Abstract
Background:
Nonalcoholic fatty liver disease (NAFLD) is strongly associated with type 2 diabetes mellitus (T2DM), and low vitamin D levels are positively associated with NAFLD and T2DM. But there is absence of convincing evidence-based medicine to confirm the efficacy of vitamin D supplementation for T2DM with NAFLD. Thus, we aimed to conduct this meta-analysis to summarize the efficacy of vitamin D supplementation for T2DM combined with NAFLD, and help to further clarify its beneficial action on diabetic patients with NAFLD.
Methods:
The study only selects clinical randomized controlled trials of vitamin D supplementation for T2DM combined with NAFLD. We will search each database from the built-in until July 2020. The English literature mainly searches Cochrane Library, Pubmed, EMBASE, and Web of Science. While the Chinese literature comes from CNKI, CBM, VIP, and Wangfang database. Meanwhile, we will retrieve clinical trial registries and grey literature. Two researchers worked independently on literature selection, data extraction, and quality assessment. The dichotomous data is represented by relative risk (RR), and the continuous is expressed by mean difference (MD) or standard mean difference (SMD), eventually the data is synthesized using a fixed effect model (FEM) or a random effect model (REM) depending on the heterogeneity. The imaging markers of liver, biomarkers of hepatic steatosis, serological indexes of hepatic fibrosis, serum NAFLD liver fat score were evaluated as the main outcomes. While several secondary outcomes were also evaluated in this study. The statistical analysis of this meta-analysis was conducted by RevMan software version 5.3.
Results:
This meta-analysis will further determine the beneficial efficacy of vitamin D supplementation for T2DM combined with NAFLD.
Conclusion:
This study determines the positive efficacy of vitamin D supplementation for diabetic patients with NAFLD.
Keywords: meta-analysis, nonalcoholic fatty liver disease, protocol, type 2 diabetes mellitus, vitamin D supplementation
1. Introduction
Nonalcoholic fatty liver disease (NAFLD) is a spectrum of fat-associated liver conditions, may progress to nonalcoholic steatohepatitis (NASH), fibrosis, and cirrhosis.[1] The insulin resistance (IR), oxidative stress, and inflammation are major contributions for the development of NAFLD.[2,3] It has become the major cause of chronic liver disease worldwide.[4–6] The epidemic proportion of NAFLD is increasing, it has been estimated to be 25% to 30% among general adults in developed countries.[7,8] NAFLD is strongly associated with metabolic syndrome (MS) or type 2 diabetes mellitus (T2DM).[9] It has been reported that the prevalence of NAFLD in T2DM is up to 70%.[7,10] T2DM and IR are surely the strongest predictors of the progression of NAFLD to advanced fibrosis and cirrhosis.[11,12] Several published articles have manifested that NAFLD substantially increased the risk of incident T2DM.[13–16] Since IR is a key driver of NAFLD and T2DM, insulin-sensitizing drugs have been used to the NAFLD and T2DM treatment.[17] However, the absence of substantial clinical evidence demonstrated that insulin-sensitizing drugs have major beneficial actions on the progression of NAFLD.
Vitamin D is a fat-soluble vitamin and regulates the bone homeostasis.[18,19] Since vitamin D is an important component of many tissues, organs, and metabolic processes. The role of vitamin D has been extended to a wide-ranging non-skeletal health problems,[20] including MS, IR, T2DM, obesity, and cardiovascular disease.[21–23] There is increasing epidemiological evidence implying that vitamin D deficiency is associated with increased risk of developing diabetes.[24–26]
Meanwhile, there has been a significant scientific interest in the relationship between vitamin D status and NAFLD. Vitamin D has numerous properties that modulate IR, fibrogenesis, chronic inflammation, suggesting that vitamin D may be a target for preventing the progression of NAFLD.[27] Several clinical studies have shown that vitamin D deficiency may contribute to the onset and progression of NAFLD.[28–30] But there are absent evidences whether the vitamin D supplementation is beneficial for diabetic patients with NAFLD. Thus, we intend to collect randomized controlled trials (RCTs) about vitamin D supplementation for T2DM combined with NAFLD based on evidence-based medicine, and conduct a meta-analysis of its efficacy to provide higher quality clinical evidence for vitamin D supplementation is beneficial for NAFLD in diabetic patients.
2. Methods
2.1. Protocol registration
The systematic review protocol has been registered on the INPLASY website (https://inplasy.com/inplasy-2020-3-0012/) and INPLASY registration number is INPLASY202030012. It is reported following the guidelines of Cochrane Handbook for Systematic Reviews of Interventions and the Preferred Reporting Items for Systematic Reviews and Meta-analysis Protocol (PRISM).[31] If there are any adjustments throughout the study, we will fix and update the details in the final report.
2.2. Inclusion criteria
2.2.1. Study design
The study only selects clinical randomized controlled trials of vitamin D supplementation for T2DM combined with NAFLD published in both Chinese and English. However, animal experiments, reviews, case reports, and non-randomized controlled trials are excluded.
2.2.2. Participants
The patients with clinically diagnosed T2DM combined with NAFLD and treatment with vitamin D supplementation, regardless of race, gender, and age. NAFLD by other causes and patients with severe heart disease, liver and kidney dysfunction, mental illness, or a relevant drug allergic history will be not included.
2.2.3. Interventions
Both groups were treated with standard diabetes treatments, including diet, exercise, hypoglycemic, and lipid-lowering therapies. The experiment group used vitamin D supplementation, while the control group applied for placebo, or no treatment. In addition, the 2 groups did not take any drugs that interfered with the outcome indicators. The follow-up time was ≥12 weeks.
2.2.4. Outcomes
The primary outcomes include the improvement in clinical efficacy and imaging markers, biomarkers of hepatic steatosis, serological indexes of hepatic fibrosis, serum NAFLD liver fat score.
Secondary outcomes are mainly composed of fasting blood glucose, 2 hours postprandial blood glucose, HbA1c, serum insulin levels, body mass index (BMI), body weight, serological markers (LDL-cholesterol, triglyceride, HDL-cholesterol, aspartate transaminase (AST), alanine transaminase (ALT), γ-glutamyl transferase (GGT), albumin, etc), HOMA-IR, and adverse events.
2.3. Search methods
2.3.1. Electronic searches
We will retrieve each database from the built-in until July 2020. The English literature mainly searches Cochrane Library, Pubmed, EMBASE, and Web of Science. While the Chinese literature comes from CNKI, CBM, VIP, and Wangfang database. We adopt the combination of heading terms and free words as search strategy which decided by all the reviewers. Search terms: vitamin D supplementation, vitamin D deficiency, 25-hydroxy vitamin D [25(OH)D], ergocalciferol(s), nonalcoholic fatty liver disease, nonalcoholic steatohepatitis, fatty liver, nonalcoholic fatty liver, liver fibrosis, liver cirrhosis, type 2 diabetes mellitus, type 2 diabetes, diabetes, diabetes mellitus. We will simply present the search process of the Cochrane Library, as shown in Table 1, adjusting different search methods according to different Chinese and English databases.
Table 1.
Cochrane Library search strategy.

2.3.2. Searching other resources
At the same time, we will retrieve other resources to complete the deficiencies of the electronic databases, mainly searching for the clinical trial registries and grey literature about vitamin D for T2DM combined with NAFLD on the corresponding website.
2.4. Data collection and analysis
2.4.1. Selection of studies
Import all literatures that meet the requirements into Endnote X8 software. Firstly, 2 independent reviewers initially screened the literatures that did not meet the pre-established standards of the study by reading the title and abstract. Secondly, download the remaining literatures and read the full text carefully to further decide whether to include or not. Finally, the results were cross-checked repeatedly by reviewers. If there is a disagreement in the above process, we can reach an agreement by discussing between both reviewers or seek an opinion from third party. PRISMA flow diagram (Fig. 1) will be used to show the screening process of the study.
Figure 1.
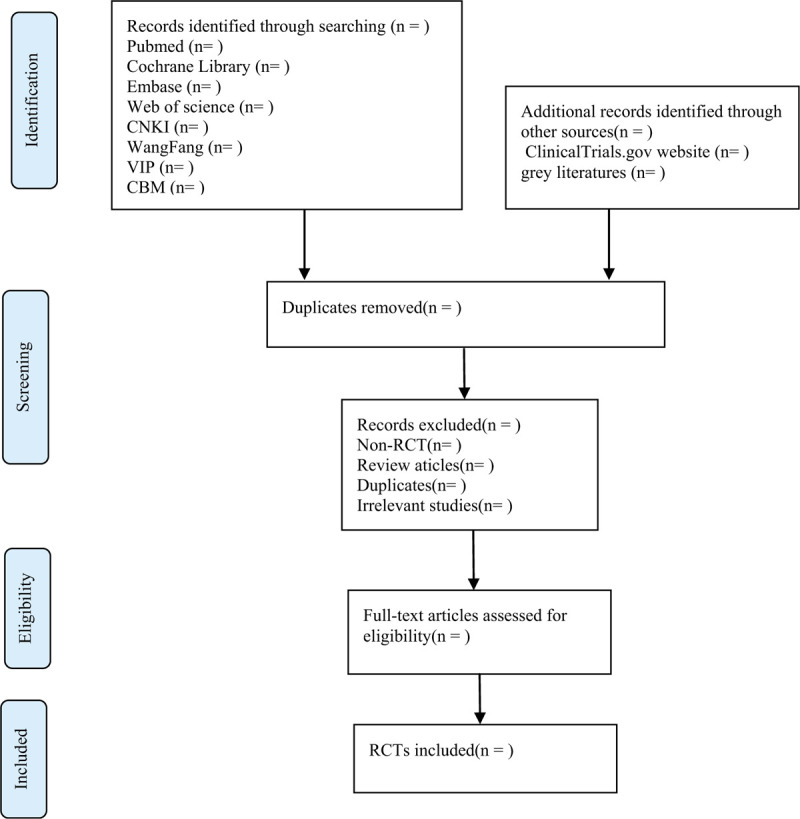
Flow chart of the study selection.
2.4.2. Data extraction and management
According to the characteristics of the study, we prepare an excel form for data collection before data extraction. Outcome indicators for eligible studies were independently extracted and filled in the data extraction form by 2 reviewers. If there is any argument, it can get an agreement by discussing through 2 reviewers or seek suggestions form third party. The main data extracted are as follows: title, author, year, fund source, sample size, age, gender, duration of disease, interventions, outcome measures, adverse reactions, etc. If you find something unclear in the study, you can contact the author of the communication directly for more detailed information. The above information was finally cross-checked by 2 reviewers.
2.4.3. Assessment of risk of bias in included studies
The quality assessment of RCTs adopts the risk of bias (ROB) assessment tool provided by the Cochrane Handbook. The following 7 items, such as random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and other bias, are evaluated by 3 grades of “low bias,” “high bias,” and “unclear bias.” The discrepancies will get a consistent conclusion by discussing between both reviewers or seeking the third-party consultation.
2.4.4. Measures of treatment effect
Different evaluation methods are selected according to the different efficacy indicators. For the dichotomous data, we will choose the effect scale indicator relative risk (RR) with 95% confidence interval (CI) to represent. While the continuous data is expressed as mean difference (MD) or standardized mean difference (SMD) with 95% CI depending on whether the measurement scale is consistent or not.
2.4.5. Dealing with missing data
The reviewers will contact the first author or correspondent author via email or telephone to obtain missing data if the relevant data is incomplete. If the missing data is still not obtained in the above way, we can synthesize the available data in the initial analysis. Furthermore, sensitivity analysis will be used to assess the potential impact of missing data on the overall results of the study.
2.4.6. Assessment of heterogeneity
Heterogeneity will be assessed by Chi-squared test and I2 test. If I2 < 50%, P > .1, we consider that no statistical heterogeneity between each study and choose fixed effect model (FEM) to synthesize the data. If I2 ≥ 50%, P < .1, indicating that there is a statistical heterogeneity, the data is integrated by the random effect model (REM). In addition, due to differences in heterogeneity, we will conduct subgroup or sensitivity analysis to look for the potential causes.
2.4.7. Data analysis
Review Manager software version 5.3 provided by the Cochrane Collaboration will be performed for data synthesis and analysis. The dichotomous data is represented by RR, continuous data is expressed by MD or SMD. If there is no heterogeneity (I2 < 50%, P > .1), the data is synthesized using a fixed effect model. Otherwise (I2 ≥ 50%, P < .1), a random effect model is used to analyze. Then subgroup analysis will be conducted based on the different causes of heterogeneity. If a meta-analysis cannot be performed, it will be replaced by a general descriptive analysis.
2.4.8. Subgroup analysis
If the results of the study are heterogeneous, we will conduct a subgroup analysis for different reasons. Heterogeneity is manifested in the following several aspects, such as race, age, gender, different intervention forms, pharmaceutical dosage, treatment course.
2.4.9. Sensitivity analysis
Sensitivity analysis is mainly used to evaluate the robustness of the primary outcome measures. The method is that removing the low-level quality study one by one and then merging the data to assess the impact of sample size, study quality, statistical method, and missing data on results of meta-analysis.
2.4.10. Grading the quality of evidence
In this systematic review, the quality of evidence for the entire study is assessed using the “Grades of Recommendations Assessment, Development, and Evaluation (GRADE)” standard established by the World Health Organization and international organizations.[32] To achieve transparency and simplification, the GRADE system divides the quality of evidence into 4 levels: high, medium, low, and very low.
3. Discussion
NAFLD has emerged a major challenge because of its prevalence, and lack of approved therapies. Documented evidence showing that NAFLD is a multisystem disease affecting multiple extrahepatic organ systems and interacting with the regulation of several metabolic/endocrine and pro-inflammatory pathways.[33] Indeed, convincing evidence manifesting that NAFLD is strongly associated with type 2 diabetes.[34]
Vitamin D has gained increasing attention in different research fields. The vitamin D receptor (VDR) may play a role in the mechanisms for the link between vitamin D deficiency and other disorders, such as diabetes,[35] nonalcoholic liver disease.[36] Recent studies have displayed that vitamin D has a key role in the regulation of oxidative, the production of pro-inflammatory cytokines, hepatocyte apoptosis, and even liver fibrosis.[37–39] It should be noted that vitamin D deficiency and NAFLD are also associated with IR and T2DM. For sure that NAFLD strongly related to T2DM, and both diseases are characterized by pro-atherogenic dyslipidemia, defined by hypertriglyceridemia, low high-density lipoprotein cholesterol concentrations, and the predominance of small dense LDL. In that low vitamin D levels are positively associated with NAFLD and T2DM. But there is absent convincing evidence-based medicine to confirm the efficacy of vitamin D supplementation for T2DM with NAFLD. Thus, we attempt to conduct this meta-analysis to analysis and summarize the efficacy of vitamin D supplementation for T2DM with NAFLD.
There are strengths in our study. Firstly, this meta-analysis provides a comprehensive assessment to whether vitamin D supplementation is beneficial for T2DM combined with NAFLD. Secondly, this study will provide clear evidence that vitamin D supplementation is good for diabetic patients with NAFLD. Moreover, RCTs will be included in our studies and appear to be high quality and low risk of bias. However, there may be some limitations in our meta-analysis. Firstly, both Chinese and English forms of research may increase the bias of the study. Secondly, the variety of race, age, gender, intervention forms, pharmaceutical dosage, and treatment course may result in higher clinical and statistical heterogeneity.
In conclusion, this study will help to determine the beneficial effects on diabetic patients with NAFLD. We hope this study will provide higher quality evidence for the benefits of vitamin D supplementation for T2DM combined with NAFLD.
Author contributions
Conceptualization: Shengju Wang, Baochao Cai.
Data curation: Shengju Wang, Baochao Cai, Xuke Han.
Formal analysis: Xuke Han, Yang Gao.
Funding acquisition: Qiu Chen.
Methodology: Shengju Wang, Baochao Cai, Xuke Han.
Project administration: Xiaoran Zhang.
Resources: Shengju Wang, Baochao Cai, Ruili Wang.
Software: Shengju Wang, Baochao Cai, Yuan Zhang.
Supervision: Qiu Chen.
Writing – original draft: Shengju Wang, Baochao Cai.
Writing – review & editing: Qiu Chen.
Footnotes
Abbreviations: ALT = alanine transaminase, AST = aspartate transaminase, BMI = body mass index, CI = confidence interval, FEM = fixed effect model, GGT = γ-glutamyl transferase, IR = insulin resistance, MD = mean difference, MS = metabolic syndrome, NAFLD = nonalcoholic fatty liver disease, NASH = nonalcoholic steatohepatitis, PRISMA-P = Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocol, RCT = randomized controlled trial, REM = random effect model, RR = relative risk, SMD = standard mean difference, T2DM = type 2 diabetes mellitus, VDR = vitamin D receptor.
How to cite this article: Wang S, Cai B, Han X, Gao Y, Zhang X, Wang R, Zhang Y, Chen Q. Vitamin D supplementation for nonalcoholic fatty liver disease in type 2 diabetes mellitus: A protocol for a systematic review and meta-analysis. Medicine. 2020;99:19(e20148).
SW and BC contributed equally to this work as co-first authors.
This study was supported by Research Project for Practice Development of National Traditional Chinese Medicine Clinical Research Bases (No. JDZX2015216).
This review is based solely on a secondary study of published literatures and does not require ethics committee approval. Its conclusion will be disseminated in conference papers, magazines, or peer-reviewed journals.
Registration number: INPLASY202030012.
The authors have no conflicts of interest to disclose.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
References
- [1].Gasbarrini G, Vero V, Miele L, et al. Nonalcoholic fatty liver disease: defining a common problem. Eur Rev Med Pharmacol Sci 2005;9:253–9. [PubMed] [Google Scholar]
- [2].Videla LA, Rodrigo R, Araya J, et al. Insulin resistance and oxidative stress interdependency in non-alcoholic fatty liver disease. Trends Mol Med 2006;12:555–8. [DOI] [PubMed] [Google Scholar]
- [3].Tilg H, Moschen AR. Insulin resistance, inflammation, and non-alcoholic fatty liver disease. Trends Endocrinol Metab 2008;19:371–9. [DOI] [PubMed] [Google Scholar]
- [4].Anstee QM, Targher G, Day CP. Progression of NAFLD to diabetes mellitus, cardiovascular disease or cirrhosis. Nat Rev Gastroenterol Hepatol 2013;10:330–44. [DOI] [PubMed] [Google Scholar]
- [5].Dyson J, Jaques B, Chattopadyhay D, et al. Hepatocellular cancer: the impact of obesity, type 2 diabetes and a multidisciplinary team. J Hepatol 2014;60:110–7. [DOI] [PubMed] [Google Scholar]
- [6].Lonardo A, Ballestri S, Marchesini G, et al. Nonalcoholic fatty liver disease: a precursor of the metabolic syndrome. Dig Liver Dis 2015;47:181–90. [DOI] [PubMed] [Google Scholar]
- [7].Bellentani S, Marino M. Epidemiology and natural history of non-alcoholic fatty liver disease (NAFLD). Ann Hepatol 2009;8: Suppl 1: S4–8. [PubMed] [Google Scholar]
- [8].Vernon G, Baranova A, Younossi ZM. Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment Pharmacol Therap 2011;34:274–85. [DOI] [PubMed] [Google Scholar]
- [9].Valenti L, Bugianesi E, Pajvani U, et al. Nonalcoholic fatty liver disease: cause or consequence of type 2 diabetes? Liver Int 2016;36:1563–79. [DOI] [PubMed] [Google Scholar]
- [10].Bril F, Cusi K. Management of nonalcoholic fatty liver disease in patients with type 2 diabetes: a call to action. Diabetes Care 2017;40:419–30. [DOI] [PubMed] [Google Scholar]
- [11].Kim D, Touros A, Kim WR. Nonalcoholic fatty liver disease and metabolic syndrome. Clin Liver Dis 2018;22:133–40. [DOI] [PubMed] [Google Scholar]
- [12].Neuschwander-Tetri BA. Non-alcoholic fatty liver disease. BMC Med 2017;15:45–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Park SK, Seo MH, Shin HC, et al. Clinical availability of nonalcoholic fatty liver disease as an early predictor of type 2 diabetes mellitus in Korean men: 5-year prospective cohort study. Hepatology (Baltimore, MD) 2013;57:1378–83. [DOI] [PubMed] [Google Scholar]
- [14].Yamazaki H, Tsuboya T, Tsuji K, et al. Independent association between improvement of nonalcoholic fatty liver disease and reduced incidence of type 2 diabetes. Diabetes Care 2015;38:1673–9. [DOI] [PubMed] [Google Scholar]
- [15].Ming J, Xu S, Gao B, et al. Non-alcoholic fatty liver disease predicts type 2 diabetes mellitus, but not prediabetes, in Xi’an, China: a five-year cohort study. Liver Int 2015;35:2401–7. [DOI] [PubMed] [Google Scholar]
- [16].Li W-D, Fu K-F, Li G-M, et al. Comparison of effects of obesity and non-alcoholic fatty liver disease on incidence of type 2 diabetes mellitus. World J Gastroenterol 2015;21:9607–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Dongiovanni P, Rametta R, Meroni M, et al. The role of insulin resistance in nonalcoholic steatohepatitis and liver disease development – a potential therapeutic target? Expert Rev Gastroenterol Hepatol 2016;10:229–42. [DOI] [PubMed] [Google Scholar]
- [18].Pacifico L, Osborn JF, Bonci E, et al. Association between vitamin D levels and nonalcoholic fatty liver disease: potential confounding variables. Mini Rev Med Chem 2019;19:310–32. [DOI] [PubMed] [Google Scholar]
- [19].Liu S, Liu Y, Wan B, et al. Association between vitamin D status and non-alcoholic fatty liver disease: a population-based study. J Nutr Sci Vitaminol (Tokyo) 2019;65:303–8. [DOI] [PubMed] [Google Scholar]
- [20].Theodoratou E, Tzoulaki I, Zgaga L, et al. Vitamin D and multiple health outcomes: umbrella review of systematic reviews and meta-analyses of observational studies and randomised trials. BMJ (Clinical research ed) 2014;348:g2035–12035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Reid IR. What diseases are causally linked to vitamin D deficiency? Arch Dis Child 2016;101:185–9. [DOI] [PubMed] [Google Scholar]
- [22].Alvarez JA, Ashraf A. Role of vitamin D in insulin secretion and insulin sensitivity for glucose homeostasis. Int J Endocrinol 2010;2010:351385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Al Mheid I, Patel RS, Tangpricha V, et al. Vitamin D and cardiovascular disease: is the evidence solid? Eur Heart J 2013;34:3691–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Belenchia AM, Tosh AK, Hillman LS, et al. Correcting vitamin D insufficiency improves insulin sensitivity in obese adolescents: a randomized controlled trial. Am J Clin Nutr 2013;97:774–81. [DOI] [PubMed] [Google Scholar]
- [25].Forouhi NG, Menon RK, Sharp SJ, et al. Effects of vitamin D2 or D3 supplementation on glycaemic control and cardiometabolic risk among people at risk of type 2 diabetes: results of a randomized double-blind placebo-controlled trial. Diabetes Obes Metab 2016;18:392–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Mitri J, Dawson-Hughes B, Hu FB, et al. Effects of vitamin D and calcium supplementation on pancreatic (cell function, insulin sensitivity, and glycemia in adults at high risk of diabetes: the calcium and vitamin D for diabetes mellitus (CaDDM) randomized controlled trial. Am J Clin Nutr 2011;94:486–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Iruzubieta P, Terán Á, Crespo J, et al. Vitamin D deficiency in chronic liver disease. World J Hepatol 2014;6:901–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Chung GE, Kim D, Kwak M-S, et al. The serum vitamin D level is inversely correlated with nonalcoholic fatty liver disease. Clin Mol Hepatol 2016;22:146–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Eliades M, Spyrou E, Agrawal N, et al. Meta-analysis: vitamin D and non-alcoholic fatty liver disease. Aliment Pharmacol Therap 2013;38:246–54. [DOI] [PubMed] [Google Scholar]
- [30].Rhee E-J, Kim MK, Park SE, et al. High serum vitamin D levels reduce the risk for nonalcoholic fatty liver disease in healthy men independent of metabolic syndrome. Endocr J 2013;60:743–52. [DOI] [PubMed] [Google Scholar]
- [31].Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ (Clinical research ed) 2015;350:g7647–17647. [DOI] [PubMed] [Google Scholar]
- [32].Balshem H, Helfand M, Schünemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 2011;64:401–6. [DOI] [PubMed] [Google Scholar]
- [33].Byrne CD, Targher G. NAFLD: a multisystem disease. J Hepatol 2015;62:S47–64. [DOI] [PubMed] [Google Scholar]
- [34].van den Berg EH, Flores-Guerrero JL, Gruppen EG, et al. Non-alcoholic fatty liver disease and risk of incident type 2 diabetes: role of circulating branched-chain amino acids. Nutrients 2019;11:705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Mitri J, Muraru M, Pittas A. Vitamin D and type 2 diabetes: a systematic review. Eur J Clin Nutr 2011;65:1005–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Targher G, Bertolini L, Scala L, et al. Associations between serum 25-hydroxyvitamin D3 concentrations and liver histology in patients with non-alcoholic fatty liver disease. Nutr Metab Cardiovasc Dis 2007;17:517–24. [DOI] [PubMed] [Google Scholar]
- [37].George N, Kumar TP, Antony S, et al. Effect of vitamin D 3 in reducing metabolic and oxidative stress in the liver of streptozotocin-induced diabetic rats. Br J Nutr 2012;108:1410–8. [DOI] [PubMed] [Google Scholar]
- [38].Roth CL, Elfers CT, Figlewicz DP, et al. Vitamin D deficiency in obese rats exacerbates nonalcoholic fatty liver disease and increases hepatic resistin and Toll-like receptor activation. Hepatology (Baltimore, MD) 2012;55:1103–11. [DOI] [PubMed] [Google Scholar]
- [39].Potter JJ, Liu X, Koteish A, et al. 1,25-dihydroxyvitamin D3 and its nuclear receptor repress human α1 (I) collagen expression and type I collagen formation. Liver Int 2013;33:677–86. [DOI] [PMC free article] [PubMed] [Google Scholar]


