Abstract
This study aimed to discuss the risk factors of perioperative blood transfusion after the application of proximal femoral nail antirotation (PFNA) in the treatment of elderly patients with femoral intertrochanteric fracture (FIF). Moreover, this study also aimed to analyze the causes of perioperative blood transfusion and provide guidance for clinical treatment.
Records of elderly patients with FIF who were treated with PFNA in our hospital from September 2014 to May 2017 were reviewed. They were divided into transfused and nontransfused groups. The Student t test, Chi-squared test, and Fisher exact test were used in univariate analysis of 11 variables. Multivariate logistic regression analysis was performed to analyze the possible risk factors associated with postoperative blood transfusion after the application of PFNA in elderly patients with FIF. Correlations were sought using the Spearman rank correlation analysis.
The univariate analysis showed that age, sex, type of fracture, admission hemoglobin (Hb), admission albumin, and intraoperative blood loss were significantly associated with perioperative blood transfusion (P = .000, .019, .000, .000, .000, and .007, respectively). The multivariate logistic regression analysis demonstrated that age (P = .019, odds ratio [OR] = 1.062), type of fracture (P = .001, OR = 4.486), and admission Hb (P = .000, OR = 0.883) were independent risk factors of postoperative blood transfusion. We found a significant positive correlation between perioperative blood transfusion and age (r = 0.264, P = .000) and type of fracture (r = 0.409, P = .000), but a negative correlation between perioperative blood transfusion and admission Hb (r = −0.641, P = .000).
The main factors affecting perioperative blood transfusion are age, fracture type, and admission Hb. These results indicate that, in high-risk patients who are older in age, more unstable fractures, and lower admission Hb, monitoring Hb concentrations during the perioperative period is important to correct severe anemia in a timely manner and avoid exacerbating existing underlying diseases and inducing severe complications.
Keywords: elderly, femoral intertrochanteric fracture, perioperative blood transfusion
1. Introduction
Intertrochanteric fractures mainly occur in the elderly population, and comprise approximately 3% to 4% of all the fractures in the general population.[1] As the elderly population is rapidly increasing, the incidence of this type of fracture has also been increasing ever year. Most of these patients also have serious cardiovascular disease, respiratory disease, hematopoietic system disease, severe osteoporosis, and so on. Anemia is one of the most common complications during the perioperative period in these patients. The primary treatment for anemia is blood transfusion. Several studies found that 30% to 70% of the elderly patients with hip fracture need perioperative allogeneic blood transfusion.2,3,4 However, the shortage of blood resources is an important issue worldwide. Moreover, some investigators have reported cases of over-cross-matching5,6 and over-transfusion,5,6,7,8,9 and clinical and evidence-based medicine supports the adoption of restrictive transfusion policies.[10] In addition, if some patients do not need intraoperative blood transfusion, preoperative routine cross-matching of 2 units of blood for patients with hip fractures can waste a little blood in blood banks and further aggravate the blood shortage problem. To formulate a restrictive and safe cross-matching policy, we must primarily be able to identify perioperative patients at risk of transfusion. Several possible factors may predict blood transfusion risk, such as age, use of platelet inhibitors, and low preoperative hemoglobin (Hb). However, only a few studies have conducted systematic research on its specific risk factors.
The purpose of this retrospective study was to discuss the risk factors of perioperative blood transfusion after the application of proximal femoral nail antirotation (PFNA) in the treatment of elderly patients with femoral intertrochanteric fracture (FIF). Moreover, we also aimed to analyze the causes of perioperative blood transfusion and provide guidance for its clinical treatment.
2. Materials and methods
2.1. Study population and study design
After obtaining approval from the Institutional Review Board of our hospital, we retrospectively reviewed the records of consecutive patients with unilateral FIF treated with PFNA between September 2014 and May 2017 at our hospital. The inclusion criteria were as follows: age over 60 years, use of PFNA, fresh closed fractures (within 7 days from injury to surgery), and no vascular or nerve injury. The exclusion criteria were as follows: bilateral FIFs, multiple traumas, pathologic fractures, open fractures, metabolic bone disease, and did not undergo surgery. In accordance with the inclusion and exclusion criteria, 198 of the 238 patients with unilateral FIFs treated with PFNA were identified from our department (Fig. 1).
Figure 1.
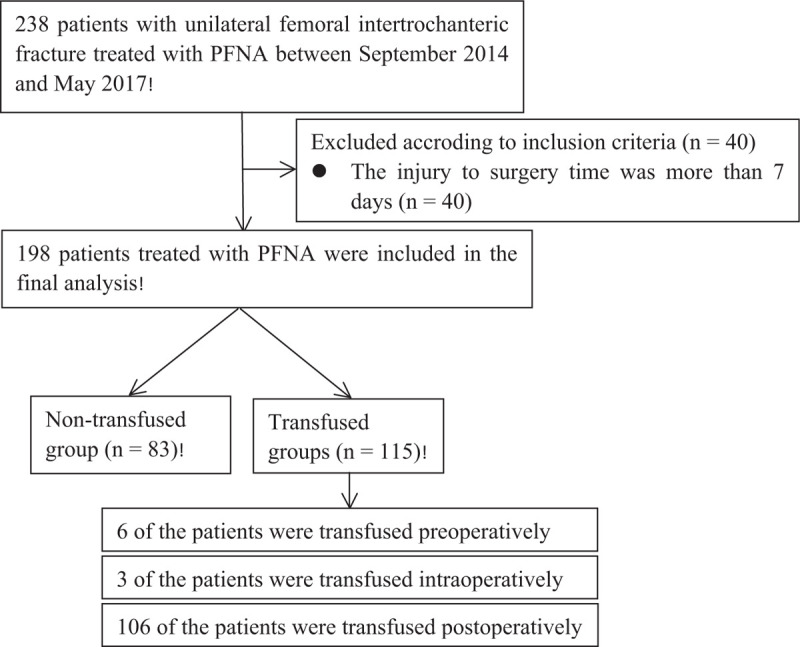
Flowchart showing progress through the study of elderly patients with femoral intertrochanteric fracture, evaluated for perioperative blood transfusion following the application of proximal femoral nail antirotation (PFNA).
The following variables from the electronic medical record system of Affiliated Dongyang Hospital of Wenzhou Medical University were used in this study: age, sex, fracture type, American Society of Anesthesiologists (ASA) grading score, paregoric or anticoagulant administration on admission, admission Hb, admission albumin, injury to surgery time, operative time, intraoperative blood loss, and with or without blood transfusion.
The patients’ characteristics were obtained through electronic medical record system. The preoperative anteroposterior and lateral radiographs of the injured hip were reviewed to determine the characteristics of the fractures. Fractures were classified as stable or unstable by the same 2 observers who had obtained the attending physician qualification certificate on the digital imaging system, respectively (DCQ and WLH), according to the modified Evans classification system (Fig. 2).11,12 On admission, the medical condition was assessed and classified according to the ASA grading system. Admission Hb was defined as the first preoperative Hb level recorded following admission with a maximum of 48 hours following admission. Admission albumin was defined as the 1st preoperative albumin following admission with a maximum of 48 hours following admission. Blood loss was estimated based on the suction apparatus and swab weight. Duration of operation in this study was measured from the time of close reduction to incision closure.
Figure 2.
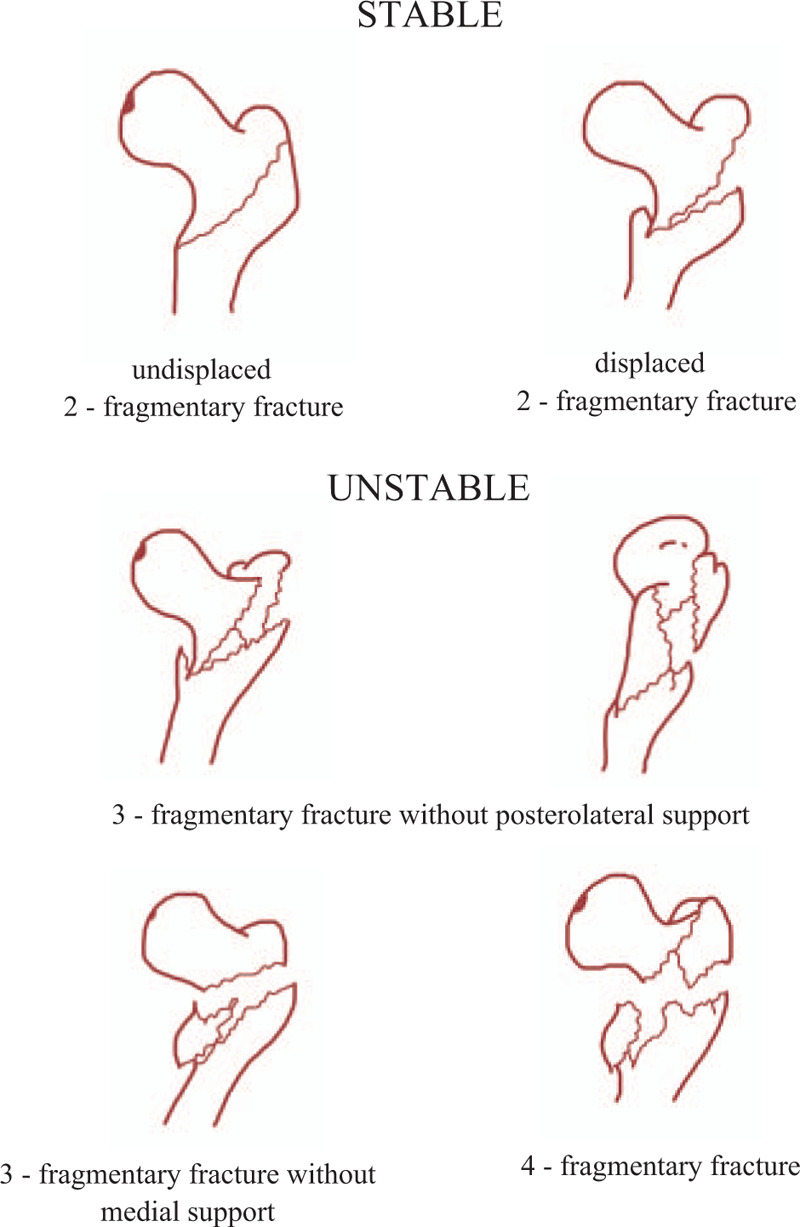
Classification of femoral intertrochanteric fractures according to Evans (1949) as modified by Jensen and Michaelsen (1975).
Our institution currently adheres to a restrictive transfusion policy. According to our transfusion protocol, patients were preoperatively transfused if their Hb level was 90 g/L, were transfused intraoperatively when their Hb level dropped below 80 g/L after excessive blood loss, and were transfused postoperatively when their Hb level dropped below 80 g/L. This transfusion trigger was raised to 90 g/L in clinically symptomatic patients. The final decision to transfuse was made by surgeons or anesthetists and was based on the low Hb levels and clinical discretion. Thus, the abovementioned recommendations are not the absolute criteria.
To evaluate the risk factors of perioperative blood transfusion, we divided the patients into transfused and nontransfused groups, depending on whether they received preoperative, intraoperative, or postoperative allogenic red blood cell (RBC) transfusion of at least 1 unit within the same hospitalization period. Neither the number of units of blood received nor the frequency of transfusion required per patient was recorded.
Operations were performed in a teaching hospital by the attending surgeon (DCQ, WLH, SJB, and LY). The first 3 operations were not included in the study analysis to eliminate the effect of the learning curve. The surgical technique followed the manufacturer's instructions. Surgeries were performed under image intensification on a traction table with the patient in the supine position. Fracture reduction was achieved by closed reduction through a longitudinal traction; the fracture site was exposed only if closed reduction was not successful.
2.2. Statistical analysis
Distributions of data were assessed. Frequency was used for categorical data, and mean ± standard deviation was used for continuous data. The Student t test was used to evaluate the significance of the difference of the means between the independent groups. The Pearson Chi-squared test and Fisher exact test were used for categorical comparisons. The transfused group was compared with the nontransfused group in terms of the collected variables. A multivariate logistic model was used to determine whether the factors were independently associated with risk of postoperative blood transfusion. All variables were included as possible predictors, and a final model was found using Wald-forward LR stepwise elimination. We used the Box Tidwell test to check the linearity assumption for quantitative variables. Final modeling results were reported with odds ratios (ORs) and 95% confidence intervals (CIs). To detect a correlation between perioperative blood transfusion and the primary and secondary predictive factors, Spearman rank correlation coefficient was calculated using a bivariate technique. All analyses were performed using the SPSS software, version 13.0 (SPSS, Inc, Chicago, IL). The level of significance was set at P < .05.
3. Results
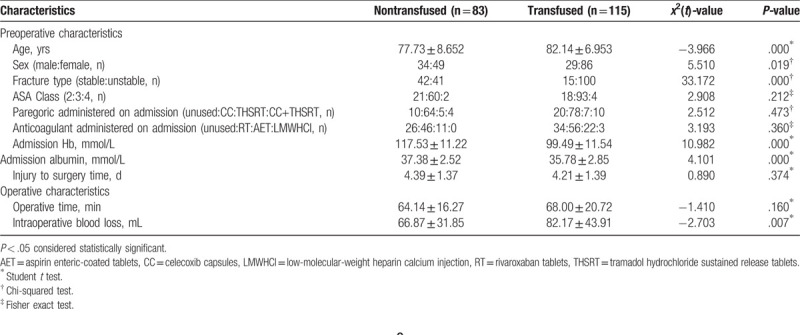
One hundred and ninety-eight of the 238 patients who treated with PFNA were included in the final analysis (Fig. 1). A total of 58.1% of patients (115/198) required perioperative blood transfusion, 3% (6/198) of the patients were transfused preoperatively, 53.5% (106/198) of the patients were transfused postoperatively, and only 1.5% (3/198) of the patients were transfused intraoperatively. Table 1 shows the general characteristics and the univariate analysis of the study population. The perioperative transfused group had a significantly higher mean age (P = .000), more female (P = .019), more unstable fractures (P = .000), lower mean admission Hb (P = .000), lower mean admission albumin (P = .000), and more intraoperative blood loss (P = .007).
Table 1.
Baseline characteristics of both groups.
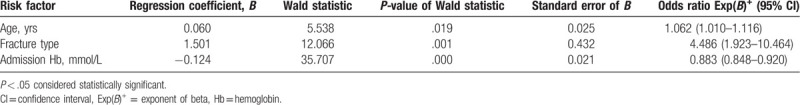
Using the build sample, multivariable logistic regression analysis of 11 potential factors revealed 3 independently predictors of postoperative blood transfusion after the application of PFNA in the treatment of elderly patients with FIF: age (OR = 1.062, 95% CI 1.010–1.116, P = .019), fracture type (OR = 4.486, 95% CI 1.923–10.464, P = .001), and admission Hb (OR = 0.883, 95% CI 0.848–0.920, P = .000) (Table 2). We made an in-depth analysis of our result and found that each increase of 1 point Hb is associated with a reduction in odds of transfusion of 11.7%.
Table 2.
Multivariate logistic regression analysis: significant risk factors for postoperative blood transfusion in elderly patients with femoral intertrochanteric fracture.
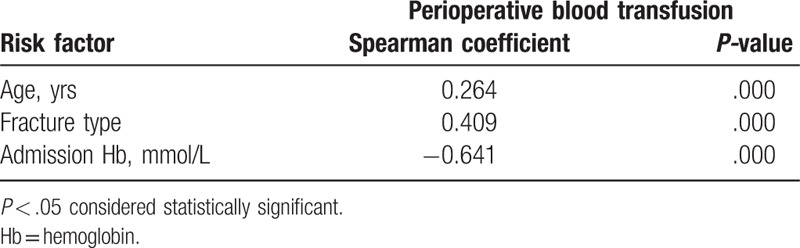
Then, according to Spearman's rank correlation analysis revealed that a positive correlation between perioperative blood transfusion and age (r = 0.264, P = .000) and type of fracture (r = 0.409, P = .000) in our study. A significantly negative correlation was found between perioperative blood transfusion and Hb concentration (r = −0.641, P = .000) (Table 3).
Table 3.
Spearman rank correlation analysis.
4. Discussion
With the rapid increase in the number of the elderly population, a clear rising trend is being observed in the morbidity and mortality of patients with FIF.[13] The mortality is known to increase with pre- or postoperative anemia.[14] In addition, Foss and Kehlet noted that postoperative anemia was associated with higher medical complications and increased length of hospital stay.[15] Therefore, regular perioperative monitoring is necessary to avoid anemia. Patients with normal preoperative Hb values may undergo surgery without allogeneic blood transfusion. The early identification of these patients might save unnecessary blood cross-matching. The purpose of the present study was to define a method to predict the need for an allogeneic blood transfusion in elderly patients admitted with FIFs. This study is important because the ability to predict the need for blood transfusion is the 1st step in determining whether timely monitoring of Hb to avoid anemia complications in patients with FIF. In addition, the frequency of blood routine review can be reduced in patients who do not need blood transfusion, which may reduce the financial burden of elderly patients.
This study focused on the factors of perioperative blood transfusion that predict the need for such transfusions based on available institutional data and transfusion protocols. Logistic regression analysis revealed that patients with FIF who are older, with more unstable fractures, and with lower admission Hb level are more likely to need perioperative blood transfusion.
Among the factors assessed to establish whether they were related to perioperative blood transfusion in patients with unilateral FIF, several of these had been studied previously. Aldebeyan et al[16] confirmed that hypoalbuminemia was closely related to complications in patients with hip fractures, but they did not directly assess the relationship between admission albumin and perioperative blood transfusion in elderly patients with FIF. As is summarized in Table 1, univariate analysis showed that admission albumin in the transfused group was lower than that in the nontransfused group. When controlling for other factors in multivariate analysis, there was no significant relation between the admission albumin and perioperative blood transfusion. The cause of this relationship is not known, but could be due to the fact that improving nutrition from food might be encouraged for patients upon admission. Some studies found that the use of platelet inhibitors has been linked to increased blood loss and transfusion requirements,17,18 whereas others have failed to show this association.19,20 Madsen et al[21] mentioned that high ASA grade was an independent risk factor for blood transfusion, whereas previous study failed to show this association.[22] In contrast with these studies,17,18,21 we found no significant relation between the ASA class, anticoagulant administration on admission and perioperative blood transfusion. In line with our findings, Hou et al[20] also reported that ASA class and anticoagulant on admission had no effect in perioperative blood transfusion. Moreover, the results of our study also suggested that operative time had no significant relationship with perioperative blood transfusion, which was consistent with Dillon's results.[22] Likewise, Hou et al[20] indicated that injury to surgery time had no significant relationship with perioperative blood transfusion, which was in accordance with our results. In addition, our results also showed that there was no correlation between sex and postoperative blood transfusion in the multivariate regression analysis, but an increased rate of blood transfusion was observed for more female in the univariate analysis, which was consistent with Madsen's results.[21] This association between sex and perioperative blood transfusion can be caused by confounding factors such as the hemoglobin levels. Because female have a lower normal reference range for hemoglobin than men but the transfusion threshold is not correspondingly lowered for female.
The multivariate regression analysis showed that there was no correlation between intraoperative blood loss and postoperative transfusion risk, but an increased rate of blood transfusion was observed for more intraoperative blood loss in the univariate analysis. The reason for this can be the fact that intraoperative blood loss, also called visible blood loss, was estimated based on the suction apparatus and swab weight, as defined in this study, but the perioperative hidden blood loss of intertrochanteric fracture was substantial, especially in elderly, with an excess of up to 6 times that observed during the surgical procedure.[15] Thus, the perioperative hidden blood loss is a confounding factor.
In this series, we specifically compared the results in patients with stable and unstable fracture patterns. We found that fracture type was a strong predictor of blood transfusion. The OR for postoperative blood transfusion was 4.486 for elderly patients with unstable FIF compared with that for patients with stable fracture. The reasons of perioperative blood transfusion of unstable fracture may be due to the instability and more bony bed bleeding at the fracture site. In addition, the fracture site may be exposed if closed reduction is not successful in the patient with unstable fracture, which may also increase bleeding and the risk of blood transfusion.
One of the best predictors of perioperative blood transfusion is, as also shown in our study, the admission Hb level. In our study, the average Hb level on admission of the nontransfused group was higher than that of the transfused group (117.53 ± 11.22 g/L vs 99.49 ± 11.54 g/L). In line with our findings, previous studies6,22 also reported that the admission Hb was an important indicator of potential perioperative blood transfusion. This is not surprising as the Hb level is a direct measurement of the patients’ RBC reserve and is also the parameter most frequently used to guide transfusion, which is also the case here.
Our study showed that old age can predict the need for perioperative blood transfusions in patients with FIFs, which was consistent with Dillon's results.[22] Patients in the transfused group were older than those in the nontransfused group (82.14 ± 6.953 years vs 77.73 ± 8.652 years). The reasons may be due to the vascular sclerosis and soft-tissue relaxation in elderly patients, which provided storage space for hemorrhage from fracture site. McManus et al[23] also reported that the radioisotope-labeled RBCs entered the interstitial space and did not participate in the systemic circulation postoperatively, which might lead to a further decline in the Hb level.
The advantage of our study are that the selected subjects were all elderly patients with FIF and all patients adopt the same fixation method of PFNA, which making our findings reproducible and highly generalizable. With a total of 198 patients who underwent same procedure, our study was sufficiently powered to identify the risk factors of perioperative blood transfusion in elderly patients with FIF. However, this study also had some limitations. First, the study's design led to data being obtained retrospectively; therefore, the final results depended on the accuracy of the documentation. Second, although the decision to transfuse was based on the restrictive transfusion policy, the final decision to transfuse was made by surgeons or anesthetists, which may have affected the outcome of the study. Third, the ASA class rather than comorbidities was used as a risk factor, which could have biased the results to some extent. Fourth, a number of complications during hip surgery, such as vascular injuries which had been reported by Tiftikçi and Serbest,[24] might influence the outcome, but these data were not available. Fifth, the sample size of our study was relatively small, which may have influenced the research results. Therefore, a follow-up with a larger sample size is warranted.
5. Conclusion
We found that the main factors affecting perioperative blood transfusion are age, fracture type, and admission Hb concentration. These results suggest that in high-risk patients who are older in age, more unstable fractures and lower admission Hb, we should monitor the changes of Hb concentration during the perioperative period, especially preoperatively and within 3 days after surgery, to timely correct severe anemia and to avoid exacerbating existing underlying diseases and inducing severe complications.
Author contributions
Cheng-Qian Dai designed the study. Cheng-Qian Dai, Li-Hong Wang, Ye-Qin Zhu and Guo-Hong Xu acquired the data, which Jun-Biao Shan, Wei-Chun Huang, Li-Hong Wei, Fang-Lun Zhou and Yong Li analyzed. Cheng-Qian Dai wrote the article, which all authors reviewed and approved for publication.
Footnotes
Abbreviations: ASA = American Society of Anesthesiologists, CIs = confidence intervals, FIF = femoral intertrochanteric fracture, Hb = hemoglobin, OR = odds ratio, PFNA = proximal femoral nail antirotation, RBC = red blood cell.
How to cite this article: Dai CQ, Wang LH, Zhu YQ, Xu GH, Shan JB, Huang WC, Wei LH, Zhou FL, Li Y. Risk factors of perioperative blood transfusion in elderly patients with femoral intertrochanteric fracture. Medicine. 2020;99:15(e19726).
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
The authors have no funding and conflicts of interest to disclose.
References
- [1]. Xu Y, Geng D, Yang H, et al. Treatment of unstable proximal femoral fractures: comparison of the proximal femoral nail antirotation and gamma nail 3. Orthopedics 2010;33:473. [DOI] [PubMed] [Google Scholar]
- [2]. Johnston P, Wynn-Jones H, Chakravarty D, et al. Is perioperative blood transfusion a risk factor for mortality or infection after hip fracture? J Orthop Trauma 2006;20:675–9. [DOI] [PubMed] [Google Scholar]
- [3]. Foss NB, Kristensen MT, Kehlet H. Anaemia impedes functional mobility after hip fracture surgery. Age Ageing 2008;37:173–8. [DOI] [PubMed] [Google Scholar]
- [4]. Foss NB, Kristensen MT, Jensen PS, et al. The effects of liberal versus restrictive transfusion thresholds on ambulation after hip fracture surgery. Transfusion 2009;49:227–34. [DOI] [PubMed] [Google Scholar]
- [5]. Khan AM, Mushtaq N, Giannakas K, et al. Cross-match protocols for femoral neck fractures--finding one that can work. Ann R Coll Surg Engl 2004;86:11–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6]. Kurdy NM, Hokan R. A cross-matching policy for fractures of the proximal third of the femur. Injury 1993;24:521–4. [DOI] [PubMed] [Google Scholar]
- [7]. Audet AM, Andrzejewski C, Popovsky MA. Red blood cell transfusion practices in patients undergoing orthopedic surgery: a multi-institutional analysis. Orthopedics 1998;21:851–8. [DOI] [PubMed] [Google Scholar]
- [8]. Carson JL, Duff A, Berlin JA, et al. Perioperative blood transfusion and postoperative mortality. JAMA 1998;279:199–205. [DOI] [PubMed] [Google Scholar]
- [9]. Carson JL, Hill S, Carless P, et al. Transfusion triggers: a systematic review of the literature. Transfus Med Rev 2002;16:187–99. [DOI] [PubMed] [Google Scholar]
- [10]. Hill SR, Carless PA, Henry DA, et al. Transfusion thresholds and other strategies for guiding allogeneic red blood cell transfusion. Cochrane Database Syst Rev 2002;CD002042. [DOI] [PubMed] [Google Scholar]
- [11]. Jensen JS, Sonne-Holm S, Tondevold E. Unstable trochanteric fractures. A comparative analysis of four methods of internal fixation. Acta Orthop Scand 1980;51:949–62. [DOI] [PubMed] [Google Scholar]
- [12]. Jensen JS. Classification of trochanteric fractures. Acta Orthop Scand 1980;51:803–10. [DOI] [PubMed] [Google Scholar]
- [13]. Bergstrom U, Jonsson H, Gustafson Y, et al. The hip fracture incidence curve is shifting to the right. Acta Orthop 2009;80:520–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14]. Carson JL, Poses RM, Spence RK, et al. Severity of anaemia and operative mortality and morbidity. Lancet 1988;1:727–9. [DOI] [PubMed] [Google Scholar]
- [15]. Foss NB, Kehlet H. Hidden blood loss after surgery for hip fracture. J Bone Joint Surg Br 2006;88:1053–9. [DOI] [PubMed] [Google Scholar]
- [16]. Aldebeyan S, Nooh A, Aoude A, et al. Hypoalbuminaemia-a marker of malnutrition and predictor of postoperative complications and mortality after hip fractures. Injury 2017;48:436–40. [DOI] [PubMed] [Google Scholar]
- [17]. Manning BJ, O’Brien N, Aravindan S, et al. The effect of aspirin on blood loss and transfusion requirements in patients with femoral neck fractures. Injury 2004;35:121–4. [DOI] [PubMed] [Google Scholar]
- [18]. Chechik O, Thein R, Fichman G, et al. The effect of clopidogrel and aspirin on blood loss in hip fracture surgery. Injury 2011;42:1277–82. [DOI] [PubMed] [Google Scholar]
- [19]. Collinge CA, Kelly KC, Little B, et al. The effects of clopidogrel (Plavix) and other oral anticoagulants on early hip fracture surgery. J Orthop Trauma 2012;26:568–73. [DOI] [PubMed] [Google Scholar]
- [20]. Hou G, Zhou F, Tian Y, et al. Predicting the need for blood transfusions in elderly patients with pertrochanteric femoral fractures. Injury 2014;45:1932–7. [DOI] [PubMed] [Google Scholar]
- [21]. Madsen CM, Jorgensen HL, Norgaard A, et al. Preoperative factors associated with red blood cell transfusion in hip fracture patients. Arch Orthop Trauma Surg 2014;134:375–82. [DOI] [PubMed] [Google Scholar]
- [22]. Dillon MF, Collins D, Rice J, et al. Preoperative characteristics identify patients with hip fractures at risk of transfusion. Clin Orthop Relat Res 2005;439:201–6. [DOI] [PubMed] [Google Scholar]
- [23]. McManus KT, Alavi VM, Lotke A, PA Noninvasive assessment of postoperative bleeding in TKA patients with Tc-99m RNCs. J Nucl Med 1987;28:565–7. [Google Scholar]
- [24]. Tiftikçi U, Serbest S. Periprosthetic proximal medial femoral cortical destruction caused by a femoral arterial pseudoaneurysm. Clin Interv Aging 2015;10:1967–70. [DOI] [PMC free article] [PubMed] [Google Scholar]


