Abstract
Parasitic diseases have been widely epidemic in China with a long history. Great endeavours made in past 70 years led to significant decrease in morbidity and mortablity caused by several major parasitic diseases, while challenges existed to eliminate parasitic diseases. Surveillance-response system has play a crucial role in identifying public health problems, ascertaining the distribution and epidemic dynamics, discovering outbreaks and epidemic anomalies, evaluating the effects of on-site intervention activities and identifying risk factors. In this article, we reviewed the progress of the surveillance system for parasitic diseases, analysed the role of NIPD in the construction and application of surveillance-response system of parasitic diseases through elaborating the surveillance activities and typical surveillance-response events led by NIPD. Suggestion and comments for improve the surveillance-response system were put forward for further control or elimination of parasitic diseases.
Keywords: Parasitic diseases, Surveillance-response system, Development and progress, NIPD
1. Background
Surveillance refers to the continuous and systematic collection of data and information, followed by analysis and interpretation of information related to public health plans and assessments, as well as the timely use of information for disease prevention and control (Groseclose and Buckeridge, 2017). The purposes of parasitic disease surveillance, specifically, is to monitor the occurrence and development patterns of diseases, provide prompt feedback and analysis of effective information, as well as to respond to and initiate rapid emergency responses (German, 2000; Yang et al., 2012). Additionally, an early warning consists of an advanced prediction that an epidemic may reach a dangerous level or an epidemic event is going to be occurred (Ameme et al., 2016). Such warnings are made with respect to a series of epidemic indicators or a possible epidemic event, based on long-term surveillance data and other basic information. It also involves the timely forecasting of development trends regarding an epidemic at a spatiotemporal level and minimizing the harm caused by the spread or occurrence of the epidemic. Alternatively, a response refers to the actions taken by the local government or agency based on the level of early warning, involving the felicitous organization of resources to carry out the emergency response plan, prevent the spread of the epidemic or reduce the extent of harm caused, to ensure the health safety of the population (Perry et al., 2007; Ren et al., 2016). Therefore, surveillance, early warnings, and responses must be strategically combined, well-coordinated, and enable a collaborative division of labour to improve the sensitivity of the surveillance system, thereby achieving the expected outcome of controlling transmission or spread of parasitic diseases (Fig. 1 ) (Tambo et al., 2014).
Fig. 1.
Relationships between surveillance, early warnings, and responses.
The transmission of parasitic diseases is influenced by many factors, such as the ecological environment, distribution of intermediate host, as well as natural factors including temperature, humidity, rainfall, and social factors including economic development, population mobilization, entertainment or production behaviours of the population (Cheng et al., 2016). Therefore, surveillance has always been a key aspect for parasitic diseases control in China. Since the establishment of our institute, most notably since it was renamed the National Institute of Parasitic Diseases, Chinese Center for Disease Control and Prevention (Zhou et al., 2005), we have gradually established and continuously improved a surveillance-response system for parasitic diseases based on the control stages of key parasitic diseases. This system has played a crucial role in understanding the epidemic dynamics, transmission patterns, and influencing factors of parasitic diseases in China, thereby facilitating the early detection of epidemics and guiding their management; while promoting on-site prevention and control activities (Feng et al., 2016b). Herein, we review the work carried out by our institute on constructing a national key parasitic disease surveillance network and developing emergency responses to epidemic events.
2. History of the parasitic disease surveillance system in China
According to the aims and surveillance contents, infectious disease surveillance in China primarily underwent three different stages, namely, disease surveillance, epidemiological surveillance, and public health surveillance (Zhou et al., 2013). Parasitic disease surveillance has also developed continuously alongside advances in surveillance technologies and changes in endemicity, which has been accompanied by expansion in terms of the scope and contents of surveillance. Monitoring surveillance sites, thematic surveillance, risk surveillance, and case reporting all served as key elements in the parasitic disease surveillance system and played unique roles over time.
2.1. Surveillance site monitoring
As schistosomiasis was given high priority by central government since the founding of the People's Republic of China, from 1950 to 1970, disease surveillance was adopted as the primary approach to carry out snail surveys focused on the occurrence and outcome (recovery or death) of schistosomiasis. This provided a reliable basis guiding for treating patients and controlling schistosomiasis outbreaks. Since 1990, the Bureau of Disease Control of the former Ministry of Health commissioned the Shanghai Medical University to conduct schistosomiasis surveillance in 14 villages of eight provinces (municipalities), which were enlarged to 21 epidemic surveillance sites from 2000 to 2004. In addition to epidemic indicators, the surveillance content also included epidemiological factors, which provided a scientific basis for understanding the epidemic changes of schistosomiasis in China and evaluating the effectiveness of different interventions (Yuan et al., 2002).
In 2002, the National Institute of Parasitic Diseases (NIPD), Chinese Academy of Preventive Medicine, renamed the National Institute of Parasitic Diseases, Chinese Center for Disease Control and Prevention, accompanying a reform from a research institute to a national institute responsible for providing technical support and guidance for national parasitic disease control and elimination through organizing national surveillance, data collection and analysis, response to parasitic disease outbreaks, etc. Construction of the infectious disease and vector surveillance network was initiated in 2005, including surveillance on schistosomiasis, malaria, soil- and food-borne parasitic diseases, and other related diseases (Chen et al., 2020). In response to changes in the strategies used for preventing and controlling each disease, our institute has organized and updated the surveillance programs in a timely manner, with adjustment or expansion of content and scope of surveillance (Xu et al., 2015).
For schistosomiasis, the national surveillance scheme evolved three versions, first developed in 2005 and upgraded in 2011 followed by revision in 2014. The surveillance scope was expanded from 80 surveillance sites in 10 provinces to the current 100% coverage rate of all schistosomiasis-endemic counties plus four counties (cities, districts) in the Three Gorges Reservoir Region which were regarded as having potential risk of schistosomiasis transmission (Table 1 ) (Zhu et al., 2013). For malaria, it was switched to the National Malaria Elimination Surveillance Program from sentinel surveillance since 2015 (Feng et al., 2016a). The National Soil-Borne Nematodiasis Surveillance Program was piloted in 2006, which was further revised in 2011 and 2016, respectively. In addition, our institute has established the National Lymphatic Filariasis Post-elimination Surveillance Program, the Pilot Program for Angiostrongyliasis Symptom Surveillance, and the Early Warning Dissemination Program (2008 version) as well as the National Echinococcosis Surveillance Program (2016 version).
Table 1.
Upgrades and adjustments to the schistosomiasis surveillance program.
| No. | Version (issue no.) | Surveillance objectives | Surveillance scope | Main content |
|---|---|---|---|---|
| 1 | 2005 pilot version (MOH-DDC [2005]74) |
|
A total of 80 surveillance sites in 10 provinces, autonomous regions, and municipalities | Routine surveillance, sudden outbreak surveillance, and sentinel surveillance (including survey on infection situation of residents, livestock and snails using serological test and microscopy techniques, as well as epidemiological factors) |
| 2 | 2011 revised edition (CCDC [2011]336) |
|
A total of 81 surveillance sites in 12 provinces, autonomous regions, and municipalities nationwide | Routine surveillance, sudden outbreak surveillance, and sentinel surveillance (including survey on infection situation of residents, livestock and snails using serological test and microscopy techniques, as well as epidemiological factors) |
| 3 | 2014 version (CCDC [2014]420) |
|
National schistosomiasis surveillance sites were set up in all schistosomiasis-endemic counties nationwide and some counties in the Three Gorges Reservoir Region. Three types of regions were classified: transmission-uninterrupted counties, transmission-interrupted counties, the and Three Gorges Reservoir Region | Routine surveillance (including case reports, case studies, early warning of acute schistosomiasis, sudden outbreak reports), sentinel surveillance (including survey on infection situation of residents, livestock and snails using serological test and microscopy techniques, as well as epidemiological factors), and risk surveillance (including infected snail surveillance and wild faeces surveillance using molecular biological methods) |
During the process of updating and improving the surveillance programs and implementing on-site organization, our institute actively fulfilled the roles of technical support, data management, and quality control. This not only enabled the continuous enrichment and improvement of the National Key Parasitic Disease Surveillance Network, but also provided a scientific basis for grasping the epidemic dynamics of parasitic diseases in China, understanding their epidemiological patterns and influencing factors, while also formulating and adjusting prevention and control measures.
2.2. Thematic surveillance
During various stages of prevention and control, our institute led and organized several national thematic surveys. Three national epidemiological-sampling surveys for schistosomiasis were conducted in 1989, 1995, and 2004, before, during and after the implementation of the World Bank Loan project for schistosomiasis control in P.R. China, respectively (Table 2 ) (Wu et al., 2007; Xu et al., 2016). The data obtained from these surveys presented the endemic status and explored the transmission patterns of schistosomiasis nationwide at that time, thus provided reference for developing the national control programs and modifying the control strategy or intervention activities.
Table 2.
Parasitological data of the three national sampling survey of schistosomiasis in China.
| Year of national sampling survey | No. villages sampled | Estimated no. people infected | Prevalence in human (%) | Prevalence in bovine (%) |
|---|---|---|---|---|
| 1989 | 353 | 1,638,103 | 10.2 | 13.3 |
| 1995 | 364 | 865,084 | 4.9 | 9.1 |
| 2004 | 239 | 726,112 | 5.1 | 5.7 |
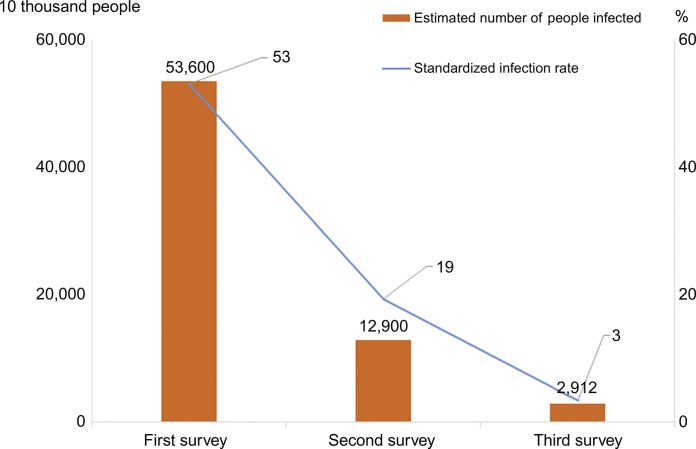
Moreover, three national surveys on the current status of key human parasitic diseases were carried out in 1988, 2002, and 2016 (Fig. 2 ) (Zhu et al., 2015), and a national survey on angiostrongyliasis epidemic foci was conducted in 2006 (Lv et al., 2009). These national cross-sectional surveys provided objective scientific data supporting comprehensive evaluation of the prevalence of parasitic diseases at different stages and progress in their prevention and control, while also providing basic information for formulating prevention and control plans at the various stages.
Fig. 2.
Three rounds national surveys on key human parasitic diseases vs the prevalence of soil-borne nematode infections.
2.3. Risk surveillance
At the turn of the 21st century, ecological changes in the environment caused by global warming, large-scale water conservation projects, increased population mobility, economic and trade development together with other social factors increased the transmission risks of parasitic diseases. Accordingly, our institute has organized and conducted several thematic risk surveillance programs, primarily focused on schistosomiasis. To evaluate the impact of climate change and large-scale water conservation projects on schistosomiasis transmission, especially for former non-endemic regions, risk surveillance was performed on snails' spread and infection status of schistosomiasis in mobile populations in 11 counties (cities) of 5 provinces (municipalities), near or along the Three Gorges Dam and the South–North Water Diversion Project, from 2008 to 2011 (Fig. 3 ). The surveillance showed that although no snail was spread to non-endemic areas, Oncomelania hupensis could survive in Caohu and Jining city in non-endemic areas and several stool positives were found in mobile populations in surveillance sites. Surveillance should be strengthened and continued in such regions (Dang et al., 2014).
Fig. 3.
Distribution of surveillance sites for potential schistosomiasis-endemic regions.
To improve the sensitivity of schistosomiasis surveillance and the early warning system, in 2010–16, the sentinel-mouse method was used for monitoring and identifying the transmission risk in major water bodies susceptible to schistosomiasis in seven provinces (Hunan, Hubei, Jiangxi, Anhui, Jiangsu, Yunnan, and Sichuan). The annual results indicated that the potential risk still exist in the lake and marshland regions although the prevalence of schistosomiasis in these regions has decreased to below the transmission control threshold (Zheng et al., 2013).
For each type of risk surveillance, the content and scope were configured and adjusted according to the actual needs of the prevention and control site. This not only helped us understand the potential transmission risks and its distribution, but also further enriched and improved on-site surveillance systems.
2.4. Case report based on active information reporting system
In 2004, an epidemic-network, direct reporting system based on infectious disease case reports was established and officially launched nationwide. This system greatly improved the coverage range, timeliness, sensitivity, and accuracy of reports on epidemic events, essentially achieving the overall goal of complete epidemic surveillance reporting (Yang et al., 2011). Thereafter, the Chinese Disease Prevention and Control Information System (with nationwide coverage) was gradually improved, with the Infectious Disease and Public Health Emergency Surveillance Report Information System as its core (Lai et al., 2014). This created a precedent for the implementation of “case, real-time, online” reporting in the field of public health in China, which fundamentally differed from the approach of the previous reporting system based on monthly reports and data aggregation by county (Li et al., 2012).
To meet the needs of key parasitic disease prevention and control strategies, The Information-management System for Parasitic Disease Control was officially launched in 2010, which was spearheaded by the Chinese Center for Disease Control, designed by NIPD, and assisted by Sinosoft Co., Ltd. (Li et al., 2010). The online system was an advance over paper-based reports in terms of data collection processes, reporting, querying statistics, analysis, and other aspects. Alongside the in-depth development of the surveillance work, this system was upgraded in 2012 and 2016. In May 2017, it was incorporated into the Chinese disease prevention and control information system platform allowing for implementation of unified system user authentication and authorization management, which not only enhanced the system security, but also improved the timeliness of epidemic reporting for key parasitic diseases, thereby playing important roles in the standardization of programmatic epidemic management and surveillance.
3. Surveillance work organized by NIPD and its role
Since 2002, NIPD has become the technical center for the national programs of parasitic diseases control, undertaking the technical guidance, organizing disease monitoring and surveillance, assessing the effects of national programs or strategies for parasitic disease control, as well as the relevant emergency responses to outbreaks of parasitic diseases and public health emergencies. The surveillance network which established by NIPD plays a crucial role in identifying public health problems, ascertaining the distribution and epidemic dynamics of major parasitic diseases nationwide, discovering outbreaks and epidemic anomalies, evaluating the effects of on-site intervention activities and identifying risk factors as well as at-risk populations and regions. Collectively, these activities effectively promote national programs of key parasitic diseases control. In this section, case studies will be presented to introduce the different roles served by the surveillance work organized by NIPD (Fig. 4 ).
Fig. 4.
Major roles of public health surveillance.
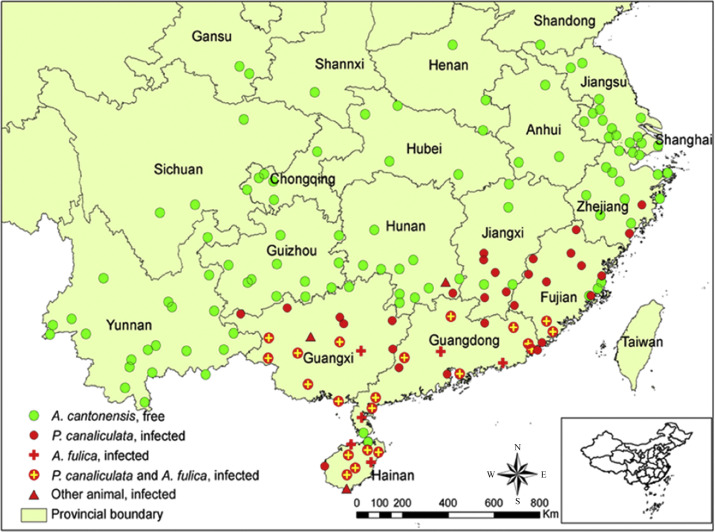
3.1. Identifying public health problems
In June 2006, a food-borne outbreak of angiostrongyliasis occurred in Beijing due to eating raw snails infected with Pomacea canaliculata (Wang et al., 2010). NIPD cooperated with the relevant agencies to undertake epidemiological surveys. A total of 160 clinically diagnosed cases were discovered, and an outbreak of food-borne angiostrongyliasis was confirmed. However, at that time, limited information was available regarding the prevalence of angiostrongyliasis and the distribution of epidemic foci in China. In light of this, after the epidemic was effectively managed, NIPD, with the support of the former Ministry of Health, organized a systematic national survey pertaining to the epidemic foci of angiostrongyliasis in 2007 and 2008 consecutively (Fig. 5 ) (Lv et al., 2009) to investigate the distribution and diffusion of A. cantonensis as well as its hosts. By clarifying the epidemic foci of this disease, the distribution of intermediate and definitive hosts and their infection status we gained further insights into the public health risks posed by angiostrongyliasis. In 2009, a pilot program for symptom surveillance and early warnings of angiostrongyliasis transmission was launched, which drove the surveillance, prevention, and control of angiostrongyliasis in various regions, thus controlling or decreasing the public health risk caused by angiostrongyliasis.
Fig. 5.
Survey results of angiostrongyliasis epidemic foci.
3.2. Grasping the distribution and trends of parasitic diseases
Following the large-scale prevention and control strategy for filariasis in China, surveillance became an important component for the control and elimination of filariasis (De-Jian et al., 2013). In the 1970s, surveillance began the next year since the endemic province reached the threshold of basic elimination of filariasis, primarily focusing on the discovery and elimination of residual sources of infection to consolidate the results of prevention and control. In the 1980s, after clarifying the indications for interrupting the transmission of filariasis, longitudinal surveillance was performed to observe dynamic changes of microfilaremia situation in human populations, and to confirm that microfilaremia and natural larval infections could no longer be found in human populations and mosquito vectors (Wang et al., 1998). By the 1990s, horizontal surveillance, longitudinal surveillance, and surveillance of floating populations were conducted to understand the changes of microfilaremia rates, the transmission trends of filariasis in human populations, as well as the status of microfilaria infections in floating populations and their impact on the elimination of filariasis. These studies provided evidence for the elimination of filariasis within a region (Fang and Zhang, 2019). In 2001, NIPD participated in the preparation of the Regional Surveillance Program for the Elimination of Filariasis and reviewed the regions that had eliminated filariasis in an effort to continue identifying and monitoring potentially weak links in terms of prevention, control, and surveillance. Since 2004, verification of filariasis elimination based on case reporting was conducted under the technical support of NIPD. Reviewing the history of filariasis surveillance can provide basic information for understanding its distribution in China while also highlighting changes in human infection rates at different stages and consolidating the achievements of filariasis elimination, thus providing a scientific basis for sustained elimination of filariasis in China.
3.3. Discovering outbreaks and epidemic anomalies
In 2005, NIPD experts noticed a sharp rise in the number of malaria cases in Anhui Province. The number of reported cases increased by over 70%, compared with that in the same period of the previous year, and appeared to be a localized outbreak. The cases were primarily concentrated in the Huanghuai River Basin, specifically in the counties (districts) of Guoyang, Mengcheng, Huaiyuan, and Guzhen, where Anopheles sinensis was the main vector of Plasmodium (Zhang et al., 2008). After reporting to the former Bureau of Disease Control of the Ministry of Health, NIPD provided technical support to local Diseases Control Center for spring interregnum treatment and health education. The Anhui Spring Interregnum Radical Treatment Program was formulated with the support of NIPD, followed by on-site supervision of treatment by NIPD experts. After implementation of effective intervention over two epidemic seasons, the reported number of malaria cases in Anhui Province decreased significantly and malaria was deemed to be effectively controlled (Pan et al., 2012).
3.4. Evaluating the effects of interventions
In 2006, the former Ministry of Health established Demonstration Pilots of Comprehensive Control for Parasitic Diseases. To evaluate the effects of integrated interventions in these demonstration areas and explore the sustainable development mechanisms for parasitic diseases control, NIPD actively conducted longitudinal observations in 12 demonstration pilots from 2011 to 2013. This enabled the continuous implementation of comprehensive prevention and control measures, as well as effective development of surveillance programs for monitoring infections in the human population, which facilitated evaluation of prevention and control efforts in the demonstration zones while also providing reference for formulating the national plan for prevention and control of major parasitic diseases (Ying-Dan et al., 2019).
3.5. Identifying risk factors in different populations and regions
For the timely detection of high-risk regions during the schistosomiasis transmission season, in the first half year of 2009, NIPD collaborated with the Jiangsu and Jiangxi Provincial Institutes for Schistosomiasis Control to conducting risk analysis based on snail surveillance data collected throughout the spring in combination with epidemic data from previous years. Early warnings were put forward and indicated that the Jiangsu Yangtze River and Poyang Lake regions of Jiangxi Province were still with high risk of schistosomiasis transmission through spatio-temporal analysis (Li et al., 2014).
Surveillance serves as the foundation for guiding effective performance of parasitic disease emergency responses, as well as an effective means for evaluating the effects of emergency management. Natural disasters may alter the natural, social, and biological factors, leading to reoccurrence or spread of parasitic diseases, thus, NIPD organized risk assessments for major parasitic diseases, such as schistosomiasis, malaria, echinococcosis, and kala-azar in disaster areas based on the accumulated surveillance data when disasters occurred, such as the Wenchuan earthquake occurred in 2008, the Gansu Zhouqu mudslide in 2010 and the Sichuan Jiuzhaigou earthquake happened in 2017, etc. Assessment showed that high transmission risk occurred as a result of the disasters, as well as persistence of infection sources in endemic areas especially those vector- or food-borne parasitic diseases (Ren et al., 2016; Tambo et al., 2014). NIPD also coordinated with local disease control and prevention agencies to carry out symptom surveillance, health education, mosquito and lacewing control, and the promotion of self-protection in disaster areas. These measures prevented the occurrence or outbreaks of major parasitic diseases following the disasters. In addition, during a series of major events such as the Beijing Olympics held in 2008, the Shanghai World Expo in 2010, and the China International Import Expo, emergency preparedness was actively conducted to ensure the success and health safety of these events.
4. Emergency response mechanisms for parasitic diseases
Following the severe acute respiratory syndrome (SARS) outbreak in 2003, stemming from high concerns over safeguarding human health and safety, the Central Committee of the Chinese Communist Party and the State Council assigned high priority status to the construction and development of emergency response systems. Once these systems were established by the state, the establishment and development of health-related emergency response systems followed. Substantial progress was made in the construction of “one plan and three systems” (i.e. contingency plan, legal system, and institutional system and mechanisms), while the emergency response teams and their capabilities were also enhanced.
In the field of parasitic disease prevention and control, the contingency plan for the emergency response to major epidemics of schistosomiasis (Pilot) and the contingency plan for the emergency response to malaria outbreaks (Pilot) were drafted by NIPD. These were the first two emergency response-contingency plans issued by the former Ministry of Health after the SARS outbreak. After assessing their validity in pilot studies over 2 years, the contingency plan for the emergency response to schistosomiasis outbreaks and the contingency plan for the emergency response to malaria outbreaks were officially published in 2006, which provided guidance for increasing the rapidity and timeliness of response in various regions, while also providing guidance for proper preparation of epidemic emergency responses.
In combination with the needs of the health emergency support work performed during the 2008 Olympics, NIPD established an emergency reserve mechanism. Materials including diagnostic reagents, medicine and other related emergency supplies for parasitic disease control and prevention were stored and managed under the guide of China CDC. The emergency reserves are updated and renewed each year, thus providing material security for emergency responses to various outbreaks. In 2012, NIPD formulated and issued a contingency plan for the emergency response to sudden outbreaks of parasitic diseases. Accordingly, a leading group, an expert technical guidance group, and an emergency response team for health-related emergency response work were set up in NIPD and served as the inception of the emergency response-contingency plan, mechanism, and teams. The emergency response-contingency plan follows the principles of unified command, tiered responsibility, rapid response, reliance on science, and management based on the law, thus providing a mechanistic assurance for the emergency response to parasitic disease outbreaks.
5. Role of the emergency response system in managing parasitic diseases
In the 70 years since our institute was established, the parasitic disease emergency response system has undergone gradual improvements and has played important roles in the effective prevention and timely management of emergency responses to various, sudden epidemic outbreaks.
5.1. Case study I: Schistosomiasis outbreaks
Between August 4th and 10th, 2003, 10 acute schistosomiasis cases were reported in Shitai County, Anhui Province. In response, NIPD organized relevant experts in a timely manner to perform an epidemiological survey, and execute rapid prevention and control measures in collaboration with experts from the Anhui Provincial Institute for Schistosomiasis Control. This case represented the first emergency response management of an epidemic outbreak that our institute had participated in after its restructuring, leading to prevent the rebound and spread of schistosomiasis effectively.
In July 2005, five acute schistosomiasis cases were reported from Wa'er Village of Xide County, Sichuan Province, through the National Schistosomiasis Direct Reporting Network System. NIPD dispatched an expert team to conduct surveys on-site and supervise the prevention and control. By implementing a series of effective prevention and control measures, the acute schistosomiasis outbreak was rapidly under control (Li et al., 2009).
5.2. Case study II: Malaria outbreaks
In July 2007, a malaria outbreak occurred in Congjiang County, Guizhou Province. NIPD organized experts to perform an on-site survey, investigate the local malaria prevention and control status, and supervise the local implementation of comprehensive measures including case findings, treatment of patients and their family members, mosquitoes control, Anopheles density monitoring, and health education. The implementation of these measures effectively controlled the epidemic, and prevented its spread, while also targeted opinions and suggestions for strengthening the local malaria prevention and control measures, were provided (Sheng et al., 2007).
In July 2010, Neijiang City of Sichuan Province reported an adverse event related to the medication in an prophylactic malaria group through the National Public Health Incident Report Management Information System (Xuelan, 2019). NIPD rapidly organized experts to supervise the investigation and management in Neijiang City. The cause of the incident was ascertained, while guidance and suggestions were offered regarding the exposed problems in terms of formulating the corresponding technical plans and emergency response-contingency plan, strengthening capacity of grassroots programs through training, and improving the quality of group medications.
5.3. Case study III: Food-borne parasitic disease outbreaks
In February 2009, surveillance data from the National Public Health Emergency Report Management Information System indicated that a serious unexplained poisoning incident had occurred in Lanping County, Nujiang, Yunnan Province. As this incident was suspected to be caused by Trichinella spiralis infection, NIPD organized experts to carry out epidemiological surveys, pathogen examination, and serological testing, along with the local Disease Control Center, to identify its cause and verify the diagnoses. The feature and scope of the epidemic was accurately determined leading to the effective control of the trichinellosis outbreak within a short time.
On February 1, 2012, an epidemic of a suspected food-borne parasitic disease was reported in Binchuan County of the Dali Bai Autonomous Prefecture, Yunnan Province. Conventional anthelmintics such as praziquantel and albendazole were ineffective, and the cause of disease was unclear. NIPD dispatched experts to the field on February 2nd and 12th to conduct active case exploration, surveys on hosts and vectors, and diagnosis through pathogen, immunological, and molecular biological testing. A specific drug against fascioliasis (triclabendazole), reserved at NIPD, was used to perform interventional treatment. We confirmed that this epidemic was caused by Fasciola gigantica, and determined that Binchuan County of Dali Bai was a natural epidemic focus of F. gigantica. The NIPD experts supervised the treatment of cases and provided suggestions for further prevention and control measures (Chen et al., 2013).
5.4. Case study IV: Filariasis outbreaks
In August 2007, the Fuchuan County in Guangxi Province reported a case of filariasis through the Infectious Disease Epidemic Surveillance Network System. Subsequently, NIPD organized experts to conduct field investigation on this filariasis event and found that Ganshang and Yinshan Natural Villages in Fuchuan County, Guangxi Province were residual epidemic foci of Bancroft's filariasis (Xue-Ming et al., 2008). The experts suggested that post-elimination surveillance of filariasis should be strengthened and a national review of residual epidemic foci of filariasis should be conducted to ensure its elimination nationwide. Until now, no new case was detected through decades of surveillance.
5.5. Case study V: Imported Africa human trypanosomiasis
In August 2017, Fujian Provincial Center for Disease Control reported an imported case of African trypanosomiasis (Chen et al., 2019). Subsequently, NIPD led a team from the World Health Organization headquarters and the Fujian Center for Disease Control to review the case and conduct additional testing. Based on analysis of the patient's clinical symptoms, epidemiological history, and laboratory test results, the patient was regarded as the first imported case of Trypanosoma brucei in China. During the same month, Huashan Hospital (affiliated with Fudan University) reported another imported case of African trypanosomiasis. Experts from NIPD conducted investigations and timely testing allowing for the determination that the patient was the second imported case infected with Trypanosoma brucei. NIPD experts provided professional guidance for case treatment and follow-up, while also actively seeking the support from the World Health Organization to establish a drug reserve at NIPD for potential imported cases in future (Liu et al., 2018).
During the management of these various epidemic outbreaks, experts of NIPD fulfilled the role of being the “final voice” as a national team in case investigations and follow-up, field survey, on-site vector control, health education, etc. In addition, NIPD ensured the timely and effective management of epidemic outbreaks, while also safeguarded the security of public health through several measures, including the on-site emergency response management of various epidemic outbreaks, improving the material, techniques, and expert reserves of NIPD, adjusting and improving the emergency response commands and organization as well as coordination mechanisms, continuously improving emergency response-contingency plans, establishing multi-departmental cooperation mechanisms, and improving the level of emergency response.
6. Conclusion
With 70 years of relentless efforts, NIPD contributed greatly to parasitic disease control in China, with substantial developments and improvements in surveillance and response capabilities. However, due to the vast territory of China and the wide range and various parasitic species, certain neglected parasitic diseases remain endemic in remote and impoverished settings. Further, the parasitic diseases which have been controlled continue to face risks of transmission or rebound. With socioeconomic development and increase in tourism, trade exchanges have become more frequent, which implies that there is also a continuous rise in the threat of imported epidemics (Zhou et al., 2018). In addition, owing to dietary and lifestyle habits, outbreaks of certain food-borne parasitic diseases may also occur locally in some areas. Therefore, NIPD should strengthen the capability of surveillance and response to parasitic diseases, while continuously improving the sensitivity and rapidity of surveillance-response systems that are compatible with the progress of disease prevention and control systems (Chun-Li et al., 2017), all of which continue to offer important practical significance for prevention and control of parasitic diseases in the future.
Acknowledgments
Acknowledgements
This study was supported by the National Special Science and Technology Project for Major Infectious Diseases of China (Grant No. 2016ZX10004222-004), the fourth round of Three-Year Public Health Action Plan (GWIV-29).
Competing interest
The authors declare that they do not have competing interests.
Authors' contributions
Y.-W. Hao, Q. Wang and S.-Z. Li conceived the study; Y.-W. Hao, Q. Wang, J. Xu and S.-Z. Li wrote and revised the manuscript; C.-L. Cao, T. Tian, Z.-L. Zhu, S.-S. Zhou, W.-P. Wu, Y.-D. Chen, Y. Zhang, J.-X. Chen, N. Xiao and X.-N. Zhou revised the manuscript and gave approval of the version to be published. All the authors read and approved the final version of the manuscript.
Contributor Information
Qiang Wang, Email: wangqiang@nipd.chinacdc.cn.
Shi-Zhu Li, Email: lisz@chinacdc.cn.
References
- Ameme D.K., Nyarko K.M., Kenu E., Afari E.A. Strengthening surveillance and response to public health emergencies in the West African sub-region: the role of Ghana FELTP. Pan Afr. Med. J. 2016;25(Suppl. 1):1. doi: 10.11604/pamj.supp.2016.25.1.10579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J.X., Chen M.X., Ai L., Xu X.N., Jiao J.M., Zhu T.J., Su H.Y., Zang W., Luo J.J., Guo Y.H., Lv S., Zhou X.N. An outbreak of human fascioliasis gigantica in Southwest China. PLoS One. 2013;8(8) doi: 10.1371/journal.pone.0071520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen N., Jin K., Xu J., Zhang J., Weng Y. Human African trypanosomiasis caused by Trypanosoma brucei gambiense: the first case report in China. Int. J. Infect. Dis. 2019;79:34–36. doi: 10.1016/j.ijid.2018.11.004. [DOI] [PubMed] [Google Scholar]
- Chen J., Ding W., Li Z., Zhou D.D., Yang P., Wang R.B., Zheng B., Sheng H.F., Guan Y.Y., Xiao N., Li S.Z., Zhou X.N. From parasitic disease control to global health: new orientation of the National Institute of Parasitic Diseases, China CDC. Acta Trop. 2020;201:105219. doi: 10.1016/j.actatropica.2019.105219. [DOI] [PubMed] [Google Scholar]
- Cheng G., Li D., Zhuang D., Wang Y. The influence of natural factors on the spatio-temporal distribution of Oncomelania hupensis. Acta Trop. 2016;164:194–207. doi: 10.1016/j.actatropica.2016.09.017. [DOI] [PubMed] [Google Scholar]
- Chun-Li C., Le-Ping S., Qing-Biao H., Bian-Li X.U., Xiao-Nong Z. Establishment of response system to emergency parasitic disease affairs in China. Chin. J. Schistosomiasis Control. 2017;29(4):397–401. doi: 10.16250/j.32.1374.2017111. [DOI] [PubMed] [Google Scholar]
- Dang H., Xu J., Li S.Z., Cao Z.G., Huang Y.X., Wu C.G., Tu Z.W., Zhou X.N. Monitoring the transmission of Schistosoma japonicum in potential risk regions of China, 2008–2012. Int. J. Environ. Res. Public Health. 2014;11(2):2278–2287. doi: 10.3390/ijerph110202278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De-Jian S., Xu-Li D., Ji-Hui D. The history of the elimination of lymphatic filariasis in China. Infect. Dis. Poverty. 2013;2(1):30. doi: 10.1186/2049-9957-2-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang Y., Zhang Y. Lessons from lymphatic filariasis elimination and the challenges of post-elimination surveillance in China. Infect. Dis. Poverty. 2019;8(1):66. doi: 10.1186/s40249-019-0578-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng J., Liu J., Feng X., Zhang L., Xiao H., Xia Z. Towards malaria elimination: monitoring and evaluation of the “1-3-7” approach at the China-Myanmar border. Am. J. Trop. Med. Hyg. 2016;95(4):806–810. doi: 10.4269/ajtmh.15-0888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng Y., Liu L., Xia S., Xu J.F., Bergquist R., Yang G.J. Reaching the surveillance-response stage of schistosomiasis control in the People's Republic of China: a modelling approach. Adv. Parasitol. 2016;92:165–196. doi: 10.1016/bs.apar.2016.02.006. [DOI] [PubMed] [Google Scholar]
- German R.R. Sensitivity and predictive value positive measurements for public health surveillance systems. Epidemiology. 2000;11(6):720–727. doi: 10.1097/00001648-200011000-00020. [DOI] [PubMed] [Google Scholar]
- Groseclose S.L., Buckeridge D.L. Public health surveillance systems: recent advances in their use and evaluation. Annu. Rev. Public Health. 2017;38:57–79. doi: 10.1146/annurev-publhealth-031816-044348. [DOI] [PubMed] [Google Scholar]
- Lai S., Liao Y., Zhang H., Li X., Ren X., Li F., Yu J., Wang L., Yu H., Lan Y., Li Z., Wang J., Yang W. Comparing the performance of temporal model and temporal-spatial model for outbreak detection in China infectious diseases automated-alert and response system, 2011–2013, China. Zhonghua Yu Fang Yi Xue Za Zhi. 2014;48(4):259–264. [PubMed] [Google Scholar]
- Li S.Z., Luz A., Wang X.H., Xu L.L., Wang Q., Qian Y.J., Wu X.H., Guo J.G., Xia G., Wang L.Y., Zhou X.N. Schistosomiasis in China: acute infections during 2005–2008. Chin Med J (Engl) 2009;122(9):1009–1014. [PubMed] [Google Scholar]
- Li H.Z., Qiang W., Zheng C.J., Qian Z., Qian Y.J., Li S.Z., Wu X.H., Dong Y.F. Development and application of information system for parasitic diseases control and prevention. Chin. J. Schistosomiasis Control. 2010;22(04):301–303. [Google Scholar]
- Li Z., Yin W., Clements A., Williams G., Lai S., Zhou H., Zhao D., Guo Y., Zhang Y., Wang J., Hu W., Yang W. Spatiotemporal analysis of indigenous and imported dengue fever cases in Guangdong province, China. BMC Infect. Dis. 2012;12:132. doi: 10.1186/1471-2334-12-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li S.Z., Zheng H., Abe E.M., Yang K., Bergquist R., Qian Y.J., Zhang L.J., Xu Z.M., Xu J., Guo J.G., Xiao N., Zhou X.N. Reduction patterns of acute schistosomiasis in the People's Republic of China. PLoS Negl. Trop. Dis. 2014;8(5) doi: 10.1371/journal.pntd.0002849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Q., Chen X.L., Chen M.X., Xie H.G., Liu Q., Chen Z.Y., Lin Y.Y., Zheng H., Chen J.X., Zhang Y., Zhou X.N. Trypanosoma brucei rhodesiense infection in a Chinese traveler returning from the Serengeti National Park in Tanzania. Infect. Dis. Poverty. 2018;7(1):50. doi: 10.1186/s40249-018-0432-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lv S., Zhang Y., Liu H.X., Hu L., Yang K., Steinmann P., Chen Z., Wang L.Y., Utzinger J., Zhou X.N. Invasive snails and an emerging infectious disease: results from the first national survey on Angiostrongylus cantonensis in China. PLoS Negl. Trop. Dis. 2009;3(2) doi: 10.1371/journal.pntd.0000368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan J.Y., Zhou S.S., Zheng X., Huang F., Wang D.Q., Shen Y.Z., Su Y.P., Zhou G.C., Liu F., Jiang J.J. Vector capacity of Anopheles sinensis in malaria outbreak areas of central China. Parasit. Vectors. 2012;5:136. doi: 10.1186/1756-3305-5-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry H.N., McDonnell S.M., Alemu W., Nsubuga P., Chungong S., Otten M.W., Jr., Lusamba-dikassa P.S., Thacker S.B. Planning an integrated disease surveillance and response system: a matrix of skills and activities. BMC Med. 2007;5:24. doi: 10.1186/1741-7015-5-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren Z., Wang D., Ma A., Hwang J., Bennett A., Sturrock H.J., Fan J., Zhang W., Yang D., Feng X., Xia Z., Zhou X.N., Wang J. Predicting malaria vector distribution under climate change scenarios in China: challenges for malaria elimination. Sci. Rep. 2016;6:20604. doi: 10.1038/srep20604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheng H.F., Zheng X., Shi W.Q., Xu J.J., Jiang W.K., Wang D.Q., Tang L.H. Factors affecting malaria outbreak in Congjiang county of Guizhou Province. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi. 2007;25(3):225–229. [PubMed] [Google Scholar]
- Tambo E., Ugwu E.C., Ngogang J.Y. Need of surveillance response systems to combat Ebola outbreaks and other emerging infectious diseases in African countries. Infect. Dis. Poverty. 2014;3:29. doi: 10.1186/2049-9957-3-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang P., Wang F., Sun Y., Wang J., Kou J., Huang Y., Kang X., Wan G., Liang Y., Wang Q. Study on the transmission threshold value of bancroftian filariasis. Chin Med J (Engl) 1998;111(3):261–264. [PubMed] [Google Scholar]
- Wang J., Qi H., Diao Z., Zheng X., Li X., Ma S., Ji A., Yin C. An outbreak of angiostrongyliasis cantonensis in Beijing. J. Parasitol. 2010;96(2):377–381. doi: 10.1645/GE-2214.1. [DOI] [PubMed] [Google Scholar]
- Wu X.H., Wang X.H., Utzinger J., Yang K., Kristensen T.K., Berquist R., Zhao G.M., Dang H., Zhou X.N. Spatio-temporal correlation between human and bovine schistosomiasis in China: insight from three national sampling surveys. Geospat. Health. 2007;2(1):75–84. doi: 10.4081/gh.2007.256. [DOI] [PubMed] [Google Scholar]
- Xu J., Xu J.F., Li S.Z., Zhang L.J., Wang Q., Zhu H.H., Zhou X.N. Integrated control programmes for schistosomiasis and other helminth infections in P.R. China. Acta Trop. 2015;141(Pt. B):332–341. doi: 10.1016/j.actatropica.2013.11.028. [DOI] [PubMed] [Google Scholar]
- Xu J., Yu Q., Tchuente L.A., Bergquist R., Sacko M., Utzinger J., Lin D.D., Yang K., Zhang L.J., Wang Q., Li S.Z., Guo J.G., Zhou X.N. Enhancing collaboration between China and African countries for schistosomiasis control. Lancet Infect. Dis. 2016;16(3):376–383. doi: 10.1016/S1473-3099(15)00360-6. [DOI] [PubMed] [Google Scholar]
- Xuelan Z.J.Y. Analysis on the characteristics of emergency public health events in Neijiang City from 2004 to 2018. Parasitoses Infect. Dis. 2019;17(03):152–156. [Google Scholar]
- Xue-Ming L.I., Yang Y.C., Huang K.L., Hong-Bo X.U., Xie Z.Y., Mai F.Z., Shang S.M., Ai-Rong S.U., Shu-Lin L.I., Fang-Qi O.U. Discovery of a residual focus of bancroftian filariasis after declaration of its transmission interruption in Guangxi. Chin. J. Parasitol. Parasit. Dis. 2008;26(6):2–408. [PubMed] [Google Scholar]
- Yang W., Li Z., Lan Y., Wang J., Ma J., Jin L., Sun Q., Lv W., Lai S., Liao Y., Hu W. A nationwide web-based automated system for outbreak early detection and rapid response in China. Western Pac. Surveill. Response J. 2011;2(1):10–15. doi: 10.5365/WPSAR.2010.1.1.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang K., Sun L.P., Huang Y.X., Yang G.J., Wu F., Hang D.R., Li W., Zhang J.F., Liang Y.S., Zhou X.N. A real-time platform for monitoring schistosomiasis transmission supported by Google Earth and a web-based geographical information system. Geospat. Health. 2012;6(2):195–203. doi: 10.4081/gh.2012.137. [DOI] [PubMed] [Google Scholar]
- Ying-Dan C., Hui-Hui Z., Ji-Lei H., Ting-Jun Z., Xiao-Nong Z. Status and working principals of soil-transmitted nematodiasis during new period in China. Chin. J. Schistosomiasis Control. 2019;31(1):23–25. doi: 10.16250/j.32.1374.2018309. [DOI] [PubMed] [Google Scholar]
- Yuan H., Jiang Q., Zhao G., He N. Achievements of schistosomiasis control in China. Mem. Inst. Oswaldo Cruz. 2002;97(Suppl. 1):187–189. doi: 10.1590/s0074-02762002000900036. [DOI] [PubMed] [Google Scholar]
- Zhang W., Wang L., Fang L., Ma J., Xu Y., Jiang J., Hui F., Wang J., Liang S., Yang H., Cao W. Spatial analysis of malaria in Anhui province, China. Malar. J. 2008;7:206. doi: 10.1186/1475-2875-7-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng H., Li S.Z., Cao C.L., Zhang L.J., Sun L.P., Yang K., Tu Z.W., Li Y.Y., Yang W.P., Gu X.N., Wu Z.S., Feng X.G., Zhu R., Xu J., Xiao N., Zhou X.N. Surveillance and response for Schistosomiasis japonica based on sentinel mice examination for cercariae-infested water in risk region, 2012. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi. 2013;31(6):428–432. [PubMed] [Google Scholar]
- Zhou X.N., Chen J.X., Chen M.G., Bergquist R. The National Institute of Parasitic Diseases, Chinese Center for Disease Control and Prevention: a new administrative structure for schistosomiasis control. Acta Trop. 2005;96(2–3):296–302. doi: 10.1016/j.actatropica.2005.07.024. [DOI] [PubMed] [Google Scholar]
- Zhou X.N., Bergquist R., Tanner M. Elimination of tropical disease through surveillance and response. Infect. Dis. Poverty. 2013;2(1):1. doi: 10.1186/2049-9957-2-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou X.N., Qian M.B., Priotto G., Franco J.R., Guo J.G. Tackling imported tropical diseases in China. Emerg. Microbes Infect. 2018;7(1):12. doi: 10.1038/s41426-018-0022-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu R., Qin Z.Q., Feng T., Dang H., Zhang L.J., Xu J. Assessment of effect and quality control for parasitological tests in national schistosomiasis surveillance sites. Zhongguo Xue Xi Chong Bing Fang Zhi Za Zhi. 2013;25(1):11–15. [PubMed] [Google Scholar]
- Zhu H.H., Zhou C.H., Chen Y.D., Zang W., Xiao N., Zhou X.N. SWOT analysis of the national survey on current status of major human parasitic diseases in China. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi. 2015;33(5):377–381. [PubMed] [Google Scholar]