Abstract
Serum amylase levels in patients with acute pancreatitis often remain or fluctuate above the upper normal limit for over a week. This study investigated the clinical characteristics of patients with prolonged hyperamylasemia and their prognoses, including recurrence.
We retrospectively analyzed patients with first attacks of acute pancreatitis in a single center between March 2010 and December 2016. Patients were divided into 2 groups according to normalization of the serum amylase levels within a week.
A total of 313 patients were enrolled after exclusion. The serum amylase levels were normalized within a week in 205 patients (65.5%, group 1) and elevated over a week in 108 patients (34.5%, group 2). Group 2 was more related to alcohol, higher computed tomography (CT) severity index, local pancreatic complication, and moderately severe pancreatitis than group 1 (P < .05). Recurrent pancreatitis developed significantly more in group 2 (39.8%) than in group 1 (19.5%) (P < .001). The factors related to recurrent pancreatitis were amylase group, sex, alcohol, CT severity index, necrosis, and severity of pancreatitis (P < .05). Multivariate analysis showed that recurrent pancreatitis was independently associated with amylase group (odds ratio [OR] 2.123, 95% confidence interval [CI]= 1.227–3.673, P = .007) and alcohol (OR 2.023, 95% CI 1.134–3.611, P = .017).
In conclusion, prolonged hyperamylasemia over a week is associated with recurrence of acute pancreatitis.
Keywords: acute pancreatitis, amylase, hyperamylasemia, recurrence
1. Introduction
Acute pancreatitis is 1 of the major diseases in the digestive system that require hospitalization. The proportion of patients with acute pancreatitis in admitted patients is as high as up to a third of patients with gastrointestinal, liver, or pancreatic diagnosis.[1] The incidence of acute pancreatitis has increased over the past decades due to improved accuracy in diagnosis and country-specific increases of gallstone occurrence or alcohol consumption.[2,3]
Serum amylase level is 1 of the diagnostic criteria of acute pancreatitis.[4] Although serum amylase level has variable sensitivities and specificity,[5] it has played a pivotal role in the diagnosis of acute pancreatitis since it was first remarked in 1929 that hyperamylasemia is associated with acute pancreatitis.[2,6] Because serum amylase has a short half-life, it declines faster than other pancreatic enzymes.[7,8] In typical acute pancreatitis, the serum amylase activity reaches its peak within the first 1 to 2 days after an attack of pancreatitis, then returns to normal levels over the next 3 to 5 days.[9,10] This change of amylase occurs regardless of the height of the initial amylase level.[8,11] On the other hand, there is a group of patients who present with acute pancreatitis whose serum amylase levels remain or fluctuate above the upper normal limit for over a week.[9] Such prolonged hyperamylasemia has been reported to be related to pancreatic complications, such as pseudocysts or necrosis.[5,12] However, some patients with prolonged hyperamylasemia of amylase have no identifiable complications and recover their serum amylase levels after a week. The clinical characteristics of patients with such prolonged hyperamylasemia including complicated and uncomplicated cases as well as their prognoses have not yet been clarified.
Therefore, we examined patients with the first episode of acute pancreatitis in order to determine the clinical characteristics and prognosis of prolonged hyperamylasemia. In addition, the factors related to the recurrence of acute pancreatitis, including its association with prolonged hyperamylasemia, were investigated.
2. Methods
2.1. Eligible patients
A total of 437 patients who were hospitalized due to the first attack of acute pancreatitis at a single center between March 2010 and December 2016 were enrolled and analyzed retrospectively. Acute pancreatitis was diagnosed when 2 of the following 3 features were presented: characteristic abdominal pain, increase of serum amylase or lipase activity at least 3 times greater than the upper limit of normal levels, or characteristic evidence of acute pancreatitis on imaging studies, such as computed tomography (CT) or magnetic resonance imaging (MRI).[4] Eighty-four patients who had underlying pancreas abnormality were excluded from the study: chronic pancreatitis (n = 48), intraductal papillary mucinous neoplasm (n = 13), pancreatic cancer (n = 12), pancreatic duct abnormality (n = 6), distal pancreatectomy (n = 3), or pancreatic cyst (n = 2). We also excluded additional 40 patients who were not followed up over 6 months (n = 32), deceased (n = 5), or were pregnant (n = 3).
2.2. Patient groups
The patients were divided into 2 groups: patients in whom serum amylase levels were normalized (≤100 U/L) within a week (group 1) and patients who showed prolonged hyperamylasemia (>100 U/L) over a week including fluctuation (group 2). We compared the clinical characteristics and prognoses between the 2 groups, and evaluated the factors related to recurrent pancreatitis, including the association with prolonged hyperamylasemia.
2.3. Clinical characteristics
The onset time of acute pancreatitis was estimated to serve as the beginning of abdominal pain. If a patient did not visit the hospital on the first day of acute pancreatitis, the first measured serum amylase level of the patient became the day 2 or 3 amylase level, with no day 1 amylase level. Serum amylase levels were determined daily, if possible, until normalization during admission to estimate recovery of pancreatitis and not to overlook complications. All patients underwent CT scans or MRI on the initial day of admission. Follow-up imaging studies, such as CT, MRI, and ultrasonography were performed in patients who showed clinical deterioration, or in order to find gallstones. Chronic pancreatitis was diagnosed with the presence of one or more of the following findings according to the M-ANNHEIM (multiple risk factors-alcohol consumption, nicotine consumption, nutritional, hereditary, efferent pancreatic duct, immunological and metabolic factors) diagnostic criteria: pancreatic calcifications, moderate or marked pancreatic ductal lesions, and marked and persistent exocrine insufficiency with pancreatic steatorrhea.[13]
2.4. Ethics statement
A patient's anonymity was carefully protected, and all study protocols were in complete compliance with the declaration of Helsinki. This study was approved by the institute research board of the Catholic University of Korea (No. HC18RESI0045).
2.5. Statistical analysis
Categorical and continuous data in 2 groups were compared by Pearson chi-square test and Student t test, respectively. When the points of data in the category were less than 5, Fisher exact test was used. Logistic regression analysis (enter method) were used in multivariate analysis of factors related to recurrent pancreatitis. A P value < .05 is considered to be significant. All statistical analyses were performed using SPSS version 20 (SPSS, Inc., Chicago, IL).
3. Results
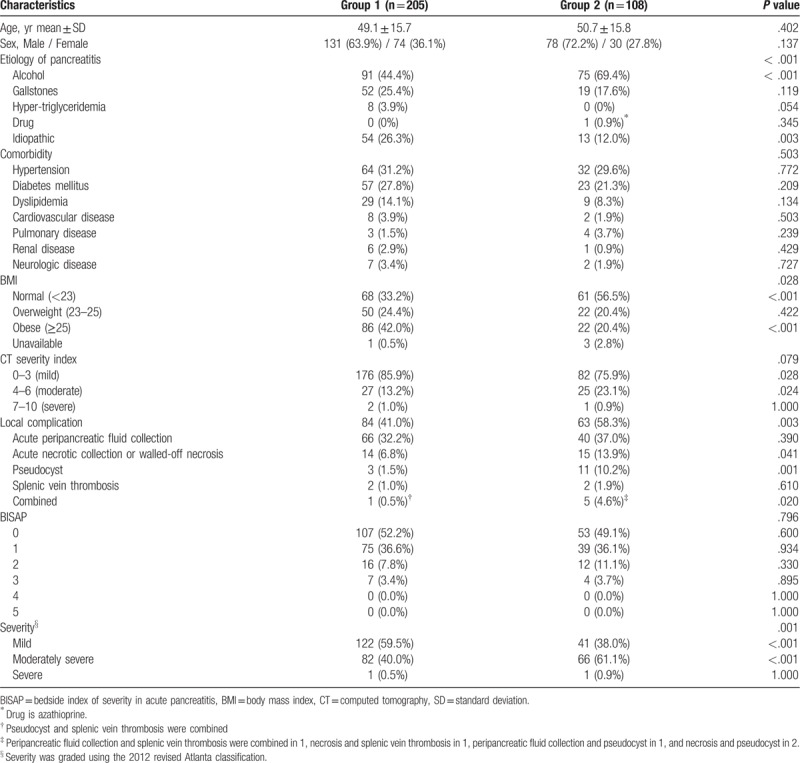
Following exclusion, a total of 313 patients were analyzed retrospectively. The average follow-up period of these patients was 1071 days (180 – 2930 days). The serum amylase levels were normalized within a week in 205 patients (65.5%, group 1) and remained or fluctuated above the upper normal limit over a week in 108 patients (34.5%, group 2). Serial daily average serum amylase levels according to group are shown in Figure 1. The average serum amylase levels in group 2 were significantly higher than those in group 1 every day for 2 weeks. There were some differences in baseline characteristics between the group 1 and 2 patients (Table 1). Group 2 revealed significantly more alcoholic cause (P < .001), normal body mass index (P < .001), moderate CT severity index (4–6, P = .024), acute necrotic collection or walled-off necrosis (P = .041), pseudocyst (P = .001), and moderately severe severity (P < .001) than group 1. Age, sex, comorbidity, and bedside index of severity in acute pancreatitis score did not differ between the 2 groups.
Figure 1.
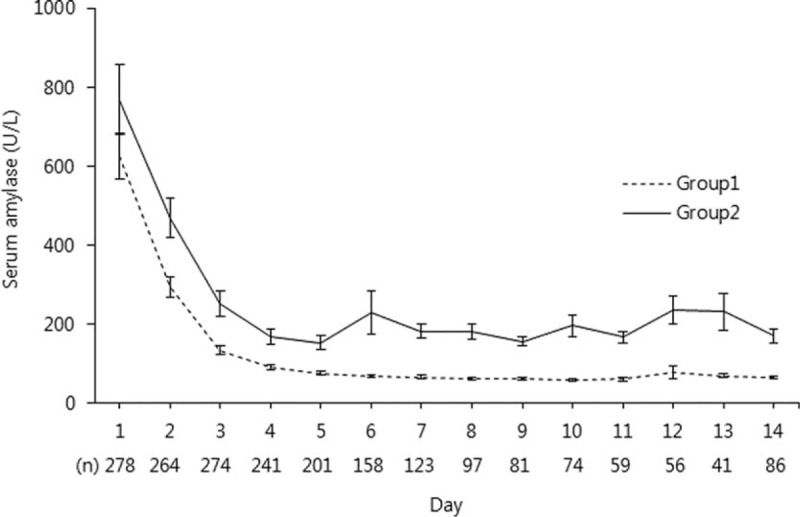
Serial average serum amylase levels (± standard deviation) according to the amylase group.
Table 1.
Baseline characteristics of patients according to normalization of serum amylase levels within a week.
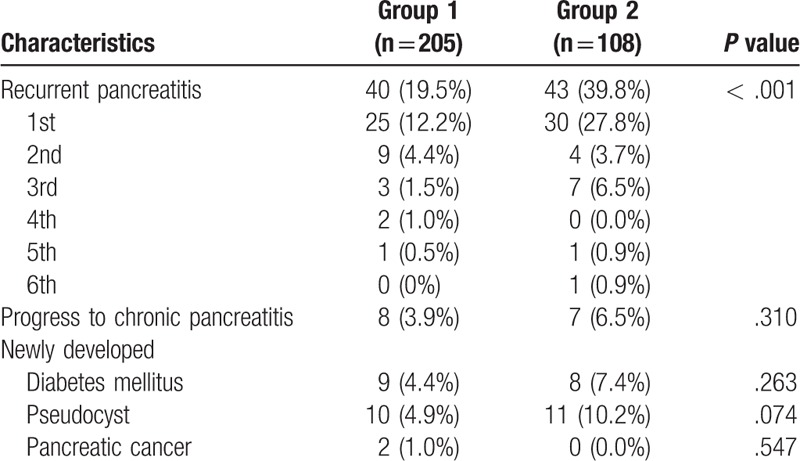
During follow-up period after first attack of acute pancreatitis, recurrent acute pancreatitis occurred in 83 (26.5%) of overall patients. Regarding amylase groups, recurrent pancreatitis occurred significantly more in group 2 than in group 1 (39.8% vs 19.5%, P < .001, Table 2). The maximum number of recurrent episodes was 5 in group 1 and 6 in group 2. Progress to chronic pancreatitis was observed more in group 2 (6.5% vs 3.9%). Newly-developed diabetes and pseudocyst were also seen more in group 2. However, these trends were not statistically significant. Pancreatic cancer was found in 2 patients (1.0%) in group 1 during follow-up, but none in group 2.
Table 2.
Follow-up findings of patient groups.
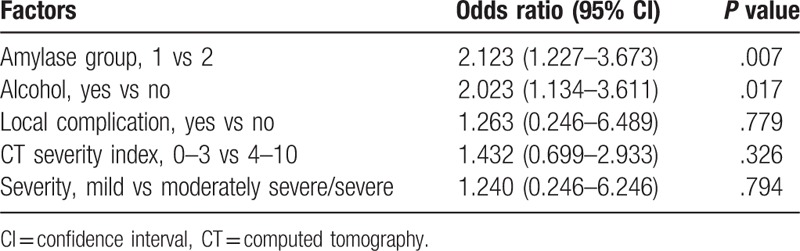
The factors related to recurrence of acute pancreatitis were analyzed (Table 3). In univariate analysis, being in group 2, male sex, alcohol, moderate CT severity index (4–6), acute necrotic collection or walled-off necrosis, and moderately severe severity (P < .05) were all related to recurrent pancreatitis. Serial daily average serum amylase levels demonstrated that the serum amylase levels in patients with recurrent pancreatitis were significantly higher than those in patients without recurrent pancreatitis on days 5, 7, 8, and 9 (P = .020, .041, .023, and .009, respectively, Figure 2). Multivariate analysis showed that recurrent pancreatitis was independently associated with the amylase group (odds ratio [OR] 2.123, 95% confidence interval [CI] 1.227–3.643, P = .007) and alcohol (OR 2.023, 95% CI= 1.134–3.611, P = .017) (Table 4).
Table 3.
Factor analysis associated with recurrent pancreatitis.
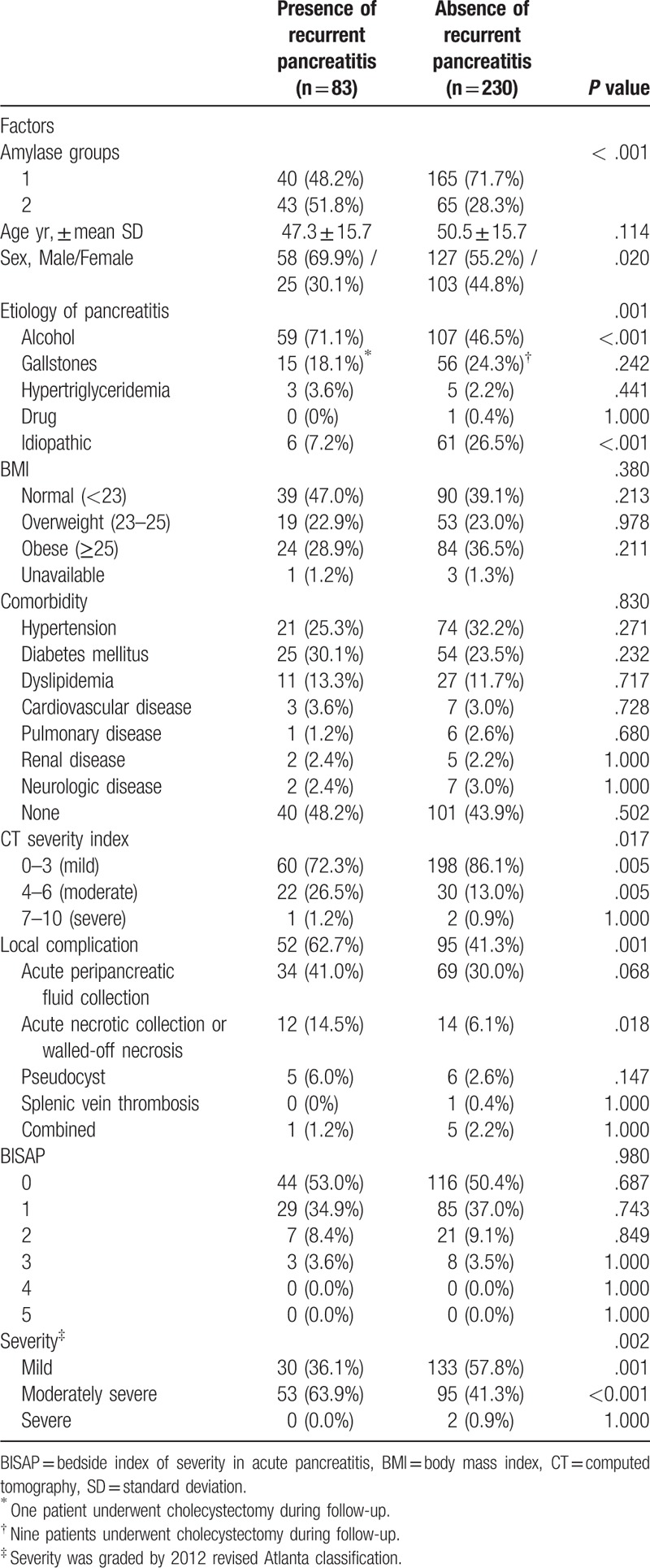
Figure 2.

Serial average serum amylase levels (± standard deviation) according to recurrence of acute pancreatitis (∗<0.05; ∗∗< 0.01).
Table 4.
Multivariate analysis of factors associated with recurrent pancreatitis.
4. Discussion
This study demonstrated that prolonged hyperamylasemia over a week occurred in 34.5% of patients with first acute pancreatitis and is related to alcohol, local complications, and severity of pancreatitis. Prolonged hyperamylasemia was independently associated with the recurrence of acute pancreatitis as well as alcohol.
In typical pancreatitis, elevated serum amylase levels returns to normal within 3 to 5 days after an attack of pancreatitis, regardless of the height of the amylase level.[9,10] It has been known that the magnitude of the serum amylase level is not correlated with the severity of acute pancreatitis.[14,15] Although the level of serum amylase has little prognostic value in acute pancreatitis, pancreatic edema and extra-pancreatic fat necrosis are well correlated with hyperamylasemia in a rat pancreatitis model.[16] Patients with prolonged elevation of serum amylase level would have the presence of pancreatic complications, such as pseudocyst, necrosis, or abscess.[5,15] However, there are some cases that do not have any identifiable causes or complications related to prolonged hyperamylasemia. A previous study reported that 24/78 (30.8%) patients had hyperamylasemia over 10 days, and that 29% of patients with prolonged hyperamylasemia did not have obvious cause for the prolonged elevation of serum amylase level.[17] Another study showed that 6/233 (2.6%) patients were observed to have significant hyperamylasemia for periods over 21 days.[9] Among six patients, there were three cases of pseudocysts, 2 cases of persistent pancreatitis, and 1 case without any complications. In etiologic aspect, there was a study that high amylase levels persisted longer in alcohol than biliary causes.[17] Our study also revealed that 45.2% of alcohol causes was related to prolonged hyperamylasemia, but 26.8% in biliary causes. Other related factors to prolonged hyperamylasemia in this study were higher CT severity index, pancreatic necrosis, pseudocyst, and moderately severe pancreatitis. These suggest that prolonged hyperamylasemia might be related to more pancreatic injury.
Data on the natural history of acute pancreatitis are limited.[18–20] Recent publications have shown the rates of recurrent pancreatitis varying from 16% to 20% overall and from 22% to 46% for alcoholic pancreatitis.[18,21] The annual relapse rates were higher for patients with alcohol (5.3%) than biliary (1.5%) or idiopathic causes (1.9%).[18] Our study showed a similar result, that recurrent pancreatitis developed in 26.5% of overall patients and in 35.5% of patients with alcoholic etiology. The recurrence of acute pancreatitis may be associated with multiple factors, such as toxic-metabolic, genetic, autoimmune, and obstructive.[22,23] A previous study showed that etiology, smoking, pancreatic necrosis, and acute physiology and chronic health evaluation II score are all associated with recurrent pancreatitis in multivariate analysis.[21] Our study demonstrated that prolonged hyperamylasemia and alcohol were independently associated with recurrent pancreatitis in multivariate analysis. Therefore, prolonged hyperamylasemia might be one of the useful predictors of recurrence in patients with acute pancreatitis, and more attention is needed to these patients.
This study has some limitations due to its retrospective design. First, serum amylase tests were not performed at the same interval in all patients. When the serum amylase levels were normalized, we did not test serum amylase level daily thereafter. Around a week after discharge, follow-up serum amylase tests were administered at the outpatient clinic. Second, in order to completely determine pancreatic local complication, follow-up imaging studies are needed. In this study, CT scans or MRI were performed in all patients on the initial day of admission, but follow-up imaging studies were performed in patients who showed clinically deterioration or to find out gallstones. In patients with mild prolonged hyperamylasemia without symptoms, we did not perform imaging studies and closely observed them by testing serum amylase levels. Follow-up imaging studies less than 2 months from the onset of acute pancreatitis have been performed in 185 patients (59.1%): CT scans in 71, MRI in 116, and ultrasonography in 63 (duplications are included).
In conclusion, prolonged hyperamylasemia over a week occurred in about one-third of patients with the first attack of acute pancreatitis. Prolonged hyperamylasemia as well as alcohol is independently associated with the recurrence of pancreatitis; therefore, closer observation and follow-up are needed in patients with prolonged hyperamylasemia. Future studies with a larger number of patients are expected to validate this study.
Author contributions
Conceptualization: Jae Hyuck Chang.
Data curation: Young Sun Kim.
Formal analysis: Young Sun Kim, Jae Hyuck Chang.
Investigation: Young Sun Kim.
Project administration: Jae Hyuck Chang.
Supervision: Jae Hyuck Chang, Tae Ho Kim, Chang Whan Kim, Jae Kwang Kim, Sok Won Han.
Writing – original draft: Jae Hyuck Chang.
Writing – review and editing: Jae Hyuck Chang.
Footnotes
Abbreviations: CI = confidence interval, CT = computed tomography, MRI = magnetic resonance imaging, OR = odds ratio.
How to cite this article: Kim YS, Chang JH, Kim TH, Kim CW, Kim JK, Han SW. Prolonged hyperamylasemia in patients with acute pancreatitis is associated with recurrence of acute pancreatitis. Medicine. 2020;99:3(e18861).
The authors have no conflicts of interest to disclose.
References
- [1].Peery AF, Crockett SD, Barritt AS, et al. Burden of gastrointestinal, liver, and pancreatic diseases in the United States. Gastroenterology 2015;149:1731–41.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Steinberg W, Tenner S. Acute pancreatitis. N Engl J Med 1994;330:1198–210. [DOI] [PubMed] [Google Scholar]
- [3].Yadav D, Lowenfels AB. Trends in the epidemiology of the first attack of acute pancreatitis: a systematic review. Pancreas 2006;33:323–30. [DOI] [PubMed] [Google Scholar]
- [4].Banks PA, Bollen TL, Dervenis C, et al. Classification of acute pancreatitis--2012: revision of the Atlanta classification and definitions by international consensus. Gut 2013;62:102–11. [DOI] [PubMed] [Google Scholar]
- [5].Yadav D, Agarwal N, Pitchumoni CS. A critical evaluation of laboratory tests in acute pancreatitis. Am J Gastroenterol 2002;97:1309–18. [DOI] [PubMed] [Google Scholar]
- [6].Elman R, Arneson N, Graham E. Value of blood amylase estimations in the diagnosis of pancreatic disease: a clinical study. Arch Surg 1929;19:943–67. [Google Scholar]
- [7].Lankisch PG, Buschmann-Kaspari H, Otto J, et al. Correlation of pancreatic enzyme levels with the patient's recovery from acute edematous pancreatitis. Klin Wochenschr 1990;68:565–9. [DOI] [PubMed] [Google Scholar]
- [8].Vissers RJ, Abu-Laban RB, McHugh DF. Amylase and lipase in the emergency department evaluation of acute pancreatitis. J Emerg Med 1999;17:1027–37. [DOI] [PubMed] [Google Scholar]
- [9].Veith FJ, Filler RM, Berard CW. Significance of prolonged elevation of the serum amylase. Ann Surg 1963;158:20–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Winslet M, Hall C, London NJ, et al. Relation of diagnostic serum amylase levels to aetiology and severity of acute pancreatitis. Gut 1992;33:982–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Banks PA. Practice guidelines in acute pancreatitis. Am J Gastroenterol 1997;92:377–86. [PubMed] [Google Scholar]
- [12].Grossman MS. Prolonged hyperamylasemia following acute pancreatitis. Am J Dig Dis 1964;9:618–24. [DOI] [PubMed] [Google Scholar]
- [13].Schneider A, Lohr JM, Singer MV. The M-ANNHEIM classification of chronic pancreatitis: introduction of a unifying classification system based on a review of previous classifications of the disease. J Gastroenterol 2007;42:101–19. [DOI] [PubMed] [Google Scholar]
- [14].Papachristou GI, Whitcomb DC. Predictors of severity and necrosis in acute pancreatitis. Gastroenterol Clin North Am 2004;33:871–90. [DOI] [PubMed] [Google Scholar]
- [15].Clavien PA, Burgan S, Moossa AR. Serum enzymes and other laboratory tests in acute pancreatitis. Br J Surg 1989;76:1234–43. [DOI] [PubMed] [Google Scholar]
- [16].Schmidt J, Lewandrowski K, Fernandez-del Castillo C, et al. Histopathologic correlates of serum amylase activity in acute experimental pancreatitis. Dig Dis Sci 1992;37:1426–33. [DOI] [PubMed] [Google Scholar]
- [17].Bockus HL, Kalser MH, Roth JL, et al. Clinical features of acute inflammation of the pancreas; analysis of ninety-four attacks in seventy-eight patients. AMA Arch Intern Med 1955;96:308–21. [DOI] [PubMed] [Google Scholar]
- [18].Lankisch PG, Breuer N, Bruns A, et al. Natural history of acute pancreatitis: a long-term population-based study. Am J Gastroenterol 2009;104:2797. [DOI] [PubMed] [Google Scholar]
- [19].Nojgaard C. Prognosis of acute and chronic pancreatitis - a 30-year follow-up of a Danish cohort. Dan Med Bull 2010;57:B4228. [PubMed] [Google Scholar]
- [20].Takeyama Y. Long-term prognosis of acute pancreatitis in Japan. Clin Gastroenterol Hepatol 2009;7:S15–17. [DOI] [PubMed] [Google Scholar]
- [21].Ahmed Ali U, Issa Y, Hagenaars JC, et al. Risk of recurrent pancreatitis and progression to chronic pancreatitis after a first episode of acute pancreatitis. Clin Gastroenterol Hepatol 2016;14:738–46. [DOI] [PubMed] [Google Scholar]
- [22].Guda NM, Romagnuolo J, Freeman ML. Recurrent and relapsing pancreatitis. Curr Gastroenterol Rep 2011;13:140–9. [DOI] [PubMed] [Google Scholar]
- [23].Kedia S, Dhingra R, Garg PK. Recurrent acute pancreatitis: an approach to diagnosis and management. Trop Gastroenterol 2013;34:123–35. [DOI] [PubMed] [Google Scholar]


