Supplemental Digital Content is available in the text
Keywords: educational models, lecture based learning, medical education, meta-analysis, problem-based learning
Abstract
Background:
Problem-based learning (PBL) combined lecture based learning (LBL) has been a trend adopted as a new medical pedagogical approach in Chinese medical teaching. This study aims to evaluate the impacts of hybrid PBL and LBL pedagogy compared with LBL teaching method on the learning achievements of clinical curriculum for Chinese medicine students.
Methods:
Randomized controlled trials (RCTs) were identified through a systematic literature search of electronic databases and article references up to June 2019. PubMed, EBSCO, Web of Science, Cochrane Library, Wanfang Database, CNKI, and China Biology Medicine database (CBM) were searched. End points included knowledge scores, skill scores, medical writing scores, comprehensive ability scores and teaching satisfaction.
Results:
Totally 20 randomized controlled studies were finally included and all Chinese literatures, involving 1817 patients. Compared with traditional LBL pedagogy, hybrid PBL and LBL pedagogy significantly increased the clinical theoretical knowledge assessment score (RR = 4.84, 95% CI: 2.92∼6.76, P < .00001), clinical skills assessment score (RR = 1.60, 95% CI: 1.39∼1.81, P < .00001), comprehensive ability score (RR = 9.13, 95% CI: 8.42∼9.84, P < .00001) and teaching satisfaction (RR = 2.58, 95% CI: 1.84∼3.62, P < .00001), The meta-regression results showed that expertise-level of students and course type were the factors that caused heterogeneity.
Conclusions:
Hybrid PBL and LBL pedagogy integrates the advantages of conventional teaching methods and novel teaching methods, remarkably improves the teaching efficacy, demonstrates easy acceptance by students, and meets the demand of modern medical education, so it is an effective approach to cultivate the medical talents with an ability of innovative thinking and can be advocated and popularized as a teaching means.
1. Introduction
The ability of clinical thinking skills, basic clinical skills and communication skills is necessary for clinical medicine students. Problem-based learning (PBL) is an important teaching approach characterized by use of clinical cases as a context for students to learn problem-solving skills and acquire knowledge involving both basic science and clinical medicine. PBL promoted a deep method for clinical medical students to train the clinical diagnosis and treatment reasoning skills, cultivate the actual clinical problems solving skills, give student's comprehensive understanding of medical courses, and increase motivation of transition to clinical training. The PBL teaching method has been extensively applied as supplementary teaching methods in Chinese medical education.[1,2]
LBL is still the most commonly used teaching method in medical education in China. With increasing application of PBL teaching method in Chinese medical students, however, some problems are found in the practice, such as students’ poor initiative, insufficient design of PBL problems, as well as lack of systematicness, and features of PBL course, especially in specialized clinical curriculums. Therefore, more and more investigators advocate PBL as a supplement to the conventional lecture based learning (LBL) method, that is, problem-based learning combined lecture based learning (PBL+LBL) teaching method. In recent years, the hybrid PBL and LBL pedagogy approach has been a trend in Chinese medical teaching.
Currently, there is still a controversy about the study results concerning the effect of PBL+LBL teaching method on the leaning achievements of specialized courses for clinical medicine students in China. Moreover, most results of individual published studies were with relatively small sample size, it is necessary to perform a meta-analysis study to quantitatively combine of the existed evidence. This study aimed to systematically and comparatively evaluate combined application of PBL and LBL teaching models (PBL+LBL group) and LBL teaching method (LBL group) on the leaning achievements of specialized courses for clinical medicine students by meta-analysis, which is expected to provide a reference for improving clinical medical education in China. The meta-analysis showed that hybrid PBL and LBL pedagogy can significantly increase knowledge scores, skill scores, medical writing scores, comprehensive ability scores and teaching satisfaction compared to the application of the LBL teaching method alone in clinical curriculum.
2. Methods
In this study, the meta-analysis conducted following the guidelines of PRISMA checklist. Ethical approval is unnecessary due to it is a review of previously reported articles and does not involve any processing of individual patient data.
2.1. Literature search
PubMed, EBSCO, Web of Science, Cochrane Library, Chinese Wanfang Database, Chinese National Knowledge Infrastructure (CNKI), and China Biology Medicine database (CBM) were systematically searched by June 2019. The following English and Chinese search words were used: “Problem-based learning”, “PBL”, “lecture based learning”, “LBL”, “randomized controlled trials”. The language was limited as Chinese or English, and the references of the included studies were also searched.
PBL is defined as a student-centered pedagogy in which a patient problem or clinical case study presented to a small group of students. LBL is defined as the time span of teaching to direct presentation of facts and concepts by the lecturer. PBL+LBL is defined as PBL as a supplement to the application of the LBL pedagogy alone in a clinical curriculum.
2.2. Screening and evaluation of literatures
The inclusion criteria were described below:
-
1)
the study objects were the clinical medicine students;
-
2)
the study design was a randomized controlled study;
-
3)
in the study grouping, PBL+LBL served as experimental group and LBL served as control group;
-
4)
the study objective was to compare the theoretical or practical teaching efficacy of specialized courses.
The exclusion criteria were as follows:
-
1)
the studies were non-randomized and non-controlled;
-
2)
the control group was PBL;
-
3)
the study results could not provide the required data information;
-
4)
the sample size was too small (<10);
-
5)
the individual case reports, conferences, review literatures, and repeatedly published studies were excluded.
The quality of literatures included into the study was independently evaluated using Cochrane Collaboration's tool for assessing the risk of bias.
2.3. Data extraction
Two investigators excluded the non-eligible literatures by reading the titles and abstracts of the obtained literatures, and further searched and read the full text of the eligible literatures. They independently extracted the literature data, mainly including title, authors, publication date, country and region, sample size, teaching courses, outcome indicators, and so on.
2.4. Primary outcome measures
The primary outcomes included clinical theory assessment score, basic clinical skills assessment score, medical writing scores, comprehensive academic performance, and teaching satisfaction.
2.5. Statistical analysis
We used fixed-effects or random-effects models to produce across-study summary relative risk (RR) with 95% confidence interval (CI). The pooled effects were calculated using fixed-effect model with the Mantel-Haenszel method when there was no significant heterogeneity or with DerSimonian-Laird weights for the random effects model when there was significant heterogeneity. The chi-square test was used to study heterogeneity between trials, and the I2 statistic was used to estimate the percentage of total variation across studies. I2 value greater than 50% was considered as significant heterogeneity. Publication bias was explored through visual inspection of funnel plots and assessed by applying the Egger weighted regression statistic with a P value < .05 indicating significant publication bias among the included studies. Correction for publication bias was performed using trim-and-fill methods. A P value < .05 was regarded as significant. All statistical analyses were performed using Review Manager (version 5, Cochrane Collaboration, Oxford, UK).
3. Results
3.1. Results of literature search
Total 126 literatures were obtained by preliminary search, 34 literatures were screened by reading the titles and abstracts, and finally 20 randomized controlled studies meeting the inclusion criteria were included after the non-eligible literatures were excluded by reading the full text (Fig. 1). All included studies were from China and involved a total of 1817 students, including 910 students in PBL+LBL group and 907 group in LBL group. Specialized courses in clinical medicine include Gynecology and obstetrics, Hepatobiliary surgery, Cardiothoracic Surgery, Dermatology and Venerology, Breast surgery, Vascular Surgery, General Practice, internal medicine, General surgery, Infectious, Internal medicine, and Pediatric. The general characteristics of the included literatures are shown in Table 1.[3–22]
Figure 1.
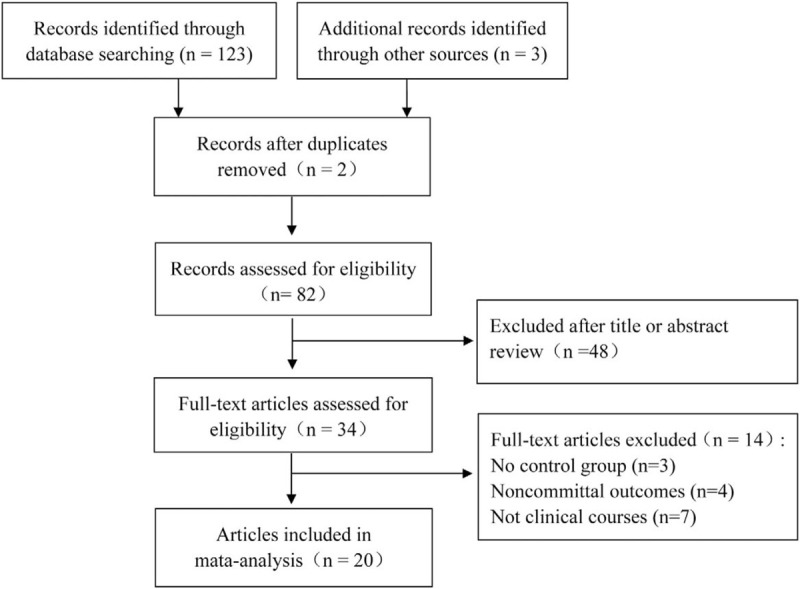
Flow diagram of studies included in the systematic review and meta-analysis.
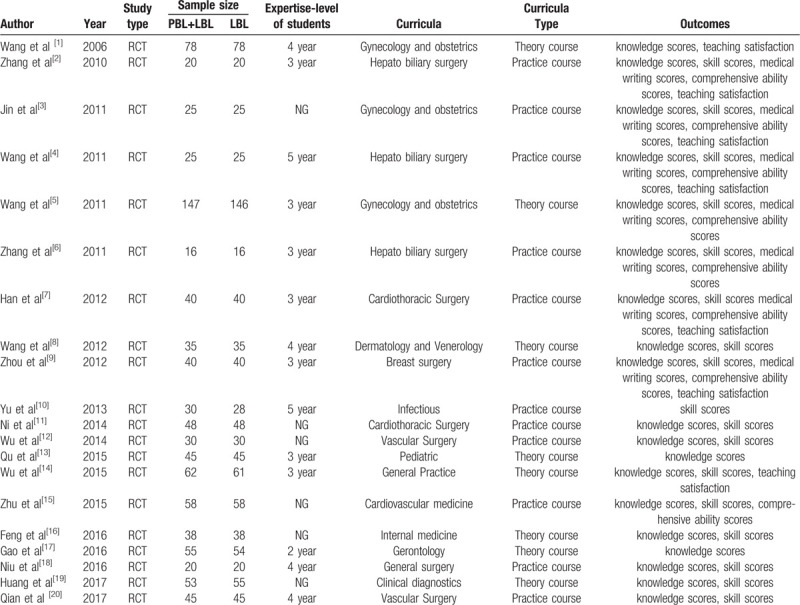
Table 1.
Characteristics of studies included in the analysis.
3.2. Results of literature quality evaluation
In 7 aspects of randomization method, allocation concealment, blinding to the study objects and implementers, blinding to the measurement of results, integrity of result data, selective report bias, and other biases, the quality of each included literature was evaluated using Cochrane Collaboration's tool for assessing the risk of bias recommended in Cochrane systematic evaluation manual, and the results were low bias, medium bias, and unclear. The summary of 20 RCT studies included is seen in Figure 2.
Figure 2.
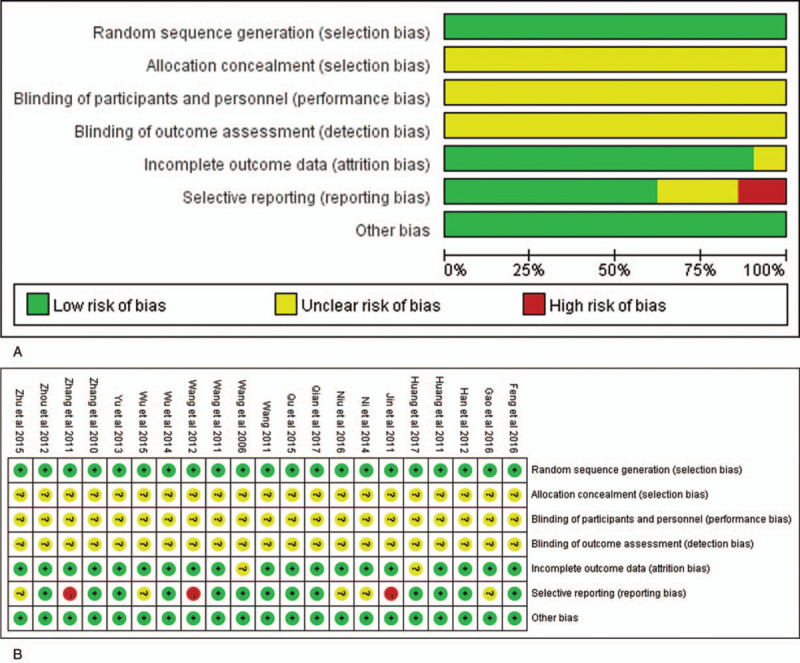
Risk of bias assessment. (A) Authors’ judgments about risk of bias graph for each included study; (B) Authors’ judgments about risk of bias summary across all included studies.
4. Meta-analysis results
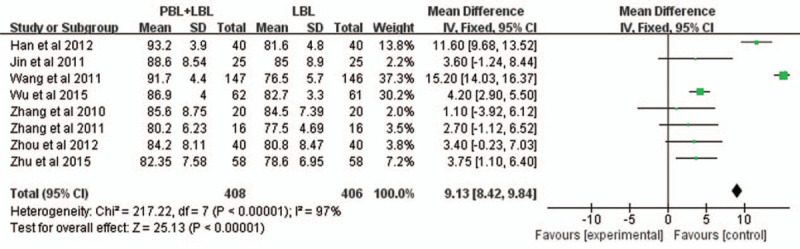
4.1. Clinical theory assessment score
The clinical theory assessment score was reported in all 20 controlled studies included, and there was high heterogeneity among these studies (P < .00001, I2 = 97%), thus the analysis was performed using random effects model. Meta-analysis results showed that the theoretical examination performance of students in PBL + LBL group was significantly better than that in LBL group (RR = 4.84, 95% CI: 2.92∼6.76, P < .00001) (Fig. 3).
Figure 3.
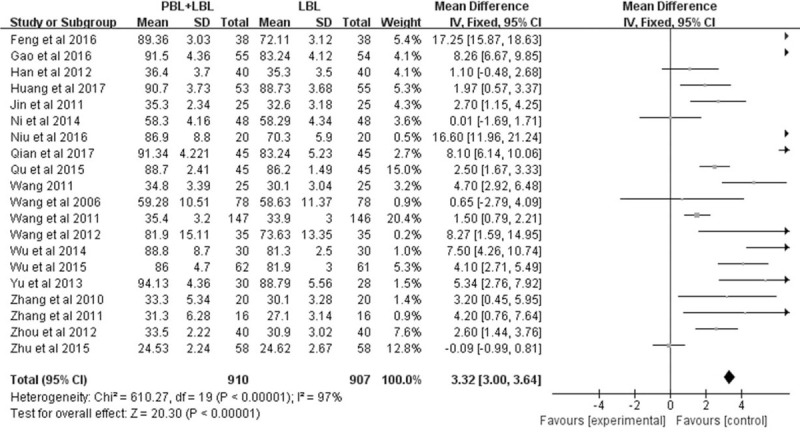
Forest plot for the meta-analysis of theory assessment score.
4.2. Clinical skills assessment score
The clinical skills assessment score was reported in 13 studies, and there was high heterogeneity among these studies (P < .00001, I2 = 98%), thus the analysis was performed using random effects model. Meta-analysis results suggested that the operation skills performance of students in PBL+LBL group was significantly superior to that in LBL group (RR = 1.60, 95% CI: 1.39∼1.81, P < .00001) (Fig. 4).
Figure 4.
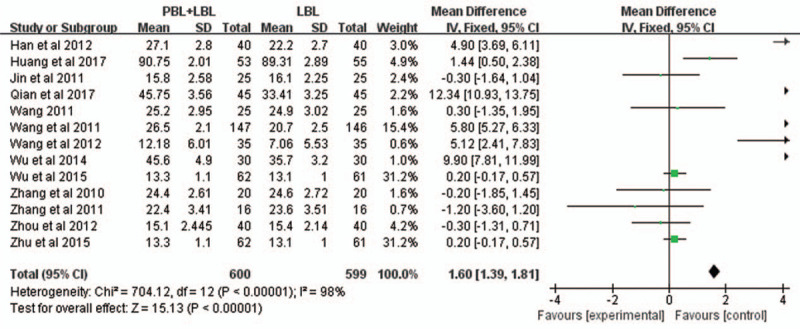
Forest plot for the meta-analysis of skills assessment score.
4.3. Medical record writing assessment score
The medical record writing assessment score was reported in 7 studies, and there was low heterogeneity among these studies (P < .00001, I2 = 87%), thus the analysis was performed using random effects model. Meta-analysis results indicated that the medical record writing assessment performance of students was significantly better in PBL + LBL group than in LBL group (RR = 3.44, 95% CI: 2.94∼3.93, P < .00001) (Fig. 5).
Figure 5.
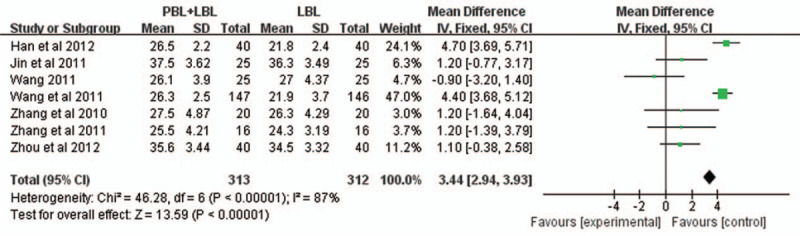
Forest plot for the meta-analysis of medical record writing assessment score.
4.4. Comprehensive ability score
The comprehensive ability score of students was reported in 8 studies, and there was low heterogeneity among these studies (P < .00001, I2 = 97%), thus the analysis was performed using random effects model. As shown by meta-analysis results, the comprehensive ability performance of students was significantly superior in PBL+LBL group to in LBL group (RR = 9.13, 95% CI: 8.42∼9.84, P < .00001) (Fig. 6).
Figure 6.
Forest plot for the meta-analysis of comprehensive ability score.
4.5. Teaching satisfaction
The teaching satisfaction evaluation of students was reported with three levels in 9 studies, specifically satisfactory in 9 studies, ordinary in 6 studies and poor in 6 studies. Meta-analysis results revealed that the proportion of students evaluating teaching as satisfactory was significantly higher in PBL + LBL group than in LBL group (RR = 2.58, 95% CI: 1.84∼3.62, P < .00001) (see Figure 7A); the proportion of students evaluating teaching as ordinary demonstrated no statistically significant difference between 2 groups (RR = 0.72, 95% CI: 0.47∼1.10, P = .13) (see Fig. 7B); in the proportion of students evaluating teaching as poor, there was no statistically significant difference between two groups (RR = 0.49, 95% CI: 0.21∼1.15, P = .10) (Fig. 7C).
Figure 7.
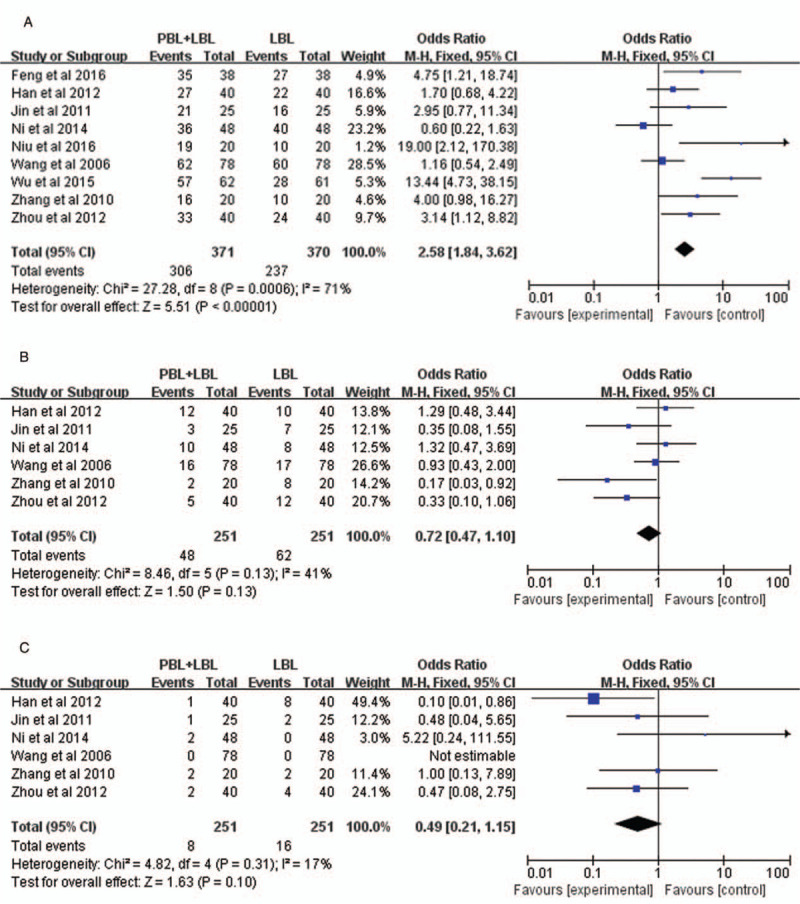
Forest plot for the meta-analysis of teaching satisfaction.
5. Discussion
Medicine is a discipline of strong practicality and cultivating the abilities and comprehensive quality of clinical medicine students is a long-standing focus of medical education reform in various countries. An important goal and challenge faced by the current medical education in China is to cultivate the clinical thinking skills, basic clinical skills and doctor-patient communication ability of medical students. PBL is possibly one of the most innovative themes in medical education; it has raised extreme debate and still continues to generate passionate discussions.[23] PBL is being increasingly favored by medical educationalists, as it has been shown by some to better prepare students for the teamwork, communication skills and patient interaction required in clinical practice.[24,25] Compared with the conventional clinical teaching methods, PBL is based on the simulation of real clinical scenes, advocates the “student-centered” idea and the initiative learning of students, and focuses on the cultivation of diagnostic thinking and problem-resolving ability. In the recent years, PBL has been extensively applied in China medical education, and it is a student-centered, teacher-orientated, discussion-based teaching method compared with the conventional LBL teaching method, can better motivate the active thinking and leaning positivity of students, puts more emphasis on cultivating the diagnostic thinking and problem-resolving ability of students.
PBL complies with the modern medical education philosophy, because it advocates and guides the self-learning ability of students and cultivates the ability of students to analyze and resolve the problems by the instruction and guidance of clinical problems. However, the application of PBL alone in the teaching practice has some shortcomings, for example, the required teaching courses cannot be finished in the relatively limited teaching hours, and only depending on the self-learning initiative of students may lead to the insufficiency in the learning systematicness and understanding deepness of knowledge points of specialized courses. The conventional lecturing-based LBL teaching method can make the medical students completely master and fully understand the relevant theoretical knowledge points of specialized courses by lecturing these knowledge points via the teacher system, but its single application easily limits the active thinking and learning of students. Therefore, PBL+LBL teaching method is effective, it can help the medical students to sturdily and systematically master the knowledge points of clinical medicine, arouse the initiative of students and train their practicing abilities to analyze and resolve the problems by the case- and problem-based guidance, and finally comprehensively improve the comprehensive quality, correct diagnosis and treatment thinking and other abilities of clinical medical students. In this RCT-based study, we systematically and comparatively evaluated the impacts of hybrid PBL and LBL pedagogy and LBL teaching method on the leaning achievements of specialized courses for clinical medical students by meta-analysis, and the results showed that hybrid PBL and LBL pedagogy was significantly superior to LBL teaching method in the clinical theoretical knowledge assessment score, clinical skills assessment score, comprehensive ability score and teaching satisfaction.
Traditional cultural values and the global economic system were widely regarded as important forces shaping medical education system in China. As stated in Healthy China 2030 blueprint, health is the indispensable prerequisite for the overall wellbeing of people as well as the foundation of economic and social development. China can continue to reform new medical education towards healthy China 2030. PBL as a student-centered educational method will play an increasingly important role to foster collaboration on realistic clinical problems under guidance of a tutor, to stimulate self-regulated learning and self-regulated activities in China medical education.
As with any study, the present study has some limitations. First, medical students who participated in the included studies came from some provinces and cities alone, so we cannot claim that this conclusion was representative of all Chinese medical students. Furthermore, all included studies in this meta-analysis were from China, this conclusion may be lack of representativeness in global and national medical education. Therefore, a replication of the study with a larger and more representative sample of medical students from China and other countries can strengthen the findings in this study. Second, considering that there are not included all clinical curriculums, such as, family medicine, psychiatry, emergency medicine, neurology and so on. Moreover, it is impossible for the researchers to use the blinding method during the whole clinical curriculum. Third, medical students in different years were not taken into account in all included studies. Students in different years of study from second year to fifth year had different workloads in clinical medicine. Students in third year represent the transition to the clinical years in China. Fourth year students have more clinical courses which involve clinical medical curriculum often focusing on disease diagnosis and treatment and paying little attention to basic clinical skills and communication skills. A final limitation is that students’ perceptions on the learning environment were not taken into account.
6. Conclusions
Our meta-analysis indicated that hybrid PBL and LBL pedagogy is more effective than LBL in improving learning knowledge, skills, comprehensive ability score and teaching satisfaction of clinical curriculum, providing evidence for the implement of PBL+ LBL in medical education in China. Hybrid PBL and LBL pedagogy integrates the advantages of conventional teaching methods and novel teaching methods, not only introduces the innovations of PBL teaching method in the teaching contents, means and approaches, but also can achieve the systemization and methodization of knowledge so that the students are able to know what it is and why it is. Furthermore, hybrid PBL and LBL teaching method significantly improve the teaching efficacy, which is easily accepted by students, and meets the demand of modern medical education. Therefore, hybrid PBL and LBL is an effective approach to cultivate the medical talents with an innovative thinking ability and can be advocated and popularized as teaching means. Hybrid PBL and LBL should be further gradually introduced into clinical medical teaching programs. At present, PBL is still not a mainstream teaching method in China and only used as a supplement to LBL teaching method in most colleges and universities, there are no specifications formed, and a variety of teaching units shall further improve the standards, teaching materials, question banks and teachers for PBL+LBL teaching.
Author contributions
Conceptualization: Chun-Xiao Liu, Wei-Wei Ouyang, Xiao-Wen Wang.
Data curation: Chun-Xiao Liu, Xiao-Wen Wang.
Methodology: Chun-Xiao Liu, Wei-Wei Ouyang.
Project administration: Chun-Xiao Liu, Wei-Wei Ouyang.
Software: Chun-Xiao Liu, Zhao-Lei Jiang.
Supervision: Xiao-Wen Wang, Zhao-Lei Jiang.
Writing – original draft: Chun-Xiao Liu.
Writing – review & editing: Xiao-Wen Wang, Dan Chen.
Supplementary Material
Footnotes
Abbreviations: CBM = China Biology Medicine database, CI = confidence interval, CNKI = Chinese national knowledge infrastructure, LBL = lecture based learning, PBL = problem-based learning, RCTs = randomized controlled trials, RR = relative risk.
How to cite this article: Liu CX, Ouyang WW, Wang XW, Chen D, Jiang ZL. Comparing hybrid problem-based and lecture learning (PBL + LBL) with LBL pedagogy on clinical curriculum learning for medical students in China: A meta-analysis of randomized controlled trials. Medicine. 2020;99:16(e19687).
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
The authors declare that they have no conflict of interests
Supplemental Digital Content is available for this article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website (www.md-journal.com).
References
- [1].Zhang S, Xu J, Wang H, et al. Effects of problem-based learning in Chinese radiology education: a systematic review and meta-analysis. Medicine (Baltimore) 2018;97:e0069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Ma Y, Lu X. The effectiveness of problem-based learning in pediatric medical education in China: A meta-analysis of randomized controlled trials. Medicine (Baltimore) 2019;98:e14052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Wang LQ, Shi XB, Ding YL. PBL+LBL double-track practice in gynaecology and obstetrics teaching (in Chinese). Res Med Educ 2006;10:940–1. [Google Scholar]
- [4].Zhang GW, Jin J, Zhou J. Appliration of PBL+LBL double-track for practice of 8-year program medical students in hepato·biliary surgery department (in Chinese). J Shanxi Med Univ 2010;12:301–3. [Google Scholar]
- [5].Jin J, Zhang GW. Application of PBL+LBL teaching methods to eightyears medical students in gynaecology and obstetrics clinic teaching (in Chinese). Basic Med Educ 2011;13:185–7. [Google Scholar]
- [6].Wang Y, Jiang X. Appliration of PBL+LBL teaching method in the practice course of hepato-biliary surgery (in Chinese). Chin Higher Med Educ 2011;12:108–9. [Google Scholar]
- [7].Wang J, Li XM, Tan XS. The application of PBL-LBL double-track model in gynecology and obstetrics teaching (in Chinese). Guide Chin Med 2011;22:19–20. [Google Scholar]
- [8].Zhang GW. Application of double-track method for practice of forgein students in hepato biliary surgery department (in Chinese). Basic Med Educ 2011;13:477–9. [Google Scholar]
- [9].Han Y, Li XF, Huang LJ, et al. The effect of double-track teaching method in the study of thoracic surgery clinical teaching (in Chinese). Prog Mod Biomed 2012;28:5594–7. [Google Scholar]
- [10].Wang ZY, Qiu HF, Dong DQ. Exploration and practice of PBL + LBLdouble-track mode in the teaching of dermatology and venerology (in Chinese). Clin Med Eng 2012;12:2266–7. [Google Scholar]
- [11].Zhou Y, Tang P, Ming J, et al. Application of PBL+LBL in breast surgery clinical probation (in Chinese). Northwest Med Educ 2012;5:1044–6. [Google Scholar]
- [12].Yu HB. Application of combination of LBL and PBL teaching method in clinical practice of infectious diseases (in Chinese). Res Teach 2013;27:141–2. [Google Scholar]
- [13].Ni YF, Yang RX, Wang J, et al. Application of problem-based learning combined with lecture-based learning in thoracic surgical clinical education (in Chinese). Basic Med Educ 2014;8:639–41. [Google Scholar]
- [14].Wu X, Zhang HJ, Li XF, et al. Application of PBL combined with LBL in the teaching of clinical training for vascular surgery (in Chinese). Prog Mod Biomed 2014;26:5167–9. [Google Scholar]
- [15].Qu SQ, Shao QL, Lv Y. The application of problem-based learning method combined with lecture based learning in the pediatric clinical practic (in Chinese). Chin Foreign Med Res 2015;6:153–4. [Google Scholar]
- [16].Wu H, Sun X, Shi RL, et al. Effect of PBL + LBL teaching method in the course of general practice introduction (in Chinese). Chin Gen Pract 2015;10:1176–80. [Google Scholar]
- [17].Zhu H, Xue H, Xu L, et al. Effect research on problem based learning united lecture based learning teaching method in clinical cardiovascular medicine (in Chinese). Chin Mod Med 2015;30:148–50. [Google Scholar]
- [18].Feng Y, Zhou JH, Jiang Y, et al. Combined application effect of PBL teaching method and LBL teaching method in internal medicine teaching (in Chinese). Chin Contin Med Educ 2016;26:7–9. [Google Scholar]
- [19].Gao P, Tang G, Xiao H, et al. Application of problem based learning (PBL) combined with lecture based learning (LBL) teaching methods in the teaching of gerontology (in Chinese). Prog Mod Biomed 2016;16:3168–71. [Google Scholar]
- [20].Niu J. Application of PBL +LBL in clinical practice of inguinal hernia disease for international students (in Chinese). Chin Contin Med Educ 2016;8:8–10. [Google Scholar]
- [21].Huang JJ, He XJ, Bai WW. Application of lecture based learning plus problem based learning method in instruction of cardiac physical examination in clinical diagnostics (in Chinese). Chin Heart J 2017;30:248–50. [Google Scholar]
- [22].Qian A. Application of Combination of PBL and LBL in Clinical Practice Teaching of Vascular Surgery (in Chinese). China Contin Med Educ 2017;9:28–9. [Google Scholar]
- [23].Tavakol M, Dennick R, Tavakol S. A descriptive study of medical educators’ views of problem-based learning[J]. BMC Med Educ 2009;9:66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Prince KJ, van Eijs PW, Boshuizen HP. Vleuten CP van der, Scherpbier AJ: General competencies of problem-based learning (PBL) and non-PBL graduates. Med Educ 2005;39:394–401. [DOI] [PubMed] [Google Scholar]
- [25].Cohen-Schotanus J, Muijtjens AM, Schonrock-Adema J, et al. Vleuten CP van der: Effects of conventional and problem-based learning on clinical and general competencies and career development. Med Educ 2008;42:256–65. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


