Abstract
Introduction:
The increase in the number of patients with prosthetic joints will entail a rise in the absolute number of infections associated with these procedures. Although less frequent, infections by Candida species are also expected to increase, and the clinical and surgical management of these cases is based on case reports and opinion of specialists. The objective of the present study was to review the available literature and describe the cases of prosthetic joint infection caused by Candida species in patients of the Institute of Orthopedics and Trauma of the University of São Paulo Faculty of Medicine Clinics Hospital (IOT-HCFMUSP) between 2007 and 2014.
Patient concerns:
Eleven patients were diagnosed with prosthetic joint infection due to Candida with mean age of 65 years. The most frequent comorbidities were heart disease and diabetes mellitus, and the main personal antecedent was previous bacterial infection in the prosthetic joint. At least one risk factor for fungal infection was present in 73% of the patients. There was no difference between the prevalence of infections caused by Candida albicans and non-albicans Candida species, and there was bacterial co-infection in 55% of the cases.
Diagnosis:
For building up the case series, patients with cultures of bone and joint specimens that were positive for Candida species and had a clinical diagnosis of prosthetic joint infection were included in the case series.
Interventions:
Surgical debridement with removal of the prosthesis was the most frequently used surgical approach (45%). All patients were treated with monotherapy, and the most frequently used antifungal agent was fluconazole. The total duration of antifungal therapy was 6 months in 73% of the cases.
Outcomes:
After the initial management, 73% of the patients achieved clinical remission.
Conclusion:
The most indicated initial management was debridement with removal of the prosthesis, and the most used treatment regimen was fluconazole monotherapy. The most prevalent treatment duration was 6 months. The initial management led to a favorable outcome in 73% of the cases.
Descriptors:
Prosthetic joint infection, Candida, treatment, and diagnosis.
Keywords: Candida, diagnosis, prosthetic joint infection, treatment
1. Introduction
The number of patients with joint prostheses has been increasing in recent decades, and 500,000 primary hip arthroplasties and over 3 million knee arthroplasties will be performed by 2030.[1] Infection is expected to occur in 1% to 5% of these procedures, with the most frequently causative agents being Gram-positive bacteria, followed by Gram-negative bacteria and fungi.2,3
Fungal infections probably account for 0.6% to 1.4% of the total number of infected arthroplasties,4,5,6,7,8 with Candida species being the most frequent agents.9,10,11 Because of the low occurrence of infections caused by fungal agents, there are no published clinical trials that address the questions regarding the clinical and surgical management of these cases. The main international guidelines concerning this topic are based on case reports and opinion of specialists.12,13,14,15
Therefore, case reports of infections caused by fungal agents, especially by Candida species, play a very important role in improving the understanding of the affected population and of the initially adopted approaches that effectively lead to remission or cure of infection.
2. Method
This research is registered under protocol number 50713015.2.0000.0068 that can be found in www.plataformabrasil.saude.gov.br.
This is a retrospective, single-center, non-consecutive case series report. The identification of the cases of infection caused by Candida species in prosthetic joints in patients of the Institute of Orthopedics and Trauma of the University of São Paulo Faculty of Medicine Clinics Hospital (IOT-HCFMUSP) was performed by searching and intersecting the following data from electronic databases: bone and joint specimen cultures positive for Candida species between 2007 and 2014, patients who underwent an arthroplasty between 2006 and 2014, and patients with a diagnosis of postoperative infection between 2006 and 2014 (ICD 10: T84.1 and T84.5).
The study included patients with available cultures of tissues of the bone-joint system that were aseptically collected, were positive for Candida species, and who had a diagnosis of prosthetic joint infection made by the medical team. Patients have provided informed consent for publication of the case.
After selection of patients, their medical records were evaluated searching for predefined data such as gender, age, comorbidities, risk factor for fungal infection, clinical and surgical aspects, and antifungal treatment. The considered outcomes were remission, when there were no signs and symptoms of infection, and relapse, when there were.
To detect the cases reported in the literature, a search was performed in the electronic databases PubMed, Embase, Web of Knowledge, and LILACS from the earliest records of the databases until March 31, 2016, using the terms (“prosthesis related infection” OR “shoulder infection” OR “elbow infection” OR “knee infection” OR “hip infection” OR “ankle infection”) AND (“mycosis” OR “candida”).
3. Results
Eleven cases of infection caused by Candida species were detected in the prosthetic joints of patients of the IOT-HCFMUSP between 2007 and 2014. Of these, 6 patients were women (55%) and 5 patients were men (45%). The mean age was 65.1 years (range, 52–85 years) (Table 1).
Table 1.
Demographic data, comorbidities, personal antecedent, signs and symptoms, and laboratorial tests of patients with prosthesis related infections due to Candida species.
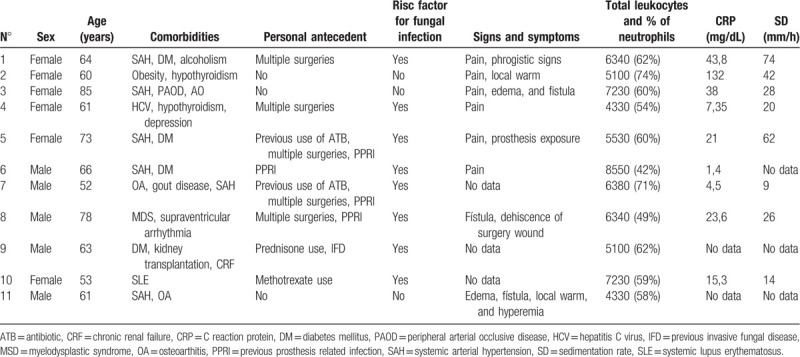
The comorbidities and personal clinical antecedents described in Table 1 show that the most prevalent comorbidity was heart disease (7/11), followed by diabetes mellitus (4/11). The most prevalent clinical antecedents were previous bacterial infections in the concerned prosthetic joint and multiple procedures in the joint, with 4 occurrences each. At least one risk factor for fungal infection was present in 73% of the cases.
Six patients had hip prostheses and five patients had knee prostheses, and the primary indication for joint prosthesis implantation was osteoarthritis (Table 2).
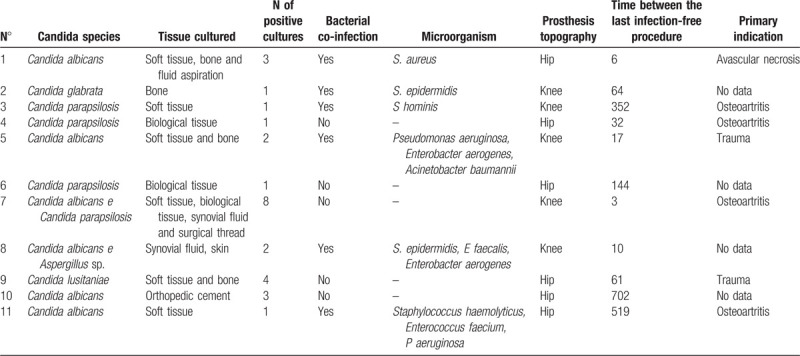
Table 2.
Microbiological and prosthesis related aspects of patients with prosthesis related infections due to Candida species.
The signs and symptoms and the nonspecific laboratory tests are described in detail in Table 1. The analysis of these data showed that pain and fistula formation were the most reported clinical findings and that no patient had leukocytosis (mean C-reactive protein level [CRP] of 31.2 mg/dL and mean sedimentation rate [SR] of 34.8 mm/h).
Table 2 shows that Candida albicans and non-albicans Candida infections were equally prevalent. There was an association between the 2 Candida species in 1 patient (patient no. 7) and between Candida and Aspergillus in another patient (patient no. 8).
Bacterial co-infection was detected in 6 cases (55%). It was caused by Gram-positive cocci in 3 cases and by an association between Gram-negative bacilli and Gram-positive cocci in another 3 cases.
The mean time between the last infection-free procedure and diagnosis of infection caused by a Candida species was 173.7 weeks (median, 61 weeks).
The most indicated initial approach was surgical debridement with removal of the prosthesis (5/11), followed by one-stage exchange (4/11) (Table 3). The time between debridement and two-stage exchange arthroplasty was 5.3 weeks. In the latter case, an antifungal agent was not added to the orthopedic cement used in the surgical procedure.
Table 3.
Initial management and antifungal treatment of patients with prosthesis related infections due to Candida species.
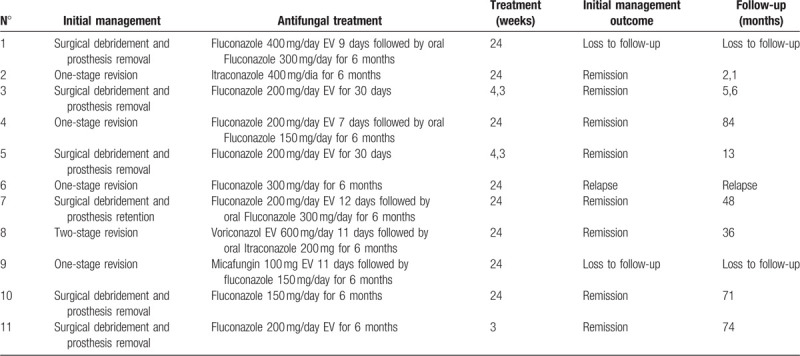
Monotherapy was used in all cases, and an intravenous antifungal agent was used in 8 patients; in 5 of these cases, there was a subsequent switch to an orally administered antifungal agent to end the treatment. The most frequently used antifungal agent was fluconazole, at doses that varied between 150 and 400 mg/day. The detailed description of the antifungal agents is shown in Table 3.
The treatment duration was 24 weeks for 8 patients and varied between 3 and 4.3 weeks for the other 3 patients.
The outcomes of the described cases are shown in Table 3, where it can be seen that the initial management led to remission in 8 cases (73%). There were 2 losses to follow-up and one recurrence with indication for surgical debridement and prosthesis removal. Amputation to control the infection was necessary in 1 patient (patient no. 5). Patient no. 8 had an infection by Pseudomonas aeruginosa in the same area after treatment of the infection caused by C albicans and Aspergillus spp. and was given suppressive chronic treatment with ciprofloxacin. Patient no. 11 had an infection by P aeruginosa, Acinetobacter baumannii, Staphylococcus haemolyticus, and Bacteroides in the same area after treatment of the infection caused by C albicans; the treatment in this case consisted of serial surgical debridement and specific antibacterial treatment, which resulted in remission of the infection.
The follow-up time of patients in remission was more than 1 year in 6 cases.
After literature review, 45 published articles were included and most of them were case reports or case series. A total of 94 cases of fungal infection were selected and analyzed.
4. Discussion
The majority of cases of prosthetic joint infection caused by Candida species occurred in women, which is in line with other published series7,10,16,17; however, there are also reports of male sex predominance.8,9,18
The mean age at diagnosis was 63 years, a result that is similar to those obtained in other studies8,10; however, there are reports of diagnosis being made in higher age groups also.7,11,16,17,18
The risk factors for fungal infection are the following: diabetes mellitus, chronic kidney disease, cancer, use of immunosuppressants, rheumatic diseases, prolonged use of antimicrobial agents, multiple procedures, and previous prosthetic joint infection.10,15,19
At least one risk factor was present in 73% of the patients included in this series. This percentage was also high in the largest published reports (varying between 69% and 100% of the patients).7,8,10,16,18
Pain was reported by 75% of the patients in this series, and edema was exhibited by 25% of them. Wang et al[17] and Azzam et al[10] reported that these symptoms were present in all patients included in their studies. Fistula formation occurred in 37.5% of the patients in the present series and has been described by other authors as varying between 57% and 80%.7,17,20
The patients did not have leukocytosis, which is in accordance with data published by other authors.11,18 The mean CRP level was 31.2 mg/dL, and it was within the normal range in 2 cases. However, Hwang et al[11] and Azzam et al[10] reported means of 4.3 and 17.5 mg/dL, respectively, and the occurrence of normal values in some patients. Normal results were also reported by Wang et al.[17] The mean SR in the present study was 34.8 mm/h, and it was within the normal range in 2 cases. However, Hwang et al[11] and Azzam et al[10] reported means of 39 and 54 mm/h with some patients also having normal values.
In the present series, C albicans and non-albicans Candida were equally prevalent. Klatte et al[18] and Anagnostakos et al[9] also reported case series with equal distribution of these infections; however, there is a divergence between studies that report the predominance of either C albicans 8,10,16 or non-albicans Candida.11,17
Bacterial co-infection occurred in 55% of the cases in this series. This percentage is similar to that reported by Ueng et al.[8] In the latter, all cases were caused by Gram-positive cocci, whereas associated Gram-negative bacilli were detected in half of the cases of the present study. Hwang et al[11] and Azzam et al[10] reported the presence of co-infection in 19% and 16% of the cases, respectively.
Infections occurred up to 1 year after the last infection-free procedure in 27% of the cases, which is in line with other publications.8,18 By contrast, all cases in the series published by Dutronc et al[7] were diagnosed up to 1 year after the placement of the prosthesis. Time between the implantation of the prosthesis and diagnosis of infection may be related to the pathophysiological mechanism of infection acquisition.
Hip prosthesis infection was the most prevalent in the present series, a finding that was also shown in studies published by other authors9,16,18; however, there are reports which show that the knee was the most affected area.7,8,10
Removal of the prosthesis with subsequent revision surgery is the procedure of choice of some authors,8,9,10,11 with remission rates varying between 89% and 100%8,11,17; however, Klatte et al[18] reported that one-stage revision had a remission rate of 90% and could be considered as a safe procedure that resulted in remission.
In the present case series, there were 4 cases of remission and 1 loss to follow-up among the 5 patients who underwent surgical debridement and prosthesis removal. There were 2 cases of remission, 1 case of recurrence, and 1 loss to follow-up among the 4 patients who underwent one-stage revision. The patients who underwent two-stage revision and surgical debridement with prosthesis retention also achieved clinical remission. The patient who underwent debridement and prosthesis retention received the diagnosis of prosthetic joint infection 3 weeks after the primary arthroplasty, which allowed an attempt to treat the infection while retaining the prosthesis.
The combined use of antifungal agents in the treatment of these infections has been widely described7,16,18,21,22,23,24,25,26,27,28,29,30,31,32; however, this strategy was not used in the present series.
According to Pappas et al,[13] the use of fluconazole and echinocandins is strongly recommended for the treatment of joint infections caused by Candida species, whereas Parvizi et al[12] stated that fluconazole or any amphotericin B product is indicated for this type of infection.
All patients included in this series received azoles for the treatment of the infection caused by Candida species. The use of both azoles7,8,9,16,17,18,23,24,25,27,32,33,34,35,36,37,38,39,40,41,42,43,44 and amphotericin B22,26,28,29,30,31,45,46,47,48,49,50,51,52,53,54 is widely described in the literature. The publications that report amphotericin B as the primary antifungal agent are mostly from the 1980s and 1990s, whereas those that report the use of azoles have been published since the 2000s.
The treatment duration for fungal infections related to prosthetic joints should vary according to the classification of the infections as acute or chronic, but the current guidelines do not address this issue. Pappas et al[13] suggest a treatment duration between 6 and 12 months in cases of chronic osteomyelitis and of 6 weeks in cases of septic arthritis, whereas Parvizi et al[12] proposed a treatment duration of 6 weeks.
Ueng et al[8] found a positive association between a longer use of antifungal agents and treatment success. In the present series, 8 patients received treatment for 6 months and only 1 of them experienced recurrence of the infection, whereas the 3 patients who were treated between 3 and 4.3 weeks had the prosthesis removed and progressed to remission.
Remission was achieved in 73% of the cases of the present series. Two patients were lost to follow-up, and two cases had a follow-up of <1 year. The rate of remission after the initial management described in the main published case series varied between 0% and 100%.11,16,17
Amputation to control the infection was necessary in 1 case of this case series. Dutronc et al[7] reported the need for amputation in 16% of the cases, and sporadic cases have also been reported in the literature.37,50
The ideal follow-up time to determine the cure of joint infections has not been well defined in the literature. In the present case series, 6 cases had a follow-up time of more than 1 year and 2 cases were followed for a shorter period. Follow-up times longer8,11,17,18 and shorter9,16 than 1 year have been reported in the literature.
This is one of the largest single-center case series of prosthetic joint infection due to Candida species and the limitations of these study are: the initial surgical approach and antifungal and dose selection varied among cases, follow up time were <1 year in two cases and there were two losses of follow-up.
Considering that prosthetic joint infection due to Candida species are rare, prospective multicenter studies are needed to provide better evidence to support clinical decisions.
Author contributions
Conceptualization: Eduardo Schincariol Saconi, Vladimir Cordeiro de Carvalho, Priscila Rosalba Domingos de Oliveira, Ana Lúcia Lei Munhoz Lima.
Data curation: Eduardo Schincariol Saconi.
Formal analysis: Eduardo Schincariol Saconi.
Methodology: Eduardo Schincariol Saconi.
Supervision: Ana Lúcia Lei Munhoz Lima.
Writing – original draft: Eduardo Schincariol Saconi.
Writing – review & editing: Vladimir Cordeiro de Carvalho, Priscila Rosalba Domingos de Oliveira, Ana Lúcia Lei Munhoz Lima.
Eduardo Schincariol Saconi: 0000-0002-0584-4347.
Footnotes
Abbreviations: ATB = antibiotic, CRF = chronic renal failure, CRP = C reaction protein, DM = diabetes mellitus, HCV = hepatitis C virus, IFD = previous invasive fungal disease, IOT-HCFMUSP = Institute of Orthopedics and Trauma of the University of São Paulo Faculty of Medicine Clinics Hospital, MSD = myelodysplastic syndrome, OA = osteoarthritis, PAOD = peripheral arterial occlusive disease, PPRI = previous prosthesis related infection, SAH = systemic arterial hypertension, SD = sedimentation rate, SLE = systemic lupus erythematosus.
How to cite this article: Saconi ES, Carvalho VC, Oliveira PR, Lima AL. Prosthetic joint infection due to Candida species: case series and review of literature. Medicine. 2020;99:15(e19735).
The authors have no conflicts of interest to disclose.
References
- [1]. Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip arthroplasty in the United States from 2005 to 2030. J Bone Jt Surg Am 2007;89:780–5. [DOI] [PubMed] [Google Scholar]
- [2]. Lima AL, Oliveira PR, Carvalho VC, et al. Periprosthetic joint infections. Interdiscip Perspect Infect Dis 2013;2013: doi: 10.1155/2013/542796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3]. Carvalho VC. Osteomielite por bacilos Gram-negativos: estudo comparativo das características clínico-microbiológicas e fatores de risco com as infecções por Staphylococcus aureus[tese]. São Paulo: Faculdade de Medicina da Universidade de São Paulo; 2013. [Google Scholar]
- [4]. Springer J, Chatterjee S. Candida albicans prosthetic shoulder joint infection in a patient with rheumatoid arthritis on multidrug therapy. J Clin Rheumatol 2012;18:52–3. [DOI] [PubMed] [Google Scholar]
- [5]. Radha S, Siddiqui B, Senevirathana S, et al. Candida albicans infection of a reverse-polarity shouder replacement in a patient with rheumatoid arthritis treated with etanercept. J Clin Rheumatol 2012;18:323. [DOI] [PubMed] [Google Scholar]
- [6]. Kojic E, Darouiche R. Candida infections of medical devices. Clin Microbiol Rev 2004;17:255–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7]. Dutronc H, Dauchy FA, Cazanave C, et al. Candida prosthetic infections: case series and literature review. Scand J Infect Dis 2010;42:890–5. [DOI] [PubMed] [Google Scholar]
- [8]. Ueng AWN, Lee C, Hu C, et al. What is the success of treatment of hip and knee candidal periprosthetic joint infection. Clin Orthop Relat Res 2013;471:3002–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9]. Anagnostakos K, Kelm J, Schmitt E, et al. Fungal periprosthetic hip and knee joint infections clinical experience with a 2-stage treatment protocol. J Arthroplasty 2012;27:293–8. [DOI] [PubMed] [Google Scholar]
- [10]. Azzam K, Parvizi J, Jungkind D, et al. Microbiological, clinical, and surgical features of fungal prosthetic joint infections: a multi-institutional experience. J Bone Jt Surg Am 2009;91: Suppl 6: 142–9. [DOI] [PubMed] [Google Scholar]
- [11]. Hwang BH, Yoon JY, Nam CH, et al. Fungal peri-prosthetic joint infection after primary total knee replacement. J Bone Joint Surg Br 2012;94:656–9. [DOI] [PubMed] [Google Scholar]
- [12]. Parvizi J, Gehrke T, Chen AF. Proceedings of the international consensus meeting on periprosthetic joint infection. Bone Joint J 2013;95-B:1450–2. [DOI] [PubMed] [Google Scholar]
- [13]. Pappas PG, Kauffman CA, Andes DR, et al. Clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis 2016;62:409–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14]. Osmon DR, Berbari EF, Berendt AR, et al. Diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis 2013;56:e1–25. [DOI] [PubMed] [Google Scholar]
- [15]. Gebauer M, Frommelt L, Acham P, et al. Management of fungal or atypical periprosthetic joint infections. J Orthop Res 2014;32:s147–51. [DOI] [PubMed] [Google Scholar]
- [16]. García-Oltra E, García-Ramiro S, Pastor JCM, et al. Infección por Candida spp. sobre prótesis articulares. Rev Esp Quim 2011;24:31–41. [PubMed] [Google Scholar]
- [17]. Wang Q-J, Shen H, Zhang X-L, et al. Staged reimplantation for the treatment of fungal peri-prosthetic joint infection following primary total knee arthroplasty. Orthop Traumatol Surg Res 2015;101:151–6. [DOI] [PubMed] [Google Scholar]
- [18]. Klatte TO, Junghans K, Al-Khateeb H, et al. Single-stage revision for peri-prosthetic shoulder infection: outcomes and results. Bone Jt J 2013;95B:391–5. [DOI] [PubMed] [Google Scholar]
- [19]. Kuiper J, van den Bekeron P, van der Stappen J, et al. 2-stage revision recommended for treatment of hip and knee prosthetic joint infections. Acta Orthop 2013;84:517–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20]. Schoof B, Jakobs O, Schmidl S, et al. Fungal periprosthetic joint infection of the hip: a systematic review. Orthop Rev (Pavia) 2015;7: doi:10.4081/or.2015.5748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21]. MacGregor RR, Schimmer BM, Steinberg ME. Results of combined amphotericin B-5-fluorcytosine therapy for prosthetic knee joint infected with Candida parapsilosis. J Rheumatol 1979;6:451–5. [PubMed] [Google Scholar]
- [22]. Younkin S, Evarts M, Steigbigel RT. Candida parapsilosis infection of a total hip-joint replacement: successful reimplantation after treatment with amphotericin B and 5-fluorocytosine. J Bone Jt Surg 1984;66:142–3. [PubMed] [Google Scholar]
- [23]. Bartalesi F, Fallani S, Salomoni E, et al. Candida glabrata prosthetic hip infection. Am J Orthop (Belle Mead NJ) 2012;41:500–5. [PubMed] [Google Scholar]
- [24]. Bland CM, Thomas S. Micafungin plus fluconazole in an infected knee with retained hardware due to candida albicans. Ann Pharmacother 2009;43:528–31. [DOI] [PubMed] [Google Scholar]
- [25]. Dumaine V, Eyrolle L, Baixench M, et al. Successful reatment of prosthetic knee Candida glabrata infection with caspofungin combined with flucitosine. Int J Antimicrob Agents 2008;31:398. [DOI] [PubMed] [Google Scholar]
- [26]. Ramamohan N, Zeineh N, Grigoris P, et al. Candida glabrata infection after total hip arthroplasty. J Infect 2001;42:74–6. [DOI] [PubMed] [Google Scholar]
- [27]. Nayeri F, Cameron R, Chryssanthou E, et al. Candida glabrata prosthesis infection following pyelonephritis and septicaemia. Scand J Infect Dis 1997;29:635–8. [DOI] [PubMed] [Google Scholar]
- [28]. Hennessy MJ. Infection of a total knee arthroplasty by Candida parapsilosis. A case report of successful treatment by joint reimplantation with a literature review. Am J KneeSurg 1996;9:133–6. [PubMed] [Google Scholar]
- [29]. Paul J, White SH, Nicholls KM, et al. Prosthetic joint infection due to Candida parapsilosis in the UK: case report and literature review. Eur J Clin Microbiol Infect Dis 1992;11:847–9. [DOI] [PubMed] [Google Scholar]
- [30]. Selmon GPF, Slater RNS, Shepperd JAN, et al. Successful 1-stage exchange total knee arthroplasty for fungal infection. J Arthroplasty 1998;13:114–5. [DOI] [PubMed] [Google Scholar]
- [31]. Koch AE. Candida albicans infection of a prosthetic knee replacement: a report and review of the literature. J Rheumatol 1988;15:362–5. [PubMed] [Google Scholar]
- [32]. Jenny JY, Goukodadja O, Boeri C, et al. May one-stage exchange for Candida albicans peri-prosthetic infection be successful? Orthop Traumatol Surg Res 2016;102:127–9. [DOI] [PubMed] [Google Scholar]
- [33]. Wiwattanawarang N. Fungal periprosthetic joint infection after total knee arthroplasty. J Med Assoc Thai 2014;97:1358–63. [PubMed] [Google Scholar]
- [34]. Deelstra JJ, Neut D, Jutte PC. Successful treatment of Candida Albicans-infected total hip prosthesis with staged procedure using an antifungal-loaded cement spacer. J Arthroplasty 2013;28: doi:10.1016/j.arth.2012.04.034. [DOI] [PubMed] [Google Scholar]
- [35]. Graw B, Woolson S, Huddleston JI. Candida infection in total knee arthroplasty with successful reimplantation. J Knee Surg 2010;23:169–74. [DOI] [PubMed] [Google Scholar]
- [36]. Kelesidis T, Tsiodras S. Candida albicans prosthetic hip infection in elderly patients: is fluconazole monotherapy an option? Scand J Infect Dis 2010;42:12–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37]. Gaston G, Ogden J. Candida glabrata periprosthetic infection: a case report and literature review. J Arthroplasty 2004;19:927–30. [DOI] [PubMed] [Google Scholar]
- [38]. Phelan DM, Osmon DR, Keating MR, et al. Delayed reimplantation arthroplasty for candidal prosthetic joint infection: a report of 4 cases and review of the literature. Clin Infect Dis 2002;34:930–8. [DOI] [PubMed] [Google Scholar]
- [39]. Bruce S, Kerry RM, Norman P, et al. Fluconazole-impregnated beads in the management of fungal infection of prosthetic joints. J Bone Joint Surg Br 2001;83:183–4. [DOI] [PubMed] [Google Scholar]
- [40]. Wada M, Baba H, Imura S. Prosthetic knee Candida parapsilosis infection. J Arthroplasty 1998;13:479–82. [DOI] [PubMed] [Google Scholar]
- [41]. Cushing RR, Fulgenzi WR. Synovial fluid levels of fluconazole in a patient with Candida parapsilosis pristhetic joint infection who had an excellent clinical response. J Arthroplasty 1997;12:950–1. [DOI] [PubMed] [Google Scholar]
- [42]. Fukasawa N, Shirakura K. Candida arthritis after total knee arthroplasty - a case of successful treatment without prosthesis removal. Acta Orthop Scand 1997;68:302–9. [DOI] [PubMed] [Google Scholar]
- [43]. Fabry K, Verheyden F, Nelen G. Infection of a total knee prosthesis by candida glabrata: a case report. Acta Orthop Belg 2005;71:119–21. [PubMed] [Google Scholar]
- [44]. Reddy KJ, Shah JD, Kale RV, et al. Fungal prosthetic joint infection after total knee arthroplasty. Indian J Orthop 2013;47:526–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45]. Goodman JS, Seibert DG, Reahl GE, et al. Fungal infection of prosthetic joints: a report of two cases. J Rheumatol 1983;10:494–5. [PubMed] [Google Scholar]
- [46]. Evans RP, Nelson CL. Staged reimplantation of a total hip prosthesis after infection with Candida albicans. J Bone Jt Surg 1990;72:1551–3. [PubMed] [Google Scholar]
- [47]. Lidder S, Tasleem A, Masterson S, et al. Candida tropicalis: diagnostic dilemmas for an unusual prosthetic hip infection. J R Army Med Corps 2013;159:123–5. [DOI] [PubMed] [Google Scholar]
- [48]. Lazzarini L, Manfrin V, De Lalla F. Candidal prosthetic hip infection in a patient with previous candidal septic arthritis. J Arthroplasty 2004;19:248–52. [DOI] [PubMed] [Google Scholar]
- [49]. Wymanm J, McGough R, Limbird R. Fungal infection of a total knee prosthesis: successful treatment using articulating cement spacers and staged reimplantation. Orthopedics 2002;25:1391–4. [DOI] [PubMed] [Google Scholar]
- [50]. Tunkel AR, Thomas CY, Wispelwey B. Candida prosthetic arthritis: report of a case treated with fluconazole and review of the literature. Am J Med 1993;94:100–3. [DOI] [PubMed] [Google Scholar]
- [51]. Brooks DH, Pupparo F. Successful salvage of a primary total knee arthroplsty infected with Candida parapsilosis. J Arthroplasty 1996;13:707–12. [DOI] [PubMed] [Google Scholar]
- [52]. Lambertus M, Thordarson D, Bidwell Goetz M. Fungal prosthetic arthritis: presentation of two cases and review of the literature. Rev Infect Dis 1988;10:1038–43. [DOI] [PubMed] [Google Scholar]
- [53]. Levine M, Rehm SJ, Wilde AH. Infection with Candida albicans of a total knee arthroplasty. Case report and review of the literature. Clin Orthop Relat Res 1988. 235–9. [PubMed] [Google Scholar]
- [54]. Lim EVA, Stern PJ. Candida infection after implant arthroplasty. A case report. J Bone Jt Surg A 1986;68:143–5. [PubMed] [Google Scholar]


