disease such as hypertension, diabetes, and chronic obstructive pulmonary disease (COPD). Three patients (Cases 1, 4, and 7) did not exhibit severe symptoms or have obvious evidence of the disease on CT scans on admission and therefore underwent a surgical procedure; fever and fatigue signs were observed after the operation.
Fig. 1.
Figs. 1-A through 1-J CT scans and radiographs showing the fractures in the present study. Fig. 1-A Case 1. Preoperative CT scan showing an intertrochanteric fracture and postoperative radiograph. Fig. 1-B Case 2. Preoperative radiograph showing a femoral fracture. Fig. 1-C Case 3. Preoperative CT scan showing a lumbar fracture. Fig. 1-D Case 4. Preoperative and postoperative radiographs for a patient with a femoral neck fracture. Fig. 1-E Case 5. Preoperative radiograph showing an intertrochanteric fracture. Fig. 1-F Case 6. Preoperative CT scan showing an intertrochanteric fracture. Fig. 1-G Case 7. Preoperative and postoperative radiographs for a patient with an intertrochanteric fracture. Fig. 1-H Case 8. Preoperative CT scan showing a fracture of the radius. Fig. 1-I Case 9. Preoperative radiograph showing an intertrochanteric fracture. Fig. 1-J Case 10. Preoperative CT scan showing a thoracolumbar fracture.
TABLE I.
Clinical Characteristics of 10 Patients with Fracture*
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | Case 8 | Case 9 | Case 10 | Total No. of Patients with Finding | |
| Clinical characteristics | |||||||||||
| Sex, age (yr) | F, 50 | F, 34 | F, 87 | F, 79 | F, 80 | F, 84 | M, 76 | F, 55 | M, 85 | F, 54 | — |
| Date of admission | Jan 2, 2020 | Jan 31, 2020 | Jan 13, 2020 | Jan 19, 2020 | Jan 20, 2020 | Jan 30, 2020 | Jan 17, 2020 | Feb 3, 2020 | Jan 16, 2020 | Feb 12, 2020 | — |
| Orthopaedic diagnosis | Intertrochanteric fracture | Femoral fracture | Lumbar fracture | Femoral neck fracture | Intertrochanteric fracture | Intertrochanteric fracture | Intertrochanteric fracture | Fracture of radius | Intertrochanteric fracture | Thoracolumbar fracture | — |
| Epidemiological history | Yes (exposure to relevant environment) | Yes (exposure to relevant environment) | Yes (exposure to relevant environment) | Yes (exposure to relevant environment) | Yes (exposure to relevant environment) | Yes (contact with infected person) | Yes (exposure to relevant environment) | Yes (exposure to relevant environment) | No | Yes (exposure to relevant environment) | 9 |
| Complications | Hypertension, diabetes | No | COPD, osteoporosis | Osteoporosis | Hypertension, diabetes, CAHD | Hypertension, osteoporosis | Cirrhosis, Alzheimer disease | No | Brain injury | Hypertension, diabetes | — |
| Orthopaedic operation | Jan 9, 2020 | No | No | Jan 21, 2020 | No | No | Jan 20, 2020 | No | No | No | 3 |
| Signs and symptoms | |||||||||||
| Fever | Yes | No | No | Yes | Yes | Yes | Yes | No | Yes | Yes | 7 |
| Cough | Yes | No | No | Yes | Yes | Yes | Yes | Yes | Yes | No | 7 |
| Fatigue | Yes | No | No | No | Yes | Yes | Yes | Yes | Yes | Yes | 7 |
| Sore throat | No | No | No | No | Yes | No | Yes | Yes | Yes | No | 4 |
| Dyspnea | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | 5 |
| Chest pain | No | No | No | No | Yes | No | No | No | No | No | 1 |
| Nasal congestion | No | No | No | No | Yes | No | No | No | No | No | 1 |
| Headache | No | No | No | No | Yes | No | No | No | No | No | 1 |
| Dizziness | No | No | No | No | Yes | Yes | No | Yes | No | No | 3 |
| Diarrhea | No | No | No | No | No | No | No | No | No | No | 0 |
| Abdominal pain | No | No | Yes | No | No | No | No | No | No | No | 1 |
| Vomiting | No | No | Yes | No | No | No | No | No | No | No | 1 |
| Limited activity | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 10 |
| Laboratory test results† | |||||||||||
| White blood-cell count (×109/L) | 13.45 (↑↑) | 4.93 | 21.9 (↑↑) | 12.37 (↑↑) | 6.43 | 6.95 | 9.6 | 4.23 | 11.27 (↑↑) | 5.21 | 4 |
| Neutrophil count (×109/L) | 11.25 (↑↑) | 3.7 | 20.4 (↑↑) | 11.45 (↑↑) | 5.24 | 4.98 | 7.48 | 3.04 | 10.06 (↑↑) | 3.6 | 4 |
| Lymphocyte count (×109/L) | 1.44 | 0.83 (↓↓) | 0.8 (↓↓) | 0.59 (↓↓) | 0.47 (↓↓) | 1.11 | 1.48 | 0.93 (↓↓) | 0.46 (↓↓) | 1.09 | 6 |
| Monocyte count (×109/L) | 0.58 | 0.33 | 0.8 (↑) | 0.33 | 0.5 | 0.85 (↑) | 0.64 (↑) | 0.24 | 0.72 (↑) | 0.33 | 4 |
| Platelet count (×109/L) | 213 | 157 | 144 | 153 | 291 | 178 | NA | 189 | 106 (↓) | 167 | 1 |
| APTT (s) | 146.7 (↑) | 26.4 (↓) | 38.3 | 31.2 | 30.3 | 31.76 | 32.2 | 29.8 | 35.5 | 38.5 | 1, 1 |
| PT (s) | 75.9 (↑) | 12.4 | 13.9 | 10.3 (↓) | 12.2 | 12.95 | 13.9 | 10.4 (↓) | 13.4 | 12.8 | 1, 2 |
| D-dimer (mg/L) | 5.32 (↑) | NA | 12.45 (↑) | 12.45 (↑) | 2.35 (↑) | 5.23 (↑) | 1,622 (↑) | 1,155 (↑) | 17.02 (↑) | 6.73 (↑) | 9 |
| Albumin (g/L) | 28.7 (↓) | 33.9 (↓) | 34 (↓) | 39.8 | 33.4 (↓) | 33.8 (↓) | 28.4 (↓) | 38.6 | 37.1 | 40.6 | 6 |
| ALT (U/L) | 0 | 20 | 15 | 15 | 10 | 42 (↑) | 15 | 5 | 18 | 36 (↑) | 2 |
| AST (U/L) | 12 | 46 (↑) | 35 | 29 | 21 | 64 (↑) | 38 | 20 | 27 | 33 | 2 |
| Total bilirubin (μmol/L) | 7.7 | 9.1 | 18.8 | 6.8 | 9.2 | 14 | 41.8 (↑) | 10 | 10.3 | 18 | 1 |
| Blood urea nitrogen (mmol/L) | 13.44 (↑) | 5.43 | 18.8 (↑) | 6.0 | 2.98 | 10.68 (↑) | 17.79 (↑) | 3.8 | 6.8 | 3.19 | 4 |
| Creatinine (μmol/L) | 419.3 (↑) | 42 (↓) | 298 (↑) | 42 (↓) | 136 (↑) | 104 | 78 | 37 (↓) | 88 | 55.5 | 3, 3 |
| Procalcitonin (ng/mL) | NA | 0.009 | 19.05 (↑) | 0.219 (↑) | 0.15 (↑) | 0.74 (↑) | 0.23 (↑) | NA | 2.35 (↑) | 0.41 (↑) | 7 |
| C-reactive protein (mg/L) | 156.9 (↑) | 6.8 (↑) | 33 (↑) | 96 (↑) | 18.9 (↑) | 14.5 (↑) | NA | 13.12 (↑) | 16.4 (↑) | 11.4 (↑) | 9 |
| Evidence of COVID-19 | |||||||||||
| SARS-CoV-2 quantitative RT-PCR | Negative | Negative | NA | Positive | Negative | Positive | Positive | Positive | Positive | Positive | 6 |
| Typical signs of viral infection on CT | Bilateral | Unilateral | Bilateral | Bilateral | Bilateral | Bilateral | Bilateral | Bilateral | Bilateral | Bilateral | 10 |
| Treatment | |||||||||||
| Oxygen inhalation | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 9 |
| Antiviral therapy | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 10 |
| Antibacterial therapy | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 10 |
| Intravenous immunoglobulin therapy | Yes | No | No | No | Yes | No | Yes | No | No | No | 3 |
| Glucocorticoid therapy | Yes | No | No | Yes | No | Yes | No | No | Yes | No | 4 |
| CKRT | Yes | No | No | No | No | No | No | No | No | No | 1 |
| NIV | No | No | Yes | No | Yes | No | Yes | No | No | No | 3 |
| IMV | No | No | No | No | No | No | No | No | No | No | 0 |
| ECMO | No | No | No | No | No | No | No | No | No | No | 0 |
| Co-infection | Coxsackie virus | No | No | Epstein-Barr virus | No | No | Candida | No | No | No | 3 |
| Clinical outcome | Remained in hospital | Remained in hospital | Died on Jan 21, 2020 | Remained in hospital | Remained in hospital | Died on Feb 7, 2020 | Died on Jan 31, 2020 | Remained in hospital | Died on Jan 24, 2020 | Remained in hospital |
COPD = chronic obstructive pulmonary disease, CAHD = coronary atherosclerosis heart disease, CKRT = continuous kidney replacement therapy, NIV = noninvasive ventilation, IMV = invasive mechanical ventilation, ECMO = extracorporeal membrane oxygenation, NA = not available.
White blood-cell count: normal range, 3.5 to 9.5 × 109/L, (↑↑) indicates leukocytosis (>10.0 × 109/L). Neutrophil count: normal range, 1.8 to 6.3 × 109/L, (↑↑) indicates neutrophilic granulocytosis (>7.5 × 109/L). Lymphocyte count: normal range, 1.1 to 3.2 × 109/L, (↓↓) indicates lymphopenia (<1.0 × 109/L). For the remaining laboratory values, the normal ranges are as follows: monocyte count, 0.1 to 0.6 × 109/L; platelet count, 125 to 350 × 109/L; APTT, 28.0 to 43.5 s; PT, 11.0 to 16.0 s; D-dimer, <0.5 mg/L FEU (fibrinogen equivalent units); albumin, 35 to 55 g/L; alanine aminotransferase (ALT), 5 to 35 U/L; aspartate aminotransferase (AST), 8 to 40 U/L; total bilirubin, 5.1 to 19.0 μmol/L; blood urea nitrogen, 2.9 to 8.2 mmol/L; creatinine, 44.0 to 106.0 μmol/L; procalcitonin, <0.05 ng/mL; C-reactive protein, 0 to 5 mg/L. For those values, (↑) or (↓) indicates an increase or decrease compared with the normal level.
Given the presence of fracture, all patients had limited function on the injured side. Seven patients each (70%) reported fever, cough, and fatigue; 4 (40%) had a sore throat; 5 (50%) presented with dyspnea; and 3 (30%) had dizziness. One patient (Case 5) (10%) reported chest pain, nasal congestion, and headache, and 1 patient (Case 3) (10%) reported abdominal pain and vomiting. No patient presented with diarrhea.
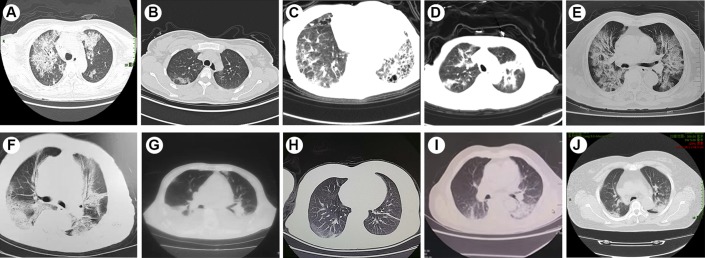
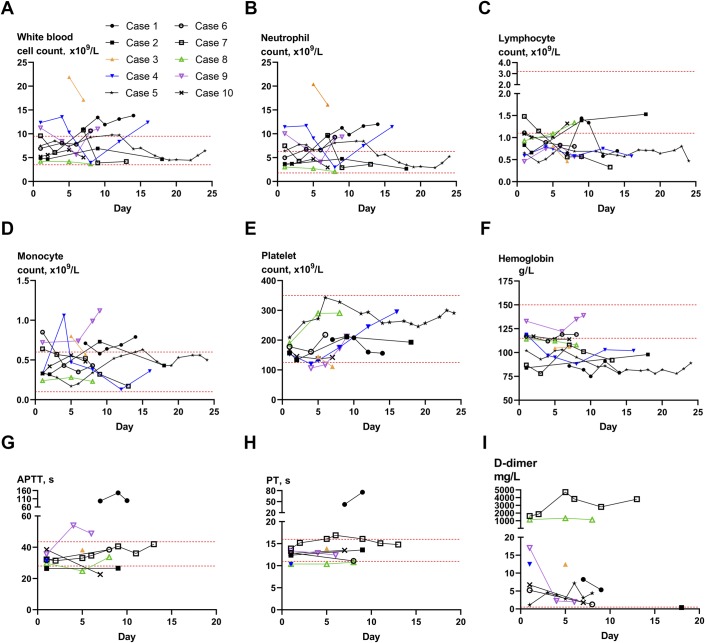
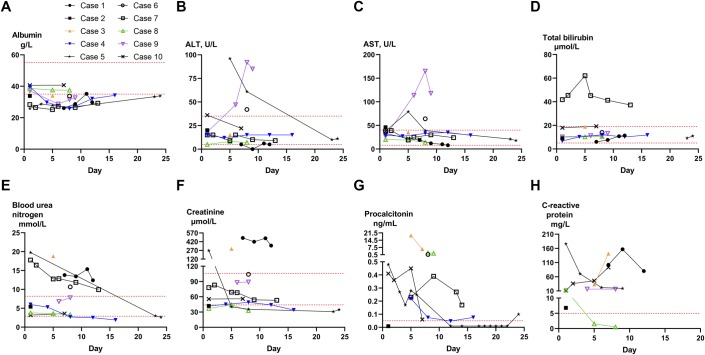
The results of laboratory tests are also shown in Table I. Four patients had leukocytosis (>10.0 × 109 cells/L), and 6 had lymphopenia (<1.0 × 109 cells/L). Additionally, 4 patients had neutrophilic granulocytosis (>7.5 × 109 cells/L) and 4 patients had an increased count of monocytes (>0.6 × 109 cells/L). Blood coagulation assays showed normal activated partial thromboplastin time (APTT) in 8 patients (80%) and normal prothrombin time (PT) in 7 patients (70%). However, because of limited activity, 9 (100%) of 9 patients had an abnormal level of D-dimer, which reached 1,155 mg/L in 1 case. Six (60%) of 10 patients had a low level of albumin because of their poor condition. Most patients had normal levels of alanine aminotransferase (ALT) (8 patients; 80%), aspartate aminotransferase (AST) (8 patients; 80%), total bilirubin (9 patients; 90%), and blood urea nitrogen (6 patients; 60%). The level of creatinine was higher than normal in 3 patients and lower than normal in 3 patients. Seven (88%) of 8 patients had an elevated procalcitonin concentration, and 9 (100%) of 9 patients had a high level of C-reactive protein. While only 6 patients (60%) tested positive for SARS-CoV-2, CT imaging demonstrated unilateral or bilateral patchy consolidation or ground-glass opacities in all patients (Fig. 2). Therefore, according to the New Coronavirus Pneumonia Prevention and Control Program (6th edition), all patients were considered or highly suspected to have COVID-19. The timing of typical signs of viral infection on CT scans (discrete ground-glass opacities in specific areas of the lung) and the timing of relevant positive SARS-CoV-2 qRT-PCR tests are listed in Appendix Table I. The detailed changes in routine blood test results, coagulation function, blood biochemistry, and infection-related biomarkers were collected starting from the date of admission (Figs. 3 and 4).
Fig. 2.
Figs. 2-A through 2-J Chest CT scans for all 10 patients. All patients but 1 had bilateral patchy consolidation and multiple ground-glass opacities. The remaining patient (Case 2) had ground-glass opacities on the right side. Fig. 2-A Case 1. Fig. 2-B Case 2. Fig. 2-C Case 3. Fig. 2-D Case 4. Fig. 2-E Case 5. Fig. 2-F Case 6. Fig. 2-G Case 7. Fig. 2-H Case 8. Fig. 2-I Case 9. Fig. 2-J Case 10.
Fig. 3.
Line graphs illustrating detailed changes in routine blood test results and coagulation function for all 10 patients, starting on the day of disease onset (Case 1) or the day of admission (Cases 2 through 9). The normal ranges of laboratory test results are as follows: white blood-cell count, 3.5 to 9.5 × 109/L; neutrophil count, 1.8 to 6.3 × 109/L; lymphocyte count, 1.1 to 3.2 × 109/L; monocyte count, 0.1 to 0.6 × 109/L; platelet count, 125 to 350 × 109/L; hemoglobin, 115 to 150 g/L; APTT, 28.0 to 43.5 s; PT, 11.0 to 16.0 s; D-dimer, <0.5 mg/L FEU (fibrinogen equivalent units).
Fig. 4.
Line graphs showing detailed changes of blood biochemistry and infection-related biomarkers for all 10 patients, starting from disease onset (Case 1) or the day of admission (Cases 2 through 9). The normal ranges of laboratory test results are as follows: albumin, 35 to 55 g/L; alanine aminotransferase (ALT), 5 to 35 U/L; aspartate aminotransferase (AST), 8 to 40 U/L; total bilirubin, 5.1 to 19.0 μmol/L; blood urea nitrogen, 2.9 to 8.2 mmol/L; creatinine, 44.0 to 106.0 μmol/L; procalcitonin, <0.05 ng/mL; C-reactive protein, 0 to 5 mg/L.
Nine (90%) of the 10 patients were managed with supplemental oxygen. All patients received antiviral therapy (oseltamivir) and antibacterial therapy (moxifloxacin). Additionally, 3 patients (30%) were managed with intravenous immunoglobulin, 3 patients were subjected to noninvasive ventilation, and 4 patients (40%) received glucocorticoids. One patient (Case 1) was managed with continuous kidney replacement therapy as she was diagnosed with decompensation of diabetic nephropathy during hospitalization. Because of the local limitations in medical technology and sudden worsening of the condition, invasive mechanical ventilation and extracorporeal membrane oxygenation were not utilized in these cases. Four patients (Cases 3, 6, 7, and 9) died on days 8, 8, 14, and 8, respectively, after admission. The remaining 6 patients remained in the hospital for further treatment. The clinical outcomes for surviving patients are not yet determined.
Discussion
The current study presents the clinical data for 10 patients with a fracture who were diagnosed with COVID-19 pneumonia. Previous investigations have documented that the clinical characteristics of patients with both a fracture and pneumonia were more serious than those of patients with only a fracture. As of February 27, 2020, of the 10 patients in the current analysis, 4 patients (Cases 3, 6, 7, and 9) had died and 3 others (Cases 1, 4, and 5) had developed severe pneumonia. These findings indicate that the development of COVID-19 pneumonia in patients with fracture can lead to severe adverse outcomes and increase mortality.
Patients with open fractures or severe injuries who are admitted to the orthopaedic trauma department require emergency surgery13,14. At the same time, most patients with hip fracture are older, many are in relatively poor physical condition, and many have underlying diseases such as hypertension, diabetes, or heart disease15,16. Such patients generally are advised to undergo surgical treatment as soon as possible. This approach not only promotes fracture-healing and facilitates recovery of mobility but also reduces various complications, such as the onset of pneumonia and deep-vein thrombosis17. If surgical treatment is not possible, these patients must remain in bed for 8 to 12 weeks, and, because of pain and the use of traction, most have to lie flat without being able to roll over, let alone stand. The stress associated with the fracture and surgical treatment can trigger a series of oxidative stress responses and excessive inflammation18. These reactions upregulate the expression of a series of inflammatory factors and decrease the immunity of the patients, increasing the likelihood of pneumonia19. Postoperative pulmonary complications have been reported to occur in 4.9% of patients after the surgical treatment of a hip fracture20. Wong et al. reported the case of an 81-year-old woman with an intertrochanteric fracture and SARS who died 7 days after surgery21. In the present study, 1 patient (Case 7) died 11 days after surgery and 3 patients (Cases 3, 6, and 9) died 8 days after admission without surgery being performed. Considering the high mortality of patients with COVID-19, surgical treatment for patients with both a fracture and COVID-19 should be carefully planned in advance. Furthermore, particular attention should be given to such patients after the surgical treatment of the fracture because of possibility of rapid deterioration of their condition.
In the present study, the common symptoms of patients with a fracture and COVID-19 pneumonia were similar to those in patients with COVID-19 but without a fracture. Laboratory tests suggested that lymphopenia was more likely to occur in patients with a fracture. Additionally, compared with the data in published articles on COVID-19, the median neutrophil count and D-dimer were higher than the upper normal limits of the corresponding indicators, which could represent the special laboratory characteristics of fractures in patients with COVID-19 (see Appendix Table II). qRT-PCR demonstrated that 3 patients (Cases 1, 2, and 5) were negative for the COVID-19 nucleic acid, whereas CT scans of the chest showed typical images of viral infection in all patients.
The present study documented that patients with a fracture may be at a higher risk of COVID-19 pneumonia. Seven of the 10 patients had a nosocomial infection. It is therefore essential to adopt strict infection-control measures. SARS-CoV-2 is thought to be transmitted directly by contact or by aerosol. Doctors, nurses, patients, and families should be wearing protective devices such as an N95 respirator and goggles.
On the basis of the current investigation, 4 major strategies for patients with a fracture and COVID-19 pneumonia can be proposed. First, nonoperative treatment should be considered for older patients with fractures, such as distal radial fractures, in endemic areas. Second, strict infection-control measures should be implemented for patients with fractures, particularly those undergoing surgical treatment. Third, patients with a fracture and COVID-19 pneumonia should be given more intensive surveillance and treatment. Fourth, surgical treatment for patients with a fracture and COVID-19 pneumonia should be performed in a negative-pressure operating room.
In summary, the symptoms of patients with a fracture with COVID-19 disease were diverse, with cough, fatigue, and fever being the main signs. Older patients with a hip fracture are at a higher risk of death. Future studies on the clinical characteristics of patients who have both a fracture and COVID-19 are essential to provide guidance for treatment in these rare cases.
Appendix
Supporting material provided by the authors is posted with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJS/F821).
Acknowledgments
Note: The views expressed in this article are those of the authors and do not represent the official policy of the China CDC. The authors thank Ximing Liu, Meng Zhao, Ming Chen, Zhonghua Guo, Chengjian He, Zheng Luo, Yaming Li, Dong Chen, Weixin Shi, and Yanzhen Qu for assistance with data collection.
Footnotes
Bobin Mi, MD, PhD, and Lang Chen, MD, contributed equally to this work.
Investigation performed at the Department of Orthopedics, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, People’s Republic of China
Disclosure: This work was supported by the National Science Foundation of China (No. 81772345), National Key Research & Development Program of China (No. 2018YFC2001502, 2018YFB1105705), National Health Commission of the People’s Republic of China (No. ZX-01-018, ZX-01-C2016153), and the Health Commission of Hubei Province (No. WJ2019Z009). The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJS/F820).
References
- 1.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020. February 7 Epub 2020 Feb 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, Zhu Y, Li B, Huang CL, Chen HD, Chen J, Luo Y, Guo H, Jiang RD, Liu MQ, Chen Y, Shen XR, Wang X, Zheng XS, Zhao K, Chen QJ, Deng F, Liu LL, Yan B, Zhan FX, Wang YY, Xiao GF, Shi ZL. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020. March;579(7798):270-3. Epub 2020 Feb 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu JT, Leung K, Leung GM. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020. February 29;395(10225):689-97. Epub 2020 Jan 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, Wang W, Song H, Huang B, Zhu N, Bi Y, Ma X, Zhan F, Wang L, Hu T, Zhou H, Hu Z, Zhou W, Zhao L, Chen J, Meng Y, Wang J, Lin Y, Yuan J, Xie Z, Ma J, Liu WJ, Wang D, Xu W, Holmes EC, Gao GF, Wu G, Chen W, Shi W, Tan W. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020. February 22;395(10224):565-74. Epub 2020 Jan 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X, Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020. February 15;395(10223):507-13. Epub 2020 Jan 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, Spitters C, Ericson K, Wilkerson S, Tural A, Diaz G, Cohn A, Fox L, Patel A, Gerber SI, Kim L, Tong S, Lu X, Lindstrom S, Pallansch MA, Weldon WC, Biggs HM, Uyeki TM, Pillai SK; Washington State 2019-nCoV Case Investigation Team. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020. March 5;382(10):929-36. Epub 2020 Jan 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, Ren R, Leung KSM, Lau EHY, Wong JY, Xing X, Xiang N, Wu Y, Li C, Chen Q, Li D, Liu T, Zhao J, Li M, Tu W, Chen C, Jin L, Yang R, Wang Q, Zhou S, Wang R, Liu H, Luo Y, Liu Y, Shao G, Li H, Tao Z, Yang Y, Deng Z, Liu B, Ma Z, Zhang Y, Shi G, Lam TTY, Wu JTK, Gao GF, Cowling BJ, Yang B, Leung GM, Feng Z. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020. January 29 Epub 2020 Jan 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020. February 15;395(10223):497-506. Epub 2020 Jan 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen YC, Lin WC. Risk of long-term infection-related death in clinical osteoporotic vertebral fractures: a hospital-based analysis. PLoS One. 2017. August 9;12(8):e0182614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rothe C, Schunk M, Sothmann P, Bretzel G, Froeschl G, Wallrauch C, Zimmer T, Thiel V, Janke C, Guggemos W, Seilmaier M, Drosten C, Vollmar P, Zwirglmaier K, Zange S, Wölfel R, Hoelscher M. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020. March 5;382(10):970-1. Epub 2020 Jan 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Health Commission of China. [The State Council’s joint prevention and control mechanism for pneumonia epidemic in response to new coronavirus infection( (6th edition).] Chinese. Accessed 2020 Mar 7 http://www.nhc.gov.cn/jkj/s3577/202003/4856d5b0458141fa9f376853224d41d7.shtml [Google Scholar]
- 12.National Health Commission of China. [The State Council’s joint prevention and control mechanism for pneumonia epidemic in response to new coronavirus infection( (5th edition).] Chinese. Accessed 2020 Feb 21 http://www.nhc.gov.cn/jkj/s3578/202002/dc7f3a7326e249c0bad0155960094b0b.shtml [Google Scholar]
- 13.Liu VX, Rosas E, Hwang J, Cain E, Foss-Durant A, Clopp M, Huang M, Lee DC, Mustille A, Kipnis P, Parodi S. Enhanced recovery after surgery program implementation in 2 surgical populations in an integrated health care delivery system. JAMA Surg. 2017. July 19;152(7):e171032 Epub 2017 Jul 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pietrafesa CA, Hoffman JR. Traumatic dislocation of the hip. JAMA. 1983 Jun 24;249(24):3342-6. [PubMed] [Google Scholar]
- 15.HIP ATTACK Investigators. Accelerated surgery versus standard care in hip fracture (HIP ATTACK): an international, randomised, controlled trial. Lancet. 2020. February 29;395(10225):698-708. Epub 2020 Feb 9. [DOI] [PubMed] [Google Scholar]
- 16.Lizaur-Utrilla A, Lopez-Prats FA. Hip attack for hip fractures: is ultra-early surgery necessary? Lancet. 2020. February 29;395(10225):661-2. Epub 2020 Feb 9. [DOI] [PubMed] [Google Scholar]
- 17.Ravi B, Pincus D, Wasserstein D, Govindarajan A, Huang A, Austin PC, Jenkinson R, Henry PDG, Paterson JM, Kreder HJ. Association of overlapping surgery with increased risk for complications following hip surgery: a population-based, matched cohort study. JAMA Intern Med. 2018. January 1;178(1):75-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mazidi M, Shivappa N, Wirth MD, Hebert JR, Vatanparast H, Kengne AP. The association between dietary inflammatory properties and bone mineral density and risk of fracture in US adults. Eur J Clin Nutr. 2017. November;71(11):1273-7. Epub 2017 Oct 11. [DOI] [PubMed] [Google Scholar]
- 19.Zhang P, Xia G, Dai L, Cheng Y, Wang Z. Laryngoscope-assisted and cotton ball wiping methods in prevention of oral and pulmonary infection in patients receiving mechanical ventilation and the influence on hypersensitive C-reactive protein and procalcitonin. Exp Ther Med. 2019. July;18(1):531-6. Epub 2019 May 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lv H, Yin P, Long A, Gao Y, Zhao Z, Li J, Zhang L, Zhang L, Tang P. Clinical characteristics and risk factors of postoperative pneumonia after hip fracture surgery: a prospective cohort study. Osteoporos Int. 2016. October;27(10):3001-9. Epub 2016 May 30. [DOI] [PubMed] [Google Scholar]
- 21.Wong KC, Leung KS, Hui M. Severe acute respiratory syndrome (SARS) in a geriatric patient with a hip fracture. A case report. J Bone Joint Surg Am. 2003. July;85(7):1339-42. [DOI] [PubMed] [Google Scholar]