Abstract
Objective:
To evaluate the differences between traditional Chinese medicine combined with western medicine and western medicine alone for the treatment of secondary tuberculosis and its impact on the evaluation of clinical efficacy and safety of patients in randomized controlled trials.
Methods:
A literature search of all major academic databases was conducted (PubMed, CNKI, Wanfang, VIP). Meta-analysis was conducted using RevMan 5.3 and Stata 12.0 software for those studies that satisfied the inclusion criteria. Ethical approval was not necessary because no people or animals were selected as subjects in this meta-analysis.
Results:
Twenty-three randomized controlled trials were included in this meta-analysis. The following indicators in the treatment group (traditional Chinese medicine decoction combined with western medicine chemotherapy) improved in comparison with those in the control group:focus absorption rate (RR:1.18; 95% CI: 1.15–1.22);sputum smear negative rate (RR: 1.17; 95% CI: 1.09–1.27);comprehensive clinical effective rate (RR: 1.18; 95% CI: 1.14–1.22);cavity closure rate (RR: 1.37; 95% CI: 1.12–1.67).
The difference of Immune function indicator likes CD4+ level (SMD: 0.76; 95% CI: −0.25 to 1.76) between the treatment group and the control group was not significant. In addition, safety evaluation indicators like the decrease rate of white blood cell (WBC) and platelets (PLT) and the elevation rate of alanine aminotransferase (ALT) and uric acid (UA) in the treatment group were reduced compared with those in the control group (P < .05).
Conclusions:
The curative effect of combining traditional Chinese and western medicine for the treatment of secondary tuberculosis is better than that of western medicine alone and is conducive to reducing the incidence of adverse reactions.
Keywords: Integrated traditional Chinese and western medicine, meta-analysis, secondary tuberculosis
1. Introduction
Currently, the incidence of tuberculosis in developed countries is generally well controlled, but it remains high in Asia and Africa, with India and China ranked first and second, respectively. The incidence in developed countries is ∼20/100,000, but 100 to 200/100,000 in Asian and African countries.[1] The reported numbers of tuberculosis cases in China have been at the top of category B infectious diseases over recent years, although the numbers have been decreasing significantly. It is estimated that there were 4.99 million active tuberculosis patients, 720,000 that were smear-positive and 1.29 million that were bacterium-positive in individuals over 15 years old in China.[2] Therefore, prevention and treatment of tuberculosis remains an urgent problem. Conventional treatment of pulmonary tuberculosis mostly relies on chemotherapy in which adverse reactions remain a significant challenge, including liver dysfunction, digestive system symptoms (nausea, belching, abdominal pain, abdominal distention, bowel ringing, etc) and circulatory system symptoms (pallor, vertigo, palpitation, fever, hypotension, etc).
Traditional Chinese medicine (TCM) is being increasingly recognized, with increasing numbers of clinical research studies of the application of Chinese medicine in the treatment of tuberculosis. However, due to differences in research methods, duration, location, and sample size, no scientific or objective research conclusions have been formed about its efficacy. Therefore, in the present study, a meta-analysis was performed based on randomized controlled trials (RCTs) of TCM integrated with western medicine for the treatment of secondary tuberculosis and compared the differences in efficacy and safety with western medicine chemotherapy alone. The aim is to provide more reliable evidence-based for the future clinical treatment of secondary tuberculosis using TCM combined with western medicine.
2. Research data and methods
2.1. Retrieval methods and strategies
A systematic search of the major electronic databases (PubMed, CNKI, Wanfang, VIP) was conducted using the keywords: “secondary tuberculosis” AND “integrated traditional Chinese and Western medicine treatment” AND “clinical efficacy.” Ethical approval was not necessary because no people or animals were selected as subjects in this meta-analysis.
2.2. Inclusion and exclusion criteria
2.2.1. Inclusion criteria
-
1.
Study design: RCTs;
-
2.
Patients: The patients in the original studies were diagnosed as secondary pulmonary tuberculosis according to the criteria through laboratory tests, symptoms and lung X-ray examination;
-
3.
Interventions: the treatment group comprised TCM decoction combined with western medicine while the control group was western medicine alone;
-
4.
Outcome measures: focus absorption, sputum negative conversion rate, clinical comprehensive efficacy, cavity closure, levels of CD4+T-cells, liver function, safety indicators.
2.2.2. Exclusion criteria
-
1.
Not a RCTs;
-
2.
Subjects were non-secondary pulmonary tuberculosis patients;
-
3.
Data were repeated in other publications;
-
4.
Randomized controlled trials were not conducted rigorously or the manuscript did not refer to the randomization methodology, repetitions or control;
-
5.
Studies with unclear definition of disease, incomplete data or therapeutic evaluation indicators;
-
6.
Review articles.
2.2.3. Quality evaluation
Retrieved articles were screened and the methodological quality evaluated using a Jadad score, including the following four aspects:
-
1.
Generation of random sequences;
-
2.
Concealment of randomization;
-
3.
Method for blinding;
-
4.
Withdrawal. The articles were then divided into low (scores of 1–3) or high (scores of 4–7) quality studies.
2.3. Data extraction
2.3.1. Basic information
The following information about each study was collected: authors, year of publication, number of cases in the treatment and control groups, intervention methods, diagnostic criteria, age of patients, and course of treatment.
2.3.2. Outcome measures
The primary Outcome measures included:
-
1.
Sputum smear negative rate;
-
2.
Comprehensive clinical effective rate was calculated by improvement rate – (Total score before treatment – Total score after treatment/Total score before treatment) × 100%, as defined in “the Guiding Principles for Clinical Research of New Drugs in Traditional Chinese Medicine”[3];
-
3.
The absorption rate of lung lesions as defined in the “Guidelines for the Implementation of the Chinese Tuberculosis Control Plan”[4];
-
4.
Closure rate of tuberculosis cavity as defined in the “Guidelines for the Implementation of the Chinese Tuberculosis Control Plan”[4];
The secondary outcome measures included:
-
1.
Immune function indicator likes CD4+ level;
-
2.
Safety evaluation indicators like the decrease rate of white blood cell (WBC) and platelets (PLT) and the elevation rate of alanine aminotransferase (ALT) and uric acid (UA).
2.3.3. Sensitivity analysis
Stata12.0 software was used to eliminate the indicators from articles sequentially for sensitivity analysis. No significant changes indicated reliable results.
2.4. Statistical analysis
For every indicator, a meta-analysis was performed using RevMan 5.3. Pooled estimates were obtained using random-effects models if the I2 statistic of heterogeneity was ≥50%, or using fixed effects model when I2 < 50%. We subjected the results to meta-analysis and evaluated the Standard Mean Differences (SMD) and relative risk (RR) in changes for outcome measure indicators from before to after treatment. Publication bias was analyzed with a funnel plot and Begg's test. P < .05 was considered statistically significant.
3. Results
A total of 602 articles were obtained from the literature search, of which 492 remained after duplicates were removed. Of these, 459 papers were excluded after reading the abstracts because they were reviews or were not RCTs. The full texts of the remaining 33 articles were obtained and after careful analysis, 10 were excluded because the quality of them was low. Finally, 23 articles were included in this review and meta-analysis. The screening process of this paper was shown in PRISMA Flow Diagram.
Of the studies included in the review, 20 were of low quality with only 3 that were of high quality, the highest having 6 points and an average of only 2.38. Among them, only two papers reported the blinding methodology, both of which were single-blind.[5,6] Basic information of all the included studies are displayed in Table 1. All the patients in western medicine groups were treated with the same chemotherapy regimen (H [isoniazid] + R [rifampicin] + Z [pyrazinamide] + E [ethambutol]), while the treatments in the combined Chinese and western medicine group was based on western medicine chemotherapy, supplemented with different Chinese medicine prescription. Traditional Chinese medicine treatment is based on the selection of different decoctions, granules, mixtures, etc according to the characteristics of different patients. More attention is paid to reducing the side effects of western medicine treatment, alleviating the patient's pain, and promoting the patient's physical recovery.
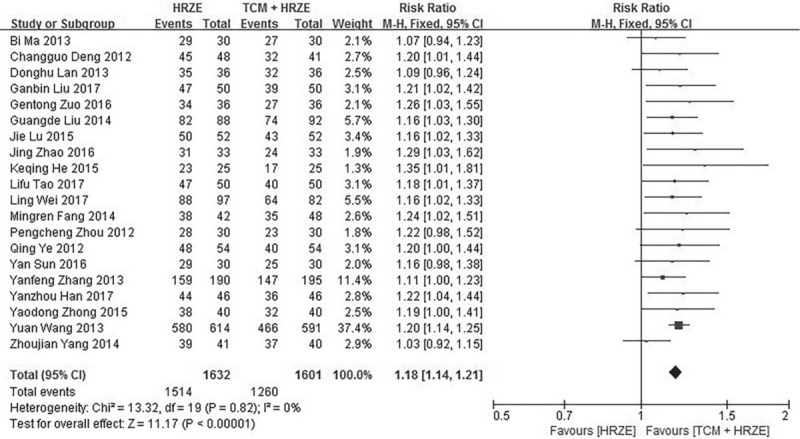
Table 1.
The basic information of included studies.
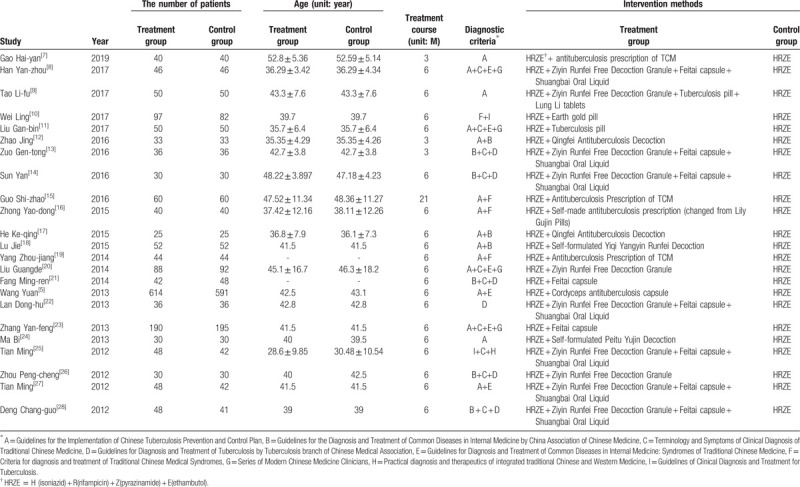
3.1. Absorption rate of lung lesions
A total of 16 articles[5,7,10–13,15–19,22,25–28] compared absorption rate of lung lesions after treatment. After a heterogeneity test (I2 = 20%, P > .05), fixed effects model was used for meta-analysis. The results, as displayed in Figure 1, indicate that the absorption rate of lesions in the treatment group was better than that in the control group (RR: 1.18; 95% CI: 1.15–1.22, P < .05).
Figure 1.
Forest plot of the absorption rate of lung lesions in the treatment and control groups.
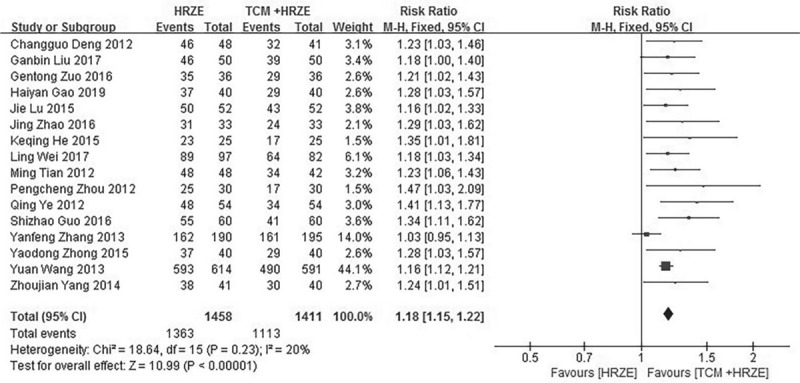
3.2. Sputum smear negative rate
Sixteen articles[5,8–10,12,14,17–20,22,23,25–28] compared sputum smear negative rate in both groups. After a heterogeneity test (I2 = 60%, P < .05), random effects model was used in the meta-analysis. The results, as displayed in Figure 2, indicate that the sputum negative conversion rate in the treatment group was 1.17-fold higher than that in the control group (RR: 1.17; 95% CI: 1.09–1.27, P < .05).
Figure 2.
Forest plot of the sputum negative conversion rate in the treatment and control groups.
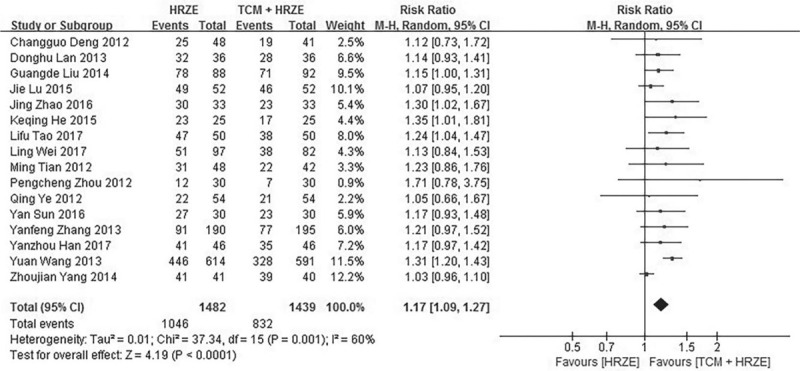
3.3. Comprehensive clinical effective rate
Twenty of the articles[5,8–14,16–24,26–28] reported comprehensive clinical efficacy in both groups. Fixed effects model was used for meta-analysis after testing for heterogeneity (I2 = 0%, P > .05). The meta-analysis indicate that the clinical efficacy of the treatment group was higher than that of the control group (RR: 1.18; 95% CI: 1.14–1.21, P < .05) (Fig. 3).
Figure 3.
Forest plot of the clinical efficacy in the treatment and control groups.
3.4. Closure rate of tuberculosis cavity
Four of the articles included in the review[10,13,27,28] studied the closure rate of tuberculosis cavities in patients of both groups. Fixed-effects model was used to conduct the meta-analysis of the four studies (heterogeneity test: I2 = 0%, P > .05). The results (Fig. 4) demonstrated that the closure rate of tuberculosis cavities in the treatment group was higher than that in the control group (RR: 1.37; 95% CI: 1.12–1.67, P < .05).
Figure 4.
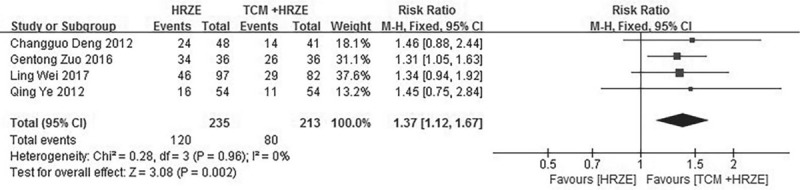
Forest plot of the closure rate of tuberculosis cavities in the treatment and control groups.
3.5. Improvement in immune function (CD4 + Level)
A total of 4 studies[13,15,22,28] compared the improvement of immune function (CD4+ levels) in both groups. A meta-analysis using random effects model (heterogeneity test: I2 = 97%, P < .05) was conducted, which suggested that the CD4+ level in the treatment group was little but not significant higher than that in the control group (Fig. 5) (SMD: 0.76; 95% CI: −0.25 to 1.76, P > .05).
Figure 5.
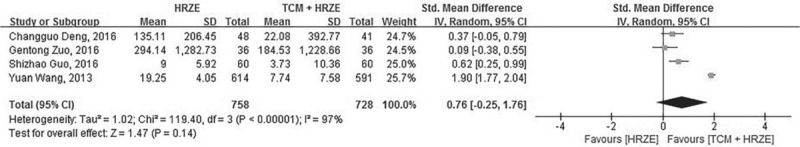
Forest plot of the CD4+ level in the treatment and control groups.
3.6. Safety evaluation indicators
3.6.1. Liver dysfunction
Six studies[5,11,16,19,20,27] reported liver damage during treatment. A meta-analysis was conducted adopting fixed-effects model (heterogeneity test: I2 = 0%, P > .05). The pooled estimate (RR, Fig. 6) for the abnormal rate of liver function in the treatment group compared to the control was 0.55 (95% CI: 0.42–0.72, P < .05).
Figure 6.
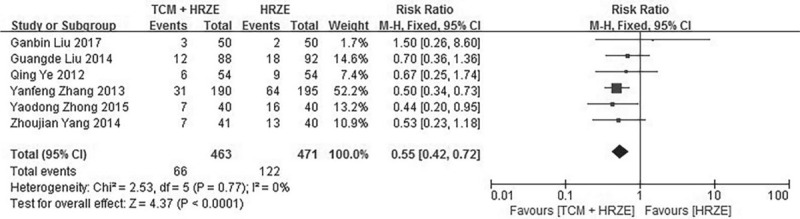
Forest plot of the abnormal rate of liver function in the treatment and control groups.
3.6.2. Decrease rate of white blood cells (WBCs)
Six manuscripts[10,11,13,20,26,27] reported changes of WBCs after treatment. A meta-analysis was performed on these 6 studies adopting fixed-effects model (heterogeneity test: I2 = 0%, P > .05). The pooled estimates (RR, Fig. 7) of the WBC decrease rate in the treatment group compared to the control group was 0.38 (95% CI: 0.25–0.59, P < .05).
Figure 7.
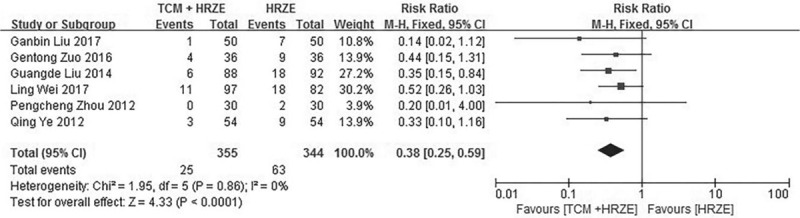
Forest plot of the WBC decrease rate in the treatment and control groups.
3.6.3. Decrease rate of PLT number
Two[10,13] of all the eligible articles reported PLT decrease rate in patients as a result of treatment. Fixed-effects model was used for meta-analysis (heterogeneity test: I2 = 0%, P > .05), the result of which (Fig. 8) indicated that the PLT decrease rate in the treatment group was significantly lower than that in the control group (RR: 0.48; 95% CI: 0.26–0.90, P < .05).
Figure 8.
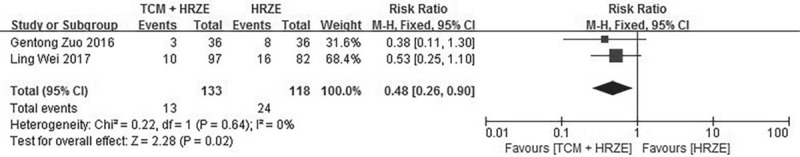
Forest plot of the PLT decrease rate in the treatment and control groups.
3.6.4. Elevation of ALT
From the eligible papers, three[10,13,26] reported elevation in ALT in patients as a result of treatment. A meta-analysis was conducted using fixed-effects model (heterogeneity test: I2 = 0%, P > .05) that demonstrated that the ALT elevation rate in the treatment group was lower than that in the control group (RR: 0.49; 95% CI: 0.28–0.85, P < .05, Fig. 9).
Figure 9.
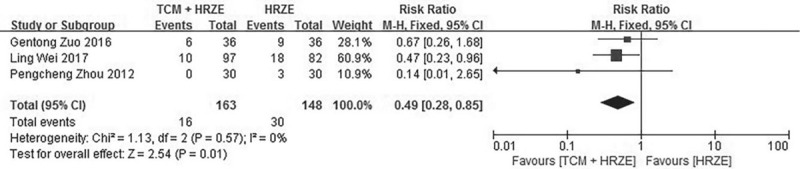
Forest plot of the ALT elevation rate in the treatment and control groups.
3.6.5. Elevation in UA
Six studies[10,13,20,25–27] reported that UA increased during treatment. Fixed effects model (heterogeneity test: I2 = 0%, P > .05) was used in the meta-analysis, the results of which indicated that the UA elevation rate in the treatment group was lower than that in the control group (RR: 0.78; 95% CI: 0.67–0.90, P < .05, Fig. 10).
Figure 10.
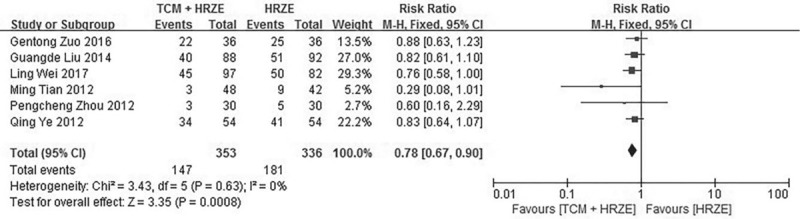
Forest plot of the UA elevation rate in the treatment and control groups.
3.6.6. Sensitivity analysis
The sensitivity analysis of the primary evaluation indicators (focus absorption rate, sputum negative rate, clinical comprehensive effective rate, cavity closure rate) showed that the pooled estimates were not affected as data from each manuscript was removed in sequence, indicating that the results of the meta-analysis were reliable and stable (Fig. 11).
Figure 11.
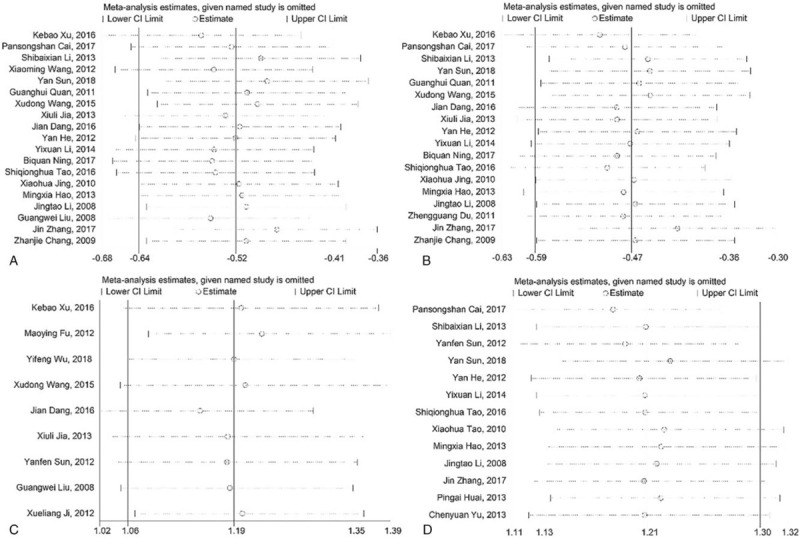
Sensitivity analysis chart (A) the absorption rate of lung lesions; (B) the sputum negative conversion rate; (C) the clinical efficacy; (D) the closure rate of tuberculosis cavities.).
3.6.7. Publication bias
Funnel plots of the meta-analyses were essentially symmetrical (Fig. 12). A Begg's test indicated that there was no strong evidence of publication bias in the meta-analysis.
Figure 12.
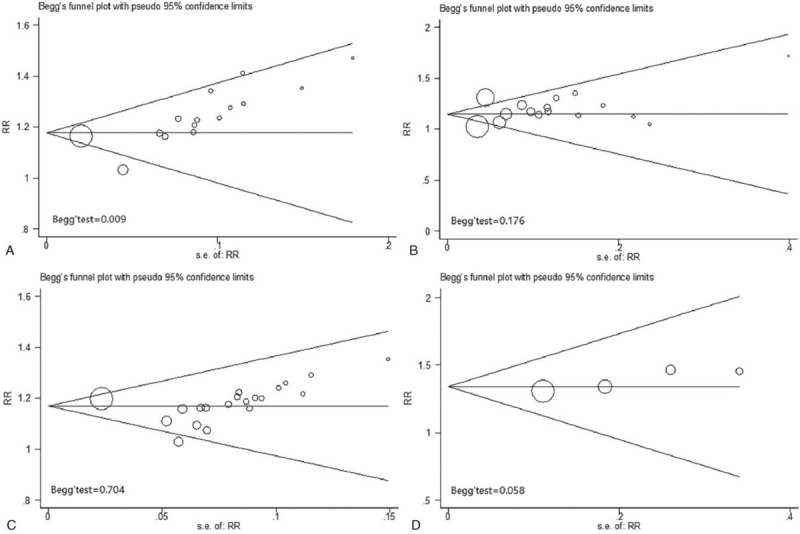
Funnel plots of publication bias. Notes: (A) the absorption rate of lung lesions, (B) the sputum negative conversion rate, (C) the clinical efficacy, and (D) the closure rate of tuberculosis cavities.
4. Discussion
Tuberculosis is a common notifiable class B infectious disease in China. Since the early 1990s, in order to control the emergence of new smear-positive tuberculosis infections more effectively, a new tuberculosis control strategy (DOTS, directly observed treatment + short course chemotherapy), as recommended by the WHO, has been gradually implemented nationwide. However, research shows that the mortality rate from tuberculosis is still high. According to this trend, tuberculosis will have a negative impact on global economic and social development and progress.[29] At present, most tuberculosis patients are given a single Western medicine chemotherapy, which has a long treatment cycle, high cost and is a painful process. It is frequently observed to cause liver dysfunction, digestive system symptoms (nausea, belching, abdominal pain, abdominal distention, borborygmus) and circulatory system symptoms (pallor, vertigo, palpitation, fever, hypotension).[30] Pulmonary tuberculosis belongs to the category of “Fei-Lao” (tuberculosis in Chinese) in TCM. It is caused by “Lao-Chong” (tubercle bacillus) and weakness of vital energy. The disease is classified as three types: deficiency of lung-yin, deficiency of both qi and yin and excessive fire due to deficiency of Yin.[31] The records of TCM research on the treatment of tuberculosis can be traced back hundreds of years, and the disease is becoming better understood. Similar symptoms (“xu-lao”, “xu-sun”) to those typical of tuberculosis were described in the medical book Internal Classic, Difficult Classic and Synopsis of the Golden Chamber. The core of TCM Decoction in treating tuberculosis lies in the use of an antimicrobial, replenishing Qi and blood, “Gu-Ben-Pei-Yuan,” relieving coughing and expectorating phlegm.
The meta-analysis of 23 RCTs of TCM integrated with Western medicine for the treatment of secondary tuberculosis demonstrated an improvement in each parameter (focus absorption rate, sputum negative conversion rate, clinical comprehensive effect and cavity closure rate) in the treatment group in comparison with that in the control group (all P < .05). This demonstrates that the therapeutic effect of TCM combined with western medicine is better than just western medicine alone.
The treatment of tuberculosis is also related to human immune function. Tuberculosis is mostly caused by infection with mycobacterium tuberculosis. It is difficult to eliminate the pathogenic bacteria, which requires T-lymphocyte mediated cellular immunity. This meta-analysis indicated that the CD4+ levels in the treatment group was higher than that of the control group (SMD: 0.76; 95% CI: 0.25–1.76, P = .14). However, only 4 studies were included in this study that reported change in immune function. A greater number of reliable RCTs with large cohorts are required to support this theory.
The meta-analysis demonstrated that the incidence of adverse events (abnormal liver function, decreased WBCs, decreased PLT and increased ALT and UA) in the treatment group was lower than in the control group (P < .05), indicating that the safety of TCM integrated with Western medicine for the treatment of secondary pulmonary tuberculosis was better than western medicine alone.
In addition, we conducted a sensitivity analysis on the main outcome indicators of the 23 studies, finding that there was low sensitivity which indicated that the results of the meta-analysis were stable and reliable. The funnel diagram is approximately symmetrical, with Begg's test demonstrating that there was no clear publication bias in this study. Thus, a high level of confidence can be placed on the reliability of the meta-analysis results.
There are some limitations in this study. The majority of the 23 RCT manuscripts included in the review had low Jadad scores, which may be due to:
-
1.
A lack of stated blinding methodology;
-
2.
The dialectical thinking of TCM treatments leading to the prescribing of different prescriptions, proportions of drugs, treatment cycles, etc, which cannot form a unified or standardized TCM treatment program;
-
3.
The research designs are not sufficiently rigorous, and the methodology requires further improvement;
-
4.
The diagnostic criteria for secondary pulmonary tuberculosis in the included studies are not entirely uniform.
Therefore, a greater number of high-quality and large-sample RCTs are required in order to more systematically evaluate the efficacy and safety of TCM combined with western medicine for the treatment of secondary tuberculosis and comprehensively provides a reliable evidence-based for its clinical application. Furthermore, the ideal study design would be, Western plus Chinese medicine versus Western medicine plus placebo. However, in our present study, the majority of the original researches about our topic were all comparing the effects of the two treatment schemes: western medicine treatment alone and western medicine plus TCM treatment. Western medicine plus placebo was rarely used in clinical practice. In our future studies, we will continue to pay close attention to Western medicine plus placebo for secondary pulmonary tuberculosis.
5. Conclusions
According to the dialectical thinking of TCM, the theory of “deficiency makes up for its origin, insecticide kills its root,” the Western medicine kills the bugs and removes the pathogens, while the TCM effects restoration.[20] Traditional Chinese medicine decoction combined with Western medicine chemotherapy can more effectively improve the clinical symptoms, improve the cure rate and reduce the adverse effects associated with Western medicine chemotherapy.
Author contributions
R. Z. planned the study.
R. Z. submitted the study.
R. Z., XW. L., XH. L., B. Z., Q. L. N. S., and C. S. performed the data analysis, wrote and modified the manuscript.
Footnotes
Abbreviations: ALT = alanine aminotransferase, CD4+ = cluster of differentiation T -cells, DOTS = directly observed treatment + short course chemotherapy, PLT = platelets, RCTs = randomized controlled trials, RR = relative risk, SMD = standard mean differences, TCM = traditional Chinese medicine, UA = uric acid, WBC = white blood cell.
How to cite this article: Li X, Li X, Liu Q, Sun N, Zhang B, Shi C, Zhang R. Traditional Chinese medicine combined with Western medicine for the treatment of secondary pulmonary tuberculosis: A PRISMA-compliant meta-analysis. Medicine. 2020;99:16(e19567).
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
The present study was funded by Subject Innovation Team of Shaanxi University of Chinese Medicine (132041933).
The authors have no conflicts of interest to disclose.
References
- [1].Xin XM, Wu YJ, Zhang HT, et al. Epidemiological characteristics and analysis of newly diagnosed tuberculosis patients. Chin J Public Health 2012;28:124. [Google Scholar]
- [2].Wang LX. Current situation of tuberculosis control in China. Public Health China Chin J Public Health 2012;28:413–4. [Google Scholar]
- [3].Zheng XY. Guiding Principles for Clinical Research of New Chinese Medicine [M]. Beijing: China Medical Science and Technology Press; 2002. [Google Scholar]
- [4].Xiao DL, Zhao MG, Wang Y. Guidelines for the Implementation of China's Tuberculosis Control Program (2008) [M]. 2009;Beijing: Press of China Union Medical University, 27-28. [Google Scholar]
- [5].Zhang YF, Liu Y, Zhang H, et al. Effect of integrative medicine on 385 cases of Yinxuhuowang Syndrome with initially treated pulmonary tuberculosis. Chin Med Emerg 2013;22:1466–8. [Google Scholar]
- [6].Liu SS, Sun LM, Wang SS, et al. Therapeutic effect and safety of integrated therapy of Chinese medicine and chemical drugs on initial treatment of pulmonary tuberculosis. Chin J Informat Tradit Chin Med 2013;20:6–9. [Google Scholar]
- [7].Gao HY. Observation on the efficacy and value of integrated traditional Chinese and western medicine in the treatment of secondary tuberculosis. Cardiovasc Dis Electr J Integr Tradit Chin Western Med 2019;7:176–7. [Google Scholar]
- [8].Han YZ, Liu F. Clinical efficacy of integrated traditional Chinese and western medicine in the treatment of newly treated secondary pulmonary tuberculosis. Health All 2017;11:135–6. [Google Scholar]
- [9].Tao LF. Syndromes and clinical treatment of newly treated secondary tuberculosis. Nei Mongol J Tradit Chin Med 2017;36:62. [Google Scholar]
- [10].Wei L, Zhou SH, Liu ZM. Clinical study on Tujin Pill combined with antituberculosis drugs for secondary tuberculosis. Med Inform 2017;30:173–4. [Google Scholar]
- [11].Liu LB, Yi LL, Yang P. Clinical effect of tuberculosis pills combined with anti-tuberculosis drugs on secondary tuberculosis. Henan Med Res 2017;26:1268–9. [Google Scholar]
- [12].Zhao J. Study on the effect of integrated Chinese and western medicine in the treatment of primary secondary pulmonary tuberculosis. Cardiovasc Dis Electr J Integr Tradit Chin Western Med 2015;3:139–41. [Google Scholar]
- [13].Zuo GT. Observation on the clinical effect of integrated traditional Chinese and western medicine in the treatment of secondary tuberculosis. Chin Primary Health Care 2016;30:78–9. [Google Scholar]
- [14].Zuo GT, Sun Y. Observation of clinical efficacy of integrated traditional Chinese and western medicine in the treatment of primary secondary pulmonary tuberculosis. Guide China Med 2016;14:177. [Google Scholar]
- [15].Guo SZ, Zhang Q, Zhang MY. Observation on the curative effect of anti-tuberculosis prescription combined with chemotherapy in the treatment of primary secondary tuberculosis of Yin deficiency and fire prosperity type. Mod J Integr Tradit Chin Western Med 2016;25:3249–51. [Google Scholar]
- [16].Zhong YD. Clinical observation on 40 cases of secondary tuberculosis of Yin deficiency and fire exuberance type treated by combination of traditional Chinese and western medicine. Chin J Ethnomed Ethnopharm 2015;24:70–1. [Google Scholar]
- [17].He KQ, Ren HF, Zong YL. Qingfei Kanglao decoction combined with chemotherapy in the treatment of secondary pulmonary tuberculosis for 25 cases. Chin Med Mod Distance Educ China 2015;13:70–1. [Google Scholar]
- [18].Lu J, Feng XY, Sun WM, et al. Clinical observation on the treatment of secondary pulmonary tuberculosis with supplementing qi and nourishing yin. China Trop Med 2015;15:1263–5. [Google Scholar]
- [19].Yang ZJ, Wu GQ, Chen C, et al. Combination of “Kanglao Formula” and western medicine for the initial treatment of secondary tuberculosis of lung (hyperactivity of fire due to yin deficiency pattern): a clinical assessment of 41 cases. Shanghai J Tradit Chin Med 2014;48:56–9. [Google Scholar]
- [20].Liu GD, Hu Y, Song SY, et al. Treatment of secondary tuberculosis with integrated traditional Chinese and western medicine. J Hebei Med Univ 2014;35:1310–2. [Google Scholar]
- [21].Fang MR. Observation of clinical efficacy of integrated traditional Chinese and western medicine in the treatment of primary secondary pulmonary tuberculosis. Med Inform 2014. 307–8. [Google Scholar]
- [22].Wang Y, Dai EL, Jia Z. A retrospective analysis of cordyceps anti-tuberculosis capsule combined with chemotherapy for 614 cases of secondary tuberculosis. J Tradit Chin Med 2013;54:1304–7. [Google Scholar]
- [23].Lan DH. Observation of curative effect of 36 cases of primary secondary pulmonary tuberculosis treated by integrated traditional Chinese and Western medicine. Contemp Med 2013;19:153–4. [Google Scholar]
- [24].Ma L, Ma YC, Wang ZH. Observation on the efficacy of integrated traditional Chinese and western medicine in the treatment of secondary tuberculosis. Shanxi J Tradit Chin Med 2013;29:19–23. [Google Scholar]
- [25].Tian M, Wang Y, Ye Q, et al. Randomized controlled clinical trial of secondary pulmonary tuberculosis treatment with integrated traditional Chinese and western medicine. Int J Tuberculosis Lung Dis (Chin Ed) 2012;1:97–100. [Google Scholar]
- [26].Zhou PC, Zhao BJ, Yu W, et al. 30 cases of secondary tuberculosis treated with integrated Chinese and western medicine. World J Integr Tradit Western Med 2012;07:52–4. [Google Scholar]
- [27].Tian M, Ye Q, Huang XQ, et al. Randomized study for combining traditional Chinese and western medicine treatment of pulmonary tuberculosis. Chin Arch Tradit Chin Med 2012;30:2394–6. [Google Scholar]
- [28].Deng CG, Tian M, Li X, et al. The clinical observation on the curative effect of initial treatment secondary pulmonary tuberculosis treated with integrated. Chin Western Med 2012;33:1321–5. [Google Scholar]
- [29].Cao YH. Analysis of current situation and epidemic trend of tuberculosis. Chin J Trauma Disability Med 2014;22:296–7. [Google Scholar]
- [30].Wang LX, Cheng SM, Chen MT, et al. The fifth national tuberculosis epidemiological survey in 2010. Chin J Antituberculosis 2012;34:485–508. [Google Scholar]
- [31].Jin X, Xie HB, Zeng H, et al. Combined traditional Chinese and western medicine treatment for multidrug-resistant pulmonary tuberculosis: a meta-analysis of randomized controlled trials. Guiding J Tradit Chin Med Pharm 2018;24:84–8. [Google Scholar]


