Abstract
Background:
The Trachway Videolight Intubating Stylet is a video-assisted system with a rigid but malleable intubating stylet that facilitates endotracheal intubation. Minimizing cervical spine movement with manual in-line stabilization is essential for patients with cervical spine injuries such as multiple trauma. However, the intubation time of the Trachway Videolight Intubating Stylet and complications associated with intubation in patients with manual in-line stabilization in the neutral-head and head-lift positions remain unclear.
Methods:
Patients (20–80 years old) who were scheduled to undergo surgery that required general anesthesia with tracheal intubation were randomly allocated to either a neutral-head (n = 62) or a head-lift position (n = 62) group. Manual in-line stabilization was performed to limit cervical spine mobility. We aimed to evaluate orotracheal intubation time and success rate in these 2 positions with the Trachway Videolight Intubating Stylet.
Results:
Intubation was faster in the head-lift than in the neutral-head position (20 ± 10 and 25 ± 13 seconds, respectively, P = .000); intubation was equally successful in the 2 positions (96.8% vs 96.8%). Responses to intubation did not differ between positions (heart rate, P = .142; visual analog scale scores for throat soreness, P = .54). The only significant predictor of intubation time was the body mass index in the head-lift position group (P = .005).
Conclusions:
Intubation using the Trachway Videolight Intubating Stylet with manual in-line stabilization is faster in the head-lift position, and therefore preferable. However, if the head-lift position is not suitable, the neutral-head position is a sensible alternative, with comparable intubation success rate, heart rate change, and postoperative throat soreness.
Keywords: difficult airway, difficult intubation predictor, intubation techniques
1. Introduction
The Trachway Videolight Intubating Stylet (Biotronic Instrument Enterprise Ltd., Tai-Chung, Taiwan) was developed to facilitate tracheal intubation. It is fabricated from stainless steel with a distal deflection, facilitating easy passage through the oral cavity and navigation of the laryngeal inlet. It is preloaded with a tracheal tube and allows the visualization of the vocal cords via a camera placed at the end of the stylet, after which the endotracheal tube is advanced into the trachea via the stylet.[1,2]
The sniffing position (head lifted and neck flexed 35° from the torso at the atlanto-occipital joint)[3,4] can facilitate endotracheal intubation with a conventional direct laryngoscope, but may exacerbate cervical spinal cord injuries such as head injury with cervical trauma.[5–7] Intubation of patients with cervical spine injury commonly involves manual in-line stabilization to prevent cervical spinal cord injury by minimizing neck extension, flexion, and rotation.[5,8–11] Indeed, such stabilization is indicated for patients with cervical spine injuries.[5,8–11] However, it is not known whether the neutral-head or the head-lift position (without neck flexion or extension) is more effective with Trachway Videolight Intubating Stylet use during manual in-line stabilization. We hypothesized that difficulty in intubation differs with respect to the neutral-head and head-lift positions with use of this equipment. To test this hypothesis, patients were assigned to the neutral-head and head-lift groups. We evaluated group differences in tracheal intubation time, intubation success rate, number of intubation attempts, heart rate responses during intubation, and postoperative visual analog scale scores for throat soreness. We also assessed airway characteristics to predict the difficulty of Trachway intubation in both head positions.
2. Methods
This study was approved by the Ethics Committee (TSGHIRB No: 2-103-05-125) of Tri-Service General Hospital, Taipei, Taiwan on November 26, 2014. The study was registered at ClinicalTrials.gov (study identifier, NCT02578992) on October 13, 2015. We obtained informed consent from each patient enrolled in this study between November 2014 and October 2015. The study included patients aged 20–80 years scheduled for various surgeries requiring general anesthesia with tracheal intubation. All patients exhibited an American Society of Anesthesiologists physical status of I–III. Exclusion criteria were the presence of airway anomalies, craniofacial anomalies, cervical spine pathologies, head and neck disease, and a high risk of regurgitation or pulmonary aspiration.
2.1. Randomization and patient groups
A randomization sequence was generated using a computer; the allocation data were sealed in opaque and pre-labeled envelopes. The participants were randomly assigned in equal numbers to 2 groups: a neutral-head position group and a head-lift position group. In the neutral-head position group, the patient's head was placed on a flat surface,[10,12,13] while in the head-lift position group, a folded blanket (7 cm in height) was placed beneath the patient's head (Fig. 1).
Figure 1.
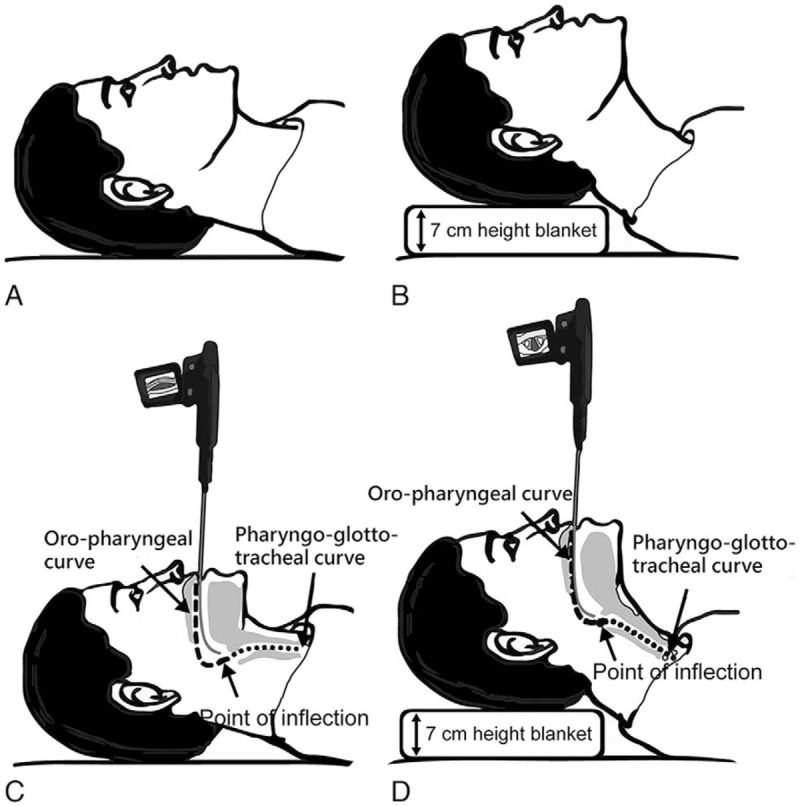
Patient's head and neck position. (A) In the neutral-head position group, the patient's head was on a flat surface, without neck flexion or extension. (B) In the head-lift position group, a folded blanket (7 cm in height) was placed beneath the patient's head. Manual in-line stabilization was achieved with an assistant grasping the mastoid process with the fingertips, cradling the mastoids, and grasping the occiput (side-of-bed assistant). The purpose was to support the head with both hands, maintain the neck in line with the body, and prevent the patient from moving.
2.2. Anesthesia induction
On arrival at the operating room, each patient's arterial blood pressure, electrocardiogram, and pulse oximeter readings were recorded. Following preoxygenation with spontaneous breathing via a facemask with 100% oxygen for 3 minutes, general anesthesia was induced with fentanyl (1–2 μg/kg), lidocaine (1–1.5 mg/kg), propofol (1.5–2 mg/kg), and rocuronium (0.6–0.9 mg/kg). In case of apnea, the patient received positive ventilation via a facemask with 100% oxygen and face mask ventilation (10/min) for approximately 2 to 3 minutes,[14] until the muscle relaxation was sufficient to facilitate proper intubation and the peripheral oxygen saturation (SpO2) level was greater than 99%. Before tracheal intubation with the Trachway Videolight Intubating Stylet, an assistant anesthesiologist, standing beside and to the left of the patient's head, performed the manual in-line stabilization (Fig. 1).
After preloading the intubating stylet with an endotracheal tube (internal diameter, 6.5–7.5 mm) (Covidien, Mansfield, MA), an anesthesiologist with experience of approximately 20 tracheal intubations with the Trachway performed a single-handed chin-lift technique[15] and inserted the intubating stylet into the patient's mouth, traversing over the tongue and into the pharynx (Fig. 1).[16] If the intubation time exceeded 35 s or the SpO2 reading decreased to <95%, the stylet was withdrawn and the patient was ventilated with 100% oxygen via a bag-mask for at least 1 minute and until the SpO2 reading was >99%. A second attempt was then performed. If the second attempt failed, the patient received 100% oxygen via a bag-mask for at least 1 minute until the SpO2 was >99%, and a GlideScope video laryngoscope (Verathon, Bothell, WA) was then used as a rescue device while cervical manual in-line stabilization was continued. Neither the backwards upwards rightwards pressure maneuver nor cricoid pressure were used during the intubation process in either group.
2.3. Data collection
All patients underwent airway assessments before the induction of anesthesia by an anesthesiologist. Details of the demographics and baseline airway characteristics were recorded (Table 1). Intubation time was defined as the interval between the intubating stylet reaching the level of the lips and the presentation of the capnography waveforms. If a second attempt was required, the intubation time was taken as the sum of the 2 Trachway attempts. If the second attempt failed, the GlideScope video laryngoscope was used as a rescue device, and the intubation time was not taken into account (Table 2). Heart rate was recorded 3 minutes before, and 1, 3, and 5 minutes after intubation (Table 2). All patients were asked to rate their postoperative throat soreness using a visual analog scale and to report whether hoarseness occurred 30 minutes after anesthesia emergence in the postanesthesia care unit. All other intubation-related complications, such as dental or mucosal damage, were recorded. The primary outcomes were the tracheal intubation time, number of intubation attempts, and intubation success rate. The secondary outcomes were the heart rate responses after intubation and the visual analog scale score of throat soreness.
Table 1.
Demographic characteristics and airway assessments.
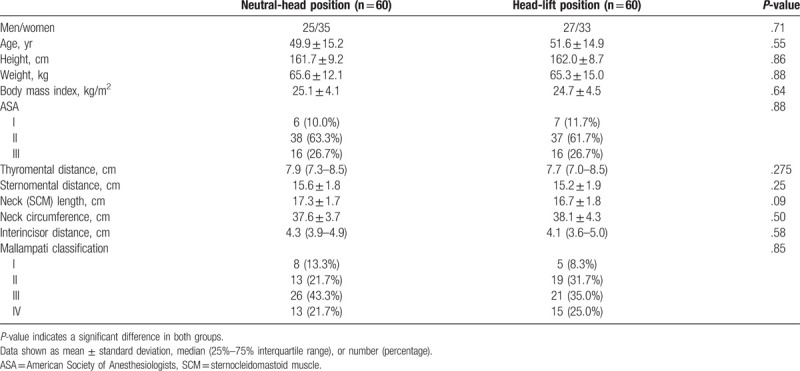
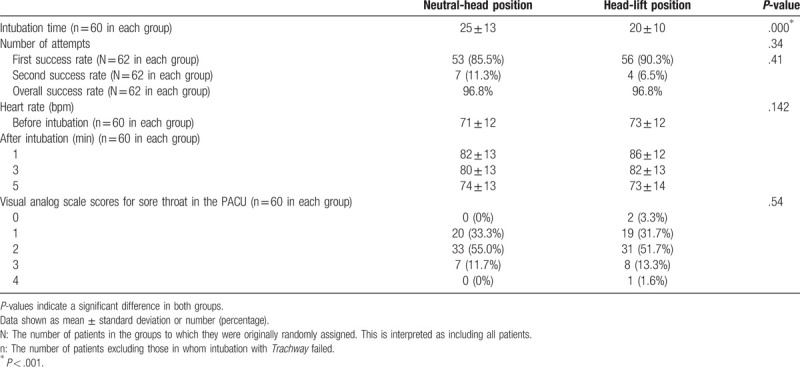
Table 2.
Comparison of the number of intubation attempts, success rate, hemodynamic response, and visual analog scale scores for sore throat in the postanesthesia care unit (PACU) between the 2 groups.
2.4. Sample size and statistical analyses
The sample size was estimated based on Kim et al,[17] which reported a mean (standard deviation) intubation time of 18.9 (15.2) s using the Trachway intubating stylet. Considering a 50% difference in intubation time to be significant with a type I error rate of 0.05 and a power of 90%, a sample size of 56 patients in each group was necessary. To allow for a potential 10% dropout rate, at least 124 patients (62 patients in each group) were required (Fig. 2). To compensate for potential dropouts, we increased the sample size to a total of 140 patients (70 in each group). Sample size estimation was performed using the G∗Power software (version 3.1.9.2, Franz Faul, Universitat Kiel, Kiel, Germany).
Figure 2.
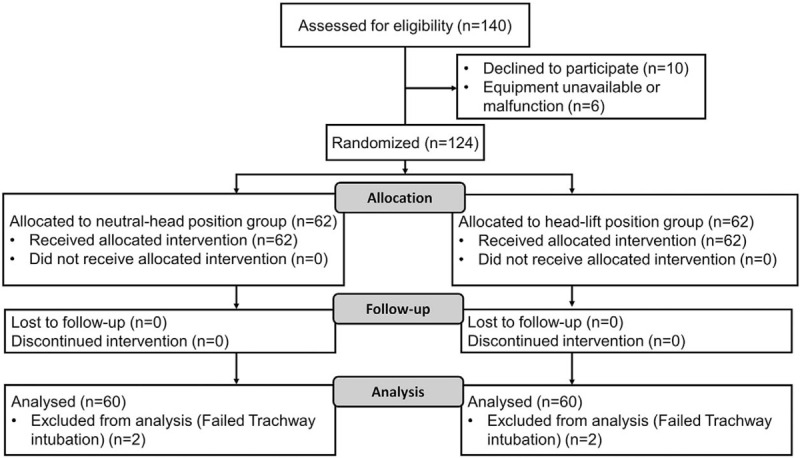
Study flow diagram.
Parametric Student t tests and nonparametric Mann–Whitney U tests were used to evaluate intergroup differences in continuous variables; Chi-square tests were used to evaluate intergroup differences in categorical variables, including patient characteristics, certain airway dimensions and assessments, the success rate, number of intubation attempts, and the visual analog scale score of throat soreness. The heart rate responses to endotracheal intubation in both groups were analyzed using 2-way analysis of variance (Table 2). Univariate and multivariate linear regression analyses were performed to identify potential predictors of intubation time in each group (Table 3). All reported probability values are 2-tailed. A P-value <.05 was considered statistically significant. Data were analyzed using the SPSS software (version 19, SPSS Inc, Chicago, IL).
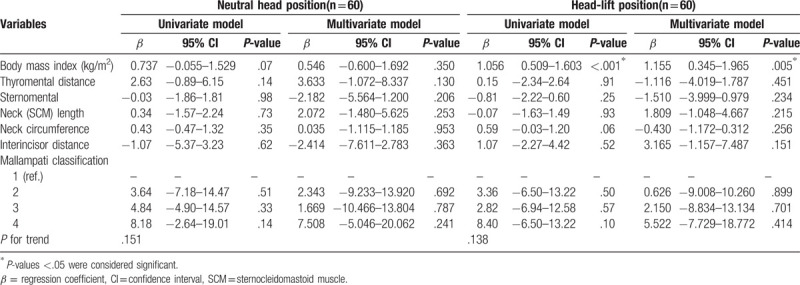
Table 3.
The results of the univariate and multivariate linear regression analyses of airway characteristic variables influencing the intubation time in the neutral-head position group and the head-lift position group.
3. Results
The trial flowchart is illustrated in Figure 1. In each group, we excluded 2 patients with intubation times >35 s over 2 attempts, who were successfully rescue-intubated with a GlideScope video laryngoscope due to Trachway intubation failure. Therefore, 60 patients were finally included in each group. There were no significant intergroup differences in airway characteristics (Table 1). The intubation time was significantly shorter in the head-lift position group than in the neutral-head position group (20 ± 10 and 25 ± 13 seconds, respectively, P = .000) (Table 2). The first attempt success rate, number of intubation attempts, overall (first and second attempt) success rates, heart rate, and visual analog scale scores for throat soreness did not differ significantly between the 2 groups (Table 2). In the univariate linear regression analyses, the body mass index (BMI) influenced intubation time in the head-lift position but not in the neutral-head group. After adjusting for potentially confounding variables, BMI remained significantly associated with intubation time in the head-lift position group (P = .005) (Table 3). Airway characteristics had no influence on intubation time or success rate. No hypoxia (SaO2 <95%), arrhythmia, hoarseness, or dental or mucosal damage was detected by the investigators in either group.
4. Discussion
The intubation time was correlated with technical difficulty and complications.[18] On average, intubation was 5 seconds faster among patients in the head-lift position than among those in the neutral-head position. The latter is recommended by the Norwegian guidelines for prehospital management of adult trauma patients with potential cervical spinal injury who require manual in-line stabilization.[10] However, the head-lift position with occipital padding increases the level of comfort during spinal immobilization.[13] Furthermore, the ideal positioning for neck immobilization is still controversial, given that the relationship between head-lift (without neck flexion or extension) and cervical cord injury is not well understood.[13,19,20] Therefore, under manual in-line stabilization, if cervical injury is mild so the head-lift position is not contraindicated, or if it is indicated because of low oxygenation saturation levels, this should be the primary choice because it reduces intubation time. Furthermore, in cases of an emergency or difficult airway, use of the head-lift position can facilitate intubation during shifting to intubation in the sniffing position with conventional direct or video laryngoscopy.[3–6] Indeed, effort to facilitate intubation success is recommended.[7] including shifting to the head-lift position that expedites intubation. However, the neutral-head position is strongly indicated in cases such as those of unstable cervical trauma because the head-lift position may increase the risk of worsening cervical pathology; this is supported by our findings that first attempt and overall (combined first and second) success rates, heart rate response, and postoperative throat soreness were indistinguishable between the 2 position groups.
Successful intubation often depends on proper patient head positioning.[3–6] Our study defined the neutral-head position as that in which the patient was lying on a flat surface without neck flexion or extension. For airway management in cervical spine injury, “neutral positioning” is encouraged, but is poorly defined and subject to controversy and individual variation. Some authors suggest that the neutral-head position is similar to the head position when standing and looking ahead.[7,10] We standardized the head-lift position by placing a 7-cm thick folded blanket beneath the patient's head. During conventional laryngoscopy, the patient's head is usually elevated by 5 to 10 cm to facilitate intubation.[13] However, head positioning during use of the Trachway Videolight Intubating Stylet is poorly described. Schriger et al found that occipital padding requirements ranging from 0 to 9.5 cm would decrease the discomfort due to spinal immobilization.[13] The optimal positioning for neck immobilization is still debated, rendering it difficult to provide recommendations for padding.[18,19] Therefore, we chose a median support level of 7 cm, which is clinically relevant yet unlikely to cause further cervical spinal cord injury because it provides the recommended lift of 0 to 9.5 cm.[13]
We successfully used the GlideScope video laryngoscope to rescue intubate patients who experienced intubation failure. However, the effect of this laryngoscope on the stability of the cervical spine during intubation is controversial.[8,21] While Robitaille et al[8] showed that it did not decrease movement of the cervical spine relative to the conventional direct laryngoscope, Kill et al[21] showed that it reduced such movement, thereby reducing the risk of secondary damage during the emergency intubation of patients with cervical spine trauma. Notably, the handles and blades of video laryngoscopes are bulkier and more curved than those of the Trachway Videolight Intubating Stylet. Thus, in patients with narrowing anterior neck space, limited mouth opening and neck extension, poor head and neck positioning, increased anteroposterior chest wall diameter, or pregnancy-related breast enlargement, it may be easier to use the Trachway than a video laryngoscope.[8] As there is no single perfect way to manage the airway in all patients with potential cervical spine injuries,[7] practitioners must use their judgment and assess the various risks (eg, spinal cord injury, aspiration, and hypoxia) [11] that render airway management in cervical spine injury challenging.[7]
An airway assessment should be conducted before endotracheal intubation[22] with the Trachway Videolight Intubating Stylet. However, predictors of the difficulty of intubation were previously unknown. We found no effect of some common predictors for intubation difficulty. BMI influenced intubation time in the head-lift position group, albeit not in the neutral-head position group. This is consistent with the results of Wang et al, who found that obesity is associated with an increased risk of difficult intubation among adult patients undergoing general surgical procedures. The lack of association between BMI in the neutral-head position group and intubation difficulty is also consistent with the results of a cohort study of elective tracheal intubation.[23] The variation in the predictive value of BMI in the 2 head positions is therefore not surprising. Future analyses should further explore the association between BMI and difficult airway or intubation time with the Trachway Videolight Intubating Stylet.
Kim et al. evaluated the Clarus Video System (Trachway) in adult patients with immobilized necks.[17] The high overall success rate that we report over 2 attempts (96.8%) is consistent with these authors’ results (94.3%). Differences between our study and theirs are as follows. First, we evaluated both the neutral-head position and the head-lift position, which can facilitate endotracheal intubation and is also used in conventional direct laryngoscopy, whereas Kim et al[17] evaluated only the neutral-head position. Second, we used “manual in-line stabilization” rather than the “cervical collar” used by Kim et al.[17] In cases of difficult or emergency airway for which laryngoscopy is considered, cervical collars may lead to higher rates of first-attempt failure, even with video laryngoscopy.[24] To facilitate mouth opening and access the airway, the anterior part of the cervical collar must often be removed during immobilization.[11] Lack of manual in-line stabilization during airway management has been associated with catastrophic neurological deterioration.[25] Manual in-line stabilization, rather than cervical collar use, potentially facilitates a more open mouth than is possible with semi-rigid cervical collars,[26] permitting Trachway Videolight Intubating Stylet intubation. Therefore, removal of the anterior part of the cervical collar in combination with manual in-line stabilization of the cervical spine has been suggested[27] to facilitate mouth opening and permit easy intubation with a Trachway Videolight Intubating Stylet. However, the application and removal of 1-piece or 2-piece cervical immobilization collars generates motion in the unstable spine, thereby risking worsening of cervical injuries.[27]
For patients with a potential cervical spine injury, rapid-sequence induction and intubation (RSII) is the preferred method for securing the airway.[5] Our anesthesia induction approach differed from the traditional components of RSII, which include preoxygenation, cricoid pressure applied after the injection of the induction agent, and avoidance of positive-pressure ventilation until the airway is secured by a cuffed endotracheal tube. These components are intended to reduce the risk of regurgitation of gastric contents during the induction of anesthesia, thereby decreasing the risk of pulmonary aspiration.[28] However, the application of cricoid pressure is the most controversial aspect of RSII.[29] Cricoid pressure involves the application of pressure at the cricoid ring to occlude the upper esophagus, thereby preventing the regurgitation of gastric contents into the pharynx, but this reduces tidal volumes, increases peak inspiratory pressure, and hampers ventilation.[30] Our study cases did not have cervical spine injuries and had a low risk of pulmonary aspiration. In consideration of the cricoid pressure-related risks, cricoid pressure was not suitable for our study cases.
The present study has some limitations. First, the anesthesiologist could not be blinded to the patient head position, which may have biased the results regarding the causal link between the Trachway Videolight Intubating Stylet and intubation time. Additionally, the observer who recorded the time was not blinded to group allocation and may have recorded the intubation time subjectively. Besides, the prolonged intubation time in the neutral-head position could be associated with operator unfamiliarity with this position, as operators are more familiar with the head-lift position. Second, the patients in the present study did not actually have cervical spine injuries but these were simulated to prohibit neck movement, and this may be why there was no decisive advantage in the head-lift position group. One must; therefore, use caution when extrapolating our results to patients with actual cervical instability. Third, intubation was only 5 seconds slower among patients in the neutral-head position than among those in the head-lift position. In general, shortening intubation procedures is still recommended because intubation procedures lasting longer than 30 seconds may increase the risk of hypoxia or arrhythmia.[31] Fourth, we did not use neuromuscular blockade and anesthesia depth monitoring (eg, bispectral index monitoring), which should be considered during intubation. However, the traditional practice of titrating the depth of anesthesia during intubation is equally useful with bispectral index value monitoring.[32]
In conclusion, our study supports the use of both head positions for orotracheal intubation with the Trachway Videolight Intubating Stylet with manual in-line stabilization. If cervical injury is minor so that the head-lift position is not contraindicated, or if it is suitable because of difficulty of ventilation with low oxygenation saturation levels, this should be the predominant choice because it reduces intubation time. However, if the head-lift position is unsuitable, we suggest that the neutral-head position is a favorable alternative due to its equal success rate and the fact that it is only 5 seconds slower than the head-lift position with equal heart rate responses and postoperative throat soreness. The minor heart rate responses and throat pain that we reported relative to previous studies[17,33] suggest reduced trauma with Trachway intubation in both head positions, and thus we recommend this instrument. Given that we report no effect of some common predictors for intubation difficulty, except for BMI in the head-lift position, future analyses should explore the associations between BMI and Trachway intubation time. Regardless of the technique, quick decision-making, familiarity with the equipment, appropriate head position, proper training, and effective communication remain the most important factors for a successful airway intervention.[34]
Acknowledgments
The authors thank the Department of Anesthesiology, Tri-Service General Hospital, and the Discipline of Anesthesiology, National Defense Medical Center.
Author contributions
Conceptualization: Wei-Hung Chan, Go-Shine Huang.
Data curation: Wei-Hung Chan, Go-Shine Huang.
Formal analysis: Wei-Hung Chan, Yu-Lung Chiu, Chiao-Pei Cheng, Yung-Chi Hsu, Mei-Hua Hu, Go-Shine Huang.
Investigation: Wei-Hung Chan.
Methodology: Wei-Hung Chan, Yu-Lung Chiu, Chiao-Pei Cheng, Yung-Chi Hsu, Go-Shine Huang.
Software: Yu-Lung Chiu.
Supervision: Go-Shine Huang.
Validation: Wei-Hung Chan, Chiao-Pei Cheng, Yu-Lung Chiu, Go-Shine Huang.
Visualization: Wei-Hung Chan, Go-Shine Huang.
Writing – original draft: Wei-Hung Chan, Chiao-Pei Cheng, Yu-Lung Chiu, Yung-Chi Hsu, Mei-Hua Hu, Go-Shine Huang.
Writing – review & editing: Wei-Hung Chan, Chiao-Pei Cheng, Yu-Lung Chiu, Yung-Chi Hsu, Mei-Hua Hu, Go-Shine Huang.
Footnotes
Abbreviations: BMI = body mass index, RSII = rapid-sequence induction and intubation, SpO2 = peripheral oxygen saturation.
How to cite this article: Chan WH, Cheng CP, Chiu YL, Hsu YC, Hu MH, Huang GS. Two head positions for orotracheal intubation with the trachway videolight intubating stylet with manual in-line stabilization: a randomized controlled trial. Medicine. 2020;99:17(e19645).
ClinicalTrials.gov study identifier number: NCT02578992.
The authors have no funding and conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
References
- [1].Hung KC, Tan PH, Lin VC, et al. A comparison of the trachway intubating stylet and the Macintosh laryngoscope in tracheal intubation: a manikin study. J Anesth 2013;27:205–10. [DOI] [PubMed] [Google Scholar]
- [2].Tseng KY, Chau SW, Su MP, et al. A comparison of trachway intubating stylet and airway scope for tracheal intubation by novice operators: a manikin study. Kaohsiung J Med Sci 2012;28:448–51. [DOI] [PubMed] [Google Scholar]
- [3].Isono S. Common practice and concepts in anesthesia: time for reassessment: is the sniffing position a “gold standard” for laryngoscopy? Anesthesiology 2001;95:825–7. [DOI] [PubMed] [Google Scholar]
- [4].Adnet F, Baillard C, Borron SW, et al. Randomized study comparing the “sniffing position” with simple head extension for laryngoscopic view in elective surgery patients. Anesthesiology 2001;95:836–41. [DOI] [PubMed] [Google Scholar]
- [5].Ollerton JE, Parr MJ, Harrison K, et al. Potential cervical spine injury and difficult airway management for emergency intubation of trauma adults in the emergency department-a systematic review. Emerg Med J 2006;23:3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Yang GZ, Xue FS, Sun C, et al. Difficult airway management: correct concepts and algorithm are important for patient safety. Chin Med J (Engl) 2016;129:1886–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Austin N, Krishnamoorthy V, Dagal A. Airway management in cervical spine injury. Int J Crit Illn Inj Sci 2014;4:50–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Robitaille A, Williams SR, Tremblay MH, et al. Cervical spine motion during tracheal intubation with manual in-line stabilization: direct laryngoscopy versus GlideScope videolaryngoscopy. Anesth Analg 2008;106:935–41. [DOI] [PubMed] [Google Scholar]
- [9].Manoach S, Paladino L. Manual in-line stabilization for acute airway management of suspected cervical spine injury: historical review and current questions. Ann Emerg Med 2007;50:236–45. [DOI] [PubMed] [Google Scholar]
- [10].Kornhall DK, Jørgensen JJ, Brommeland T, et al. The Norwegian guidelines for the prehospital management of adult trauma patients with potential spinal injury. Scand J Trauma Resusc Emerg Med 2017;25:1.–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Martini RP, Larson DM. Clinical evaluation and airway management for adults with cervical spine instability. Anesthesiol Clin 2015;33:315–27. [DOI] [PubMed] [Google Scholar]
- [12].Greenland KB, Edwards MJ, Hutton NJ. External auditory meatus-sternal notch relationship in adults in the sniffing position: a magnetic resonance imaging study. Br J Anaesth 2010;104:268–9. [DOI] [PubMed] [Google Scholar]
- [13].Schriger DL, Larmon B, LeGassick T, et al. Spinal immobilization on a flat backboard: does it result in neutral position of the cervical spine? Ann Emerg Med 1991;20:878–81. [DOI] [PubMed] [Google Scholar]
- [14].Baraka AS, Taha SK, Aouad MT, et al. Preoxygenation: comparison of maximal breathing and tidal volume breathing techniques. Anesthesiology 1999;91:612–6. [DOI] [PubMed] [Google Scholar]
- [15].Lee AR, Yang S, Shin YH, et al. A comparison of the BURP and conventional and modified jaw thrust manoeuvres for orotracheal intubation using the Clarus Video System. Anaesthesia 2013;68:931–7. [DOI] [PubMed] [Google Scholar]
- [16].Costa F, Mattei A, Massimiliano C, et al. The Clarus Video System as a useful diagnostic tool. Anaesthesia 2011;66:135–6. [DOI] [PubMed] [Google Scholar]
- [17].Kim JK, Kim JA, Kim CS, et al. Comparison of tracheal intubation with the airway scope or clarus video system in patients with cervical collars. Anaesthesia 2011;66:694–8. [DOI] [PubMed] [Google Scholar]
- [18].Yoo JY, Park SY, Kim JY, et al. Comparison of the McGrath videolaryngoscope and the Macintosh laryngoscope for double lumen endobronchial tube intubation in patients with manual in-line stabilization: a randomized controlled trial. Medicine (Baltimore) 2018;97:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].De Lorenzo RA, Olson JE, Boska M, et al. Optimal positioning for cervical immobilization. Ann Emerg Med 1996;28:301–8. [DOI] [PubMed] [Google Scholar]
- [20].Meldon SW, Brant TA, Cydulka RK, et al. Out-of-hospital cervical spine clearance: agreement between emergency medical technicians and emergency physicians. J Trauma 1998;45:1058–61. [DOI] [PubMed] [Google Scholar]
- [21].Kill C, Risse J, Wallot P, et al. Videolaryngoscopy with glidescope reduces cervical spine movement in patients with unsecured cervical spine. J Emerg Med 2013;44:750–6. [DOI] [PubMed] [Google Scholar]
- [22].Apfelbaum JL, Hagberg CA, Caplan RA, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology 2013;118:251–70. [DOI] [PubMed] [Google Scholar]
- [23].Wang T, Sun S, Huang S. The association of body mass index with difficult tracheal intubation management by direct laryngoscopy: a meta-analysis. BMC Anesthesiol 2018;18:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Aoi Y, Inagawa G, Hashimoto K, et al. Airway scope laryngoscopy under manual inline stabilization and cervical collar immobilization: a crossover in vivo cinefluoroscopic study. J Trauma 2011;71:32–6. [DOI] [PubMed] [Google Scholar]
- [25].Farmer J, Vaccaro A, Albert TJ, et al. Neurologic deterioration after cervical spinal cord injury. J Spinal Disord 1998;11:192–6. [PubMed] [Google Scholar]
- [26].Goutcher CM, Lochhead V. Reduction in mouth opening with semi-rigid cervical collars. Br J Anaesth 2005;95:344–8. [DOI] [PubMed] [Google Scholar]
- [27].Prasarn ML, Conrad B, Del Rossi G, et al. Motion generated in the unstable cervical spine during the application and removal of cervical immobilization collars. J Trauma Acute Care Surg 2012;72:1609–13. [DOI] [PubMed] [Google Scholar]
- [28].Rohsbach C, Wirth S, Lenz K, et al. Survey on the current management of rapid sequence induction in Germany. Minerva Anestesiol 2013;79:716–26. [PubMed] [Google Scholar]
- [29].El-Orbany M, Connolly LA. Rapid sequence induction and intubation: current controversy. Anesth Analg 2010;110:1318–25. [DOI] [PubMed] [Google Scholar]
- [30].Ellis DY, Harris T, Zideman D. Cricoid pressure in emergency department rapid sequence tracheal intubations: a risk-benefit analysis. Ann Emerg Med 2007;50:653–65. [DOI] [PubMed] [Google Scholar]
- [31].Nolan JP, Deakin CD, Soar J, et al. European resuscitation council guidelines for resuscitation 2005. Section 4. Adult advanced life support. Resuscitation 2005;67 Suppl 1:S39–86. [DOI] [PubMed] [Google Scholar]
- [32].Arya S, Asthana V, Sharma JP. Clinical vs. bispectral index-guided propofol induction of anesthesia: a comparative study. Saudi J Anaesth 2013;7:75–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Shribman AJ, Smith G, Achola KJ. Cardiovascular and catecholamine responses to laryngoscopy with and without tracheal intubation. Br J Anaesth 1987;59:295–9. [DOI] [PubMed] [Google Scholar]
- [34].Karlik J, Aziz M. Recent trends in airway management. F1000Res 2017;6:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]


