Patients with cancer are at high risk for serious illness and death from COVID-19. The pandemic has altered the routine for oncology patients. Their lives depend on their ability to receive medical care, but every visit to a health-care facility exposes them to the risk of contracting the virus; therefore, concerns about getting infected might interfere with their continuity of care. Does oncology treatment outweigh the risk of infection? The psychological pressure of uncertainty for patients with cancer is particularly high. In this difficult phase, these patients need guidance and support.
Professional guidance becomes of extreme importance for reducing the risk of contracting the virus, promoting patients' safety, treatment, and compliance, and ameliorating patients' stress. Several medical centres and national and international oncology societies are attempting to provide guidance to patients, but their extent and content vary; some national oncology societies have not provided any recommendations at all. We have developed an international scientific panel with the aim to review available guidelines from 63 oncology societies (appendix p 2) and provide summarised comprehensive recommendations for patients with cancer. 29 of 63 oncology societies provided some form of guidance for patients, either as their own recommendation statements or as a link to guidance from other societies (we only considered links to guidelines written in the society's native language). As most patients worldwide do not speak English, the language of guidance delivery is a major barrier to the dissemination of recommendations in different countries (figure ). Therefore, we have translated the summary of the comprehensive recommendations into 22 languages (Arabic, Bulgarian, Catalan, Chinese, Croatian, Czech, Dutch, English, French, German, Greek, Hungarian, Italian, Japanese, Norwegian, Polish, Portuguese, Romanian, Serbian, Slovenian, Spanish, and Swedish). The text and translations can be found at the European Cancer Patients Coalition and Hellenic Cancer Federation websites. We are working on a translation into Urdu. 48 physicians from 27 countries voluntarily participated in the working panel.
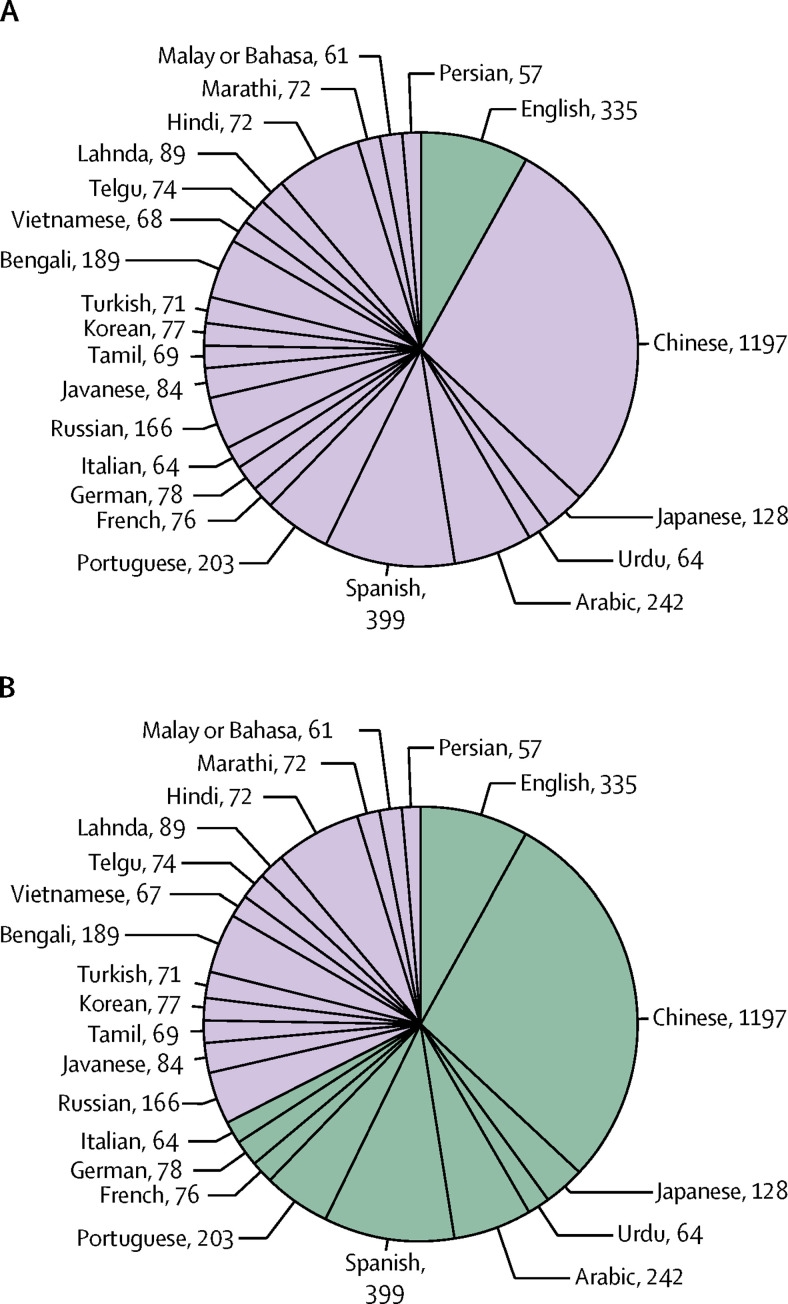
Figure.
Number of people (in millions) whose native language is in the top 23 most spoken worldwide
(A) Comparison of the number of English speakers (green) with speakers of the remaining 22 languages; the proportion of English speakers is 8%. (B) Number of people whose native language is covered by our multilanguage translation (green); the proportion of people able to access guidelines in their native language is 68%.
Our panel identified six main areas of recommendations. The English version of the guidance with references is presented in the appendix (pp 4–26). The first area concerns general considerations for patients with cancer during the COVID-19 pandemic (appendix p 4). Patients with cancer are at higher risk for infection, admission to the intensive care unit, and death. This high risk is related to the immunosuppression caused by a variety of factors, such as the disease itself, low performance status, cachexia, and the effect of treatments (surgery, chemotherapy, corticosteroids, radiotherapy, and bone marrow transplantation). The degree of immunosuppression depends on the type of cancer, the patient's age, fitness, comorbidities, the type of therapy, and the time since last therapy. Patients with haematological malignancies, especially those who received bone marrow transplants recently, are at particularly high risk. Patients with cancer are encouraged to ask their physicians about their individual risk. COVID-19 symptoms appear 2–14 days after exposure and include fever, cough, runny nose, sore throat, body aches, diarrhoea, and loss of smell or taste. Immediate medical attention should be sought for more severe symptoms, such as high fever, difficulty breathing, chest pain, confusion, and blue lips or face. Patients with cancer should have a low threshold for seeking medical attention if they have any new symptoms.
The second area of recommendation regards specific protocols or any special measure that people with cancer should take to avoid COVID-19 infection (appendix p 6). The best way to prevent infection is to avoid exposure to the virus by implementing strict hygienic and behavioural measures. Patients with cancer and household members should follow these measures more strictly given their high risk of infection. Cancer survivors might not be at such high risk but should contact their physician to find out more about their individual risk. Hygienic measures include frequent hand washing, disinfecting objects, avoiding handling objects in public places, and washing fruits and vegetables. Behavioural modifications include staying at home, not gathering in public places, and not touching other people. Travel, non-essential home visitors, the use of public transport, and the purchase of unpackaged food should be avoided. The use of a face mask is recommended, at least in crowded places, but not as a replacement for other established preventive measures. It should be worn when visiting a cancer centre or hospital.
The third area of recommendation reflects on what to do if someone is symptomatic, and indicates to patients whether there are any vaccines, treatment, or dietary or other supplementations that are effective against COVID-19 infection (appendix p 9). Patients with cancer should avoid people with a known exposure, infected asymptomatic people, and infected symptomatic people for at least 14 days and until their symptoms have resolved. If a patient with cancer experiences new cold-like symptoms, they should contact their oncologist and remain strictly quarantined. Currently, there are no vaccines or drugs that have been proven to treat or prevent COVID-19. There is no evidence that dietary interventions, complementary and alternative medicines, or supplements can treat or prevent COVID-19.
The fourth area of recommendation is related to mental health: guidance on managing anxiety and stress (appendix p 11). Patients with cancer are encouraged to live as healthily as they can. Some recommendations include breathing fresh air, engaging in physical exercise and creative activities, and having quality time with their families. Rest, sleep, and healthy eating are important. Patients' levels of stress and anxiety are generally high during a pandemic, especially because they are already dealing with cancer. Some suggestions to counteract these negative feelings include communication with friends and family, engaging in pleasant activities, meditation, yoga and physical exercise, eating healthily, avoiding excessive exposure to the news, and following good sleep hygiene. Patients who feel that they cannot cope with their stress should talk to their doctor.
Building trust between physicians and patients to enhance patients' confidence in medical staff decisions and improve their compliance with medical advice is important, and is the fifth area of recommendation (appendix p 13). The main goal of the medical team is to keep patients safe from COVID-19 while retaining the highest quality of care for their cancer. Patients should trust their physicians regarding deviations from their usual care. Treatment for infected or exposed patients might be deferred by 14 days or longer. For all patients with cancer, the possibilities of delaying or holding treatment are being evaluated on a case-by-case basis, according to the overall clinical picture, the aggressiveness of the cancer, and the potential health risks from COVID-19. During the acute phase of the pandemic, preventive care, elective procedures, some chemotherapy treatments, and supportive treatments are being postponed. Many visits are being converted to telephone or video visits. Cancer centres are altering the routines that patients are used to. It is important that patients remain confident that their oncology teams are there to support them. Patients need to be aware that a lot of misleading information circulates on the internet. The best sources of safe information online can be found on official websites provided by medical centres, oncology societies, and governments.
Finally, the sixth area of recommendation concerns the procedures at cancer centres (appendix p 16). Patients and visitors who have symptoms or have been exposed to an infected person should not visit their cancer centre, but should first call their doctor's office for further instruction. Symptomatic patients who arrive at the hospital should wear a face mask and report their symptoms upon arrival. All patients should keep a safe distance from other individuals. Not more than one visitor should accompany the patient. Patients and visitors must wash their hands upon entering and leaving the centre. At the hospital, patients with known or suspected COVID-19 are being kept in separate wards, and no visitors are allowed. For patients without COVID-19, only one visitor is allowed (or none in some places). Patients with cancer need to think about their goals of care in advance and discuss them with their loved ones and physicians. There is no evidence that COVID-19 is transmittable by blood. Blood donors are encouraged to continue donating unless they have new symptoms or a possible exposure to COVID-19.
Patients with cancer are facing unprecedented circumstances. We believe that a summary of recommendations from different oncology societies across the globe and their multilanguage translation will provide useful guidance to patients and caregivers.
Acknowledgments
We declare no competing interests. All authors cooperated in a voluntary form without any financial contribution. European Cancer Patients Coalition members cooperated actively during the project and used their website for the promotion of the multilanguage guidance summaries
Contributor Information
International Oncology Panel and European Cancer Patient Coalition collaborators:
Branka Petricevic, Nataliya Chilingirova, Iglika Mihaylova, Theodoros Tsakiridis, Carl Salembier, Konstantinos Papadimitriou, Ramon Andrade De Mello, Giovanna Araujo Amaral, Nathália Moisés Neves, Rodrigo Dias, Junlin Yi, Natalija Dedic Plavetic, Katarina Antunac, Panteleimon Kountourakis, Jindrich Kopecky, Christos Christopoulos, Ida Pavese, Stefanie Corradini, George Zarkavelis, Alexandra Papadaki, Areti Gkantaifi, Vasilios Theodorelos, Antonio Capizzello, Jozsef Lovey, Francesco Cellini, Mario Dambrosio, Dan Takeuchi, Haytham Hamed Saraireh, Ranveig Røtterud, Marzanna Chojnacka, Athanasios Papachristos, Igor Djan, Lazar Popovic, Cvetka Grašic Kuhar, Primož Strojan, Nadia Hindi, Antonis Valachis, Mari Åhs, Berardino De Bari, Olalla Santa Cruz, Hassan Hameed, Elena Takeuchi, Kathi Apostolidis, Antonella Cardone, Paulina Gono, and Panagiotis Filis
Supplementary Material
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.