Abstract
Background:
Nonadherence to prescribed therapy is a significant challenge at the primary healthcare level of South Africa. There are documented evidence of the potential impact of mobile health technology in improving adherence and compliance to treatment. This study assessed the effect of unidirectional text messaging on adherence to dietary and activity regimens among adults living with diabetes in a rural setting of Eastern Cape, South Africa.
Methods:
This was a 2-arm, multicenter, parallel, randomized controlled trial, involving a total of 216 patients with diabetes with uncontrolled glycemic status randomly assigned into the intervention (n = 108) and the control group (n = 108). Participants in the intervention arm received daily educational text messages on diabetes and reminders for 6 months, while the control arm continued with standard care only. A validated, self-developed adherence scale was used to assess participants’ adherence to diets and physical activity. Descriptive statistics and linear regression were used to assess changes in adherence and the effect of the intervention on adherence to therapy.
Results:
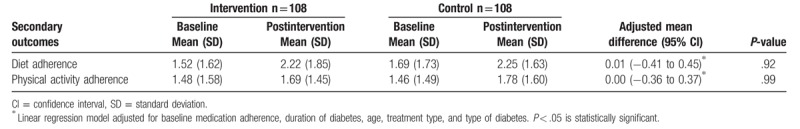
On a scale of 8, the mean medication adherence level for the intervention group was 6.90 (SD ± 1.34) while that of the control group was 6.87 (SD ± 1.32) with no statistical difference (P = .88). The adjusted mean change in the medication adherence level was 0.02 (−0.33 to 0.43) with no significant difference (P = .79). There was however a low level of adherence to dietary recommendations (1.52 ± 1.62), and physical activity (1.48 ± 1.58) at baseline, and both groups demonstrated a nonsignificant increase in dietary (P = .98) and physical activity adherence (P = .99) from baseline to the follow-up period.
Conclusion:
There is a moderate level of adherence to medication and a low level of adherence to dietary and physical activity recommendation in this setting. The text messaging intervention did not bring about any significant improvement in medication, dietary and physical activity adherence levels. There is a need to design effective strategies for improving adherence to recommended lifestyle changes in this setting.
Keywords: adherence, diabetes, diet, mobile health, physical activity, short message services, South Africa
1. Introduction
Treatment success is highly dependent on the level of adherence among patients.[1] Non-adherence to medication therapy is often associated with poor treatment outcomes, high healthcare costs, poor quality of life, worsening health of the individuals, development of complications, and ultimately death.[1–8] Generally, patients suffering from chronic conditions are reportedly non-adherents, with only half adhering in developed nations and a far lesser number in the developing worlds.[9,10]
Among patients with diabetes, adherence and compliance to treatment and other recommended therapy are quite important to achieve treatment targets; yet, reports show a low level of adherence among these patients.[11–13] Non-adherence among patients with diabetes contributes significantly to poor glycemic control, which gives rise to both microvascular and macrovascular complications.[14] These complications further impose a more significant burden on the individual, reduce their health-related quality of life, increase the risk of premature mortality, and impact tremendously on the already overstretched healthcare system.[15] Notably, adherence to treatment goes beyond medical therapy; it includes other forms of management such as the prescribed behavioral modifications, appointments, among others.[16]
Various barriers to adherence have been identified and these include poor communication between the healthcare provider and the patient, poor knowledge of the disease condition and the therapy, duration of drug use, complexity of the regimen, fear and experience of side effects, costs of medication, lack of trust in the physician, and lack of conviction on the need for treatment.[17–20] In addition, socio-demographic factors such as younger age, low level of education and low level of income also contribute to poor adherence rate among patients with diabetes.[15,21]
The need for a more convenient measure of assisting patients in adhering to treatment is of utmost importance,[22] and thus the emergence of mobile health (mHealth) technologies in improving health becomes imperative. According to World Health Organization (WHO), the use of mHealth to promote treatment compliance includes the use of phone calls, voice, or short message services (SMS) for transmitting reminder messages, to promote compliance to treatment, eradication of diseases, and scaling the challenges with drug resistance.[23] This has been demonstrated among individuals with various health conditions. For instance, in Europe, the use of mHealth was used as a measure for promoting treatment compliance among individuals with chronic illnesses such as diabetes, tuberculosis, human immunodeficiency virus/acquired immunodeficiency syndrome, obesity, asthma, and chronic obstructive pulmonary disease.[24–26] The same measure was also adopted in Czech Republic for reminding women to take their oral contraceptive pills, using SMS.[27] Likewise, this measure has been employed in New Zealand for smokers in the widely acclaimed and effective study called Txt2Quit, where smokers were sent support messages toward their attempt to quit smoking.[28] The same measure has been adopted and documented by few studies in Africa and other resource-poor settings and among different socio-economic groups.[29,30] However, there is hardly such measure in place in South Africa for chronic disease management, except the newly developed website, solely developed for assessing people for diabetes,[31] which may also not be accessible to those in rural areas.
Concerning the use of SMS reminders as a measure of promoting medication adherence among patients with diabetes, Vervloet et al[32] documented a significant improvement in medication adherence among patients living with diabetes in the Netherlands following 6 months of sending SMS reminders. However, Arora et al[33] showed a non-significant improvement in medication adherence among low-income Latino patients with diabetes following a unidirectional text messaging intervention. Similarly, another study conducted among Asian-Indian patients with diabetes showed a non-significant improvement in the number of annual check-up and adherence with dietary prescriptions.[34] This also corroborates the findings of Sugita et al[35] among Japanese patients with diabetes. Obviously, there are conflicting results on the impact of text messaging on adherence and compliance to therapy, and more importantly so, there is a gap in knowledge on this measure in the sub-Saharan African settings, including South Africa. This study sought to determine effect of a unidirectional text messaging on adherence to recommended diets and activity among patients with diabetes attending primary healthcare clinics in a low-resource setting of Eastern Cape, South Africa. The Eastern Cape Province suffers a great deal of diabetes burden and a high level of suboptimal control. The findings of this study could inform public health policy and provide guidance for improvement in clinical guidelines and practice, if proven to be effective.
2. Methods
2.1. Study design
A multicenter, 2-arm, parallel, randomized controlled trial design was adopted to assess the efficacy of a 6-month mobile phone SMS intervention in addition to standard diabetes care in improving adherence to recommended therapy among patients diabetes in low-resource settings of South Africa.
2.2. Study setting
The study was conducted at the outpatient departments of 6 selected primary healthcare centers in 2 health districts in Eastern Cape, South Africa. The Eastern Cape Province was created in 1994, and includes areas from the Xhosa homelands of the Transkei and Ciskei, as well as part of the Cape Province. The Eastern Cape Province is made up of 2 metropolitan municipalities; Buffalo City and the Nelson Mandela Bay Metropolitan Municipality and 6 district municipalities: Alfred Nzo, Amathole, Chris Hani, Joe Gqabi, Oliver Reginald Tambo, and Sarah Baartman.[36] The study was conducted at 6 selected primary healthcare centers out-patient departments in Buffalo City Municipality and Amathole Districts, of the Eastern Cape Province, South Africa.
2.3. Study population
This study forms part of a larger study which assessed the efficacy, acceptability, and feasibility of mHealth in improving adherence to antidiabetic therapy and glycemic control. The study population were adults with uncontrolled diabetes attending the selected primary healthcare clinics in Buffalo City Metropolitan Municipality and Amathole health districts, who met the eligibility criteria.
2.4. Inclusion criteria
The inclusion criteria were age 18 years and above; diagnosed of diabetes at least in the last 6 months; currently receiving treatment at selected clinics; on a stable medication for at least 3 months prior to recruitment; a HbA1c level >7% or a fasting blood sugar >7.0 mmol/L, morning random blood sugar more than 10 mmol/L; possession of a mobile phone with ability to retrieve and read SMS or have someone who is available to help with reading the SMS daily; willingness to receive SMS for the period of the study.
2.5. Exclusion criteria
Participants were excluded if they had health or mental conditions that could interfere with the study or the ability to use the mobile phone or comprehend messages, pregnancy or plan to fall pregnant in the next 6 months, debilitated or handicapped in such a way that obtaining anthropometric measurements could be challenging.
Eligible participants were recruited sequentially at the selected health facilities on the clinic days. The recruitment process started in July and August 2018. Intervention commenced in September 2018 to February 2019. Postintervention data collection commenced in March and April 2019.
2.6. Sample size calculation
Considering the mean baseline physical activity adherence of 1.48 (±1.58) among the study participants, we assume the standard care improves the adherence level by 0.5 and the intervention adds an extra 0.5. At a standard deviation of 1 and an alpha error level of 5%, the calculation gives a power of 90% with just 78 patients in each arm of the study. Thirty percent loss to follow-up was anticipated and a final sample size of 105 participants were required in each group.[37]
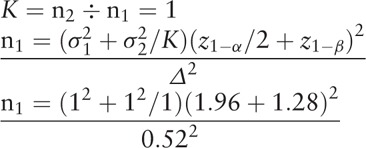 |
where n1 = 78, n2 = K∗n1 = 78, Δ = |μ2 − μ1| = absolute difference between 2 mean values, σ1, σ2 = variance of mean #1 and #2, n1 = sample size for group #1, n2 = sample size for group #2, α = probability of type I error (usually 0.05), β = probability of type II error (usually 0.2), z = critical Z-value for a given α or β, and k = ratio of sample size for group #2 to group #1.
2.7. Randomization
The guideline for the management of diabetes is the same across all the primary healthcare facilities in South Africa,[38] thus all clinics were considered eligible; although the quality of care might vary across various health facilities as a result of available infrastructures as well as the available human resources and the experiences of the care providers. Of all the 8 health districts, 2 were conveniently selected, out of which 6 clinics were randomly selected. Demographic and other basic information were obtained to screen for eligible participants from the selected clinics. From the sample size calculation, 108 participants was required in each arm of the study; therefore, 36 participants are required from each of the 6 selected clinics. Thirty-six participants were randomly selected from the list of eligible participants from each clinic, adjusting for age and mean duration of diabetes. Baseline data were obtained from the randomly selected participants, after which individuals were randomly assigned to either the intervention or the control arm using their assigned identification number, following a simple randomization technique, with a 1:1 allocation ratio. Participants in the intervention arm were then contacted to ascertain their preferences in terms of the preferred language of communication; either the locally spoken isiXhosa language or English, preferred time of receiving SMS, name, and contact of next of kin or the available support person. The flowchart for the recruitment, randomization, allocation, and retention of study participants is shown in Figure 1.
Figure 1.
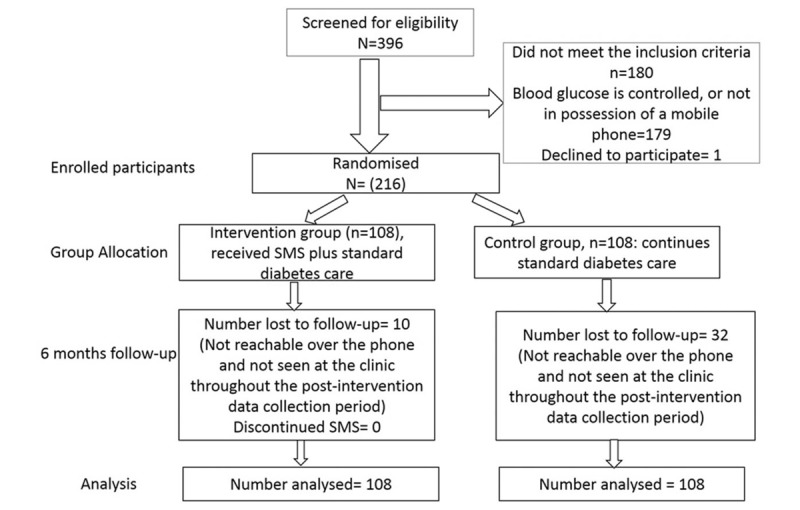
Flowchart of study participants.
2.8. Blinding
The study statistician involved in the randomization was blinded to every identifying information to avoid bias. Due to the nature of the study, it was impossible for the research staff conducting the SMS intervention as well as the participants in the intervention arm to be blinded to the intervention; however, participants in the control arm were blinded to the intervention. The participants involved in the intervention were privately contacted after randomization to remind them of the intervention process and aim. Also, the outcome measure, medication adherence was blinded to treatment allocation.
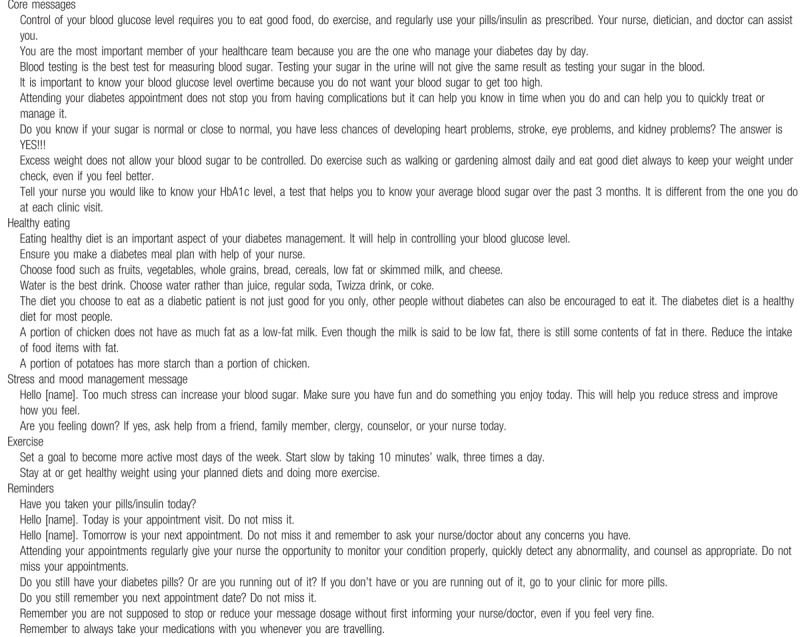
2.9. SMS development
The principal investigator, supervisor, family physician, and a nurse developed the contents of the SMS. The team followed the Society for Endocrinology, Metabolism and Diabetes of South Africa guideline for the management of diabetes, the health education materials from the National Diabetes Education Programme and some sample messages from the previously documented studies which were documented to be efficient.[30] Also, the healthcare needs as well as the observed gaps in the baseline date influenced the content of the SMS. The SMS was developed in English and translated to isiXhosa by a professional translator. The 2 versions of the messages were then pretested by sending them out to various people, including those with little or no level of education, to ascertain whether it is easy, simple, and clear. Modifications were made using various feedbacks received. Some examples of the sent text messages are presented in Table 1.
Table 1.
Examples of short message service contents.
2.10. Data collection
The assessment of medication adherence was conducted at baseline and at 6 months after randomization. At baseline, demographic data such as age, gender, level of education, employment status, and average monthly income were obtained using a validated questionnaire via face-to-face interviews. Clinical history, such as duration of illness and presence of comorbidity, was obtained through the review of clinical records.
Participants’ adherence to diets and activity was assessed with a self-developed questionnaire. The 7-item instrument addresses diverse measures through which patients do not comply with recommended therapy such as forgetfulness, carelessness, or assumption of improved health or deterioration of health or users’ feelings. Each of the items had a “Yes” or “No” response. The questions with the Yes/No responses were: Are there times when you do not remember to follow recommended diets? Was there any day in the past week that you just decided not follow your recommended diets? Was there any time you stopped the recommended diets because you did not enjoy it? Was there any time you decided not to follow recommended diets because you felt your sugar is now controlled? Is the need to comply with recommended diets stressing you? Did you follow the recommended diets yesterday?
The same scale was modified to assess adherence to recommended physical activity. The modified scale consisted of 7 items, and the alpha coefficient value was 0.68 for the physical activity scale and 0.64 for the diet scale. Apart from the alpha coefficient level of the scale, the face, content, and construct validity of the scale provides an acceptable level of validity and reliability of the scales as measures of adherence in the various aspects of recommended healthcare regimen.
2.11. Study intervention procedure
Both the intervention and the control groups proceeded with their usual care including all medical visits, tests, and diabetes support programs. In addition, the intervention group received short message services (SMS) at an agreed time of the day, tailored according to their needs, care plan, and goals. Participants also received reminders, motivational and support messages, and advice on lifestyle behaviors like diets, physical activity, smoking cessation, medication, and appointment reminders. Text messages were sent through an online bulk messages platform, which allow messages to be scheduled for a specific time, and show the message delivery status. Participants in the control arm only continued with their usual diabetes care at their clinics.
2.12. Ethical considerations
University of Fort Hare Research Ethics Committee granted the ethical approval for this study. Approval was also sought from the Eastern Cape Departments of health, included health districts as well as the clinic managers. Verbal and written informed consent was obtained from the participants prior to the commencement of the study, after due explanation of the research purpose and aims. Rights to anonymity and confidentiality were ensured throughout the study and participants consented to referral to further care in case of detection of abnormal findings.
2.13. Data analysis
Statistical analysis followed the intention-to-treat principle. Descriptive statistics were used to summarize the demographic and baseline characteristics. Continuous variables were summarized as numbers of observed values, means, standard deviation, minimum, and maximum. Categorical variables were described as frequency and percentages. Chi-squared and Fisher exact test were used to assess the difference between groups for categorical baseline variables. For continuous variables, analysis of variance was used to assess the difference in the baseline characteristics of the study participants between the intervention and control groups. Linear regression was used to examine the effect of the intervention on adherence between the groups and 2 periods. The assumption underlying the analysis of missing variables was that the data were missed completely at random. Missing data were imputed for using the mean score. Sensitivity analyses were performed using a complete case analysis and the worst case scenario. All statistical tests were 2-sided at 5% significance level. A P-value of <.05 was considered statistically significant. The Statistical Package for Social Sciences (SPSS) version 23 was used for data analysis (SPSS Inc, Chicago, IL).
3. Results
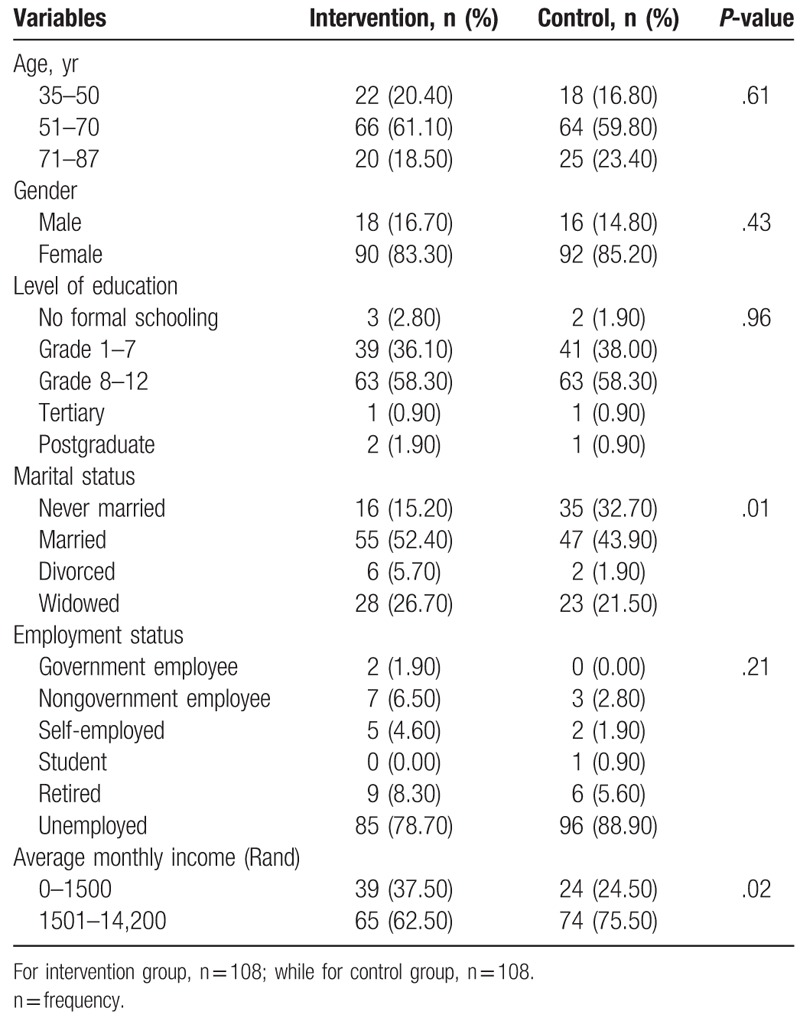
Of the 216 participants, 108 were in the intervention arm and 108 in the control arm. For both the intervention and control groups, majority of the participants were females (83.30% vs 85.20%). More than half of the study participants had secondary level of education (58.30% vs 58.30%), and the majority had no form of employment (78.70%; 88.90%). Overall, the mean age of the participants was 60.64 (standard deviation [SD] ±11.58) years, while the mean income per month was 108.45 (SD ±120.20) United States Dollars (Table 2).
Table 2.
Demographic characteristics of study participants by study groups.
The majority of the participants had type 2 diabetes (97.20% vs 90.70%) for both the intervention and control groups, were on oral pills (76.90% vs 74.10%), had concomitant hypertension (80.60% vs 85.50%), and were receiving treatment for hypertension (75.00% vs 86.80%). Only a small percentage of the participants had no health comorbidity; 27.80% and 16.70% for the intervention and control groups, respectively. The mean duration of diabetes was 9.06 (SD ±7.38) years, while that of diabetes treatment was 8.81 (SD ±7.20) years.
On a scale of 1 to 8, the mean medication adherence level for both groups was 6.88 (SD ±1.33).
Table 3 shows a low level of adherence to dietary recommendations, and physical activity among both groups demonstrated a slight increase from baseline to follow-up period. Nonetheless, there was no significant difference in the mean change in dietary adherence (P = .98) and physical activity adherence (P = .99) between those in the control and the intervention arm (Table 3).
Table 3.
Impact of short message services intervention on participants’ adherence level.
4. Discussion
Patients suffering from chronic diseases, especially those in the developing nations, have a low level of adherence to therapy.[9] In this study, there was a moderate level of adherence to medication use among participants. However, adherence to dietary regimen and physical activity was extremely low, both among the study participants in the intervention and the control arm. This is a source of concern as both pharmacotherapy and lifestyle modifications are required to attain good health outcomes and adequate glycemic control.[14] Thus the intervention was targeted at the low level of adherence to diets and physical activity.
The SMS intervention did not bring about any significant improvement in the participants’ level of adherence to dietary recommendations. The probable explanation for this could be the inability of the text messaging to address the various underlying factors for low adherence to dietary recommendations within the short period. For instance, the most cited reasons for nonadherence with dietary recommendations were inadequate knowledge and high cost of healthy diets. Although, evidence from the participants’ responses on how helpful the text messaging intervention was showed that the SMS intervention has great potential for improving dietary knowledge, and this may consequently improve adherence, if continued for a longer period. However, high cost of healthy diets cannot be easily influenced by text messaging. Probably, government policies and interventions which could increase the availability of healthy food items to the populace might play an important role, even though this might not be realizable within a short period. Another possible reason for the poor adherence to dietary recommendation is the cultural beliefs and practices of the patients. Some authors already documented some unhealthy dietary practices such as over-eating and binge eating among black Africans, which they also further linked to stress.[39,40] Clinicians should develop more culturally acceptable, motivating, and practical strategies that frequently reinforces the importance of healthy dietary practices. For example, cooking classes that demonstrates ways of adopting the locally available food items to suit the nutritional requirements of the patients could be of help.
Finally, the study recorded a low level of adherence to recommended physical activity, which also did not improve after the text messaging intervention. This is concerning, given the significant role of physical activity on cardio-metabolic health.[41,42] Evidence gathered from the study showed that lack of time as well as ill-health were the major factors contributing to the high level of physical inactivity among the participants. Aside this, a large number of the participants do not particularly see the need to exercise. A physical activity model developed by Cox already opined that knowledge of exercise might not translate into uptake as there are several interconnected factors which include social, environmental, personal, and internal factors.[43] There is a need to feel motivated to do exercise and also enjoy exercising to regularly engage in it.[44] As indicated by Horne et al,[45] apart from the motivation to exercise offered by the health workers or text messaging, supports from family members also play a crucial role in patients’ decisions to engage in exercise. This gap was not covered by the SMS intervention as the messages were basically targeted at the patients and further encouragement from family members could have gone a long way in bringing out a change. There exist a conflict on the role of health status on activity pattern. While some believe poor health status could motivate chronic patients to engage more in activities,[46] we found that poor health is one of the reasons why participants in this study did not engage in physical activity regularly (unpublished data), despite the messages encouraging them to commence activities slowly and as tolerated. The government also has some important roles to play in promoting activity uptake by providing physical activity equipment and facilities, creating a safe neighborhood for exercising and employment of more professional exercise trainers who will provide more individualized guidance to patients,[46,47] especially in rural settings.
4.1. Strengths and limitations
The main limitation was the use of self-reported measure of assessing adherence which has a potential of response bias. In addition, the loss to follow-up might have constituted a threat, although we conducted sensitivity analyses, which showed similar outcome. Further, only few of the clinics in the selected districts, and only 2 of the 8 health districts in the province were sampled, thus, we cannot generalize the findings to the entire province. Notwithstanding the limitations of the study, the experimental design employed and the use of a multicenter approach provides strength to the study. Finally, the finding of this study could serve as a reference point for other related studies in the province, and even in the South African context.
5. Conclusion
There is a moderate level of adherence to medication and a low level of adherence to dietary and physical activity recommendations in this setting, which were partly related to health, cultural and socioeconomic factors. The text messaging intervention did not bring about any significant improvement in the dietary and physical activity adherence levels. There is a need to design more effective strategies for improving adherence to recommended lifestyle changes in this setting.
Acknowledgments
The authors are grateful to all study participants for their patience and time. Likewise, they appreciate the management and staff of the various healthcare facilities who took part in this study as well as the clinicians who contributed in one way or the other to the study.
Author contributions
Conceptualization: Eyitayo Omolara Owolabi, Daniel Ter Goon.
Data curation: Eyitayo Omolara Owolabi, Anthony Idowu Ajayi.
Formal analysis: Eyitayo Omolara Owolabi, Anthony Idowu Ajayi.
Investigation: Eyitayo Omolara Owolabi.
Methodology: Eyitayo Omolara Owolabi, Anthony Idowu Ajayi.
Project administration: Eyitayo Omolara Owolabi.
Supervision: Daniel Ter Goon.
Writing – original draft: Eyitayo Omolara Owolabi.
Writing – review & editing: Eyitayo Omolara Owolabi, Daniel Ter Goon, Anthony Idowu Ajayi.
Eyitayo Omolara Owolabi orcid: 0000-0001-5575-7842.
Footnotes
Abbreviations: mHealth = mobile health, SEMDSA = Society for Endocrinology, Metabolism and Diabetes of South Africa, SMS = short message services, SPSS = Statistical Package for Social Sciences, WHO = World Health Organization.
How to cite this article: Owolabi EO, Goon DT, Ajayi AI. Impact of mobile phone text messaging intervention on adherence among patients with diabetes in a rural setting: a randomized controlled trial. Medicine. 2020;99:12(e18953).
EOO received a doctoral study grant from the South African National Research Foundation.
The study protocol and data will be made available by the principal investigator upon reasonable request.
The authors have no conflicts of interest to disclose.
References
- [1].Jimmy B, Jose J. Patient medication adherence: measures in daily practice. Oman Med J 2011;26:155–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].DiBonaventura DM, Copher R, Basurto E, et al. Patient preferences and treatment adherence among women diagnosed with metastatic breast cancer. Am Health Drug Ben 2014;7:386–96. [PMC free article] [PubMed] [Google Scholar]
- [3].Egede LE, Gebregziabher M, Dismuke CE, et al. Medication nonadherence in diabetes: longitudinal effects on costs and potential cost savings from improvement. Diabetes Care 2012;35:2533–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Egede LE, Gebregziabher M, Echols C, et al. Longitudinal effects of medication nonadherence on glycemic control. Ann Pharmacother 2014;48:562–70. [DOI] [PubMed] [Google Scholar]
- [5].Jha AK, Aubert RE, Yao J, et al. Greater adherence to diabetes drugs is linked to less hospital use and could save nearly $5 billion annually. Health Aff 2012;31:1836–46. [DOI] [PubMed] [Google Scholar]
- [6].Nasseh K, Frazee SG, Visaria J, et al. Cost of medication nonadherence associated with diabetes, hypertension, and dyslipidemia. Am J Pharm Benefits 2012;4:e41–7. [Google Scholar]
- [7].Roebuck MC, Liberman JN, Gemmill-Toyama M, et al. Medication adherence leads to lower health care use and costs despite increased drug spending. Health Aff 2011;30:91–9. [DOI] [PubMed] [Google Scholar]
- [8].Polonsky WH, Henry RR. Poor medication adherence in type 2 diabetes: recognizing the scope of the problem and its key contributors. Patient Prefer Adherence 2016;10:1299–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Cramer JA, Benedict A, Muszbek N, et al. The significance of compliance and persistence in the treatment of diabetes, hypertension and dyslipidaemia: a review. Int J Clin Pract 2008;62:76–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Osterberg L, Blaschke T. Adherence to medication. N Engl J Med 2005;353:487–97. [DOI] [PubMed] [Google Scholar]
- [11].Eaddy MT, Cook CL, O’Day K, et al. How patient cost-sharing trends affect adherence and outcomes: a literature review. Pharm Ther 2012;37:45–55. [PMC free article] [PubMed] [Google Scholar]
- [12].Bagonza J, Rutebemberwa E, Bazeyo W. Adherence to anti diabetic medication among patients with diabetes in eastern Uganda; a cross sectional study. BMC Health Serv Res 2015;15:168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Kagee A. Treatment adherence in South African primary health care. S Afr Fam Pract 2004;46:26–30. [Google Scholar]
- [14].Kirkman MS, Rowan-Martin MT, Levin R, et al. Determinants of adherence to diabetes medications: findings from a large pharmacy claims database. Diabetes Care 2015;38:604–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Nolan CJ, Damm P, Prentki M. Type 2 diabetes across generations: from pathophysiology to prevention and management. Lancet 2011;378:169–81. [DOI] [PubMed] [Google Scholar]
- [16].Garcia-Perez LE, Alvarez M, Dilla T, et al. Adherence to therapies in patients with type-2 diabetes. Diabetes Ther 2013;4:175–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Coleman CI, Limone B, Sobieraj DM, et al. Dosing frequency and medication adherence in chronic disease. J Manag Care Pharm 2012;18:527–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].de Vries ST, Keers JC, Visser R, et al. Medication beliefs, treatment complexity, and non-adherence to different drug classes in patients with type 2 diabetes. J Psychosom Res 2014;76:134–8. [DOI] [PubMed] [Google Scholar]
- [19].Gadkari AS, McHorney CA. Medication nonfulfillment rates and reasons: narrative systematic review. Curr Med Res Opin 2010;26:683–705. [DOI] [PubMed] [Google Scholar]
- [20].Walz L, Pettersson B, Rosenqvist U, et al. Impact of symptomatic hypoglycemia on medication adherence, patient satisfaction with treatment, and glycemic control in patients with type 2 diabetes. Patient Prefer Adherence 2014;8:593–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Curkendall SM, Thomas N, Bell KF, et al. Predictors of medication adherence in patients with type 2 diabetes mellitus. Curr Med Res Opin 2013;29:1275–86. [DOI] [PubMed] [Google Scholar]
- [22].Nieuwlaat R, Wilczynski N, Navarro T, et al. Interventions for enhancing medication adherence. Cochrane Database Syst Rev 2014;CD000011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].World Health Organization. mHealth: new horizons for health through mobile technologies. mHealth: new horizons for health through mobile technologies. Geneva, Switzerland, 2011 [Google Scholar]
- [24].Holtz B, Whitten P. Managing asthma with mobile phones: a feasibility study. Telemed J E Health 2009;15:907–9. [DOI] [PubMed] [Google Scholar]
- [25].Liu WT, Huang CD, Wang CH, et al. A mobile telephone-based interactive self-care system improves asthma control. Eur Respir J 2011;37:310–7. [DOI] [PubMed] [Google Scholar]
- [26].Quinn CC, Shardell MD, Terrin ML, et al. Cluster-randomized trial of a mobile phone personalized behavioral intervention for blood glucose control. Diabetes Care 2011;34:1934–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Corker J. Ligne Verte” toll-free hotline: using cell phones to increase access to family planning information in the Democratic Republic of Congo. Cases Pub Health Comm Market 2010;4:23–37. [Google Scholar]
- [28].Li J. Mobile phones and the Internet as quitting smoking aids. Cases in Pub Health Comm Market 2009;3:204–18. [Google Scholar]
- [29].Pop-Eleches C, Thirumurthy H, Habyarimana JP, et al. Mobile phone technologies improve adherence to antiretroviral treatment in a resource-limited setting: a randomized controlled trial of text message reminders. AIDS (London, England) 2011;25:1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Islam SMS, Niessen LW, Ferrari U, et al. Effects of mobile phone SMS to improve glycemic control among patients with type 2 diabetes in Bangladesh: a prospective, parallel-group, randomized controlled trial. Diabetes Care 2015;38:e112–3. [DOI] [PubMed] [Google Scholar]
- [31].Chowles T. Merck Launches Diabetes mHealth Programme. eHealth News, South Africa, February 22, 2016. Available at: https://ehealthnews.co.za/merck-diabetes-mhealth-programme/. Accessed April 27, 2019. [Google Scholar]
- [32].Vervloet M, van Dijk L, Santen-Reestman J, et al. SMS reminders improve adherence to oral medication in type 2 diabetes patients who are real time electronically monitored. Int J Med Inform 2012;81:594–604. [DOI] [PubMed] [Google Scholar]
- [33].Arora S, Peters AL, Burner E, et al. Trial to examine text message-based mHealth in emergency department patients with diabetes (TExT-MED): a randomized controlled trial. Ann Emerg Med 2014;63:745–54. [DOI] [PubMed] [Google Scholar]
- [34].Shetty AS, Chamukuttan S, Nanditha A, et al. Reinforcement of adherence to prescription recommendations in Asian Indian diabetes patients using short message service (SMS)—a pilot study. J Assoc Physicians India 2011;59:711–4. [PubMed] [Google Scholar]
- [35].Sugita H, Shinohara R, Yokomichi H, et al. Effect of text messages to improve health literacy on medication adherence in patients with type 2 diabetes mellitus: a randomised controlled pilot trial. Nagoya Med J 2017;79:313–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Statistics South Africa South African Statistics, 2011. South Africa, 1-190. Available at: http://www.statssa.gov.za/publications/SAStatistics/SAStatistics2011.pdf 2011. Accessed 18 June, 2019. [Google Scholar]
- [37].Kane SP. Sample Size Calculator. ClinCalc. Available at: https://clincalc.com/stats/SampleSize.aspx. Updated November 10, 2018. Accessed July 17, 2019. [Google Scholar]
- [38].Amod A, Motala A, Levitt N, et al. Type 2 diabetes guideline. Journal of Endocrinology, Metabolism and Diabetes of South Africa, 17:S1–94.arwaha A. Health advice smartphone app launches in South Africa. Technology. Available at: http://www.bbc.co.uk/news/10407081 Accessed September 18, 2019. [Google Scholar]
- [39].Bowleg L. The problem with the phrase women and minorities: intersectionality-an important theoretical framework for public health. Am J Public Health 2012;102:1267–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Assari S, Lee DB, Nicklett EJ, et al. Racial discrimination in health care is associated with worse glycemic control among black men but not black women with type 2 diabetes. Front Public Health 2017;5:235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Miltona K, Macnivenb R, Bauman A. Review of the epidemiological evidence for physical activity and health from low- and middle-income countries. Glob Public Health 2014;9:369–81. [DOI] [PubMed] [Google Scholar]
- [42].Wen CP, Wai JPM, Tsai MK, et al. Minimum amount of physical activity for reduced mortality and extended life expectancy: a prospective cohort study. Lancet 2011;378:1244–53. [DOI] [PubMed] [Google Scholar]
- [43].Cox CL. An interaction model of client behaviour: the theoretical prescription for nursing. Adv Nurs Sci 1982;5:41–56. [DOI] [PubMed] [Google Scholar]
- [44].Monakali S, Goon DT, Seekoe E, et al. Health-promoting lifestyle behaviours among primary healthcare professional nurses in Eastern Cape Province, South Africa. Glob J Health Sci 2018;11:92. [Google Scholar]
- [45].Horne M, Skelton DA, Speed S, et al. The influence of primary health care professionals in encouraging exercise and physical activity uptake among white and South Asian older adults: experiences of young older adults. Patient Educ Couns 2010;78:97–103. [DOI] [PubMed] [Google Scholar]
- [46].Gobbi S, Sebastião E, Papini CB, et al. Physical inactivity and related barriers: a study in a community dwelling of older. J Aging Res 2012;2012:685190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Costello E, Kafchinski M, Vrazel J, et al. Motivators, barriers, and beliefs regarding physical activity in an older adult population. J Geriatr Phys Ther 2011;34:138–47. [DOI] [PubMed] [Google Scholar]


