Abstract
Background:
The use of cemented and cementless fixations in primary total knee arthroplasty (TKA) in young patients is controversial. Previous reviews predominantly relied on data from retrospective studies. This systematic review and meta-analysis of randomized controlled trials (RCTs) evaluated the optimal fixation mode in TKA for young patients.
Methods:
The PubMed, Embase, Medline, Web of Science, and full Cochrane Library electronic databases were searched from inception to July 2018. The outcome measurements consisted of functional outcomes (Knee Society Score [KSS], range of motion [ROM]), radiolucent lines, aseptic loosening, total complications, and reoperation rate. Study data were pooled using a random-effects model.
Results:
Six RCTs were included in the systematic review and meta-analysis. The mean follow-up period was 12 years (range, 2–16.6 years). Cementless TKA was associated with higher KSS-function (P < .0001), higher KSS-pain (P = .005), better ROM recovery (P = .01), and fewer radiolucent lines (<1 mm) (P = .04) compared with cemented TKA. No significant intergroup differences were observed for KSS-knee, total complications, aseptic loosening, or reoperation rate. These results based on a random-effects model were unchanged by sensitivity analysis assumptions.
Conclusion:
Cementless TKA was substantially superior to cemented TKA in young patients. Although the complication and survival rates were similar between groups, better clinical outcomes were obtained with cementless fixation. Further well-designed studies with long follow-up durations are necessary to confirm our findings.
Keywords: cemented, cementless, meta, systematic review, total knee arthroplasty, young
1. Introduction
Historically, total knee arthroplasty (TKA) has been used primarily in relatively sedentary elderly patients with end-stage knee osteoarthritis. However, TKA is now being performed in a growing number of patients aged 65 years or younger. In the Australian Joint Replacement Register, TKA patient demographics are slowly changing to younger patients, with the number of patients younger than 65 years of age having increased by 40% from the start of the register in 2002 until 2007.[1] Patients younger than 65 years are predicted to represent the majority of the anticipated primary TKA cases between 2010 and 2030.[2] TKA is a proven effective treatment in young patients[3,4] despite the fact that they are more active and demanding; thus, more mechanical complications and potential revisions may occur over time.
Debate over the use of cemented versus cementless fixation in TKA has persisted since the introduction of the latter. Cemented TKA is still the gold standard in TKA with excellent clinical outcomes and implant survivorship for up to 20 years.[5] However, it has been reported that the cemented TKA is associated with higher failure rates in younger and more active patients, with bone cement's lack of remodeling capacity as well as third-body wear over the long term of cemented fixation.[6–8] On the other hand, cementless fixation remains of interest to avoid the problems of cement longevity and preserve bone stock for potential revisions.[9] A more physiological bond between bone and implant is suggested to result in improved survival since it resists aseptic loosening.[10] Several studies have demonstrated the relationship between bone ingrowth and long-term implant stability and fixation durability.[11,12] Nevertheless, signs of osteolysis have also been observed with cementless TKA.[13]
Cementless fixation has not been widely accepted to date because several early implant designs failed, while many others did not show superiority to cemented fixation.[14] To our knowledge, it remains controversial whether cementless or conventional cemented fixation is superior in terms of postoperative functional recovery, implant survival, total complications, and radiological performance for primary TKA in young patients. Previous systematic reviews attempted to synthesize available evidence to explore the clear superiority of one modality over the other in young patients but drew different conclusions. However, these reviews were hampered by a limited number of randomized clinical trials (RCTs) available for analysis at the time.[1,15] In this context, the present systematic review and meta-analysis aimed to include the highest-level evidence available to determine the functional outcomes and clinical reliability of cementless components versus those of conventional cemented components for young patients undergoing primary TKA. A review and meta-analysis of the highest-level evidence in the current literature will allow us to better inform orthopedic surgical colleagues, general practitioners, physiotherapists, and patients about the outcomes of such surgery in young patients.
2. Materials and methods
2.1. Eligibility criteria and search strategy
The study protocol was developed and executed in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses statement.[16] This study was registered in the Research Registry. The studies included in our meta-analysis had to meet all of the following inclusion criteria in the PICOS order: Population: patients (≤65 years) who received primary TKA; Intervention: patients received cementless fixation in TKA; Comparison intervention: patients received cemented fixation in TKA; Outcome measures: at least one of the following outcome measures was reported: complication, reoperation, radiological outcomes, and functional results; Study design: RCTs with restriction to the English language. The exclusion criteria were: non-English language papers; non-RCTs such as case reports, animal trials, letters, retrospective studies, and reviews; conference abstracts and duplicate reports; and studies with no data analysis and/or power analysis.
From database inception to July 2018, 2 independent investigators used the following electronic databases to search existing literature: PubMed, Embase, Medline, Web of Science, and the full Cochrane Library. The detailed search strategy was as follows: (total knee arthroplasty or total knee replacement) and (cemented or cementless or uncemented) and (prospective or random). The reference lists of the included studies were also checked for additional studies that were not identified in the database search. This study is reported in line with Assessing the Methodological Quality of Systematic Reviews guidelines. Ethical approval was not necessary because the present meta-analysis was performed based on previously published studies.
2.2. Study selection
Articles were exported to EndNote and the duplicates were removed. Two independent authors screened the titles and abstracts of the potentially relevant studies to determine their eligibility based on the criteria. Disagreements were resolved through a discussion with a third author.
2.3. Data extraction
Two independent authors extracted the following descriptive raw information from the selected studies, including inclusion and exclusion criteria, first author, publish year, study design, sample size, mean age, sex ratio, detailed intervention protocols, follow-up time, and outcome measures. Disagreements were resolved through discussion with the third author. The outcome measurements consisted of functional outcomes (Knee Society Score [KSS], range of motion [ROM]), radiolucent lines, aseptic loosening, total complications, and reoperation. If the data were missing or could not be extracted directly, we contacted the corresponding authors to ensure that the information was integrated. Otherwise, we calculated them using the Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 guidelines. If necessary, we omitted extracting the incomplete data.
2.4. Quality assessment
The Cochrane risk of bias tool was used to evaluate the risk of bias of the included RCTs by 2 independent reviewers.[17] RCT quality was assessed using the following 7 items: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other bias. Kappa values were used to measure the degree of agreement between the 2 reviewers and were rated as follows: fair, 0.40 to 0.59; good, 0.60 to 0.74; and excellent, >0.75. Any controversy was resolved by discussion with a third author to reach a final consensus.
2.5. Data analysis
The statistical analyses in the present study were performed using Review Manager Software (RevMan Version 5.3; The Cochrane Collaboration, Copenhagen, Denmark). Risk ratios (RR) with a 95% confidence interval (CI) or mean differences (MD) with 95% CI were assessed for dichotomous or continuous outcomes, respectively. Significance was set at P < .05. The heterogeneity was assessed using the Q test and I2 statistics. An I2 ≥ 40% was considered to represent significant heterogeneity. The study data were pooled using the random-effects model. The Z test was used to assess the overall effect.
The publication bias was assessed by using funnel plots diagram. As many outcome measures were investigated, we only evaluated publication bias of reoperation rates, total complications, and radiolucent lines. The funnel plot asymmetry was evaluated by an Egger linear regression test to reveal any possible publication bias. Sensitivity analyses were undertaken to determine the potential source of heterogeneity when significant.
3. Results
3.1. Study selection
A total of 935 potentially relevant studies were initially identified by 2 independent reviewers from the following 5 databases: 219 from PubMed, 243 from EMBASE, 213 from Web of science, 182 from Medline, and 76 from the full Cochrane Library. After the duplicates were removed, the remaining 364 studies were screened; of them, 33 were subjected to full-text review. Eight RCTs involving patients younger than 65 years of age met the inclusion and exclusion criteria. Of the 25 studies excluded at full-text review, 2 were reviews,[1,15] 1 was a registry study,[18] 1 was a retrospective study,[19] and 21 RCTs included patients over the age of 65 years. Furthermore, 3 publications by Henricson et al[20] reported the same patients in 2008, 2013,[21] and 2016,[22] so we considered only the study of 2016. Ultimately, 6 RCTs were included in the further analysis (Fig. 1).[10,22–26]
Figure 1.
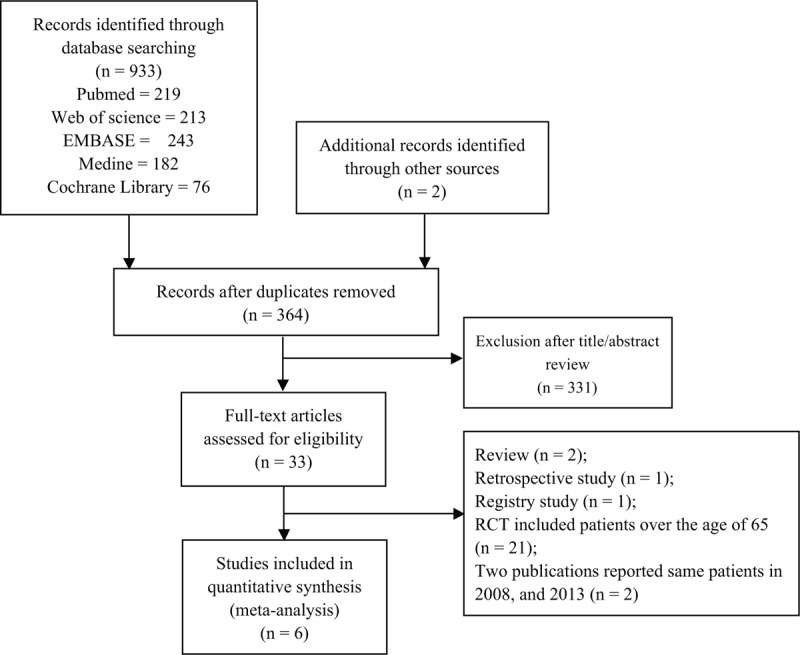
Flow diagram showing details of the literature search.
3.2. Study characteristics and quality assessment
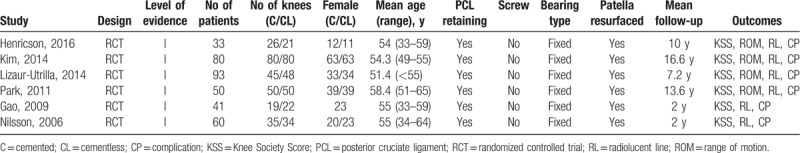
Table 1 outlines the characteristics of the 6 included RCTs involving 510 knees (255 for the cemented group; 255 for the cementless group). The participant age range in the included studies was 33 to 65 years, while the follow-up range was 2 to 16.6 years. All prostheses were designed as posterior cruciate ligament—retaining with a fixed tibial platform. None of the studies used screws for additional reinforcement or resurfaced the patella.
Table 1.
Study characteristics and patient demographic details.
The critical appraisal of the included studies using the Cochrane risk of bias tool is detailed in Fig. 2 and summarized in a stacked bar chart in Fig. 3. All trials included in this review clearly described inclusion and exclusion criteria. Only 1 study did not report the randomization method used.[22] The allocation concealment method was reported in 4 studies.[10,24–26] Only the Lizaur-Utrilla et al[23] study was double-blind; the remaining 5 studies did not blind the study staff or patients, which introduced high potential for performance bias. One study did not mention the personnel responsible for outcome measures,[22] while 3 studies[10,24,26] failed to report investigator blinding, indicating high detection bias. The proportion of patients lost to follow-up was <20% in all studies, indicating low attrition bias. All studies reported the results of all predefined measures, indicating low reporting bias. No other bias was detected. The overall kappa value regarding the evaluation of risk of bias was 0.899, meaning an excellent inter-reviewer degree of agreement.
Figure 2.
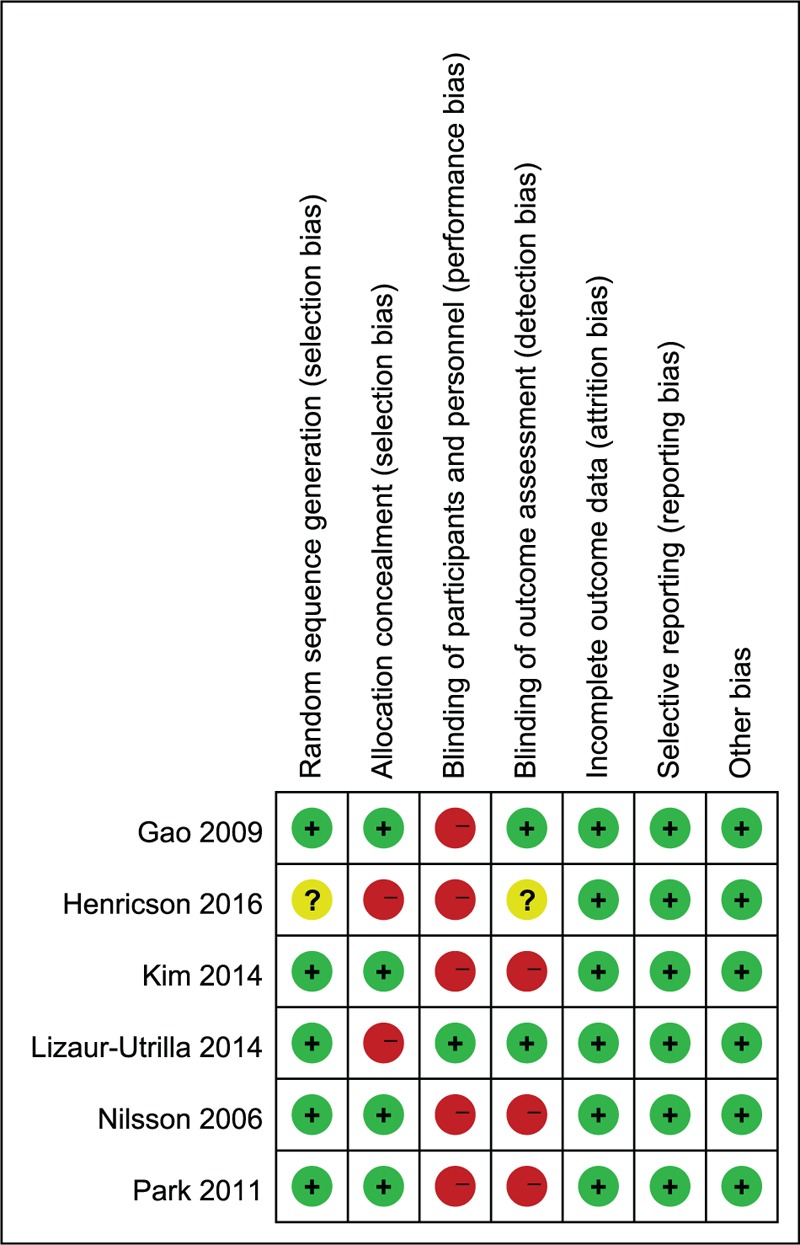
Risk of bias summary.
Figure 3.
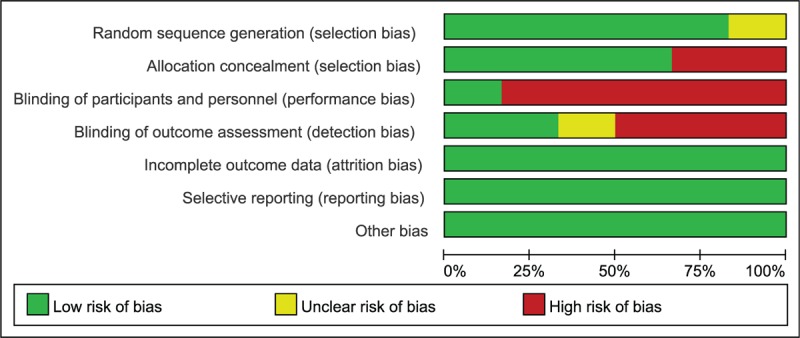
Risk of bias graph.
3.3. Meta-analysis results
3.3.1. Functional outcomes
Four studies[22,23,25,26] involving 250 knees showed no benefit of cementless fixation over cemented fixation in KSS-knee (MD, 0.20; 95% CI, –2.53 to 2.93; P = .89; I2 = 62%). A sensitivity analysis was conducted to determine the source of the heterogeneity. The pooled data from the 5 remaining studies supported a similar KSS-knee between the groups after exclusion of the Lizaur-Utrilla et al[23] study (MD, –1.17; 95% CI, –2.62 to 0.29; P = .12; I2 = 0%; Fig. 4A). Pooling data from 3 studies[23,24,26] involving 262 knees demonstrated a significant benefit favoring cementless over cemented fixation in KSS-function (MD, 4.48; 95% CI, 2.29–6.66; P < .0001; I2 = 0%; Fig. 4B). The pooling of data from 4 studies[22–25] involving 281 knees also demonstrated a significant benefit favoring cementless over cemented fixation in KSS-pain (MD, 3.03; 95% CI, 0.94–5.12; P = .005; I2 = 0%; Fig. 4C). Similarly, the pooling of data from 4 studies[10,22–24] involving 400 knees indicated a benefit of cementless over cemented fixation in ROM (MD, 5.28; 95% CI, 1.14–9.43; P = .01; I2 = 0%; Fig. 4D).
Figure 4.
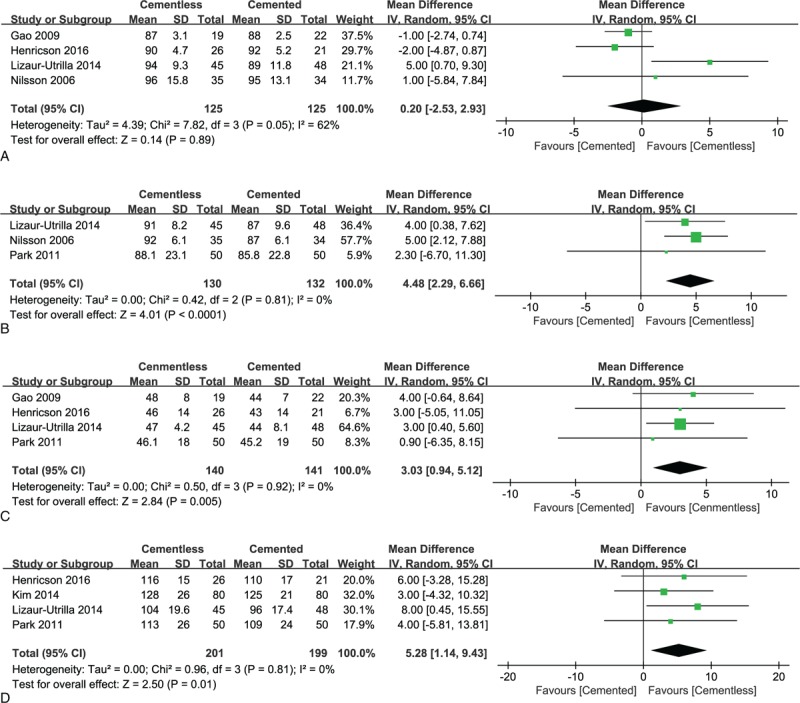
A. Forest plots of Knee Society Knee Score of the cemented and cementless groups. B. Forest plots of Knee Society Function Score of the cemented and cementless groups. C. Forest plots of Knee Society Pain Score of the cemented and cementless groups. D. Forest plots of range of motion of the cemented and cementless groups.
3.3.2. Radiological outcomes
Based on 6 studies[10,22–26] with 510 knees reporting radiolucent line (<1 mm), the presentation of radiolucency under the tibial or femoral component was much lower in the cementless group (18.4% in the cemented group and 9.8% in the cementless group; RR, 0.61; 95% CI, 0.38–0.98; P = .04; I2 = 13%; Fig. 5A). However, the pooling of data from 5 studies[10,22–25] involving 441 knees revealed no significant intergroup difference in aseptic loosening of the components (RR, 1.08; 95% CI, 0.27–4.33; P = .92; I2 = 0%; Fig. 5B).
Figure 5.
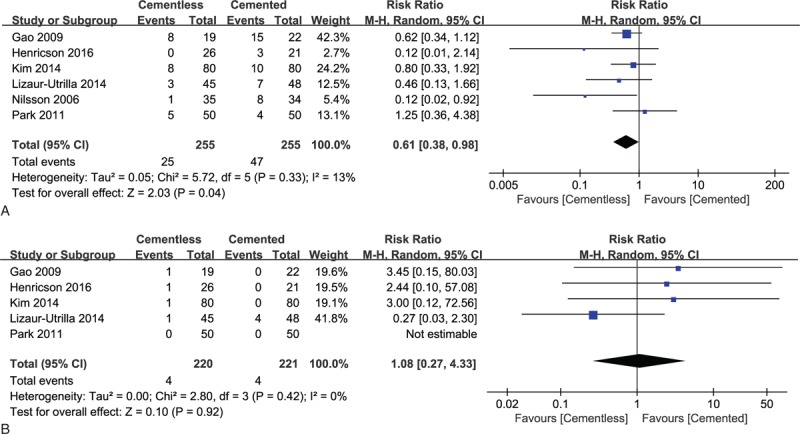
A. Forest plots of radiolucent line of the cemented and cementless groups. B. Forest plots of aseptic loosening of the cemented and cementless groups.
3.3.3. Total complications and reoperation
Six studies[10,22–26] with 510 knees reported the results of total complications at the last follow-up. The cementless and cemented groups had similar incidences of postoperative complications (14 and 17, respectively; RR, 0.83; 95% CI, 0.42–1.65; P = .60; I2 = 0%; Fig. 6A). The major 3 complications for the cementless group were persistent anterior knee pain, aseptic loosening, and deep infection, while aseptic loosening, deep infection, and neurological complications were most common in the cemented group. Similarly, there was no significant difference in reoperation rates, indicating that survivorship at a mean 12-year follow-up with reoperation for all causes as the end point was comparable between the 2 groups (RR, 0.70; 95% CI, 0.33–1.47; P = .35; I2 = 0%; Fig. 6B).
Figure 6.
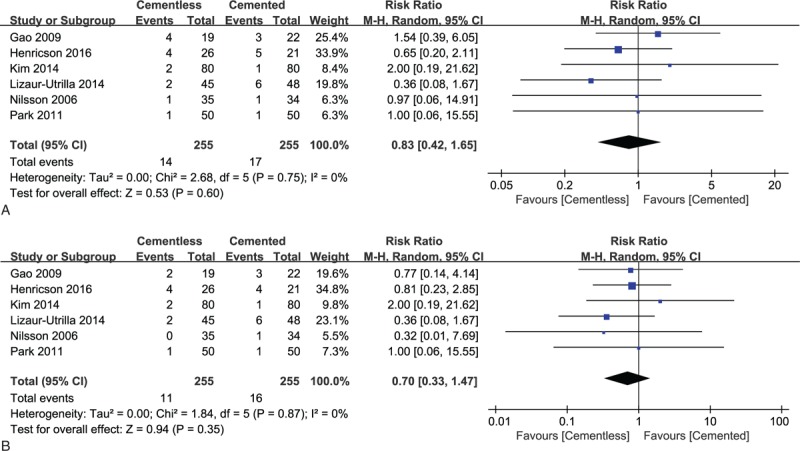
A. Forest plots of total complications of the cemented and cementless groups. B. Forest plots of reoperation rates of the cemented and cementless groups.
3.4. Publication bias
The funnel plots of reoperation, total complications, and radiolucent lines were symmetrical, indicating a low risk of publication bias (Fig. 7A–C).
Figure 7.
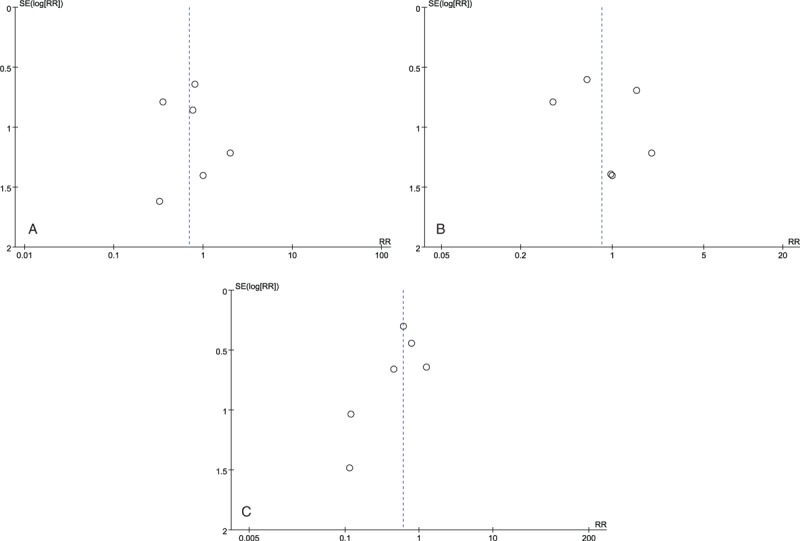
A. Funnel plots of reoperation rates of the cemented and cementless groups. B. Funnel plots of total complications of the cemented and cementless groups. C. Funnel plots of radiolucent line of the cemented and cementless groups.
4. Discussion
In this systematic review and meta-analysis of 6 RCTs with >500 knees comparing postoperative outcomes of cemented and cementless fixation in primary TKA for young patients, the latter group reported higher KSS-function, higher KSS-pain, better ROM recovery, and fewer radiolucent lines (<1 mm). No statistically significant intergroup differences in KSS-knee, aseptic loosening rates, total complication rates, and reoperation rates were detected. These results based on a random-effects model were unchanged by the sensitivity analysis assumptions.
Regarding functional recovery, the present meta-analysis revealed a similar KSS-knee between the groups (P = .89; I2 = 62%). When we excluded the source of heterogeneity in the sensitivity analysis, the statistical result was still reliable (P = .12; I2 = 0%). However, the results of the meta-analysis first demonstrated that patients with the cementless component had significantly higher KSS-function, KSS-pain, and ROM at the last follow-up. To our knowledge, no clinical differences were seen in many prospective randomized studies that compared cementless and cemented fixation, but these studies included a mixture of age groups.[27,28] Mont et al[19] also found no clinical differences between the cementless and cemented groups of young patients at a mean follow-up of 7 years, but theirs was a retrospective study. Patients younger than 65 years are generally more physically active and place higher demands and stresses on their implants. The cause of the differences in clinical outcomes in the present study is unclear. However, we hypothesized that cementless components in young patients had increased stability at the medium- and long-term, whereas cemented components might have progressive fixation defects, though not necessarily loosening, which could cause pain and mobility restrictions that affect the scores.
In our meta-analysis, total complications were comparable regardless of component fixation. However, complications were uncommon, and our study may have been underpowered to detect clinically meaningful differences between surgical fixations. Moreover, the sample size within any cemented or cementless group among the included studies was 19 to 80 knees. Therefore, it is plausible that rare events were undetected in some studies due to the small study size. In clinical practice, implant survival is the main issue related to TKA. The challenge today is to design implants and modes of fixation that will last for 30 years or more to suit these younger patients. In their registry study of 778 patients younger than 55 years with a mean follow-up of 14 years, Gioe et al[18] found better survival in the cemented TKA group. However, since a higher number of cemented implants was studied (738 vs 40 cementless), the significance of this result is greater for the cemented group. Here we found no statistically significant differences in reoperation rates (6.3% for the cemented group vs 4.3% for the cementless group); therefore, according to the available evidence, cementless fixation might be as durable as cemented fixation for young patients undergoing primary TKA. However, most fixation-related failures tend to occur 10 years ago,[29] potential intergroup differences might have gone undetected in some included studies with a 2-year follow-up.[25,26] Therefore, it is necessary and worthwhile to obtain longer-term follow-up data to present a more comprehensive picture of cementless or cemented fixation in young patients.
Radiolucent lines are radiolucent intervals between the implant and the adjacent bone.[30] According to Aebli et al,[31] radiolucent lines might occur due to imperfect cuts of the tibial plateau or due to micromotions leading to gap formation, which may prevent osteointegration in cementless TKA inducing the formation of fibrous tissue or osteoporotic regions. The presence of lines may be positively associated with loosening or instability, including migration, and inadequate load distribution.[32] Earlier studies[33,34] demonstrated that radiolucent lines occurred more frequently in cases of cementless TKA, further resulting in a consensus to use cemented component in tibial plateaus. Contrary to their conclusion, our study revealed that cementless TKA was associated with fewer radiolucent lines under the tibial or femoral component. Additionally, the loosening rates were similar between the groups. However, the radiolucency described in our study was non-progressive (<1 mm) and can occur with well-fixed components, so it should not necessarily be interpreted as loosening. Mutsuzaki et al[32] demonstrated a significant correlation between continual moderate knee pain and the appearance of tibial radiolucent lines. Our meta-analysis demonstrated better pain relief with cementless fixation than with cemented fixation at the last follow-up, which might have resulted from the relatively fewer radiolucent lines in the components.
Several reviews have compared the clinical efficacy and reliability of cementless and cemented fixation in primary TKA. A recently published meta-analysis[35] reported similar implant survivorship and clinical outcomes between full-cementless and full-cemented fixation in TKA, but elderly patients only were included in 4 of the RCTs.[28,36–38] A previous review conducted by Franceschetti et al[15] also showed similar functional outcomes, radiological outcomes, and survival rates for cemented and cementless TKA. However, only 2 RCTs[10,23] were included in their study, and the levels of evidence of the other included studies were very low. Aujla and Esler[1] performed a systematic review to analyze the functional outcomes of TKA performed in young patients. Postoperative clinical and functional KSS scores averaged 91.5 and 89.2 versus 92.2 and 82.2 for the cemented implant group, findings that were consistent with our results. However, they revealed a significantly higher all-cause revision rate for cementless TKA, with a revision rate of 7.0% for cemented prostheses and 2.3% for uncemented prostheses. However, they were unable to perform a meta-analysis or a weighted mean difference analysis due to the lack of homogeneity in the studies. Similarly, they only included 2 RCTs.[10,23]
The present study is the first meta-analysis to assess cemented versus cementless TKA in young patients. Our study strictly demonstrated a clear superiority of cementless fixation in postoperative functional recovery in cases of primary TKA for this special group. We only included RCTs to provide a high-quality evidence basis for the further application of cementless fixation and offer a clinical basis for the development of cementless prostheses. Despite our study's strengths, some limitations should be acknowledged. First, we included only RCTs published in English, which may have excluded potentially eligible studies with relevant findings. Second, the follow-up length of 2 years in 2 of the included studies[25,26] was relatively short for the comprehensive evaluation of implant prognosis. Trials with longer follow-up periods are still needed. Third, although only 6 RCTs were included in the meta-analysis, evidence of them was level I; thus, future high-quality studies with larger sample sizes are needed to confirm these findings.
5. Conclusions
Cementless TKA was substantially superior to cemented TKA in young patients. Although the complication and survival rates were similar between groups, better clinical outcomes were obtained with cementless fixation. Further well-designed studies with long follow-up durations are needed to confirm our conclusions. Ultimately, the choice of fixation in primary TKA should consider surgeon preference and experience as well as patient preference.
Author contributions
Conceptualization: Kaifeng Zhang.
Data curation: Jian Zhou.
Formal analysis: Kun Wang.
Funding acquisition: Han Sun.
Investigation: Shuxiang Li, Jian Zhou.
Methodology: Kaifeng Zhang.
Project administration: Kaifeng Zhang, Guofeng Wu, Jian Zhou.
Resources: Han Sun, Guofeng Wu.
Software: Shuxiang Li.
Supervision: Xiaoliang Sun.
Validation: Guofeng Wu.
Writing – original draft: Kun Wang.
Writing – review & editing: Kun Wang, Han Sun, Xiaoliang Sun.
Footnotes
Abbreviations: KSS = Knee Society Score, RCTs = randomized controlled trials, ROM = range of motion, TKA = total knee arthroplasty.
How to cite this article: Wang K, Sun H, Zhang K, Li S, Wu G, Zhou J, Sun X. Better outcomes are associated with cementless fixation in primary total knee arthroplasty in young patients: A systematic review and meta-analysis of randomized controlled trials. Medicine. 2020;99:3(e18750).
The authors have no conflicts of interest to disclose.
References
- [1].Aujla RS, Esler CN. Total knee arthroplasty for osteoarthritis in patients less than fifty-five years of age: a systematic review. J Arthroplasty 2017;32:2598–603. [DOI] [PubMed] [Google Scholar]
- [2].Kurtz SM, Lau E, Ong K, et al. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res 2009;2:2606–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Tai CC, Cross MJ. Five- to 12-year follow-up of a hydroxyapatite-coated, cementless total knee replacement in young, active patients. J Bone Joint Surg Br 2006;88:1158–63. [DOI] [PubMed] [Google Scholar]
- [4].Whiteside LA, Viganò R. Young and heavy patients with a cementless TKA do as well as older and lightweight patients. Clin Orthop Relat Res 2007;464:93–8. [DOI] [PubMed] [Google Scholar]
- [5].Attar FG, Khaw FM, Kirk LM, et al. Survivorship analysis at 15 years of cemented press-fit condylar total knee arthroplasty. J Arthroplasty 2008;23:344–9. [DOI] [PubMed] [Google Scholar]
- [6].Abdel MP, Bonadurer GF, Jennings MT, et al. Increased aseptic tibial failures in patients with a BMI ≥ 35 and well-aligned total knee arthroplasties. J Arthroplasty 2015;30:2181–4. [DOI] [PubMed] [Google Scholar]
- [7].Brown TE, Harper BL, Bjorgul K. Comparison of cemented and uncemented fixation in total knee arthroplasty. Orthopedics 2013;36:380–7. [DOI] [PubMed] [Google Scholar]
- [8].Carr AJ, Robertsson O, Graves S, et al. Knee replacement. Lancet 2012;379:1331–40. [DOI] [PubMed] [Google Scholar]
- [9].Behery OA, Kearns SM, Rabinowitz JM, et al. Cementless vs cemented tibial fixation in primary total knee arthroplasty. J Arthroplasty 2017;32:1510–5. [DOI] [PubMed] [Google Scholar]
- [10].Kim YH, Park JW, Lim HM, et al. Cementless and cemented total knee arthroplasty in patients younger than fifty-five years. Which is better? Int Orthop 2014;38:297–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Hofmann AA, Heithoff SM, Camargo M. Cementless total knee arthroplasty in patients 50 years or younger. Clin Orthop Relat Res 2002;102–7. [DOI] [PubMed] [Google Scholar]
- [12].Hofmann AA, Goldberg TD, Tanner AM, et al. Surface cementation of stemmed tibial components in primary total knee arthroplasty: minimum 5-year follow-up. J Arthroplasty 2006;21:353–7. [DOI] [PubMed] [Google Scholar]
- [13].Nolan JF, Bucknill TM. Aggressive granulomatosis from polyethylene failure in an uncemented knee replacement. J Bone Joint Surg Br 1992;74:23–4. [DOI] [PubMed] [Google Scholar]
- [14].Berger RA, Lyon JH, Jacobs JJ, et al. Problems with cementless total knee arthroplasty at 11 years followup. Clin Orthop Relat Res 2001;196–207. [DOI] [PubMed] [Google Scholar]
- [15].Franceschetti E, Torre G, Palumbo A, et al. No difference between cemented and cementless total knee arthroplasty in young patients: a review of the evidence. Knee Surg Sports Traumatol Arthrosc 2017;25:1749–56. [DOI] [PubMed] [Google Scholar]
- [16].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Gioe TJ, Novak C, Sinner P, et al. Knee arthroplasty in the young patient: survival in a community registry. Clin Orthop Relat Res 2007;464:83–7. [DOI] [PubMed] [Google Scholar]
- [19].Mont M, Lee CW, Sheldon M, et al. Total knee arthroplasty in patients <50 years old. J Arthroplasty 2002;17:538–43. [DOI] [PubMed] [Google Scholar]
- [20].Henricson A, Linder L, Nilsson KG. A trabecular metal tibial component in total knee replacement in patients younger than 60 years: a two-year radiostereophotogrammetric analysis. J Bone Joint Surg Br 2008;90:1585–93. [DOI] [PubMed] [Google Scholar]
- [21].Henricson A, Rösmark D, Nilsson KG. Trabecular metal tibia still stable at 5 years: an RSA study of 36 patients aged less than 60 years. Acta Orthop 2013;84:398–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Henricson A, Nilsson KG. Trabecular metal tibial knee component still stable at 10 years. Acta Orthop 2016;87:504–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Lizaur-Utrilla A, Miralles-Muñoz FA, Lopez-Prats FA. Similar survival between screw cementless and cemented tibial components in young patients with osteoarthritis. Knee Surg Sports Traumatol Arthrosc 2014;22:1585–90. [DOI] [PubMed] [Google Scholar]
- [24].Park JW, Kim YH. Simultaneous cemented and cementless total knee replacement in the same patients: a prospective comparison of long-term outcomes using an identical design of NexGen prosthesis. J Bone Joint Surg Br 2011;93:1479–86. [DOI] [PubMed] [Google Scholar]
- [25].Gao F, Henricson A, Nilsson KG. Cemented versus uncemented fixation of the femoral component of the NexGen CR total knee replacement in patients younger than 60 years: a prospective randomised controlled RSA study. Knee 2009;16:200–6. [DOI] [PubMed] [Google Scholar]
- [26].Nilsson KG, Henricson A, Norgren B, et al. Uncemented HA-coated implant is the optimum fixation for TKA in the young patient. Clin Orthop Relat Res 2006;448:129–39. [DOI] [PubMed] [Google Scholar]
- [27].Choy WS, Yang DS, Lee KW, et al. Cemented versus cementless fixation of a tibial component in LCS mobile-bearing total knee arthroplasty performed by a single surgeon. J Arthroplasty 2014;29:2397–401. [DOI] [PubMed] [Google Scholar]
- [28].Fricka KB, Sritulanondha S, McAsey CJ. To cement or not? Two-year results of a prospective, randomized study comparing cemented vs. cementless total knee arthroplasty (TKA). J Arthroplasty 2015;31:55–8. [DOI] [PubMed] [Google Scholar]
- [29].Fernandez-Fairen M, Hernández-Vaquero D, Murcia A, et al. Trabecular metal in total knee arthroplasty associated with higher knee scores: a randomized controlled trial. Clin Orthop Relat Res 2013;471:3543–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Sadoghi P, Leithner A, Weber P, et al. Radiolucent lines in low-contact-stress mobile-bearing total knee arthroplasty: a blinded and matched case control study. BMC Musculoskelet Disord 2011;12:142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Aebli N, Krebs J, Schwenke D, et al. Progression of radiolucent lines in cementless twin-bearing low-contact-stress knee prostheses: a retrospective study. J Arthroplasty 2004;19:783–9. [DOI] [PubMed] [Google Scholar]
- [32].Mutsuzaki H, Watanabe A, Kinugasa T, et al. Radiolucent lines are decreased at 3 years following total knee arthroplasty using trabecular metal tibial components. J Int Med Res 2018;46:1919–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Rand JA. Cement or cementless fixation in total knee arthroplasty? Clin Orthop Relat Res 1991;273:52–62. [PubMed] [Google Scholar]
- [34].Rosenberg AG, Barden RM, Galante JO. Cemented and ingrowth fixation of the Miller-Galante prosthesis. Clinical and roentgenographic comparison after three- to six-year follow-up studies. Clin Orthop Relat Res 1990;71–9. [PubMed] [Google Scholar]
- [35].Zhou K, Yu H, Li J, et al. No difference in implant survivorship and clinical outcomes between full-cementless and full-cemented fixation in primary total knee arthroplasty: a systematic review and meta-analysis. Int J Surg 2018;53:312–9. [DOI] [PubMed] [Google Scholar]
- [36].Baker PN, Khaw FM, Kirk LM, et al. A randomised controlled trial of cemented versus cementless press-fit condylar total knee replacement: 15-year survival analysis. J Bone Joint Surg Br 2007;89:1608–14. [DOI] [PubMed] [Google Scholar]
- [37].Nelissen RG, Valstar ER, Rozing PM. The effect of hydroxyapatite on the micromotion of total knee prostheses. A prospective, randomized, double-blind study. J Bone Joint Surg Am 1998;80:1665–72. [DOI] [PubMed] [Google Scholar]
- [38].Carlsson A, Björkman A, Besjakov J, et al. Cemented tibial component fixation performs better than cementless fixation: a randomized radiostereometric study comparing porous-coated, hydroxyapatite-coated and cemented tibial components over 5 years. Acta Orthop 2005;76:362–9. [PubMed] [Google Scholar]


