Abstract
Background:
The findings on the association between elevated plasma homocysteine levels and the risk of the trial of org 10172 in acute stroke treatment (TOAST) of ischemic stroke have been inconsistent in Chinese. So far, there is no meta-analysis about the association between Hcy and the TOAST subtypes of ischemic stroke in Chinese. This study; therefore, aimed to evaluate whether elevated homocysteine levels are associated with the TOAST subtypes of ischemic stroke using a meta-analysis.
Materials and methods:
A systematic search of electronic databases were conducted for studies reporting homocysteine levels in ischemic stroke and the TOAST of ischemic stroke to April 18, 2018. The data were extracted after the application of inclusion and exclusion criteria. All the data were analyzed using Stata software version 9.0 (Stata Corp LP, College Station, TX). The standardized mean difference (SMD) and 95% confidence interval (CI) were used to compare continuous variables.
Results:
Thirteen studies comprising 3114 participants (2243 patients and 871controls) met the eligibility criteria and were included in the meta-analysis. The meta-analysis revealed that the ischemic stroke group had significantly higher levels of homocysteine than controls (SMD = 1.15, 95% CI = 0.85–1.45, P < .05). The subgroup analyses suggested that the groups of patients with large-artery atherosclerosis, small-vessel occlusion, cardioembolism, stroke of other determined etiology and stroke of undetermined etiology had significantly higher levels of homocysteine compared to those in the control group (large-artery atherosclerosis: SMD = 2.12, 95% CI = 1.40–2.84, P < .05; small-vessel occlusion: SMD = 1.10, 95% CI = 0.72–1.48, P < .05; CE: SMD = 1.17, 95% CI = 0.64–1.71, P < .05; stroke of other determined etiology: SMD = 0.88, 95% CI = 0.53–1.24, P < .05; stroke of undetermined etiology: SMD = 1.50, 95% CI = 0.66–2.33, P < .05, respectively).
Conclusion:
This meta-analysis found that ischemic stroke patients and the TOAST of ischemic stroke patients in Chinese had significantly higher homocysteine levels than the controls, suggesting that serum homocysteine levels may be a risk factor for ischemic stroke and the TOAST subtypes of ischemic stroke in Chinese.
Keywords: homocysteine, ischemic stroke, meta-analysis, TOAST
1. Introduction
A stroke is defined as “a clinical syndrome consisting of rapidly developing clinical signs of focal (or global in the case of coma) disturbance of cerebral function lasting more than 24 hours or leading to death with no apparent cause other than a vascular origin.[1]” Ischemic stroke, also known as cerebral infarction, which accounts for 85% of all strokes,[2] is one of the most common cerebrovascular diseases. It is characterized by a high incidence, morbidity, and mortality and endanger the health and lives of patients. It is the major cause of disability and the second leading cause of death in the world.[3] According to the trial of org 10172 in acute stroke treatment (TOAST) criteria,[4] ischemic stroke can be divided into large-artery atherosclerosis (LAA), small-vessel occlusion (SAO), cardioembolism (CE), stroke of other determined etiology (SOE), and stroke of undetermined etiology (SUE). In addition to the traditional risk factors such as hypertension, diabetes, and smoking, studies have found that homocysteine (Hcy) is an independent risk factor for cardiovascular and cerebrovascular diseases.
Hcy, a sulfhydryl-containing amino acid, is an important intermediate product of methionine and cysteine metabolism. Its serum level can increase in specific conditions such as congenital enzyme defects, chronic renal and liver dysfunction, and treatment with several drugs. High Hcy levels caused by metabolic disorders of Hcy are an independent risk factor for hypertension,[5] myocardial infarction,[6–8] peripheral arterial occlusive disease,[9,10] venous thrombosis,[11,12] hemorrhagic strokes,[13,14] and ischemic stroke.[15–19] In recent years, researchers have placed increasing emphasis on high Hcy levels, and a number of case-control studies have been conducted to explore the correlation between Hcy and ischemic stroke.[20] Nevertheless, the results have been inconsistent. Stroke has become the first leading cause of death in Chinese, and the most common type is the ischemic stroke.[21] But only a few research papers have explored the relationship between Hcy and the TOAST subtypes of ischemic stroke in Chinese. What's more, the correlations between Hcy and the TOAST subtypes of ischemic stroke are thus still unclear in Chinese. So far, there is no meta-analysis about the association between Hcy and the TOAST subtypes of ischemic stroke in Chinese. The published studies on Hcy and ischemic stroke have also had only modest sample sizes, which has limited their significance. By performing a meta-analysis, the prevailing method for the quantitative summary of different results, the data can be assessed using a reasonable sample size. The purpose of the present meta-analysis was to quantitatively assess the findings from prospective studies on plasma Hcy levels and the risk of ischemic stroke and its TOAST subtypes.
2. Methods
This protocol is conducted according to the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols statement.[22] Ethical approval was unnecessary in this study because this paper was a statistical analysis based on the previous articles.
2.1. Publication search
A comprehension search was conducted on the PubMed, EMBASE, and Chinese biomedicine databases for articles up to April 18, 2018. The following keywords were used: “stroke” OR “ischemic stroke” OR “cerebral ischemia,” “brain ischemia,” and “plasma homocysteine” OR “homocysteine” OR “Hcy” OR “plasma Hcy.” Case-control studies that included the subtype of TOAST in ischemic stroke were chosen. Of the studies with overlapping data published by the same author, only the most recent or complete study was included in this meta-analysis.
2.2. Inclusion and exclusion criteria
The following criteria were used to identify eligible studies that had investigated the association between plasma Hcy levels and ischemic stroke:
-
(1)
case-control studies written in English and Chinese;
-
(2)
studies that assessed the correlation between Hcy and patients with ischemic stroke;
-
(3)
studies that included ischemic stroke patients and healthy controls;
-
(4)
studies that provided information on the plasma Hcy levels in the case and control groups at the onset of ischemic stroke; and
-
(5)
studies that used the TOAST classification standard.
The exclusion criteria were as follows:
-
(1)
not using TOAST classification standard;
-
(2)
publications with duplications or studies with overlapping data from the same author;
-
(3)
abstracts, case reports, proceedings, letters, reviews, and meta-analyses;
-
(4)
incomplete outcome data; and
-
(5)
a score of 6 points on the Newcastle–Ottawa scale (NOS).
2.3. Data extraction and quality assessment
Two reviewers independently extracted the following data from each included study using a standard form: first author's name, year of publication, country of origin, ethnicity, Hcy levels (mean ± standard), and the TOAST subtypes. A quality assessment was conducted according to the NOS criteria for retrospective studies.[23]
2.4. Statistical analysis
All the meta-analyses were performed using Stata version 9.0 (Stata Corp LP, College Station, TX). The standardized mean difference (SMD) with a 95% confidence interval (CI) was used for the continuous variables. Heterogeneity among the studies was measured via I2 tests, and studies with an I2 higher than 50% were considered to have high heterogeneity. A fixed effects model was used when there was no significant heterogeneity among the studies; otherwise, a random effects model was used. To identify possible sources of heterogeneity within the included studies, subgroup analyses were performed based on the TOAST subtypes. Funnel plots were used to evaluate potential systematic bias in the studies. Two-sided P-values < .05 were considered statistically significant.
3. Results
3.1. Study characteristic
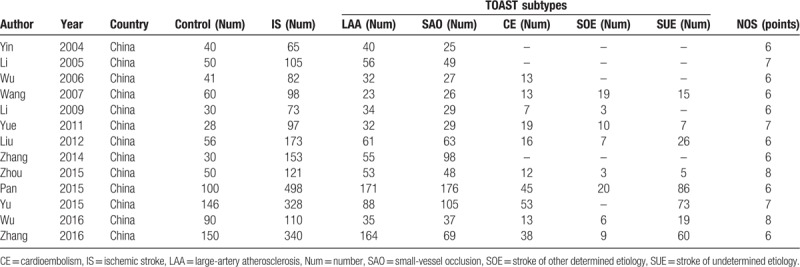
After screening the abstracts, 229 possible studies were identified considered, and 20 studies in Chinese people were considered eligible after a detailed review. Notwithstanding 7 for scoring <6 points using the NOS criteria (Fig. 1). This process resulted in selection of 13 studies[24–36] involving 3114 participants (2243 patients and 871 controls) for the meta-analysis. Of the included studies, 12 reported on ischemic stroke,[24–32,34–36] 13 on the LAA subtype,[24–36] 13 on the SAO subtype,[24–36] 9 on the CE subtype,[26,27,29,30,32–36] 8 on the SOE subtype,[27,29,30,32–36] and 8 on the SUE subtype[27,29,30,32–36] (Table 1). The studies included in the meta-analysis were generally of high quality.
Figure 1.
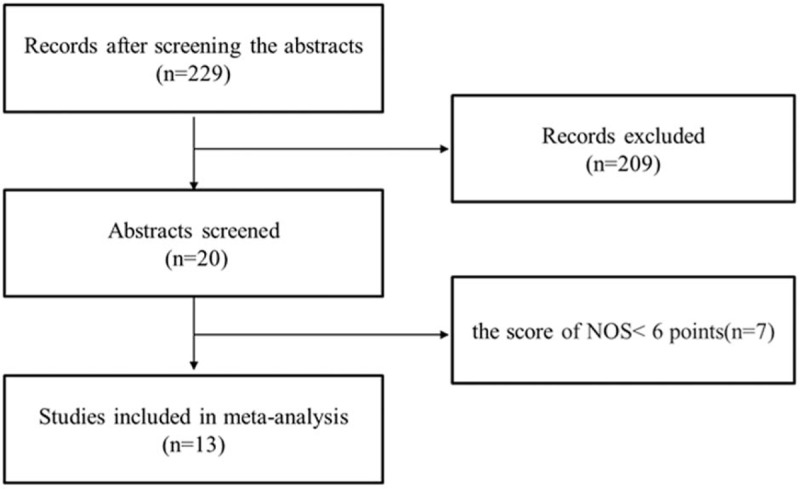
Study selection flow.
Table 1.
Study characteristics.
3.2. Association between Hcy and the TOAST of ischemic stroke
There was heterogeneity among the studies reporting differences of plasma Hcy levels between ischemic stroke, LAA and the healthy controls (I2 = 89.9%, I2 = 97.2%). The ischemic stroke and the TOAST subtypes in the 13 included studies showed obvious heterogeneity. Thus, a random effects model was used to pool the data. An incorporate analysis showed that the ischemic stroke patients had significantly higher levels of Hcy compared to the controls (SMD = 1.15, 95% CI = 0.85–1.45, P < .05) (Fig. 2). In the subgroup analysis, in which the participants were stratified by the TOAST subtypes of ischemic stroke, the TOAST subtypes had significantly higher levels of Hcy compared to the controls (LAA: SMD = 2.12, 95% CI = 1.40–2.84, P < .05; SAO: SMD = 1.10, 95% CI = 0.72–1.48, P < .05; CE: SMD = 1.17, 95% CI = 0.64–1.71, P < .05; SOE: SMD = 0.88, 95% CI = 0.53–1.24, P < .05; SUE: SMD = 1.50, 95% CI = 0.66–2.33, P < .05) (Fig. 3). The LAA patients had higher serum Hcy levels compared to the SAA, CE, SOE, SUE patients (SMD = 1.03, 95% CI = 0.45–1.61, P < .05; SMD = 1.54, 95% CI = 0.60–2.48, P < .05; SMD = 1.18, 95% CI = 0.56–1.79, P < .05; SMD = 1.42, 95% CI = 0.47–2.37, P < .05, respectively) (Fig. 4). While the SAO patients had higher serum Hcy levels compared to the SUE (SMD = -0.05, 95% CI = −0.52–0.43, P < .05). There were no significant differences between SAO and CE, SOE patients (SMD = 0.27, 95% CI = 0.03–0.50, P > .05; SMD = 0.44, 95% CI = 0.08–0.81, P > .05). The CE patients had higher serum Hcy levels compared to the SUE (SMD = −0.32, 95% CI = −0.81–0.16, P < .05), and there were no statistical differences between the CE and SOE patients plasma Hcy levels (SMD = 0.28, 95% CI = −0.01–0.57, P > .05). Additionally, there were no statistically significantly differences between the SOE and SUE patients (SMD = −0.35, 95% CI = −0.64 to −0.07, P > .05).
Figure 2.
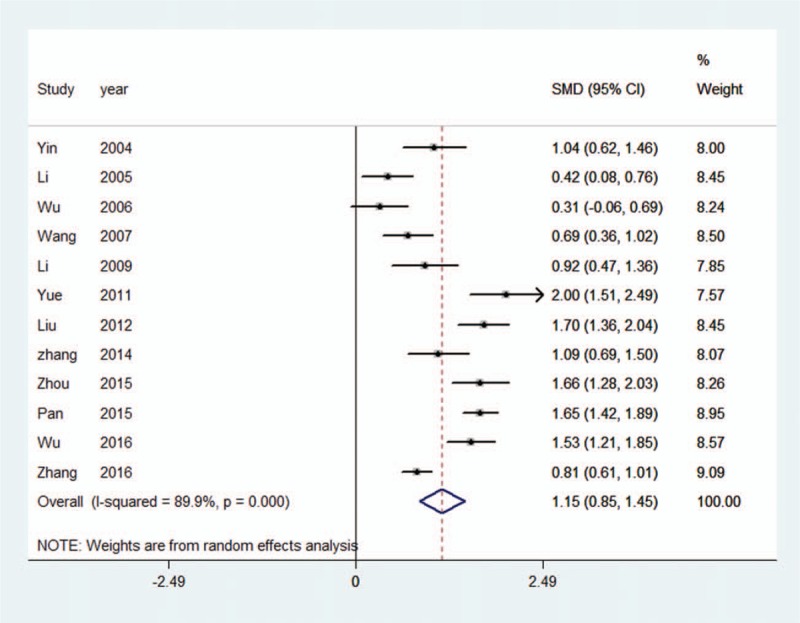
Meta-analysis of 12 studies reporting on homocysteine levels in patients with ischemic stroke compared to the controls.
Figure 3.
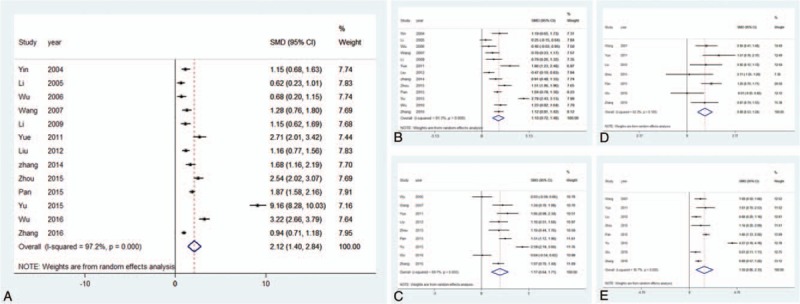
The TOAST of ischemic stroke, A (LAA vs Con), B (SAO vs Con), C (CE vs Con), D (SOE vs Con), E (SUE vs Con). CE = cardioembolism, CI = confidence interval, Con = control, LAA = large-artery atherosclerosis, SAO = small-vessel occlusion, SOE = stroke of other determined etiology, SUE = stroke of undetermined etiology, TOAST = the trial of org 10172 in acute stroke treatment.
Figure 4.
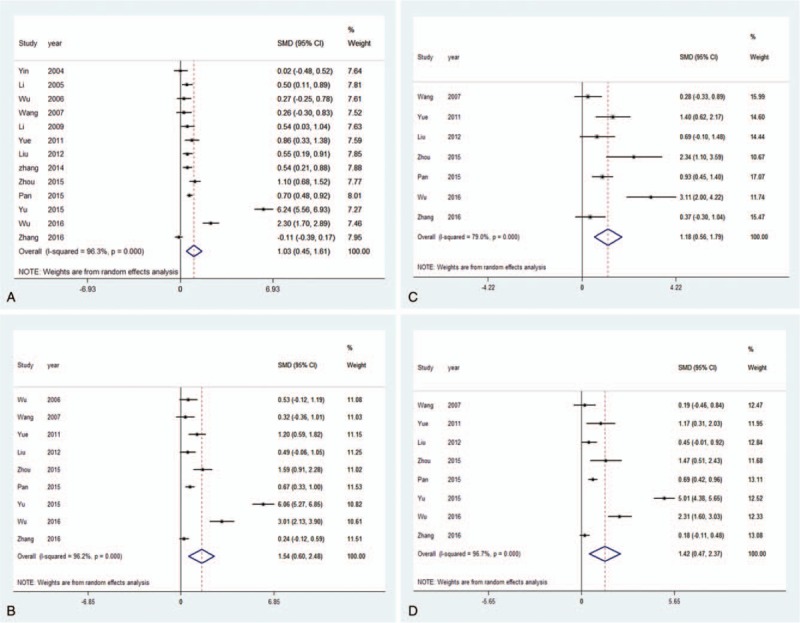
Meta-analysis on homocysteine levels in patients with large-artery atherosclerosis stroke compared to the other TOAST subtypes. A (LAA vs SAO), B (LAA vs CE), C (LAA vs SOE), D (LAA vs SUE). CE = cardioembolism, LAA = large-artery atherosclerosis, SAO = small-vessel occlusion, SOE = stroke of other determined etiology, SUE = stroke of undetermined etiology, TOAST = the trial of org 10172 in acute stroke treatment.
3.3. Regression analysis
A regression analysis was conducted based on the ischemic stroke and the TOAST subtypes. We conducted a regression analysis on the data through “year.” We concluded that heterogeneity accounted for 87.65% of residual variation, and “year” could explain 33.41% of the studies’ variations for the ischemic stroke patients.
3.4. Publication bias
The funnel plot and Egger tests were performed to quantitatively evaluate the publication bias of the literature on ischemic stroke. The results of the Egger test provided statistical evidence for funnel plot symmetry (P = .123) in the overall results, suggesting the absence of publication bias. No significant publication bias was detected using funnel plot tests in the subgroup analyses for differences between the Hcy levels of ischemic stroke and the TOAST subtypes patients and the controls (Fig. 5).
Figure 5.
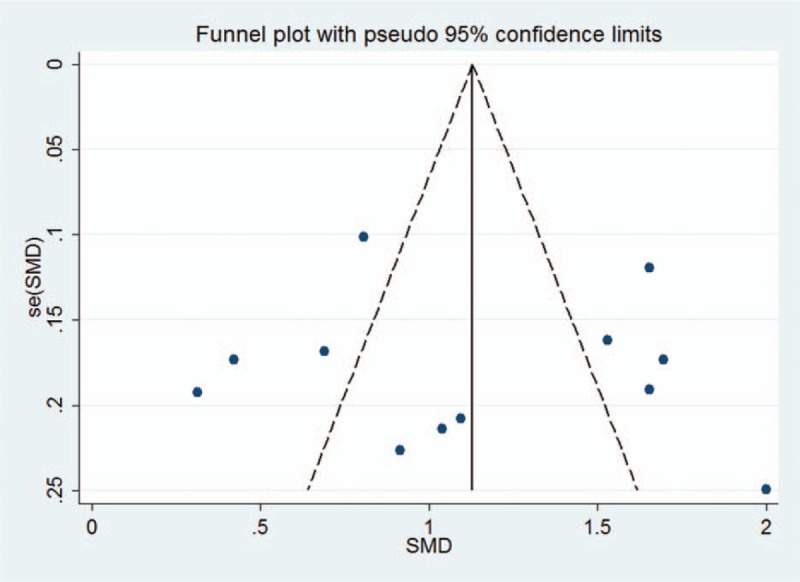
Funnel plot to detect risk of publication bias in the meta-analysis.
4. Discussion
Ischemic stroke, an important clinical problem, has been well studied but the mechanism of ischemic stroke is still relatively unclear. Hcy is not only a risk factor for, but also correlated with, stroke severity, worse prognosis,[18,37–39] and stroke recurrence.[40–42] Furthermore, some studies have found that patients who have high Hcy levels are roughly twice as likely to have a stroke as normal people.[17,40]
Although increasing evidence has demonstrated that elevated Hcy levels may be an important contributor in the development of ischemic stroke, a handful of studies have suggested the different view.[13,43] At present, there are few research papers about the relationship between Hcy and the TOAST subtypes of ischemic stroke in the Chinese. The correlations between Hcy and the TOAST subtypes of ischemic stroke in Chinese are thus still unclear. In China, studies have shown that Hcy is correlated with ischemic stroke closely especially in the subtype of SAO and LAA.[24,35,36] Some studies have indicated that Hcy is only related to LAA.[32–34,44] But research on the relationship between Hcy and CE, SOE, SUE is rare, and to date, only 2 studies showed that Hcy is related to the all the subtypes of TOAST,[35,36] 1 study showed that Hcy has not related with SOE.[34] In this study, we extracted data on Hcy levels from 13 studies and found that the Hcy levels in the Chinese patients with ischemic stroke and the TOAST subtypes were significantly higher than in the healthy controls, suggesting that Hcy levels could be an aggravating factor in atherosclerosis, and high Hcy levels might be one of the risk factors for ischemic stroke. The precise mechanism of Hcy on the susceptibility of ischemic stroke remains unresolved. Most of the studies on high Hcy levels as a cause of ischemic stroke have found that Hcy damages endothelial cells, increase vascular smooth muscle, the inflammatory process, oxidative insult, and enhances the production of fibrinogen leading to abnormal coagulation together with platelet dysfunction.[1,45–49]
We also found Hcy significantly higher in LAA patients than the other TOAST subtypes patients in Chinese. Indeed, Hcy is more likely higher in patients with the LAA subtype of ischemic stroke. It can be speculated that the increased plasma Hcy may promote atherosclerosis of the great vessels, and atherosclerosis plays a key role in the occurrence of LAA. The increased production of reactive oxygen species caused by Hcy may directly injury endothelial cells especially hydrogen peroxide[50–52] and decline nitric oxide bioavailability which is concomitant with diminishing of nitric oxide including vasoconstriction, smooth muscle proliferation, increase platelet activation and leucocyte recruitment.[52,53] In addition, Hcy enhances the release of arachidonic acid from platelets to generate reactive oxygen species, leading to calcium and lipid deposits in the endothelial wall. Together, these changes degrade arterial elasticity and accelerate the process of atherosclerosis.[12,54–58] In our study, Hcy in SAO patients were higher than SOE patients, and the CE patients were higher than SUE patients in Chinese.
There was no meta-analysis about Hcy and ischemic stroke subtypes in non-Chinese people. Studies which have evaluated the relationship between Hcy levels and stroke subtypes have shown different results in non-Chinese people. Eikelboom et al[59] reported that Hcy was associated with a higher risk of LAA and SAO compared with controls. Ashjazadeh et al[60]conducted a study in 171 Iranian patients with acute ischemic stroke and concluded that Hcy has a strong association with cardioembolic subtype. A South London study in 457 stroke patients reported Hcy was significantly greater in small vessel disease and cardioembolic compared with controls.[61] An Italy study reported that Hcy is an independent risk factor for all subtypes of ischemic stroke.[62] Two other studies in a Turkish population demonstrated that Hcy had a significant role in large vessel atherothrombotic and cardioembolic stroke.[63,64] The different results in non-Chinese people and Chinese people caused by racial difference, regional difference, difference food habits and other factors. The methylene tetrahydrofolate reductase (MTHFR), cystathionine β-synthase (CBS), and methionine synthase (MS) are the key enzymes in Hcy metabolism. Studies have shown that the heterozygous mutation frequency of MTHFR C677T in Chinese[65] is higher than that which reported abroad,[66] and the homozygous mutation frequency of MTHFR C677T in Chinese[65] is the same with reported abroad.[66] The mutation frequency of CBS 844ins68 and MS A2756G in Chinese[65,67] was significantly lower than that in abroad[68,69] and the mutation frequency of MS A2756G in Chinese[65] is lower than that in Caucasians.[70,71] These genes play an important role in the synthesis and metabolism of Hcy. Some studies have shown that the MTHFR C677T polymorphism is associated with ischemic stroke,[72–75] while some studies have showed the different opinion.[76,77] A domestic meta-analysis[78] provided evidence that CBS T833C genetic polymorphism was associated with the risk of stroke. Nevertheless, the results from subgroups of Chinese and Caucasian are different. In the Chinese subgroup, the result showed CBS T833C polymorphism lead to increased incidence of stroke. Furthermore, the staple food is grains and the non-staple food is vegetables and some meat in China. In western countries, meat (such as: cattle, sheep, fish, pig, etc) is the main diet and the proportion of meat in the diet is higher than Chinese.
The finding of a few studies suggest that a 3 mmol/L lower total Hcy level could be associated with a 10% lower risk of recurrent strokes.[79] Recent studies have indicated that the risk of ischemic stroke in populations with high Hcy levels is 1.71 higher than among those with low levels.[80] Some studies have indicated founded that lowering Hcy levels can reduce the risk of ischemic stroke.[80,81] Accordingly, clarifying the correlation between Hcy and ischemic stroke, and reducing the Hcy levels of at-risk patients may play a role in the prevention of ischemic stroke.
The present study had several limitations. First, the different detection methods employed in the indicated studies to determine plasma Hcy levels may have sensitivity and reliability issues. Second, we were unable to analyze the effect of the acute stress reaction of ischemic stroke on plasma Hcy levels since there were insufficient data about Hcy levels before the onset of ischemic stroke. Third, few studies reported on other risk factors, such as blood pressure, blood glucose, obesity, and sexuality, in the results of their subgroup analyses. There is thus certainly a need for larger and wider case-control studies to explore the role of other factors that are likely to cause ischemic stroke.
5. Conclusions
Our meta-analysis found that the patients with ischemic and the TOAST subtypes in our study had significantly higher Hcy levels than in the healthy controls, and elevated Hcy levels may; therefore, be a risk factor for ischemic stroke and the TOAST subtypes of ischemic stroke in Chinese. However, further prospective population-based studies are needed to longitudinally evaluate the association between Hcy levels and the progression of different ischemic stroke subtypes. Additionally, the relatively limited number of eligible studies may influence the sensitivity of statistical analyses. Further randomized controlled trials with larger numbers of participants are necessary to confirm these findings.
Author contributions
Data curation: Tao Zhang, Yaogang Zhang, Jianhua Li.
Formal analysis: Tao Zhang, Yuan Jiang.
Investigation: Yuan Jiang, Meiyuan Tian.
Project administration: Shuhua Zhang, Tingting Tie, Yan Cheng.
Validation: Yan Cheng, Xiaoming Su, Zhu Man, Jing Hou, Li Sun.
Writing – original draft: tao zhang, Yuan Jiang.
Writing – review & editing: Yuan Jiang, Yanyan Ma.
Footnotes
Abbreviations: CE = cardioembolism, CI = confidence interval, Hcy = homocysteine, LAA = large-artery atherosclerosis, SAO = small-vessel occlusion, SMD = standardized mean difference, SOE = stroke of other determined etiology, SUE = stroke of undetermined etiology, TOAST = the trial of org 10172 in acute stroke treatment.
How to cite this article: Zhang T, Jiang Y, Zhang S, Tie T, Cheng Y, Su X, Man Z, Hou J, Sun L, Tian M, Zhang Y, Li J, Ma Y. The association between homocysteine and ischemic stroke subtypes in Chinese: A meta-analysis. Medicine. 2020;99:12(e107498).
TZ and YJ contributed equally to this work.
This work was funded by the QinghaiScience and Technology Foundation (No 2019-ZJ-922).
The authors have no conflicts of interest to disclose.
References
- [1].Hatano S. Experience from a multicentre stroke register: a preliminary report. Bull World Health Organ 1976;54:541–53. [PMC free article] [PubMed] [Google Scholar]
- [2].Bamford J, Sandercock P, Dennis M, et al. A prospective study of acute cerebrovascular disease in the community: the Oxfordshire Community Stroke Project 1981-86. 1. Methodology, demography and incident cases of first-ever stroke. J Neurol Neurosurg Psychiatry 1988;51:1373–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics--2013 update: a report from the American Heart Association. Circulation 2013;127:e6–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Adams HP, Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in acute stroke treatment. Stroke 1993;24:35–41. [DOI] [PubMed] [Google Scholar]
- [5].Lee JH, Oh E, Oh MS, et al. Highly variable blood pressure as a predictor of poor cognitive outcome in patients with acute lacunar infarction. Cogn Behav Neurol 2014;27:189–98. [DOI] [PubMed] [Google Scholar]
- [6].Nygård O, Nordrehaug JE, Refsum H, et al. Plasma homocysteine levels and mortality in patients with coronary artery disease. N Engl J Med 1997;337:230–6. [DOI] [PubMed] [Google Scholar]
- [7].Hoogeveen EK, Kostense PJ, Beks PJ, et al. Hyperhomocysteinemia is associated with an increased risk of cardiovascular disease, especially in non-insulin-dependent diabetes mellitus: a population-based study. Arterioscler Thromb Vasc Biol 1998;18:133–8. [DOI] [PubMed] [Google Scholar]
- [8].Makris M. Hyperhomocysteinemia is a risk factor for venous and arterial thrombosis. Br J Haematol 1998;101: Suppl 1: 18–20. [PubMed] [Google Scholar]
- [9].Malinow MR, Kang SS, Taylor LM, et al. Prevalence of hyperhomocyst(e)inemia in patients with peripheral arterial occlusive disease. Circulation 1989;79:1180–8. [DOI] [PubMed] [Google Scholar]
- [10].Clarke R, Daly L, Robinson K, et al. Hyperhomocysteinemia: an independent risk factor for vascular disease. N Engl J Med 1991;324:1149–55. [DOI] [PubMed] [Google Scholar]
- [11].Bos GM, den Heijer M. Hyperhomocysteinemia and venous thrombosis. Semin Thromb Hemost 1998;24:387–91. [DOI] [PubMed] [Google Scholar]
- [12].den Heijer M, Rosendaal FR, Blom HJ, et al. Hyperhomocysteinemia and venous thrombosis: a meta-analysis. Thromb Haemost 1998;80:874–7. [PubMed] [Google Scholar]
- [13].Sun Y, Chien KL, Hsu HC, et al. Use of serum homocysteine to predict stroke, coronary heart disease and death in ethnic Chinese. 12-year prospective cohort study. Circ J 2009;73:1423–30. [DOI] [PubMed] [Google Scholar]
- [14].Hultdin J, Van Guelpen B, Winkvist A, et al. Prospective study of first stroke in relation to plasma homocysteine and MTHFR 677C > T and 1298A > C genotypes and haplotypes - evidence for an association with hemorrhagic stroke. Clin Chem Lab Med 2011;49:1555–62. [DOI] [PubMed] [Google Scholar]
- [15].Bostom AG, Rosenberg IH, Silbershatz H, et al. Nonfasting plasma total homocysteine levels and stroke incidence in elderly persons: the Framingham Study. Ann Intern Med 1999;131:352–5. [DOI] [PubMed] [Google Scholar]
- [16].Bots ML, Launer LJ, Lindemans J, et al. Homocysteine and short-term risk of myocardial infarction and stroke in the elderly: the Rotterdam Study. Arch Intern Med 1999;159:38–44. [DOI] [PubMed] [Google Scholar]
- [17].Han L, Wu Q, Wang C, et al. Homocysteine, ischemic stroke, and coronary heart disease in hypertensive patients: a population-based, prospective cohort study. Stroke 2015;46:1777–86. [DOI] [PubMed] [Google Scholar]
- [18].Shi Z, Guan Y, Huo YR, et al. Elevated total homocysteine levels in acute ischemic stroke are associated with long-term mortality. Stroke 2015;46:2419–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Chen S, Dong Z, Cheng M, et al. Homocysteine exaggerates microglia activation and neuroinflammation through microglia localized STAT3 overactivation following ischemic stroke. J Neuroinflammation 2017;14:187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Yang G, Wang Y, Zeng Y, et al. Rapid health transition in China, 1990-2010: findings from the global burden of disease study 2010. Lancet 2013;381:1987–2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Zhou M, Wang H, Zeng X, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet 2019;394:1145–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;350:g7647. [DOI] [PubMed] [Google Scholar]
- [23].Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-analyses. Ottawa (ON): Ottawa Hospital Research Institute; 2009. [Google Scholar]
- [24].Yin SW, Ding SW, Dai JY, et al. The significance of serum homocysteine levels in 65 patients with cerebral infarction. Chin J Geriatr 2004;23:203. [Google Scholar]
- [25].Li N, Zhang YG, Guo XH, et al. Study on the association between homocysteine and the size of cerebral infarction. Chin J Rehabil Theory Pract 2005;11:370–1. [Google Scholar]
- [26].Wu JF. The analysis of plasma homocysteine levels in patients with atherosclerotic cerebral infarction. Med J Commun 2006;20:533–5. [Google Scholar]
- [27].Wang K, Pan XD, Ma AJ, et al. The TOAST subtypes of ischemic stroke in young adults and its related genes. Chin J Cerebrovasc Dis 2007;1:16–22. [Google Scholar]
- [28].Li XH, Liu P, Liu Y. The relationship between the plasma homocysteine levesl and the clinical subtypes of cerebral infarction. Med Philosophy 2009;30:53–5. [Google Scholar]
- [29].Yue H, Wang Y. The association between the homocysteine levels and the trail of Org10 172 in acute stroke treatment of the acute ischemic stroke. Chin Remed Clin 2011;11:840–1. [Google Scholar]
- [30].Liu XY. Analysis of the relation between acute ischemic stroke subtypes and plasma homocysteine levels. In: Wang Y.J., editor. Neurology, 2012. 11 [Google Scholar]
- [31].Zhang JH, Ma LL, Li JK, et al. Distribution characteristics of T lymphocyte subsets in peripheral blood of patients with the TOAST subtypes of cerebral infarction. Guangdong Med J 2014;35:3178–80. [Google Scholar]
- [32].Pan GQ, Wang WG. The Association between different subtypes of ischemic stroke and plasma homocysteine levels. Pract Prevent Med 2015;22:847–8. [Google Scholar]
- [33].Yu DL, Ming L, Tang XY, et al. Plasma markers and different subtypes of acute cerebral infarction: a correlation study. Chin Gen Med 2015;18:516–20. [Google Scholar]
- [34].Zhou ZQ, Huang YY, Song HF, et al. Study on the relationship between TOAST subtypes of ischemic stroke and homocysteine and uric acid levels. Chin Med Innov 2015;12:17–9. [Google Scholar]
- [35].Wu LP, Huang YX, Chen LK. The relationship between homocysteine, hr-CRP and the severity, classification of acute cerebral infarction. Guangxi Med J 2016;38:1285–6. [Google Scholar]
- [36].Zhang WB, Zheng YY, Yan F, et al. Clinical study on the relationship between homocysteine and the subtypes of acute ischemic stroke. Chin J Clin 2016;10:2193–6. [Google Scholar]
- [37].Adinolfi LE, Zampino R, Restivo L, et al. Chronic hepatitis C virus infection and atherosclerosis: clinical impact and mechanisms. World J Gastroenterol 2014;20:3410–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Kwon HM, Lee YS, Bae HJ, et al. Homocysteine as a predictor of early neurological deterioration in acute ischemic stroke. Stroke 2014;45:871–3. [DOI] [PubMed] [Google Scholar]
- [39].Zhong C, Lv L, Liu C, et al. High homocysteine and blood pressure related to poor outcome of acute ischemia stroke in Chinese population. PLoS One 2014;9:e107498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Iso H, Moriyama Y, Sato S, et al. Serum total homocysteine concentrations and risk of stroke and its subtypes in Japanese. Circulation 2004;109:2766–72. [DOI] [PubMed] [Google Scholar]
- [41].Ji Y, Song B, Xu Y, et al. Prognostic significance of homocysteine levels in acute ischemic stroke: a prospective cohort study. Curr Neurovasc Res 2015;12:334–40. [DOI] [PubMed] [Google Scholar]
- [42].Kumral E, Saruhan G, Aktert D, et al. Association of hyperhomocysteinemia with stroke recurrence after initial stroke. J Stroke Cerebrovasc Dis 2016;25:2047–54. [DOI] [PubMed] [Google Scholar]
- [43].Verhoef P, Hennekens CH, Malinow MR, et al. A prospective study of plasma homocyst(e)ine and risk of ischemic stroke. Stroke 1994;25:1924–30. [DOI] [PubMed] [Google Scholar]
- [44].Zhang W, Zhang X. Correlation between the youth cerebral infarction in different TOAST classifications and high homocysteine. Cell Biochem Biophys 2015;71:39–42. [DOI] [PubMed] [Google Scholar]
- [45].Poddar R, Sivasubramanian N, DiBello PM, et al. Homocysteine induces expression and secretion of monocyte chemoattractant protein-1 and interleukin-8 in human aortic endothelial cells: implications for vascular disease. Circulation 2001;103:2717–23. [DOI] [PubMed] [Google Scholar]
- [46].Zhang C, Cai Y, Adachi MT, et al. Homocysteine induces programmed cell death in human vascular endothelial cells through activation of the unfolded protein response. J Biol Chem 2001;276:35867–74. [DOI] [PubMed] [Google Scholar]
- [47].Sánchez-Moreno C, Jiménez-Escrig A, Martín A. Stroke: roles of B vitamins, homocysteine and antioxidants. Nutr Res Rev 2009;22:49–67. [DOI] [PubMed] [Google Scholar]
- [48].Banecka-Majkutewicz Z, Sawuła W, Kadziński L, et al. Homocysteine, heat shock proteins, genistein and vitamins in ischemic stroke--pathogenic and therapeutic implications. Acta Biochim Pol 2012;59:495–9. [PubMed] [Google Scholar]
- [49].Chen SF, Cui CL, Wu P, et al. Relationship of serum homocysteine level with nutritional status and HbA1c level in elderly inpatients. Int J Clin Exp Med 2013;6:779–84. [PMC free article] [PubMed] [Google Scholar]
- [50].Starkebaum G, Harlan JM. Endothelial cell injury due to copper-catalyzed hydrogen peroxide generation from homocysteine. J Clin Invest 1986;77:1370–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Mansoor MA, Bergmark C, Svardal AM, et al. Redox status and protein binding of plasma homocysteine and other aminothiols in patients with early-onset peripheral vascular disease. Homocysteine and peripheral vascular disease. Arterioscler Thromb Vasc Biol 1995;15:232–40. [DOI] [PubMed] [Google Scholar]
- [52].Thambyrajah J, Townend JN Homocysteine and atherothrombosis--mechanisms for injury. Eur Heart J 2000;21:967–74. [DOI] [PubMed] [Google Scholar]
- [53].Hossain M, Qadri SM, Liu L. Inhibition of nitric oxide synthesis enhances leukocyte rolling and adhesion in human microvasculature. J Inflamm (Lond) 2012;9:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Tyagi N, Givvimani S, Qipshidze N, et al. Hydrogen sulfide mitigates matrix metalloproteinase-9 activity and neurovascular permeability in hyperhomocysteinemic mice. Neurochem Int 2010;56:301–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Naess H, Nyland H, Idicula T, et al. C-reactive protein and homocysteine predict long-term mortality in young ischemic stroke patients. J Stroke Cerebrovasc Dis 2013;22:e435–40. [DOI] [PubMed] [Google Scholar]
- [56].Petras M, Tatarkova Z, Kovalska M, et al. Hyperhomocysteinemia as a risk factor for the neuronal system disorders. J Physiol Pharmacol 2014;65:15–23. [PubMed] [Google Scholar]
- [57].Pushpakumar S, Kundu S, Sen U. Endothelial dysfunction: the link between homocysteine and hydrogen sulfide. Curr Med Chem 2014;21:3662–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Pinna A, Zinellu A, Tendas D, et al. Plasma homocysteine and asymmetrical dimethyl-l-arginine (ADMA) and whole blood DNA methylation in early and neovascular age-related macular degeneration: a pilot study. Curr Eye Res 2016;41:88–96. [DOI] [PubMed] [Google Scholar]
- [59].Eikelboom JW, Hankey GJ, Anand SS, et al. Association between high homocyst(e)ine and ischemic stroke due to large- and small-artery disease but not other etiologic subtypes of ischemic stroke. Stroke 2000;31:1069–75. [DOI] [PubMed] [Google Scholar]
- [60].Ashjazadeh N, Fathi M, Shariat A. Evaluation of homocysteine level as a risk factor among patients with ischemic stroke and its subtypes. Iran J Med Sci 2013;38:233–9. [PMC free article] [PubMed] [Google Scholar]
- [61].Khan U, Crossley C, Kalra L, et al. Homocysteine and its relationship to stroke subtypes in a UK black population: the south London ethnicity and stroke study. Stroke 2008;39:2943–9. [DOI] [PubMed] [Google Scholar]
- [62].Parnetti L, Caso V, Santucci A, et al. Mild hyperhomocysteinemia is a risk-factor in all etiological subtypes of stroke. Neurol Sci 2004;25:13–7. [DOI] [PubMed] [Google Scholar]
- [63].Üstündağ M, Orak M, Güloğlu C, et al. The role of serum ferritin, pro-brain natriuretic peptide and homocysteine levels in determining ischaemic stroke subtype, severity and mortality. Hong Kong J Emerg Med 2010;17:13. [Google Scholar]
- [64].Tascilar N, Ekem S, Aciman E, et al. Hyperhomocysteinemia as an independent risk factor for cardioembolic stroke in the Turkish population. Tohoku J Exp Med 2009;218:293–300. [DOI] [PubMed] [Google Scholar]
- [65].Fu Y, Liu JR, Ni PH, et al. The relationship of plasma homocysteine levels and polymorphism in homocysteine metabolism related enzyms with brain stroke. Chin J Geriatr 2005;24:413–7. [Google Scholar]
- [66].Cattaneo M. Hyperhomocysteinemia, atherosclerosis and thrombosis. Thromb Haemost 1999;81:165–76. [PubMed] [Google Scholar]
- [67].Dai CW, Zhang GS. Study on homocysteine metabolism related enzymes gene mutations in Chinese patients with ischemic cardiovascular and cerebrovascular diseases. Chin J Hematol 2001;22:36–9. [PubMed] [Google Scholar]
- [68].Tsai MY, Yang F, Bignell M, et al. Relation between plasma homocysteine concentration, the 844ins68 variant of the cystathionine beta-synthase gene, and pyridoxal-5’-phosphate concentration. Mol Genet Metab 1999;67:352–6. [DOI] [PubMed] [Google Scholar]
- [69].Tsai MY, Bignell M, Yang F, et al. Polygenic influence on plasma homocysteine: association of two prevalent mutations, the 844ins68 of cystathionine beta-synthase and A (2756)G of methionine synthase, with lowered plasma homocysteine levels. Atherosclerosis 2000;149:131–7. [DOI] [PubMed] [Google Scholar]
- [70].Tsai MY, Welge BG, Hanson NQ, et al. Genetic causes of mild hyperhomocysteinemia in patients with premature occlusive coronary artery diseases. Atherosclerosis 1999;143:163–70. [DOI] [PubMed] [Google Scholar]
- [71].Wang XL, Duarte N, Cai H, et al. Relationship between total plasma homocysteine, polymorphisms of homocysteine metabolism related enzymes, risk factors and coronary artery disease in the Australian hospital-based population. Atherosclerosis 1999;146:133–40. [DOI] [PubMed] [Google Scholar]
- [72].Al-Allawi NA, Avo AS, Jubrael JM. Methylenetetrahydrofolate reductase C677T polymorphism in Iraqi patients with ischemic stroke. Neurol India 2009;57:631–5. [DOI] [PubMed] [Google Scholar]
- [73].Mejia Mohamed EH, Tan KS, Ali JM, et al. TT genotype of the methylenetetrahydrofolate reductase C677T polymorphism is an important determinant for homocysteine levels in multi-ethnic Malaysian ischaemic stroke patients. Ann Acad Med Singapore 2011;40:186–91. [PubMed] [Google Scholar]
- [74].Kalita J, Srivastava R, Bansal V, et al. Methylenetetrahydrofolate reductase gene polymorphism in Indian stroke patients. Neurol India 2006;54:260–3. [DOI] [PubMed] [Google Scholar]
- [75].Fekih-Mrissa N, Mrad M, Klai S, et al. Methylenetetrahydrofolate reductase (C677T and A1298C) polymorphisms, hyperhomocysteinemia, and ischemic stroke in Tunisian patients. J Stroke Cerebrovasc Dis 2013;22:465–9. [DOI] [PubMed] [Google Scholar]
- [76].Dikmen M, Ozbabalik D, Gunes HV, et al. Acute stroke in relation to homocysteine and methylenetetrahydrofolate reductase gene polymorphisms. Acta Neurol Scand 2006;113:307–14. [DOI] [PubMed] [Google Scholar]
- [77].Zoltán S, Somogyvári F, Szabó M, et al. Interactions between the MTHFR C677T and MTHFR A1298C mutations in ischaemic stroke. Ideggyogyaszati Szemle 2006;3-4:107–12. [PubMed] [Google Scholar]
- [78].Ding R, Lin S, Chen D. The association of cystathionine β synthase (CBS) T833C polymorphism and the risk of stroke: a meta-analysis. J Neurol Sci 2012;312:26–30. [DOI] [PubMed] [Google Scholar]
- [79].Toole JF, Malinow MR, Chambless LE, et al. Lowering homocysteine in patients with ischemic stroke to prevent recurrent stroke, myocardial infarction, and death: the vitamin intervention for stroke prevention (VISP) randomized controlled trial. JAMA 2004;291:565–75. [DOI] [PubMed] [Google Scholar]
- [80].Wang L, Shen J, Chen CX, et al. The association between homocysteine and the different ischemic stroke subtypes: a meta-analysis. Chin J Gerontol 2018;38:2052–5. [Google Scholar]
- [81].Huang X, Li Y, Li P, et al. Association between percent decline in serum total homocysteine and risk of first stroke. Neurology 2017;89:2101–7. [DOI] [PubMed] [Google Scholar]


