Abstract
Background:
Ultrasonic measurements of tongue thickness and condylar translation were recently introduced to predict difficult laryngoscopy in non-obstetric patients. We designed the present study to evaluate the performance of these two ultrasonic indicators in predicting difficult laryngoscopy in healthy parturients.
Methods:
The 119 parturients undergoing elective cesarean delivery were enrolled. Tongue thickness and condylar translation measured by ultrasonography, and Modified Mallampati test (MMT) score, inter-incisor distance (IID) and modified Cormack-Lehane grading system (MCLS) were measured and recorded before anesthesia. The primary outcome was difficult laryngoscopy defined as MCLS 3 or 4. The association between these variables and difficult laryngoscopy were analyzed by using multivariable logistic regression and receiver operating characteristic (ROC) curve.
Results:
Compared to the Easy Laryngoscopy Group, the tongue thickness was significantly higher and the condylar translation and IID were significantly lower in the Difficult Laryngoscopy Group. Tongue thickness and condylar translation but not MMT score and IID were proved to be two independent predictors for difficult laryngoscopy by multivariate logistic regression, with the odds ratios of 2.554 (95% confidence interval (CI), 1.715 to 3.802) and 0.457 (95% CI, 0.304 to 0.686). The area under the ROC curve to predict difficult laryngoscopy for tongue thickness was 0.93 (95% CI, 0.88–0.98) and for condylar translation was 0.77 (95% CI, 0.67–0.86), which were significantly higher than those for MMT score (0.67, 95% CI, 0.56–0.77) and IID (0.65, 95% CI, 0.55–0.76).
Conclusions:
Compared with MMT and IID, tongue thickness and condylar translation measured by ultrasonography appear to be better indicators for predicting difficult laryngoscopy in parturients.
The trial was registered at the Chinese Clinical Trial Registry (ChiCTR)(www.chictr.org), registration number ChiCTR-ICR-1800019991.
Keywords: difficult airway, parturient, ultrasonic indicators
1. Introduction
Preoperative evaluation is important to identify parturients at risk for difficult airway and failed intubation is an important cause of anesthetic-related maternal mortality.[1] However, a standardized evaluation method is still unclear, as published studies have indicated variable estimates of diagnostic test accuracy.[1] At present, the traditional methods based on body surface anatomies, such as modified Mallampati test (MMT) score, upper lip bite test, the inter-incisor distance (IID), thyromental distance (TMD), and modified Cormack-Lehane grading system (MCLS) are usually used to predict obstetrics difficult airway.[2] Honarmand et al[3] suggested that the ratio of height to thyromental distance may prove more useful than MMT, and the upper lip bite test for predicting difficult laryngoscopy in obstetric population. Hirmanpour et al[4] indicated that the difficult intubation was associated with TMD, increasing neck circumference (NC), the ratio of height to thyromental distance (RHTMD), and the ratio of neck circumference to thyromental distance (NC/TMD) in obstetric patients scheduled for caesarean delivery. However, using the preoperative airway predictive indices, in isolation and combination, usually fails to accurately predict difficult airway and the accuracy and precision of prediction also need to be further improved.
Ultrasound is a safe, fast, portable equipment providing the real-time dynamic image with strong repeatability.[5] It has been reported to be applied widely in airway management including awake intubation, evaluation of difficult airway, determining the location of the endotracheal tube and the position of the laryngeal mask, predicting successful extubation, positioning cricothyroid membrane and the tracheal incision, as well as evaluation of pulmonary abnormal state in recent years.[5] Hall et al[6] suggested that the increased tongue thickness is associated with both difficult laryngoscopy and difficult intubation. In addition, the translated condyle distance, which reflects the temporomandibular joint (TMJ) mobility, could be measured directly and accurately with ultrasonography.[7] A limited condylar translation has been reported to have the capacity for predicting difficult laryngoscopy in non-pregnant subjects.[7] Recently, ultrasonic measurements of tongue thickness and condylar translation have been proved to be successful to predict difficult laryngoscopy in non-obstetric patients. However, no study has investigated whether tongue thickness and condylar translation measured by ultrasonography can effectively predict difficult airway in pregnant women. Therefore we designed the present study to evaluate the performance of tongue thickness and condylar translation measured by ultrasonography in predicting difficult airway, with comparison of these 2 indicators with MMT score and IID, in parturients undergoing an elective cesarean delivery.
2. Materials and methods
This study was registered by Lili Xu on 2018/12/11 at the Chinese Clinical Trial Registry (ChiCTR) (www.chictr.org), with the registration number of ChiCTR-ICR-1800019991. It was approved by the Research Ethics Committee of Women's Hospital, Zhejiang University School of Medicine (20180120). All patients provided written informed consent. One hundred and twenty-nine parturients, American Society of Anesthesiologists (ASA) Class I-II, were included in the study. The inclusion criteria were parturients with the regular antenatal visit, age ≥18 years, monofetal pregnancy at ≥37 weeks gestation undergoing elective cesarean delivery. Exclusion criteria were parturients with a history of cardiovascular disease, hypertension, chronic obstructive pulmonary disease, arrhythmia, diabetes mellitus, cerebrovascular disease, maxillofacial deformity, oropharyngeal maxillofacial and cervical tumors, unstable cervical, fracture or spinal cord injury, loose and fallen fore-tooth, alcoholism or mental health disease, as well as severe vision, hearing or intellectual disabilities, language barrier, not able to communicate or willing to participate in the study. All parturients underwent elective cesarean delivery with an anticipated operative time of 1 h. This study was a prospective, randomized, double-blind trial employing modified Cormack-Lehane grading system (MCLS) to divide the parturients into 2 groups.
All parturients received a standardized combined spinal and epidural (CSE) anesthesia. In the operating room, standard monitoring included the electrocardiogram (ECG), heart rate (HR), pulse oxygen saturation (SpO2), systolic blood pressure (SBP), diastolic blood pressure (DBP) and mean arterial pressure (MAP). After oxygen was inhaled by the mask, CSE was performed by an attending anesthesiologist with the patient in the left lateral position. In brief, epidural puncture was performed with an 18-G Tuohy needle at the estimated L1–2 interspace and the method of loss-of-resistance-to-air technique (the air volume was not more than 2 ml) was used to identify the epidural space. An epidural catheter was then threaded 3 to 4 cm cephalad into the epidural space. 3 ml of 2% lidocaine was administered through the catheter. Thereafter, spinal puncture was performed a 27-G spinal needle with pencil tip. After certification of the spinal needle in the subarachnoid space, 3 ml of 15 mg ropivacaine was injected. Postoperative analgesia was conducted by patient-controlled epidural analgesia with 0.2% ropivacaine 100 ml.
The parturients received airway assessments including MMT score, IID, and MCLS at 1 hour before surgery by another anesthesiologist who was not involved in the anesthetic performance. The MMT score[8] (class 1, soft palate, uvula, fauces and pillars visible; class 2, soft palate, fauces and pillars visible; class 3, only soft palate visible; and class 4, soft palate not visible) was assessed by asking each patient to open the mouth maximally while seated and protrude the tongue without phonation. The IID[4] (distance between the upper and lower incisors at the midline) was measured by asking each patient to open the mouth as widely as possible. The difficulty of laryngoscopy was assessed with MCLS[8] (grade 1, full view of the glottis could be obtained; grade 2, only the posterior commissure of the glottis could be seen; grade 3, only the epiglottis could be seen; and grade 4, even the epiglottis could not be seen), the result was determined during Macintosh laryngoscopy after delivery by another senior anesthesiologist not involved in the anesthetic performance. Before Macintosh laryngoscopy, a bolus of intravenous midazolam 1.0 to 2.5 mg were given and a continuous infusion of remifentanil 0.1 to 0.6 μg/kg/ min was started and adjusted as needed.[7,8] The parturients remained responsive to commands, showed increasing difficulty in keeping the eyes open, and tolerated a forceful jaw thrust.[9] The parturients were given 1% tetracaine spraying on the base of the tongue and the throat and then asked to open their mouth to allow insertion of the laryngoscope.[10] If any significant gag or cough was observed, the laryngoscope was removed.[10] Parturients with MCLS 3 or 4 were assigned into Difficult Laryngoscopy Group (DL Group) and parturients with MCLS 1 or 2 were assigned into Easy Laryngoscopy Group (EL Group).
The ultrasound-guided difficult airway prediction measurements including tongue thickness and condylar translation were also performed at 1 hour before surgery by another senior anesthesiologist who was unknown of the anesthetic performance by using a KONICA MINOLTA ultrasound system (SONIMAGE HS1, KONICA MINOLTA Inc, Shanghai, China). The parturient were placed in a supine position with her head back to the olfactory position. Tongue thickness was performed using a low-frequency convex array ultrasound probe (4 MHz) placed under the chin of the median sagittal plane. Tongue thickness is defined as the maximum vertical dimension from the surface of the tongue to the subcutaneous skin and the normal valve is ≤6.1 cm[11] (Fig. 1). Then condylar translation was performed using a high-frequency linear array ultrasound probe (5–14 MHz) placed in front of the ear between the level of the external auditory canal and the nasal tip or philtrum. Condylar translation is defined as the distance of the condyle tip sliding and the normal valve is ≤1.1 cm[12] (Fig. 2). The primary end-points of the study were MCLS, tongue thickness and condylar translation and the secondary end-points were MMT score, IID, weight and body mass index (BMI).
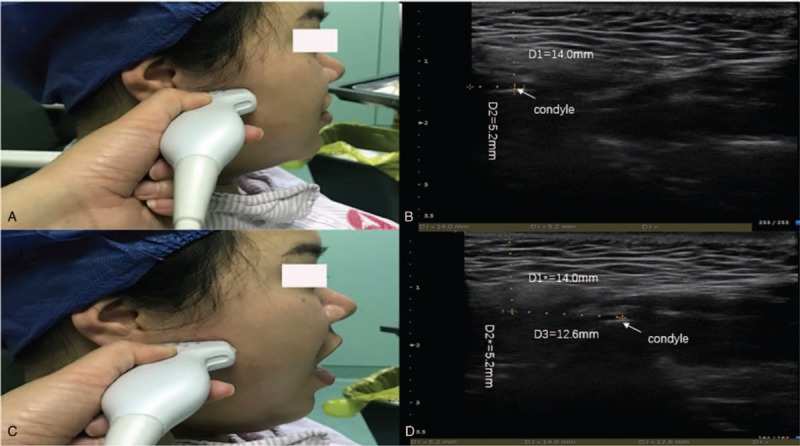
Figure 1.

Tongue thickness measured by ultrasonography. (A) The curved probe was placed under the chin in the median sagittal plane. (B) The probe was adjusted to obtain the entire tongue outline clearly in the screen. Tongue thickness was measured as the maximal vertical dimension from the tongue surface to the submental skin. The tongue thickness of one patient was 5.6 cm.
Figure 2.
The condylar translation measured by ultrasonography. The condylar translation measurement. Transducer position (A and C) and images (B and D) captured separately when the mouth was opened and closed. When the 2 images were compared, the mandibular condyle position could be found shifted from one point (crosshair marked “1” in B and D) to the other (the other crosshair in D). The condylar translation distance of one patient is 15.15 mm (D).
3. Statistical analysis
SPSS 23.0 (SPSS, Inc., Chicago, IL) was used for statistical analysis. After a pilot study in 10 parturients, we estimated there would be a mean difference of 3.1 cm in tongue thickness between groups with a standard deviation of 3.4 cm. With an alpha risk set at 5% and the power at 90%, a minimum of 27 parturients in each group was required to detect a difference. Numerical data between groups, including tongue thickness, condylar translation, and IID, were analyzed with the Student's t test. Nominal data, including MMT score, was analyzed by the χ2 test. Multivariate logistic regression analyses were performed to identify multivariate predictors of difficult laryngoscopy. A receiver operating characteristic (ROC) curve was used to describe the discrimination abilities of the predictive indicators. The area under the ROC curve (AUC) provides a global summary statistic of test accuracy, and guidelines suggest that 0.5<AUC≤0.7 represents low accuracy, 0.7<AUC≤0.9 represents moderate accuracy, and 0.9<AUC≤1.0 represents high accuracy. An AUC above 0.75 is considered as good. The 95% confidence interval (CI) was calculated, and statistical significance was accepted as P < .05. Their cut-off values of tongue thickness, condylar translation, MMT score, and IID were calculated according to AUC. The number of true-positive, true-negative, false-positive and false-negative, sensitivity, specificity, positive predictive value and negative predictive value of tongue thickness, condylar translation, MMT score, and IID were calculated by Student's t test according to their cut-off values. Correlations between continuous variable data or ordinal category data were analyzed with the Pearson correlation analysis or the Spearman correlation analysis as appropriate.
4. Results
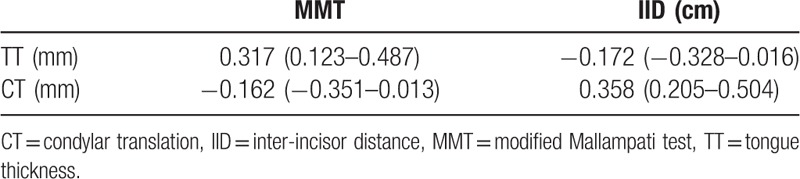
Ten parturients were excluded due to not meeting inclusion criteria, declined to participate or other reasons. Weight and BMI in the DL Group are significantly higher than those in the EL Group (P < .05) (Table 1). There were no significant differences in other patient characteristics between the 2 groups (P > .05) (Table 1). Compared to the EL Group, the tongue thickness was significantly higher (P < .05) and the condylar translation and IID were significantly lower (P < .05) in the DL Group (Table 2). There were significant differences in the MMT score between the two groups (P < .05) (Table 2). Tongue thickness and condylar translation but not MMT score and IID were proved to be 2 independent predictors for difficult laryngoscopy by multivariate logistic regression, with the odds ratios of 2.554 (95% confidence interval (CI), 1.715 to 3.802) and 0.457 (95% CI, 0.304 to 0.686) (Table 3). The regression equation for predicting difficult laryngoscopy in pregnant women is logit P = −46.540 + .938 tongue thickness −0.784 condylar translation. The area under the ROC curve to predict difficult laryngoscopy for tongue thickness (0.93, 95% CI, 0.88–0.98) and condylar translation (0.77, 95% CI, 0.67–0.86), which were significantly higher than those for MMT score (0.67, 95% CI, 0.56–0.77) and IID (0.65, 95% CI, 0.55–0.76) (Fig. 3). The sensitivity and specificity for tongue thickness and condylar translation are 85%, 91% and 70%, 81% and those for MMT score and IID are 73%, 61%, and 98%, 73%. Their cut-off values are 58.65 mm 11.05 mm, 3 and 4.75 cm (Table 4). The correlation coefficient of tongue thickness to MMT score and condylar translation to IID were 0.317 (95% CI, 0.123 to 0.487) and 0.358 (95% CI, 0.205 to 0.504) (Table 5).
Table 1.
Patient characteristics.
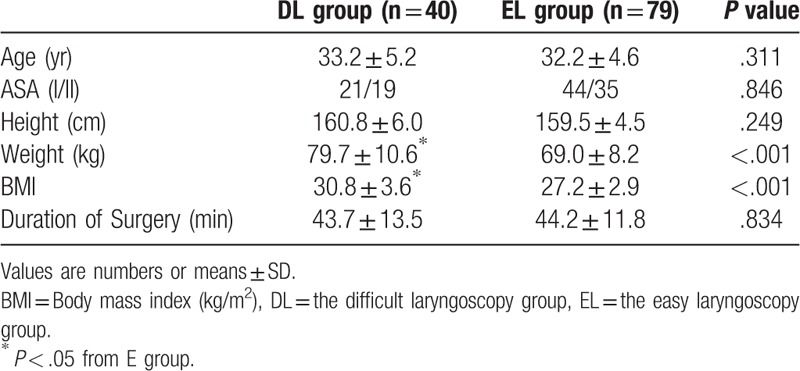
Table 2.
Variables for predicting difficult laryngoscopy.
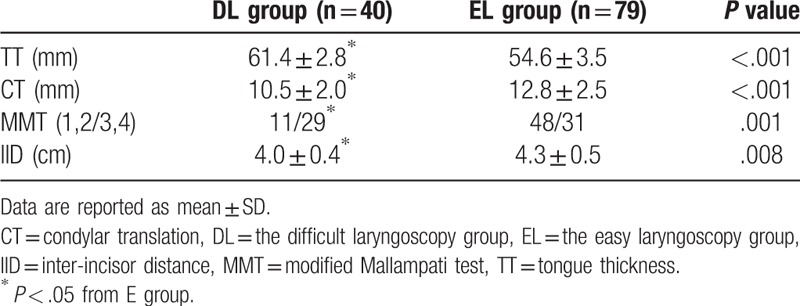
Table 3.
Multivariate logistic regression analyses identified the factors that were independently associated with difficult laryngoscopy.
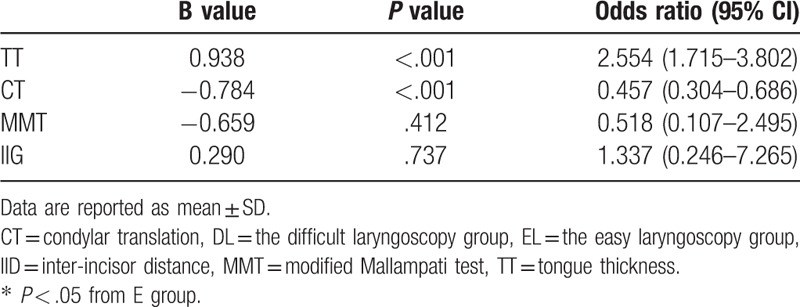
Figure 3.
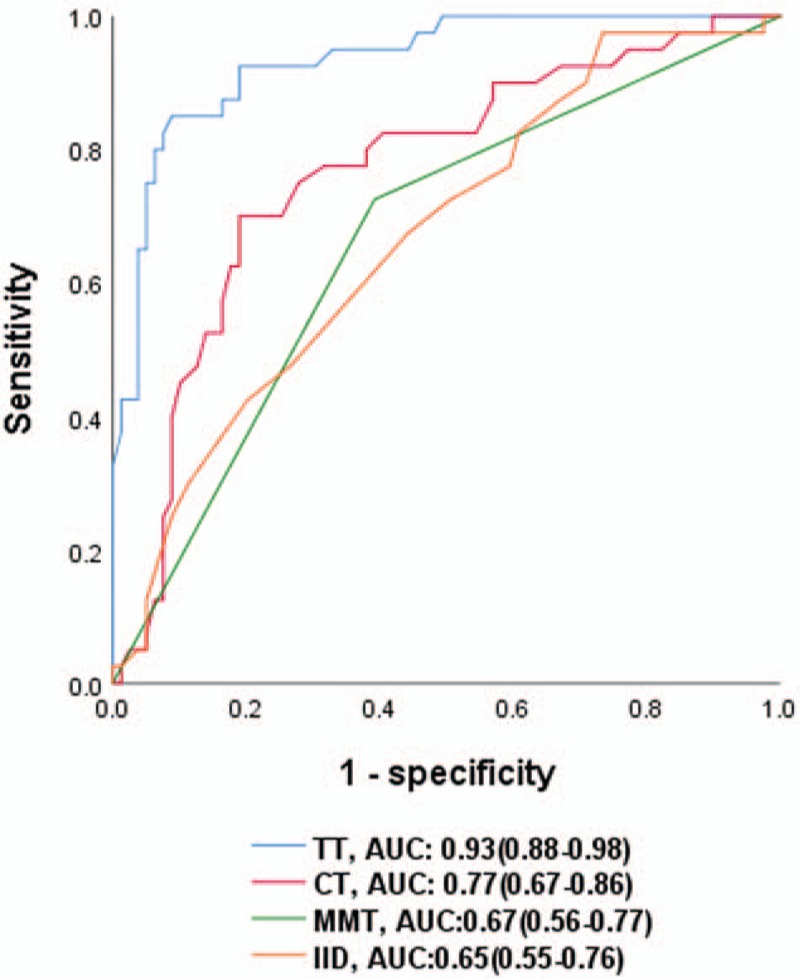
ROC curve. Receiver operating characteristic curve analysis of airway assessment tests and their areas under the curve (AUC; value and its 95% confidence interval) for predicting difficult laryngoscopy. TT: tongue thickness; CT: condylar translation; MMT: modified Mallampati test; IID: inter-incisor distance.
Table 4.
Evaluation of different diagnostic tests for difficult laryngoscopy.
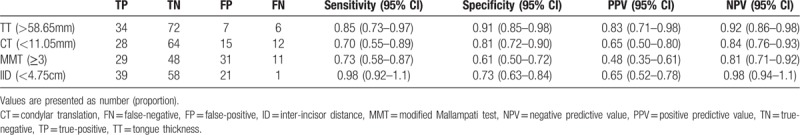
Table 5.
The correlation coefficient of tongue thickness or condylar translation to MMT or IID.
5. Discussion
Our study showed that tongue thickness and condylar translation but not MMT score and IID were proved to be 2 independent predictors for difficult laryngoscopy by multivariate logistic regression analyses, indicating that compared with MMT and IID, tongue thickness and condylar translation measured by ultrasonography were better ultrasonographic variables for predicting difficult laryngoscopy in parturients.
The management of difficult airway in obstetric patients is still a challenge facing by anesthesiologists and always warrants extra attention and care.[13] The key influence factors include gestation related anatomical and physiological changes in pregnancy, environment, training matters, unpredictability and the limitation of anesthesia preparation time.[14] Difficult airway remains to be one of the most common causes of anesthesia-related maternal complications including brain damage and death[1] in obstetric patients. Consequently, how to carry out timely, accurate and efficient airway evaluation is of particular importance, which can identify the difficult airway and avoid unexpected difficult airway management.[1]
At present, some traditional methods based on the body surface anatomy, including example, MMT score, upper lip bite test, IID, TMD, and MCLS, have been used to forecast the obstetric difficult airway.[2,15] In our previous study, we also successfully used MMT score, thyromental distance (TMD), IID, and atlanto-occipital extension for preoperative airway assessments in patients with ankylosing spondylitis.[6] Moreover, Raza et al[16] observed the frequency of change in MMT score during labor in hypertensive compared to normotensive parturients and found that MMT score showed a 2-fold increase in hypertensive compared to normotensive parturients during labor; requiring additional caution during airway management. Ahuja et al[17] evaluated the airway during and after labor in women with or without preeclampsia and found MMT score increased from the pre-labor to the post-labor period in both severely preeclamptic and normotensive pregnant women and those with prolonged labor are more susceptible to changes in airway dimensions. Our study determined the ability to predict difficult visualization of the larynx from the preoperative airway predictive indices and showed that parturients in the difficult laryngoscopy group had higher weight and BMI while lower IID and there were significant differences in the MMT score between the two groups. These anatomic indicators were not independently associated with difficult laryngoscopy by multivariate logistic regression, indicating that they have a certain correlation with the difficult laryngoscopy in parturients but their forecasting accuracy and the relations between anatomic indicators and difficult airway remain to be further improved.
However, the traditional methods based on body surface anatomies cannot provide dynamic airway management.[11] Visualized procedures like ultrasonography can provide the point of care real-time dynamic anatomical assessment of the airway in perioperative, emergency and critical care settings.[5] Furthermore, the ultrasonography has the advantages of noninvasive, convenient and inexpensive, which can bring new breakthroughs in the predition of difficult airway.[18] Nowadays, some preoperative ultrasonic indicators have been widely used to predict difficult airway. Ultrasonography can image a patient's tongue and accurately measure tongue thickness at the olfactory location in the ‘sniffing’ position.[18] This variable can reflect the internal characteristics of the anatomy of the upper airway and requires less patient collaboration than traditional techniques. Yao et al[11] found increased tongue thickness measured by ultrasonography (>6.1 cm) was an independent predictor for difficult tracheal intubation [sensitivity 0.75, 95% confidence interval (CI) 0.60 to 0.86; specificity 0.72, 95% CI, 0.70 to 0.74] with an area under the curve of 0.78 (95% CI, 0.77 to 0.80) for predicting difficult tracheal intubation, indicating tongue thickness measured by ultrasonography and its ratio to tongue chin distance present significant capacities to predict difficult tracheal intubation. In our study, tongue thickness was assessed using submental ultrasonography in the median sagittal plane before anesthesia. We showed that parturients in the difficult laryngoscopy group had higher tongue thickness measured by ultrasonography, which was proved to be an independent predictor for difficult laryngoscopy by multivariate logistic regression, with the odds ratios of 2.554 (95% CI, 1.715 to 3.802). The area under the ROC curve to predict difficult laryngoscopy for tongue thickness was 0.93 (95% CI, 0.88–0.98), which was significantly higher than those for MMT score (0.67, 95% CI, 0.56–0.77). The sensitivity and specificity for tongue thickness are 85%, 91% and those for MMT score are 73%, 61%. Their cut-off values are 58.65 mm and 3. Moreover, the correlation coefficient of tongue thickness to MMT score was 0.317 (95% CI, 0.123 to 0.487). These results suggested that compared with MMT score, tongue thickness measured by ultrasonography appears to be a more accurate indicator for difficult laryngoscopy and thus can be used to predict difficult airway in pregnant women.
TMJ is a complex joint and demonstrates morphological differences in various patients.[19] There are certain indirect or related TMJ mobility evaluations including the upper lip bite test, mandibular protrusion distance, and maximum interval of the condyle to the tragus.[19] Moreover, IID is the most commonly used method for assessing TMJ mobility, but it can only be used in an indirect or a vague manner.[19] The translated condyle distance can be measured directly and accurately with sonography through condylar translation measurements, which can reflect TMJ mobility and has become important and valuable in performing difficult airway evaluations.[19] Sahin et al[20] determined the reliability and the accuracy of condylar translation measurements for predicting difficult intubation and found condylar translation measured can be used for predicting difficult tracheal intubation in patients and the risk of difficult tracheal intubation may increase because of the decrease in protraction degrees and incisor gap. Yao et al[12] found that compared with indirect assessments, such as mouth opening and other parameters, mandibular condylar mobility, as assessed directly using sonography, was correlated with difficult laryngoscopy and demonstrated an independent and notably predictive property. Our study showed that the difficult laryngoscopy group had limited condylar translation measured by ultrasonography, which was proved to be an independent predictor for difficult laryngoscopy by multivariate logistic regression, with the odds ratios of 0.457 (95% CI, 0.304 to 0.686). The area under the ROC curve to predict difficult laryngoscopy for condylar translation was 0.77 (95% CI, 0.67–0.86), which were significantly higher than those for IID (0.65, 95% CI, 0.55–0.76). The sensitivity and specificity for condylar translation are 70%, 81% and those for IID are 98%, 73%. Their cut-off values are 11.05 mm and 4.75 cm. The correlation coefficient of condylar translation to IID was 0.358 (95% CI, 0.205 to 0.504). Our results suggested that compared with IID, condylar translation measured by ultrasonography is a more dependable index for difficult laryngoscopy and therefore can be applied to predict difficult airway in pregnant women.
This study has several limitations. First, there were only 119 parturients undergoing elective cesarean delivery in our study. We would recruit more pregnant women to determine the best ultrasonic technology and its cutoff points for prediction difficult laryngoscopy and avoid overestimating the predictive power of the tested indicators in our future study. Second, we did not choose special parturient such as pregnancy hypertension, preeclampsia or undergoing emergency cesarean delivery who are now considered to be at high risk of difficult laryngoscopy. Future studies are needed to investigate the feasibility and reliability of ultrasonic technology to predict difficult airway and evaluate the application value in those pregnant women. Third, this study only applied ultrasonic technology in perioperative parturients and accurately measured tongue thickness and condylar translation in predicting difficult laryngoscopy. Future studies will examine more ultrasound measurements such as anterior neck soft tissue thickness at hyoid bone (DSHB) and anterior commissure (DSAC) to predict obstetric difficult laryngoscopy. Fourth, in our study, parturients were given a bolus of midazolam and a continuous infusion of remifentanil when they experienced the evaluation of the larynx with direct laryngoscopy. Although the Cormack-Lehane grade may be poorer in the conscious patients than in unconscious patients, the results may reflect the diagnostic ability of the preoperative airway predictive indices to predict difficult direct laryngoscopy in some degree.[21]
This study demonstrates that tongue thickness and condylar translation measured by ultrasonography appear to be more accurate indicators for predicting difficult laryngoscopy in pregnant women as compared with MMT and IID. Combining tongue thickness with condylar translation can be used to predict difficult laryngoscopy in pregnant women and the regression equation for predicting difficult laryngoscopy is logit P = −46.540 + .938 tongue thickness −0.784 condylar translation. Future investigations should focus on exploring the reliability and the accuracy of tongue thickness and condylar translation and their relations with other ultrasonic prediction measurements.
Footnotes
Abbreviations: ASA = American Society of Anesthesiologists, AUC = area under the ROC curve, BMI = body mass index, CI = confidence interval, CSE = combined spinal and epidural, DBP = diastolic blood pressure, DL = difficult laryngoscopy, DSAC = anterior neck soft tissue thickness at anterior commissure, DSHB = anterior neck soft tissue thickness at hyoid bone, ECG = electrocardiogram, EL = easy laryngoscopy, HR = heart rate, IID = inter-incisor distance, MAP = mean arterial pressure, MCLS = modified Cormack-Lehane grading system, MMT = modified Mallampati test, NC = neck circumference, RHTMD = ratio of height to thyromental distance, ROC = receiver operating characteristic, SBP = systolic blood pressure, SpO2 = pulse oxygen saturation, TMD = thyromental distance, TMJ = temporomandibular joint.
How to cite this article: Xu L, Dai S, Sun L, Shen J, Lv C, Chen X. Evaluation of 2 ultrasonic indicators as predictors of difficult laryngoscopy in pregnant women: a prospective, double blinded study. Medicine. 2020;99:3(e18305).
LX and SD contributed to this work equally.
This study was approved by the Research Ethics Committee of Women's Hospital, Zhejiang University School of Medicine (20180120).
This study was supported the National Natural Science Foundation of China (81400929, 81471240, 81641042 and 81603545), the Innovative Talents Project of Zhejiang province (2016) and the Bureau of Chinese Medicine, Zhejiang, China (2018ZB065).
The authors have no conflict of interest.
References
- [1].Mushambi MC, Kinsella SM, Popat M, et al. Obstetric anaesthetists“ association and difficult airway society guidelines for the management of difficult and failed tracheal intubation in obstetrics. Anaesthesia 2015;70:1286–306. 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Jones K, Dobson A, Maguire S. Emergency airway management in obstetric general anaesthesia. Anaesthesia 2015;70:887–8. 2. [DOI] [PubMed] [Google Scholar]
- [3].Honarmand A, Safavi MR. Prediction of difficult laryngoscopy in obstetric patients scheduled for Caesarean delivery. Eur J Anaesthesiol 2008;25:714–20. [DOI] [PubMed] [Google Scholar]
- [4].Hirmanpour A, Safavi M, Honarmand A, et al. The predictive value of the ratio of neck circumference to thyromental distance in comparison with four predictive tests for difficult laryngoscopy in obstetric patients scheduled for caesarean delivery. Adv Biomed Res 2014;3:200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Kristensen MS, Teoh WH, Graumann O, et al. Ultrasonography for clinical decision-making and intervention in airway management: From the mouth to the lungs and pleurae. Insights Imaging 2014;5:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Hall EA, Showaihi I, Shofer FS, et al. Ultrasound evaluation of the airway in the ED: a feasibility study. Crit Ultrasound J 2018;10:3.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Chen HY, Wu SK, Lu CC, et al. Assessing the mobility of the mandibular condyle by sonography. Patient Prefer Adherence 2014;8:1419–25. 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Lili X, Zhiyong H, Jianjun S. A comparison of the GlideScope with the Macintosh laryngoscope for nasotracheal intubation in patients with ankylosing spondylitis. J Neurosurg Anesthesiol 2014;26:27–31. 6. [DOI] [PubMed] [Google Scholar]
- [9].Johnson KB, Swenson JD, Egan TD, et al. Midazolam and remifentanil by bolus injection for intensely stimulating procedures of briefduration: experience with awake laryngoscopy. Anesth Analg 2002;94:1241–3. [DOI] [PubMed] [Google Scholar]
- [10].Xu YC, Xue FS, Luo MP, et al. Median effective dose of remifentanil for awake laryngoscopy and intubation. Chin Med J (Engl) 2009;122:1507–12. [PubMed] [Google Scholar]
- [11].Yao W, Wang B. Can tongue thickness measured by ultrasonography predict difficult tracheal intubation? Br J Anaesth 2017;118:601–9. 7. [DOI] [PubMed] [Google Scholar]
- [12].Yao W, Zhou Y, Wang B, et al. Can mandibular condylar mobility sonography measurements predict difficult laryngoscopy? Anesth Analg 2017;124:800.8. [DOI] [PubMed] [Google Scholar]
- [13].Mushambi MC, Jaladi S. Airway management and training in obstetric anaesthesia. Curr Opin Anaesthesiol 2016;29:261.9. [DOI] [PubMed] [Google Scholar]
- [14].Scott-Brown S, Russell R. Video laryngoscopes and the obstetric airway. Int J Obstet Anesth 2015;24:137–46. 10. [DOI] [PubMed] [Google Scholar]
- [15].Xue FS, Sun C, Liu GP, et al. Predicting difficult laryngoscopy using ultrasound technique. J Crit Care 2016;34:131–2. [DOI] [PubMed] [Google Scholar]
- [16].Raza D, Ismail S. Change in Mallampati class during labor: hypertensive versus normotensive parturients. Acta Anaesthesiol Scand 2018;[Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- [17].Ahuja P, Jain D, Bhardwaj N, et al. Airway changes following labor and delivery in preeclamptic parturients, a prospective case control study. Int J Obstet Anesth 2018;33:17–22. [DOI] [PubMed] [Google Scholar]
- [18].Andruszkiewicz P, Wojtczak J, Sobczyk D, et al. Effectiveness and validity of sonographic upper airway evaluation to predict difficult laryngoscopy. J Ultrasound Med 2016;35:2243–52. [DOI] [PubMed] [Google Scholar]
- [19].Belda I, Ayuso MA, Sala-Blanch X, et al. A predictive test for difficult intubation in laryngeal microsurgery. Validation study. Rev Esp Anestesiol Reanim 2017;64:71–8. 15. [DOI] [PubMed] [Google Scholar]
- [20].Sahin SH, Yilmaz A, Gunday I, et al. Using temporomandibular joint mobility to predict difficult tracheal intubation. J Anesth 2011;25:457–61. 16. [DOI] [PubMed] [Google Scholar]
- [21].Gupta S, Macneil R, Bryson G. Laryngoscopy in conscious patients with remifentanil: how useful is an ”awake look"? J Clin Anesth 2012;24:19–24. [DOI] [PubMed] [Google Scholar]


