Abstract
Irritable bowel syndrome (IBS)-like symptoms tend to be common in inflammatory bowel disease (IBD) patients even during the long-standing remission phase, and quality of life (QOL) seem to reduce in IBD patients with such symptoms. Thus, the aim of this study was to define the prevalence of IBS-like symptoms in inactive IBD patients using Rome IV criteria and evaluate the effect of IBS-like symptoms on QOL.
Total 137 patients with IBD (56 with ulcerative colitis (UC) and 81 with Crohn disease (CD), who had been in long-standing remission according to the clinical scoring system and 123 control participants were included. These patients completed questionnaires to evaluate IBS-like symptoms according to Rome IV criteria, and the impact of these symptoms on the QOL of inactive IBD patients was compared with and without IBS-like symptoms according to disease-specific inflammatory bowel disease questionnaire (IBDQ).
Depending on our research, IBS-like symptoms were found in 32% (18/56) of patients with inactive UC, 35% (29/81) of patients with inactive CD, and 13.8% (17/123) of control participants (P < .001). The QOL seemed to be significantly lower in both inactive UC and CD patients with IBS-like symptoms than in those without such symptoms (P < .001).
In conclusion, we defined that the prevalence of IBS-like symptoms in IBD patients in remission is 2 to 3 times higher than that in healthy control participants, and significantly lower IBDQ scores showed QOL was reduced in inactive IBD patients with IBS-like symptoms as compared with patients without IBS-like symptoms.
Keywords: inflammatory bowel disease, irritable bowel syndrome, prevalence, Rome IV
1. Introduction
Inflammatory bowel diseases (IBD), including ulcerative colitis (UC) and Crohn disease (CD), are mainly gastrointestinal tract pathologies presented by symptoms such as abdominal pain, chronic diarrhea, bloody stool, weight loss, and some extraintestinal manifestations.[1] The clinical course differs substantially, some patients experience frequent relapses, or some have long-standing complete remission, whereas some patients live with chronic active disease.[2] IBD has a significant lifelong impact on a patient's quality of life (QOL).[3] The QOL in IBD is mostly depended on the disease activity,[3] but large studies between IBD patients in long-standing remission and the general population are needed.
Irritable bowel syndrome (IBS) is a functional bowel disorder presented with abdominal discomfort or pain mainly associated with changing bowel habits.[4] There is a lot of different epidemiological study made by various definitive scale. In the general aspect, IBS seems to be the most common functional gastrointestinal disorder seen in both primary and secondary care.[5,6] Researchers defined that IBS affects about 10% of the general population in North America and Europe,[4,7] but the etiology behind the IBS remains obscure. In a study, nearly 25% of patients with IBS report the onset of their symptoms after an infectious process.[8] This fact has led to the hypothesis that IBS could be an inflammatory disorder.[9] Furthermore, a significant number of patients with IBD in remission phase demonstrate IBS-like bowel symptoms, without any signs of active inflammation.[10] However, Barbara et al[11] pointed out that previous transient or chronic inflammation can cause persistent gut dysfunction. Further studies showed that only some patients develop such chronic symptoms after an inflammatory or infectious process, mainly etiology is unclear, but psychological factors seem to have an important role.[12,13]
The relation between IBS-like symptoms and IBD patients in long-standing remission remains obscure. Recent reports showed that IBD could manifest IBS-like symptoms even after mucosal healing and complete long-standing remission achieved.[14–18] Persistent microinflammation and increased permeability of the gastrointestinal mucosa seems to be the potential cause.[19] IBS-like symptoms are thought to occur in higher prevalence in inactive IBD patients than in healthy controls.[20] In a study with the Swedish population, the reported prevalence of IBS-like symptoms in inactive IBD patients seemed to be 2 to 3 times higher than in the normal population.[16] Minderhoud et al[4] reported that one-third of UC patients also had IBS-like symptoms according to Rome II criteria. Most of the studies for understanding IBS-like symptoms in IBD patients in remission phase used the Rome II and Rome III criteria.[4,15,21]
In this study, we decided to assess this relationship with Rome IV criteria. IBD and functional gastrointestinal disorders such as IBS cause substantial morbidity and reduction in QOL[22] İnvestigation of QOL in patients with IBD by generic and disease-specific questionnaires is common. Those disorders cause significant disabilities in patients’ life and are responsible for increasing health-service budgets.[7,23]
Therefore, the aims of the present study were to determine the prevalence of IBS-like symptoms in a Turkish population with IBD in remission against control groups using Rome IV criteria and to assess the relation of IBS-like symptoms on the QOL of patients in the remission phase.
2. Methods
2.1. Participants
In this study, we consecutively enrolled 137 inactive IBD patients (56 with UC and 81 with CD) in our outpatient gastroenterology clinic of Dokuz Eylul University Hospital. The remission stage of IBD was defined as clinically inactive by the physician using specific activity indexes. For the evaluation of patients with CD, the Harvey-Bradshaw index was used and score ≤4 points defined as clinical remission. Harvey-Bradshaw index is a clinical disease activity indice that is determined by several clinical symptoms including general well-being, bowel habits, abdominal pain, abdominal mass, and such complications. For the evaluation of patients with UC, Modified Mayo Scoring System was used. According to the Modified Mayo Scoring system, remission is defined as having a disease-activity index of ≤2 points. Patients had surgery history excluded and also patients who have coexisting complicated comorbidities, colorectal cancer history, extraintestinal manifestations, alcohol and substance dependence history, and pregnant patients were excluded. Finally, 56 patients with UC and 81 with CD were admitted to be in long-standing remission and were included in the study. Total of 123 participants were selected as controls from participants who visited the internal medicine outpatient clinic of the same hospital during the same time duration. All participants were interviewed, and 2 questionnaires applied. IBS-like symptoms questioned by ROME IV criteria and QOL level evaluated by IBDQ.[17]
2.2. Instruments
ROME IV diagnostic questionnaire was used to evaluate IBS-like symptoms. Patients were accepted as having IBS-like symptoms who experienced recurrent abdominal pain, on average, at least 1 day/week in the last 3 months, associated with ≥2 of the following criteria: related to defecation, associated with a change in frequency of stool, associated with a change in the appearance of stool. Those criteria have to fulfill for the last 3 months with symptom onset at least 6 months before diagnosis.
Investigation of QOL in patients with IBD by generic and disease-specific questionnaire is common. In our population to determine QOL, we used disease-specific IBDQ,[24,25] which has been validated in the Turkish population as well. IBDQ measures include 36 multi-items that evaluate the individual's general well-being and QOL.
Consequently, we compared the control group and the inactive IBD patients based on the prevalence of IBS-like symptoms and total IBDQ score results for determining the QOL level. Besides, we obtained medical records of participants and compared age, sex, duration of disease, the location of disease, history of smoking, treatment history between participants with and without IBS-like symptoms.
2.3. Data analysis
All analyses were performed using the SPSS17 statistical package program. The normal distribution suitability of the numerical variables was tested with the Shapiro Wilk test. Numerical variables were described using mean and standard deviation, categorical variables using frequency and percentage values. Correlation between the categorical variables χ2 test, the relationship between numerical variables was investigated by Spearman correlation analysis. Two independent means were compared with the Mann–Whitney U test. Again the independent mean was compared with the posthoc Dunn test after the Kruskal–Wallis test. Statistical significance was defined as a value of P < 0.05.
2.4. Ethical considerations
This study was approved by the Ethics Committee of the Dokuz Eylul University Faculty of Medicine (2018/35–15), and before enrolling the participants in the study, written informed consent was obtained from all participations.
3. Result
3.1. Patients’ characteristics
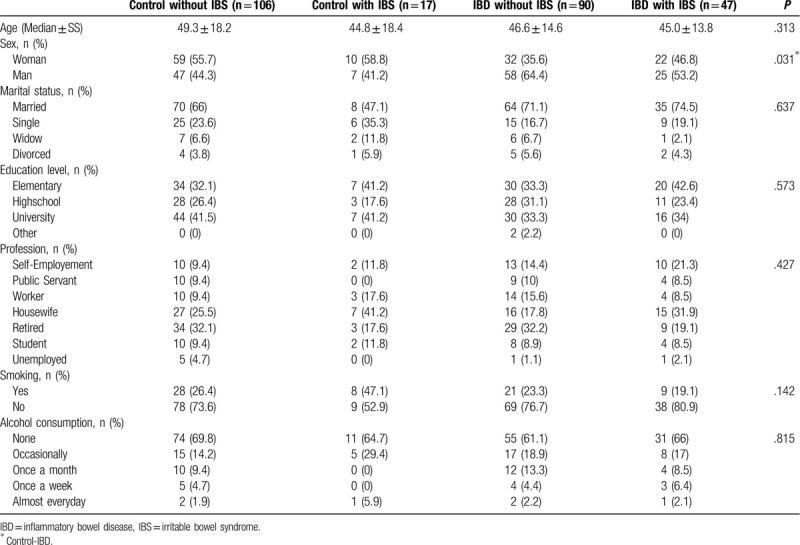
Data were analyzed from a total of 137 enrolled patients with inactive IBD, 81 had the inactive CD, and 56 had inactive UC and 123 control participants. The sample size detected after adequate power analysis. Study population enrolled 4 groups: control group, control group with IBS-like symptoms, inactive IBD patients without IBS-like symptoms, and inactive IBD patients with IBS-like symptoms. The demographic characteristics of our study population are shown in Table 1. Mean age was 49.3 ± 18.2 years in the control group, 44.8 ± 18.4 years in the control group with IBS-like symptoms, 46.6 ± 14,6 years in the inactive IBD patients without IBS-like symptoms, 45.0 ± 13.8 years in the inactive IBD patients with IBS-like symptoms. Adequate matching was achieved for sex and age. There was no statistical significance. Males accounted for 44.3% in the control group, 41.2% in the control group with IBS-like symptoms, 64.4% in the inactive IBD patients without IBS-like symptoms, 53.2% in the inactive IBD patients with IBS-like symptoms. The male dominance was found in the inactive IBD patients without IBS-like symptoms, and only statistically significance was found with the control group (P = .031). There is no statistical significance found between 4 groups in the marital status, history of smoking, education level, profession, and alcohol consumption.
Table 1.
Demographic characteristics of the participants.
3.2. IBS-like symptoms
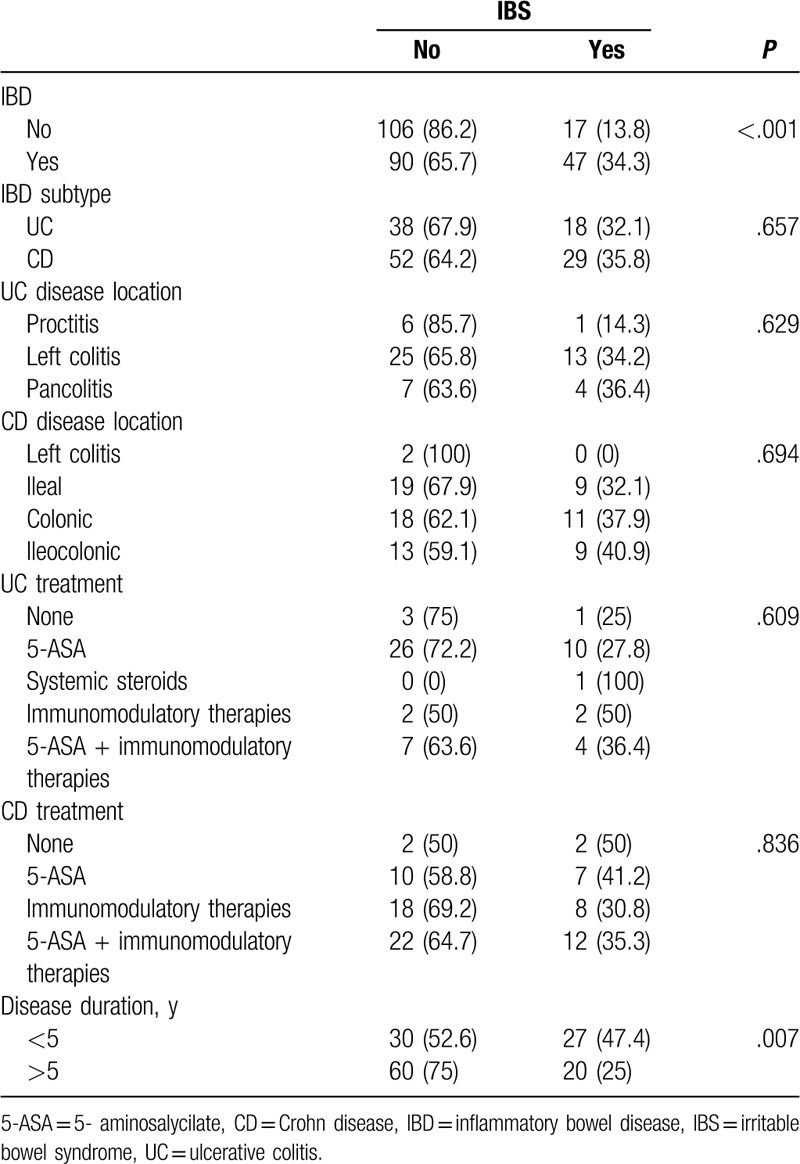
Using the Rome IV criteria, IBS-like symptoms were found in 34.3% (47/137) of patients with inactive IBD, but only 13.8% (17/123) of healthy control participants. Among inactive IBD patients, 32.1% (18/56) of inactive UC patients reported IBS-like symptoms, whereas this was reported by 35.8% (29/81) of inactive CD patients. Thus, we have defined that the prevalence of IBS-like symptoms in both UC and CD patients in remission was about 2 to 3 times higher than in control participants. This difference had a statistically significant (P < .001). However, when we compared UC and CD patients, there is no statistically significant difference found in IBS-like symptoms between these 2 groups. The characteristics of inactive IBD patients with and without IBS-like symptoms are shown in Table 2. The occurrence of IBS-like symptoms was unrelated to age, to the extent of the disease, and the use of chronic IBD treatment in both UC and CD patients. The duration of the disease seemed to be longer in patients with IBS-like symptoms, and statistically, significance was found (P = .007).
Table 2.
The characteristics of inactive IBD patients with and without IBS–like symptoms.
3.3. Quality of life findings
Inflammatory bowel disease questionnaire (IBDQ) is a disease-specific quality of life score which is validated in the Turkish population to asses QOL. Each question is scored from 1 to 7; total scores range from 36 to 252, with a higher score defining a more favorable quality of life and health state. Obtained scores of the IBDQ dimensions are depicted in Table 3.
Table 3.
Inflammatory bowel disease questionnaire mean scores in inactive IBD subtypes with and without irritable bowel syndrome-like symptoms comparison with disease characteristics.
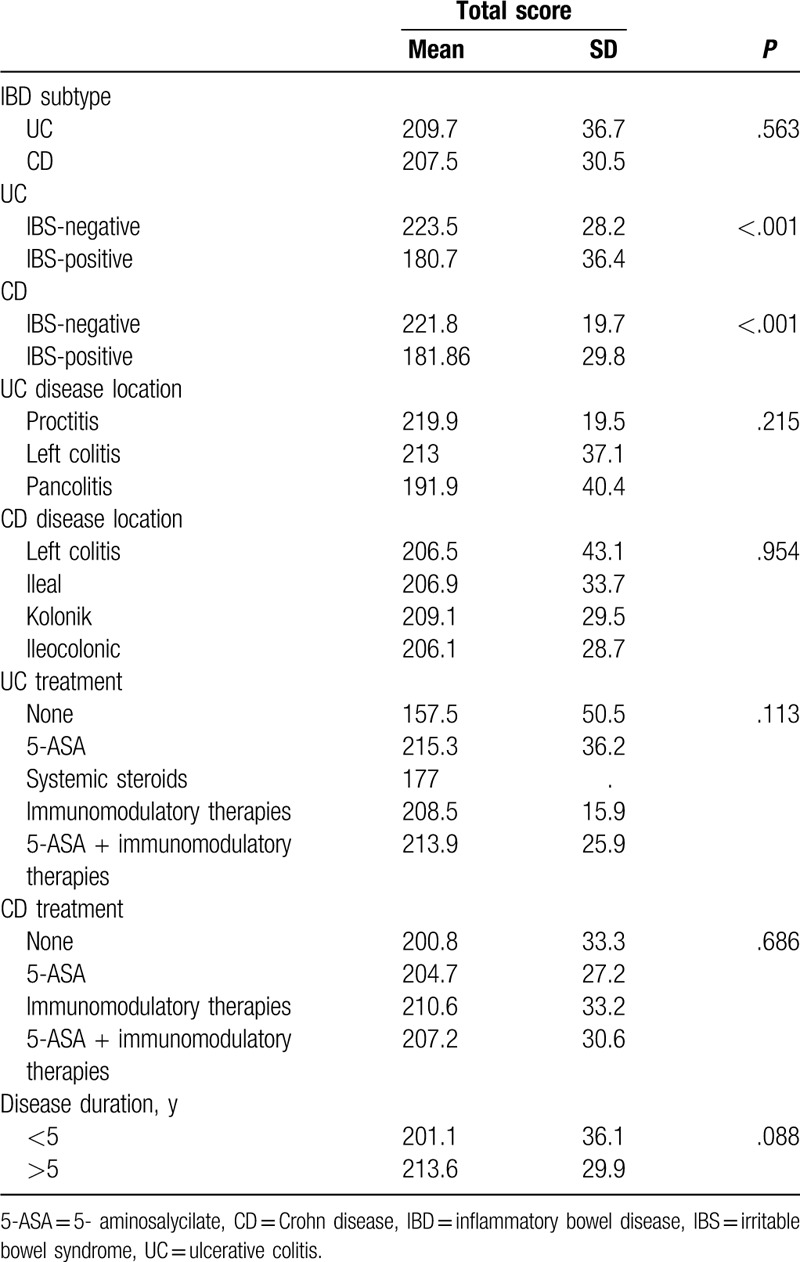
IBDQ score level was significantly lower in CD (181.86 ± 29.8 vs 221.8 ± 19.7; P < .001) and UC (180.7 ± 36.4 vs 223.5 ± 28.2; P < .001) patients with IBS-like symptoms than in those without IBS-like symptoms (Fig. 1).
Figure 1.
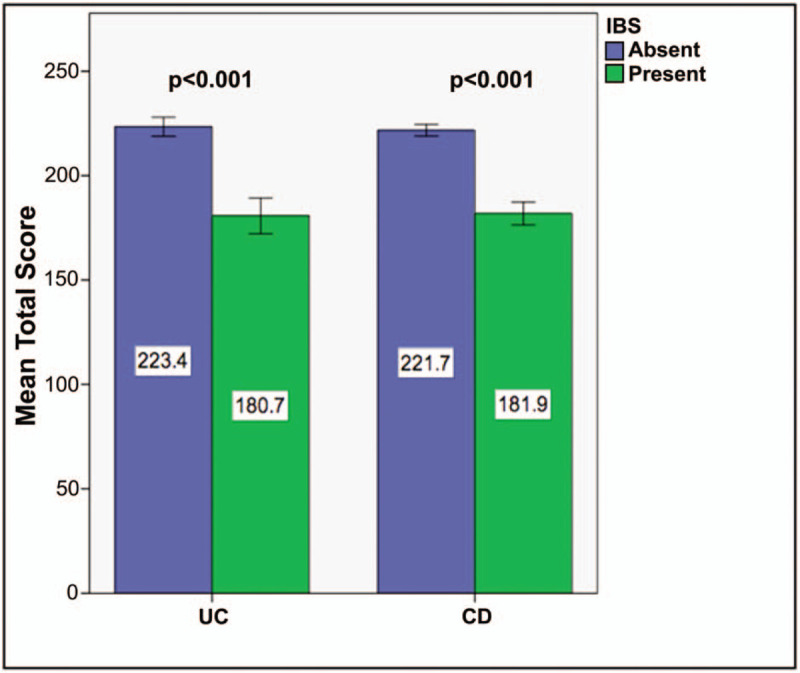
IBDQ score in inactive UC and CD patients with and without irritable bowel syndrome (IBS)-like symptoms. CD Crohn diease, IBDQ = Inflammatory Bowel Disease Questionnaire, IBS = irritable bowel syndrome, UC = ulcerative colitis.
There was no statistically significant difference in the total score between patients with UC and CD (209.7 ± 36.7 vs. 207.5 ± 7.5; P = .563). In the UC and CD patients in remission, we did not find obvious differences in total scores of the IBDQ, between disease duration, current treatment, and disease location.
4. Discussion
Rome IV diagnostic criteria underwent a final and were released in June 2016. In the present study, we made a definition of IBS-like symptoms using Rome IV diagnostic criteria[26] to investigate the prevalence of IBS-like symptoms both in inactive IBD patients and control participants. Currently, there is no large prevalence study released depend on Rome IV criteria. Depends on the current literature, our study has importance due to being a first IBS prevalence study evaluated by Rome IV criteria. Generally, the prevalence of IBS using the Rome III diagnostic criteria was reported to be about 10% to 15% in healthy control participants.[27,28] In this study, using Rome IV diagnostic criteria, IBS-like symptoms were found in 32% of patients with inactive ulcerative colitis, 35% of patients with inactive CD, and 13.8% of healthy control participants. We have shown that the prevalence of IBS-like symptoms in IBD patients in remission is about 2 to 3 times higher than in controls. Findings confirm previous reports indicating the high prevalence of IBS-like symptoms in IBD patients in different populations all around the world. In a study with the French population, the prevalence of IBS-like symptoms was 35.4% and 38% in inactive CD and UC patients, respectively.[19] Another prevalence study using Rome III criteria made with the Japanese population has shown that the prevalence of IBS-like symptoms 27.1% for inactive CD and 17.5% for inactive UC.[20] Because of the different diagnostic scoring system is used for diagnosis of IBS-like symptoms, true IBS prevalence is still unclear. Minderhoud et al[4] used Rome II criteria in their study, and they reported that one-third of the UC patients in long-standing remission suffer from IBS-like symptoms. Keohane et al[29] reported that 59.7% of inactive CD patients and 38.6% of inactive UC patients fulfilled the Rome II criteria for IBS. In another study, Simern et al[16] have used the gastrointestinal symptom rating scale to assess IBS-like symptoms, and they showed that the prevalence of IBS-like symptoms in IBD patients in long-standing remission is 2 to 3 times higher than in the normal population.
In our study, we strictly defined inactive IBD status, and we used Rome IV criteria for our diagnosis of IBS. In our population, the male/female ratio in both UC and CD patients with IBS seems equal, and it does not show any significant difference. But in a study of Anzari et al,[21] this ratio was >2 in patients with inactive UC. On the contrary, in another report from Pace et al,[30] female dominance has shown, and the proportion of female/male among UC patients with IBS was around 2. Most of the previous studies have reported a higher rate of IBS-like symptoms with CD than with UC. In our research, there was no statistically significant difference found in IBS-like symptoms between CD and UC. The possible reason could be we defined inactivity criteria strictly, those patients are in a long-standing remission phase, and we exclude the patients to have a history of surgery.
Currently, the mechanism of IBS-like symptoms’ impacts on IBD remains obscure. There are a lot of hypotheses considered by researchers. Despite no signs of active inflammation in inactive IBD patients, IBS-like symptoms tend to be at a higher frequency than the general population.[31] It may be argued that it is more challenging to exclude residual microinflammation in the mucosa of the patients in the remission phase, may there were no evidence of active inflammation detected by the physician. In the report from Keohane et al,[29] they defined inactive IBD as C-reactive protein (CRP) <10 mg/L, absence of the use of corticosteroids or biological agents over the previous 6 months, and CD activity index ≤150[11] or a UC activity index ≤3.[12] Ansari et al[21] defined inactive UC without inflammatory markers such as serum CRP level; they assessed by the number of bowel movements, the presence or absence of bloody stool, mucosal findings, and overall physician assessment based on the Mayo index. In our study, we defined inactive IBD status using Harvey Bradshaw index for CD and Modified Mayo Index for UC and physicians global assessment reviewed. Due to mucosal inflammation wasn’t under our scope, no firm conclusions regarding cause or effect can be drawn from this study. Still, we clearly detected that significant relation exist with IBD and IBS1-like symptoms even in the remission phase. In a study by Barbara et al[11] with mice detected that transient or chronic inflammation could lead to persistent gut dysfunction. However, only some of the patients after bacterial gastroenteritis develop long-standing gut dysfunction.[32] Researchers hypothesized that psychological and biological factors might contribute to the mechanism of the development of IBS-like symptoms after gastroenteritis.[13] In a study, Cremon et al[33] reported that some functional gastrointestinal disorders seemed to occur following childhood Salmonella-induced infectious enteritis. Keohane et al[29] showed that levels of the fecal calprotectin as a marker of microinflammation are significantly increased in IBD patients with IBS-like symptoms. Thus, residual microinflammation considered as the main trigger of IBS-like symptoms in a patient with inactive IBD.[34,35] In our study, we reported that the duration of disease was significantly longer in IBD patients with IBS-like symptoms than those without such symptoms. Long-term residual microinflammation may be related to the onset of IBS symptoms. Depending on a study of Nebot et al,[19] the occurrence of IBS-like symptoms in patients with inactive IBD is related to the persistent subclinical inflammation and persistent increase in tumor necrosis factorn α in colonic mucosa. It may contribute to the epithelial barrier defects and colonic paracellular permeability, which is similar in IBS patients. Clarification of the relationship between residual microinflammation and IBS-like symptoms needs further long-term study.
In this study, as a disease-specific quality of life questionnaire, IBDQ was used, and we compared findings for IBD patients with and without IBS symptoms. Our results have shown that significantly lower IBDQ scores found in both UC and CD patients with IBS-like symptoms as compared with patients without IBS-like symptoms. Furthermore, in the literature, patients with IBS-like symptoms demonstrated reduced well-being and lower levels of quality of life relative to those without IBS-like symptoms. Minderhoud et al[4] observed that the presence of IBS-like symptoms impaired the patient's quality of life. In another research, health-related QOL seemed to be significantly reduced in UC patients with IBS-like symptoms.[21] Also, in the literature, there is considerable evidence that the QOL in patients with IBD is impaired, and that patients with CD generally have poorer QOL than patients with UC.[3,36] However, in our study, the patients with UC reported similar general well-being and quality of life score as compared to patients with CD. No age difference was seen between different groups. Also, we did not find obvious differences in total scores of the IBDQ, between disease duration, current treatment, and disease location.
The present study has some potential limitations. First, we did not evaluate the microinflammation marker in this study, such as fecal calprotectin, CRP, colonoscopy. For illuminating pathophysiology behind IBS-like symptoms, detection of the mucosal change by biopsy in the future study will be reasonable.
5. Conclusions
In conclusion, with this present study, we reported that the prevalence of IBS-like symptoms in inactive IBD patients is 2 to 3 times higher than in healthy control participants, and significantly lower IBDQ scores showed QOL was reduced in inactive IBD patients with IBS-like symptoms as compared with patients without IBS-like symptoms. This study has importance due to being the first IBS prevalence study using Rome IV diagnostic questionnaire in the current literature. In order to no evidence of obvious disease activity in patients in long-standing remission, the main cause behind the pathophysiology of IBS-like symptoms could be residual microinflammation and transient or chronic inflammation. Further future studies with large study populations are needed for evaluating the pathophysiology of these symptoms and optimize the management of these patients.
Author contributions
Data curation: Muhammet Ozer, Rumeysa Colak.
Formal analysis: Muhammet Ozer, Goksel Bengi, Hale Akpinar.
Investigation: Muhammet Ozer, Goksel Bengi.
Methodology: Muhammet Ozer, Ozan Cengiz, Rumeysa Colak, Goksel Bengi, Hale Akpinar.
Project administration: Muhammet Ozer.
Resources: Muhammet Ozer, Rumeysa Colak, Goksel Bengi, Hale Akpinar, Ozan Cengiz.
Software: Muhammet Ozer.
Supervision: Goksel Bengi, Hale Akpinar.
Writing – original draft: Muhammet Ozer, Rumeysa Colak, Goksel Bengi, Ozan Cengiz, Hale Akpinar.
Writing – review & editing: Muhammet Ozer, Goksel Bengi, Rumeysa Colak, Ozan Cengiz, Hale Akpinar.
Footnotes
Abbreviations: CD = Crohn disease, IBD = inflammatory bowel disease, IBDQ = Inflammatory Bowel Disease Questionnaire, IBS = irritable bowel syndrome, QOL = quality of life, UC = ulcerative colitis.
How to cite this article: Ozer M, Bengi G, Colak R, Cengiz O, Akpinar H. Prevalence of irritable bowel syndrome-like symptoms using Rome IV criteria in patients with inactive inflammatory bowel disease and relation with quality of life. Medicine. 2020;99:19(e20067).
The authors report no conflicts of interest.
References
- [1].Kucharzik T, Maaser C, Lugering A, et al. Recent understanding of IBD pathogenesis: implications for future therapies. Inflamm Bowel Dis 2006;12:1068–83. [DOI] [PubMed] [Google Scholar]
- [2].Andres PG, Friedman LS. Epidemiology and the natural course of inflammatory bowel disease. Gastroenterol Clin North Am 1999;28:255–81. vii. [DOI] [PubMed] [Google Scholar]
- [3].Drossman DA, Patrick DL, Mitchell CM, et al. Health-related quality of life in inflammatory bowel disease. Functional status and patient worries and concerns. Dig Dis Sci 1989;34:1379–86. [DOI] [PubMed] [Google Scholar]
- [4].Minderhoud IM, Oldenburg B, Wismeijer JA, et al. IBS-like symptoms in patients with inflammatory bowel disease in remission; relationships with quality of life and coping behavior. Dig Dis Sci 2004;49:469–74. [DOI] [PubMed] [Google Scholar]
- [5].Mitchell CM, Drossman DA. Survey of the AGA membership relating to patients with functional gastrointestinal disorders. Gastroenterology 1987;92(5 pt 1):1282–4. [DOI] [PubMed] [Google Scholar]
- [6].Thompson WG, Heaton KW, Smyth GT, et al. Irritable bowel syndrome in general practice: prevalence, characteristics, and referral. Gut 2000;46:78–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Koloski NA, Talley NJ, Boyce PM. The impact of functional gastrointestinal disorders on quality of life. Am J Gastroenterol 2000;95:67–71. [DOI] [PubMed] [Google Scholar]
- [8].Chaudhary NA, Truelove SC. The irritable colon syndrome. A study of the clinical features, predisposing causes, and prognosis in 130 cases. Q J Med 1962;31:307–22. [PubMed] [Google Scholar]
- [9].Collins SM. Irritable bowel syndrome could be an inflammatory disorder. Eur J Gastroenterol Hepatol 1994;6:478–82. [Google Scholar]
- [10].Isgar B, Harman M, Kaye MD, et al. Symptoms of irritable bowel syndrome in ulcerative colitis in remission. Gut 1983;24:190–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Barbara G, Vallance BA, Collins SM. Persistent intestinal neuromuscular dysfunction after acute nematode infection in mice. Gastroenterology 1997;113:1224–32. [DOI] [PubMed] [Google Scholar]
- [12].Collins SM, McHugh K, Jacobson K, et al. Previous inflammation alters the response of the rat colon to stress. Gastroenterology 1996;111:1509–15. [DOI] [PubMed] [Google Scholar]
- [13].Gwee KA, Leong YL, Graham C, et al. The role of psychological and biological factors in postinfective gut dysfunction. Gut 1999;44:400–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Fukuba N, Ishihara S, Tada Y, et al. Prevalence of irritable bowel syndrome-like symptoms in ulcerative colitis patients with clinical and endoscopic evidence of remission: prospective multicenter study. Scand J Gastroenterol 2014;49:674–80. [DOI] [PubMed] [Google Scholar]
- [15].Piche T, Ducrotte P, Sabate JM, et al. Impact of functional bowel symptoms on quality of life and fatigue in quiescent Crohn disease and irritable bowel syndrome. Neurogastroenterol Motil 2010;22:626–e174. [DOI] [PubMed] [Google Scholar]
- [16].Simren M, Axelsson J, Gillberg R, et al. Quality of life in inflammatory bowel disease in remission: the impact of IBS-like symptoms and associated psychological factors. Am J Gastroenterol 2002;97:389–96. [DOI] [PubMed] [Google Scholar]
- [17].Halpin SJ, Ford AC. Prevalence of symptoms meeting criteria for irritable bowel syndrome in inflammatory bowel disease: systematic review and meta-analysis. Am J Gastroenterol 2012;107:1474–82. [DOI] [PubMed] [Google Scholar]
- [18].Farrokhyar F, Marshall JK, Easterbrook B, et al. Functional gastrointestinal disorders and mood disorders in patients with inactive inflammatory bowel disease: prevalence and impact on health. Inflamm Bowel Dis 2006;12:38–46. [DOI] [PubMed] [Google Scholar]
- [19].Vivinus-Nebot M, Frin-Mathy G, Bzioueche H, et al. Functional bowel symptoms in quiescent inflammatory bowel diseases: role of epithelial barrier disruption and low-grade inflammation. Gut 2014;63:744–52. [DOI] [PubMed] [Google Scholar]
- [20].Tomita T, Kato Y, Takimoto M, et al. Prevalence of irritable bowel syndrome-like symptoms in Japanese patients with inactive inflammatory bowel disease. J Neurogastroenterol Motil 2016;22:661–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Ansari R, Attari F, Razjouyan H, et al. Ulcerative colitis and irritable bowel syndrome: relationships with quality of life. Eur J Gastroenterol Hepatol 2008;20:46–50. [DOI] [PubMed] [Google Scholar]
- [22].Whitehead WE, Burnett CK, Cook EW, 3rd, et al. Impact of irritable bowel syndrome on quality of life. Dig Dis Sci 1996;41:2248–53. [DOI] [PubMed] [Google Scholar]
- [23].Leong SA, Barghout V, Birnbaum HG, et al. The economic consequences of irritable bowel syndrome: a US employer perspective. Arch Intern Med 2003;163:929–35. [DOI] [PubMed] [Google Scholar]
- [24].Guyatt G, Mitchell A, Irvine EJ, et al. A new measure of health status for clinical trials in inflammatory bowel disease. Gastroenterology 1989;96:804–10. [PubMed] [Google Scholar]
- [25].Russel MG, Pastoor CJ, Brandon S, et al. Validation of the Dutch translation of the Inflammatory Bowel Disease Questionnaire (IBDQ): a health-related quality of life questionnaire in inflammatory bowel disease. Digestion 1997;58:282–8. [DOI] [PubMed] [Google Scholar]
- [26].Schmulson MJ, Drossman DA. What is new in Rome IV. J Neurogastroenterol Motil 2017;23:151–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Miwa H. Prevalence of irritable bowel syndrome in Japan: Internet survey using Rome III criteria. Patient Prefer Adherence 2008;2:143–7. [PMC free article] [PubMed] [Google Scholar]
- [28].Kaji M, Fujiwara Y, Shiba M, et al. Prevalence of overlaps between GERD, FD and IBS and impact on health-related quality of life. J Gastroenterol Hepatol 2010;25:1151–6. [DOI] [PubMed] [Google Scholar]
- [29].Keohane J, O’Mahony C, O’Mahony L, et al. Irritable bowel syndrome-type symptoms in patients with inflammatory bowel disease: a real association or reflection of occult inflammation? Am J Gastroenterol 2010;105:1788.9-94; quiz 95. [DOI] [PubMed] [Google Scholar]
- [30].Pace F, Molteni P, Bollani S, et al. Inflammatory bowel disease versus irritable bowel syndrome: a hospital-based, case-control study of disease impact on quality of life. Scand J Gastroenterol 2003;38:1031–8. [DOI] [PubMed] [Google Scholar]
- [31].Agreus L, Svardsudd K, Nyren O, et al. Irritable bowel syndrome and dyspepsia in the general population: overlap and lack of stability over time. Gastroenterology 1995;109:671–80. [DOI] [PubMed] [Google Scholar]
- [32].Neal KR, Hebden J, Spiller R. Prevalence of gastrointestinal symptoms six months after bacterial gastroenteritis and risk factors for development of the irritable bowel syndrome: postal survey of patients. BMJ (Clinical research ed) 1997;314:779–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Cremon C, Stanghellini V, Pallotti F, et al. Salmonella gastroenteritis during childhood is a risk factor for irritable bowel syndrome in adulthood. Gastroenterology 2014;147:69–77. [DOI] [PubMed] [Google Scholar]
- [34].Jonefjall B, Strid H, Ohman L, et al. Characterization of IBS-like symptoms in patients with ulcerative colitis in clinical remission. Neurogastroenterol Motil 2013;25:756–e578. [DOI] [PubMed] [Google Scholar]
- [35].Mawe GM, Collins SM, Shea-Donohue T, et al. Changes in enteric neural circuitry and smooth muscle in the inflamed and infected gut. Neurogastroenterol Motil 2004;16: suppl 1: 133–6. [DOI] [PubMed] [Google Scholar]
- [36].Hjortswang H, Ström M, Almer S. Health related quality of life in Swedish patients with ulcerative colitis. Am J Gastroenterol 1998;93:2203–11. [DOI] [PubMed] [Google Scholar]


