Abstract
This study aims to examine the association between sleep duration and cognitive impairment in community-dwelling Chinese older adults.
The associations between sleep duration and cognitive function have been widely studied across various age ranges but are of particular importance among older adults. However, there are inconsistent findings regarding the relationship between sleep duration and cognitive function in the literature.
This study is an observational cross-sectional study. We analyzed data from 1115 Chinese individuals aged 60 and older from 3 Chinese communities (Beijing, Hefei, and Lanzhou). Cognitive impairment was defined as a Mini-Mental State Examination total score less than 24 points. Odds ratios (ORs) of associations were calculated and adjusted for potential confounders in logistic regression models.
The prevalence of cognitive impairment was 25.7% (n = 287). Controlling for all demographic, lifestyle factors, and coexisting conditions, the adjusted OR for cognitive impairment was 2.54 (95% CI = 1.70–3.80) with <6 hours sleep and 2.39 (95% CI = 1.41–4.06) with >8 hours sleep.
Both short and long sleep durations were related to worse cognitive function among community-dwelling Chinese elderly adults.
Keywords: aging, cognitive impairment, self-report, sleep duration
1. Introduction
As the world population ages, an increasing number of people will begin to have age-related disorders, including cognitive impairment.[1] In China, more than 10% of older individuals experience cognitive impairment, ranging from mild deficits to dementia.[2,3] Therefore, studying the risk factors to reduce the incidence of cognitive impairment is becoming an increasingly important area of research.[4]
The associations between sleep duration and cognitive function have been widely studied across various age ranges but are of particular importance among older adults, given that changes in sleep duration and cognitive performance are quite prevalent in this group. Studies investigating the relationship between sleep duration and cognitive function in older adults have reported inconsistent findings.[5–7] A study in Spain showed that long, but not short, sleep duration was associated with decreased cognitive function.[5] Self-reported low sleep quality among postmenopausal women was reported to be associated with decreased cognitive test performance and difficulty in concentrating.[8] A study in Finland reported that short and long sleep durations were associated with both objectively assessed and self-reported decreases in cognitive functioning.[5] However, the Nurses’ Health Study showed that neither long nor short sleep duration was associated with a decline in cognitive function after a 2-year follow-up.[9]
We expanded on these previous studies by recruiting a community-dwelling elderly population sample from 3 cities in China to evaluate the association between self-reported sleep hours and short and long sleep durations with global cognitive function.
2. Materials and methods
2.1. Participants
Participants were selected from 3 cities in China: Beijing (North China), Hefei (Central China), and Lanzhou (Northwest China). We randomly selected 1 aged community from each city, and from November 2017 to May 2018, approximately 400 residents aged over 60 years old were randomly selected from each community. Data collection methods and ethical approvals have been described previously.[4] The study protocols were approved by the Chinese Academy Medical Sciences, and all participants provided written informed consent. The questionnaires were completed by trained nurses. We excluded those with severe mental disorders and hearing impairments, and the final sample size was 1115 in this study (85 incomplete questionnaires, 7.1%). Age was divided into 3 groups: 60 to 69, 70 to 79, and over 80 years. Education levels were classified into 3 categories: primary school and under, middle school, and college and over.
2.2. Cognition measurement
The Mini-Mental State Examination (MMSE) screening test was administered to participants by trained nurses. The MMSE is a measure of general cognitive function that measures orientation to time and place, attention and calculation, language and memory.[10] The MMSE has good sensitivity (71%–92%) and specificity (56%–96%) in screening for cognitive impairment and dementia.[7] The summed scores from the MMSE ranged from 0 to 30, where higher values denoted better cognitive functioning. Cognitive impairment was defined as having MMSE scores of less than 24 points.
2.3. Sleep hours and covariates
We collected self-reported sleep duration as an estimate of hours of nightly sleep in the 2 weeks prior to the interview, using the following question: “During the past 2 weeks, how many hours, on average, did you sleep each night?” Respondents reported the number of hours in 30-minute increments. The responses ranged from 3 to 12 hours of sleep with a median of 7 hours. We examined self-reported sleep hours in categories of short sleep (< 6 hours) and long sleep (> 8 hours), with 6 to 8 hours of nightly sleep as the reference. Body mass index (BMI) was calculated based on weight and height and divided into categories using the recommended cutoffs of <18.5, 18.5 to 25, 25 to 30, and >30. Smoking status was classified as either smoker or nonsmoker in the past 2 years. Persons who self-reported consumption of beer, wine, or cocktails were classified as consumers of alcohol. Salty taste and dessert preference were dichotomized based on whether the participant had diet preferences in the past 2 years (self-reported). Physical activities were assessed by frequency (0 = never, 1 = sometimes, 2 = often). In the analysis, persons who self-reported “sometimes” and “often” were classified as participants, while those who self-reported “never” were classified as nonparticipants. Coexisting conditions such as hypertension, stroke, diabetes, and cancer were self-reported by the participants.
2.4. Analysis
Descriptive statistics were generated for the demographic variables, including age, sex, education, BMI, lifestyle factors, and coexisting conditions. The results are presented as the mean ± standard deviation or median (interquartile range) for the continuous variables according to the distribution of the data and as the proportion for categorical variables. The distribution of sleep hours was compared between demographic variables, lifestyle factors, and coexisting conditions. χ2 tests or ANOVA were used to compare between groups. For the associations between short, long, and normal sleep durations and cognitive impairment, we first performed a univariate logistic regression analysis, followed by a model adjusted for age, sex, and education; and finally, a model that further accounted for coexisting conditions. The associations between sleep and cognitive impairment were determined, and 95% confidence intervals (CIs) were calculated for the odds ratio (OR) estimates. All analyses were performed using Stata version 15.0.
3. Results
There were 1115 participants (age >= 60 years), ranging in age from 60 to 99 years, who completed the cognition test and social support questionnaire. After the cognitive function screening (median MMSE score was 24; p25–p75: 19–28), 287 (25.7%) elderly participants were considered cognitively impaired in this study. Age and sex were strongly associated with cognitive impairment. We divided the participants into 3 groups based on age; the prevalence of cognitive impairment in the advanced age groups was higher than that in the lower age group (P = .002). The female participants showed lower cognitive function than the male participants (P < .001). A higher education level was associated with a reduced risk of cognitive impairment (P < .001). Cognitive impairment was different among the BMI groups, and this was consistent with findings in the literature.[11,12] Lifestyle factors, except dessert preference, may be associated with cognitive performance in this study. Hypertension patients were more likely to have cognitive impairment, while the differences were not significant between the diabetes, stroke, and cancer patients and nonpatients in this study (Table 1).
Table 1.
Demographic variables, lifestyle factors, and coexisting conditions of the 1115 participants.
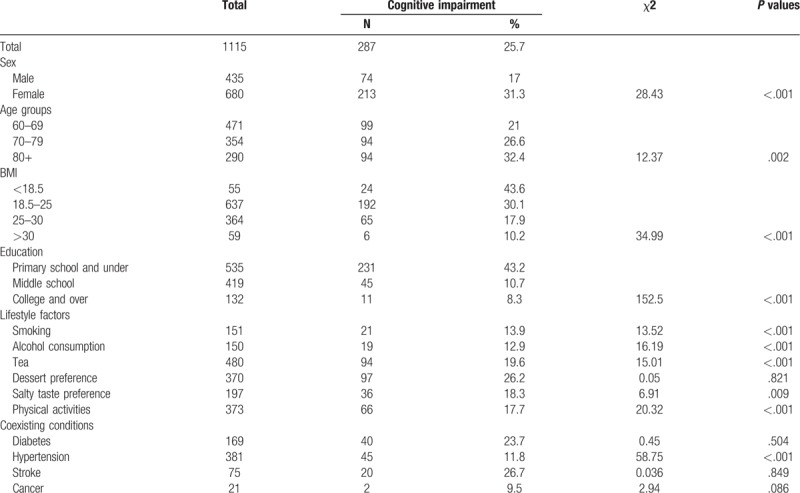
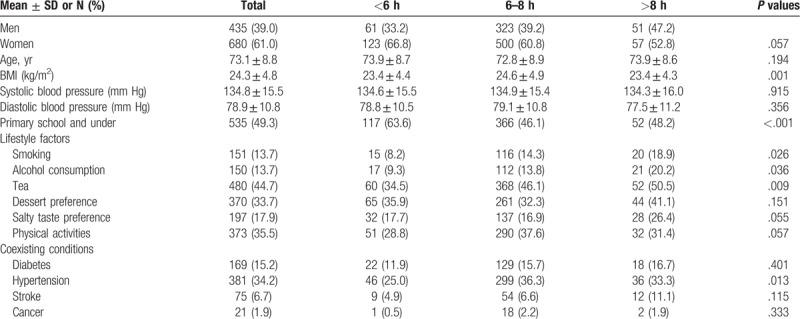
Table 2 presents the characteristics of the overall sample and across categories of sleep duration. Self-reports of < 6 hours of sleep were observed in 16.5% (n = 184) of the sample, and reports of > 8 hours of sleep were observed in 9.7% (n = 108). The participants reporting > 8 hours or <6 hours of sleep were older, had lower BMI and lower education experience than participants reporting 6 to 8 hours of sleep. The older persons who had lifestyle risk factors such as smoking, drinking alcohol or tea, and salty taste preferences had a longer duration of sleep than those without these factors. Participants who engaged in physical activities seemed to have normal sleep duration in this study. There were no significant differences in the sex ratio, dessert preference or frequencies of diabetes, stroke, or cancer among the groups.
Table 2.
The characteristics of the overall sample and across categories of sleep duration.
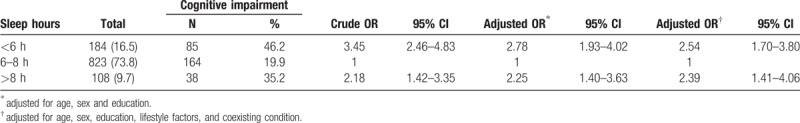
Self-reported sleep durations were associated with cognitive impairment in this study. Figure 1 demonstrates the inverted U-shaped function of the MMSE scores by sleep duration across ages and sexes. Table 3 shows the crude and adjusted ORs for cognitive impairment according to hours of sleep. With the 6 to 8 hours sleep duration as the referent, the crude ORs for cognitive impairment were 3.45 (95% CI = 2.46–4.83) in those with <6 hours sleep and 2.18 (95% CI = 1.42–3.35) in those with >8 hours sleep. Controlling for age, sex, and education, the adjusted OR for cognitive impairment was 2.78 (95% CI = 1.93–4.02) in those with <6 hours sleep and 2.25 (95% CI = 1.40–3.63) in those with >8 hours sleep. We continued to adjust for all demographic variables, lifestyle factors, and coexisting conditions in the full model and found that the associations between both short and long durations of sleep and cognitive impairment were still significant, with adjusted ORs of 2.54 (95% CI = 1.70–3.80) and 2.39 (95% CI = 1.41–4.06), respectively.
Figure 1.
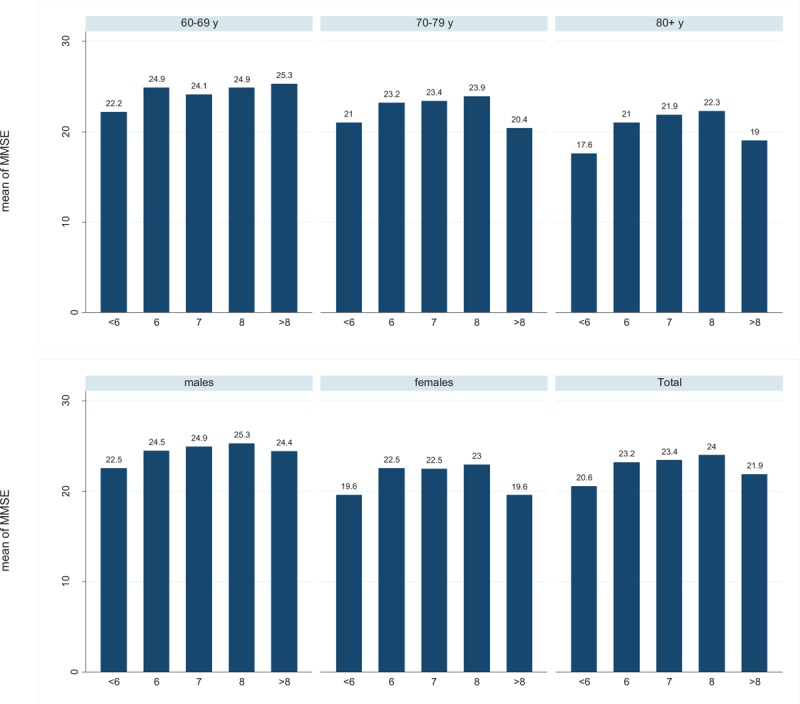
The mean MMSE scores and sleep durations by age and sex.
Table 3.
Association of sleep duration with cognitive impairment among Chinese community-dwelling elderly individuals.
4. Discussion
We enrolled 1115 residents in 3 urban communities to assess the associations between sleep duration and cognitive impairment. The distributions of sleep duration were different among the groups based on lifestyle factors. The persons without risk factors such as smoking, drinking, and engaging in less physical activities tended to have normal daily sleep durations (6–8 hours). Lower BMI and chronic diseases may be associated with either short or long sleep durations. Both short and long sleep durations were significantly associated with cognitive impairment among the elderly individuals in this study after adjusting for demographic factors, lifestyle factors, and coexisting conditions.
Although not the focus of the present study, sleep duration categories were associated with sociodemographic and lifestyle variables, in accordance with a number of prior studies.[13] In the present sample, the short sleepers tended to be less educated; the long sleepers tended to have lifestyle risk factors such as smoking and drinking. Smoking has been related to both short and long durations of sleep among Iranian women.[14] Self-reported long sleepers were more likely to have reported increased alcohol intake in a dietary nutrition study in the US,[13] which may have important health consequences. Many studies have investigated the associations between sleep duration and obesity, but the results have been inconsistent. Short sleep durations were associated with lower BMI in a cohort study in Japan.[15] The Shanghai Women's Health Study found that high BMI, waist to hip ratio, and waist circumference were associated with long sleep durations after adjustment for energy intake and other confounders.[16] In this study, people with normal sleep durations had higher BMI than those with short or long sleep durations. The relationship between sleep duration and BMI could be reciprocal, and physiologic studies are needed to better understand the effect of sleep duration on weight regulation.[16] Short sleep duration was inversely associated with tea consumption. A possible explanation for our finding is the development of a tolerance to the sleep-reducing effects of caffeine.[16] Further study on the association between sleep duration and tea consumption is necessary to obtain causal inferences. It is beyond the scope of the current paper to speculate regarding these associations, but it should be noted that these differences may play a role in how cognitive impairment is associated with sleep. For this reason, future studies should also include these covariates in any analysis.
Our findings are consistent with studies in the literature where findings have been mixed but have tended to suggest that shorter or longer sleep durations, or both, are associated with worse cognitive function.[6,17,18] Short or long sleep durations were found to be an important sleep-related factor that was independently associated with memory impairments in the Guangzhou Biobank Cohort Study.[19] Short sleep duration has been cross-sectionally associated with initial cognitive impairment.[20] The Nurses’ Health Study cohort found that women who reported a short duration of sleeping (≤5 h/night) were at increased risk for cognitive impairment in cross-sectional analyses.[20] A community-based study of men and women over 60 years old reported that short sleep durations were significantly associated with lower cognitive function, particularly in tests of attention/concentration and orientation.[21] Poor sleep was reported to be associated with impaired cognitive function in a study of older women with osteoporotic fractures.[22] Although the data are limited, these results could suggest that self-reported sleep was associated with impaired cognitive function. One hypothesis to explain this is that factors that regulate the perception of sleep quality may also be related to a brain state that affects cognitive function.[23] The associations in this work were based on a cross-sectional design, and reverse causation may exist. Thus, it is also possible that diminished cognitive function results in a brain state that leads to altered sleep perception.
The association between long sleep duration and cognitive impairment has been found in some previous studies. A study in Spain concluded that long sleep durations were associated with poorer cognitive function in older adults from the general population: the risk of cognitive impairment increased across sleep duration groups from 7 to ≥ 11 hours.[5] In a cross-sectional study in people aged 75 to 85 years in both sexes, it was observed that those who reported longer sleep duration performed significantly worse on a measure of verbal short-term memory.[24] Long sleep duration could reflect both a greater physiological need for sleep and a mechanism to compensate for poor quality sleep.[25] A relationship between sleep breathing disorders, which are fairly frequent in elderly people, and cognitive impairment has also been observed.[26] Long sleep duration could also be explained by sleep fragmentation. Fragmented sleep measured by actigraphy was associated with worse global cognitive function, independent of sleep duration, in a cross-sectional analysis of the Rush Memory and Aging Project.[27]
Our study had several limitations. First, this study was a cross-sectional study and cannot provide causal relationships between sleep duration and cognitive impairment. Additional longitudinal studies are needed to validate the findings. Second, residual confounding effects from unmeasured variables were possible and may have contributed to the observed associations. Sleep duration is a complex physiological process that is influenced by many factors, such as psychology, sleeping habits, and sleep medication. Additionally, apolipoprotein E has been strongly associated with cognition.[28,29] These unmeasured factors could have confounded the associations under study. Third, sleep duration was derived from a self-reported questionnaire item without investigating the questionnaire reliability or objective sleep patterns, which may have also introduced bias. Individuals with cognitive impairment, especially those affected by memory impairment may not accurately report the sleep duration. Further studies with prospective designs and objective assessments of sleep-related factors in addition to self-reported data are warranted. Furthermore, studies of incident dementia suggest that sleep problems increase the risk of dementia.[30–32] Sleep and Alzheimer disease (AD) may have a bidirectional relationship. However, an important consideration is that the diagnosis of AD typically occurs years after the onset of pathological changes of AD in the brain.[33] Studies with substantially longer follow-up times rather than cross-sectional trials are needed to discern the directionality and underlying mechanisms of the relationship between AD and sleep abnormalities.[33] Last, it is possible that the associations may not be fully generalizable outside of this study because the sample was comprised only of those from 3 urban communities.
In summary, the present study showed that both long and short sleep durations were related to cognitive function among Chinese community-dwelling older individuals. Less than optimal demographics, an unhealthy lifestyle, and poor health conditions were related to short or long sleep durations.[16] Future research is necessary to better understand the mechanisms by which sleep duration might be associated with cognitive function. Interventional studies based on sleep treatment for the prevention of cognitive impairment are needed in the future.
5. Ethics
The study protocols and participant consent forms were approved by the Chinese Academy Medical Sciences (X170315009); all participants provided written informed consent.
Acknowledgments
Funding: Supported by the Fundamental Research Funds for the Central Universities (3332019112)
Author contributions
Data curation: Zhiwei Lian, Jinlei Li.
Original draft: Gongwu Ding, Jinlei Li.
Review & editing: Gongwu Ding.
Explanation: Jinlei Li.
Footnotes
Abbreviations: AD = Alzheimer disease, BMI = body mass index, CI = confidence interval, MMSE = Mini-Mental State Examination, OR = odds ratios.
How to cite this article: Ding G, Li J, Lian Z. Both short and long sleep durations are associated with cognitive impairment among community-dwelling Chinese older adults. Medicine. 2020;99:13(e19667).
The authors have no funding and conflicts of interest to disclose.
References
- [1].Wang B, He P, Dong B. Associations between social networks, social contacts, and cognitive function among Chinese nonagenarians/centenarians. Arch Gerontol Geriatr 2015;60:522–7. [DOI] [PubMed] [Google Scholar]
- [2].Chan KY, Wang W, Wu JJ, et al. Epidemiology of Alzheimer's disease and other forms of dementia in China, 1990-2010: a systematic review and analysis. Lancet 2013;381:2016–23. [DOI] [PubMed] [Google Scholar]
- [3].Nie H, Xu Y, Liu B, et al. The prevalence of mild cognitive impairment about elderly population in China: a meta-analysis. Int J Geriatr Psychiatry 2011;26:558–63. [DOI] [PubMed] [Google Scholar]
- [4].Li J, Wang Z, Lian Z, et al. Social networks, community engagement, and cognitive impairment among community-dwelling Chinese older adults. DEE 2019;9:330–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Kronholm E, Sallinen M, Suutama T, et al. Self-reported sleep duration and cognitive functioning in the general population. J Sleep Res 2009;18:436–46. [DOI] [PubMed] [Google Scholar]
- [6].Devore EE, Grodstein F, Duffy JF, et al. Sleep duration in midlife and later life in relation to cognition. J Am Geriatr Soc 2014;62:1073–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Ramos AR, Dong C, Elkind MSV, et al. Association between sleep duration and the mini-mental score: the Northern Manhattan study. J Clin Sleep Med 2013;9:669–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Kavikondala S, Jiang CQ, Zhang WS, et al. Intergenerational “mismatch” and adiposity in a developing population: the Guangzhou biobank cohort study. Soc Sci Med 2010;70:834–43. [DOI] [PubMed] [Google Scholar]
- [9].Devore E, Grodstein F, Schernhammer E. Sleep duration and cognitive function: the Nurses’ Health Study. Alzheimers Dement 2012;8: Suppl 1: P233. [Google Scholar]
- [10].Folstein MF, Folstein SE, McHugh PR. Mini-mental state. a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189–98. [DOI] [PubMed] [Google Scholar]
- [11].Li J, Ogrodnik M, Kolachalama VB, et al. Assessment of the mid-life demographic and lifestyle risk factors of dementia using data from the Framingham Heart Study Offspring Cohort. J Alzheimers Dis 2018;63:1119–27. [DOI] [PubMed] [Google Scholar]
- [12].Li J, Ogrodnik M, Devine S, et al. Practical risk score for 5-, 10-, and 20-year prediction of dementia in elderly persons: Framingham Heart Study. Alzheimers Dement 2018;14:35–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Grandner MA, Jackson N, Gerstner JR, et al. Dietary nutrients associated with short and long sleep duration. Data from a nationally representative sample. Appetite 2013;64:71–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Kripke DF, Garfinkel L, Wingard DL, et al. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry 2002;59:131–6. [DOI] [PubMed] [Google Scholar]
- [15].Tamakoshi A, Ohno Y. JACC Study Group. Self-reported sleep duration as a predictor of all-cause mortality: results from the JACC study, Japan. Sleep 2004;27:51–4. [PubMed] [Google Scholar]
- [16].Tu X, Cai H, Gao Y-T, et al. Sleep duration and its correlates in middle-aged and elderly Chinese women: the Shanghai Women's Health Study. Sleep Med 2012;13:1138–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Ferrie JE, Shipley MJ, Akbaraly TN, et al. Change in sleep duration and cognitive function: findings from the Whitehall II Study. Sleep 2011;34:565–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Blackwell T, Yaffe K, Ancoli-Israel S, et al. Association of sleep characteristics and cognition in older community-dwelling men: the MrOS sleep study. Sleep 2011;34:1347–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Xu L, Jiang CQ, Lam TH, et al. Short or long sleep duration is associated with memory impairment in older Chinese: the Guangzhou Biobank Cohort Study. Sleep 2011;34:575–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Tworoger SS, Lee S, Schernhammer ES, et al. The association of self-reported sleep duration, difficulty sleeping, and snoring with cognitive function in older women. Alzheimer Dis Assoc Disord 2006;20:41–8. [DOI] [PubMed] [Google Scholar]
- [21].Ohayon MM, Vecchierini M-F. Daytime sleepiness and cognitive impairment in the elderly population. Arch Intern Med 2002;162:201–8. [DOI] [PubMed] [Google Scholar]
- [22].Blackwell T, Yaffe K, Ancoli-Israel S, et al. Poor sleep is associated with impaired cognitive function in older women: the study of osteoporotic fractures. J Gerontol A Biol Sci Med Sci 2006;61:405–10. [DOI] [PubMed] [Google Scholar]
- [23].Regestein QR, Friebely J, Shifren JL, et al. Self-reported sleep in postmenopausal women. Menopause 2004;11:198–207. [DOI] [PubMed] [Google Scholar]
- [24].Schmutte T, Harris S, Levin R, et al. The relation between cognitive functioning and self-reported sleep complaints in nondemented older adults: results from the Bronx aging study. Behav Sleep Med 2007;5:39–56. [DOI] [PubMed] [Google Scholar]
- [25].Faubel R, López-García E, Guallar-Castillón P, et al. Usual sleep duration and cognitive function in older adults in Spain. J Sleep Res 2009;18:427–35. [DOI] [PubMed] [Google Scholar]
- [26].Cohen-Zion M, Stepnowsky C, Marler null, et al. Changes in cognitive function associated with sleep disordered breathing in older people. J Am Geriatr Soc 2001;49:1622–7. [DOI] [PubMed] [Google Scholar]
- [27].Lim ASP, Yu L, Costa MD, et al. Increased fragmentation of rest-activity patterns is associated with a characteristic pattern of cognitive impairment in older individuals. Sleep 2012;35:633B–40B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Ball K, Berch DB, Helmers KF, et al. Effects of cognitive training interventions with older adults: a randomized controlled trial. JAMA 2002;288:2271–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Wilson RS, Bennett DA, Bienias JL, et al. Cognitive activity and incident AD in a population-based sample of older persons. Neurology 2002;59:1910–4. [DOI] [PubMed] [Google Scholar]
- [30].Potvin O, Lorrain D, Forget H, et al. Sleep quality and 1-year incident cognitive impairment in community-dwelling older adults. Sleep 2012;35:491–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Lim ASP, Kowgier M, Yu L, et al. Sleep fragmentation and the risk of incident Alzheimer's disease and cognitive decline in older persons. Sleep 2013;36:1027–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Yaffe K, Laffan AM, Harrison SL, et al. Sleep disordered breathing, hypoxia, and risk of mild cognitive impairment and dementia in older women. JAMA 2011;306:613–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Ju Y-ES, Lucey BP, Holtzman DM. Sleep and Alzheimer disease pathology–a bidirectional relationship. Nat Rev Neurol 2014;10:115–9. [DOI] [PMC free article] [PubMed] [Google Scholar]


