The world is currently facing the COVID-19 pandemic and countries are one-by-one increasing restrictive measures on their populations. To avoid rapid transmission of the virus, governmental authorities have had to impose nationwide lockdowns. Humans were asked to be patient and stay inside their home, imposing social distancing and limiting drastically any human contact. France was not an exception, and such constrain inflicted inhabitants to change their habits, without notice, which eventually altered their perception of health risks. It would not take long to foresee the consequences of prolonged physical inactivity, social isolation, behavioral addiction, impatience, and so on [1]. While as a bariatric multidisciplinary team, we could not pursue our surgical activity in the matter, we began to be aware of the fallouts, through our teleconsultation service. To illustrate the common awareness we shared, we conducted a global survey on the behavioral modification towards food consumption during the third week of confinement.
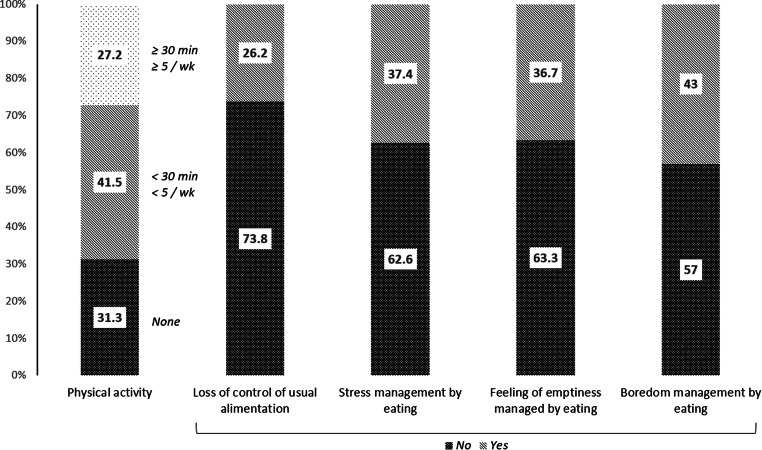
An automated questionnaire including five simple and straight-forward questions was diffused through social media in France. The population of the study was unspecific. A thousand ninety-two individuals replied to the questionnaires in no more than 7 days. Results are available in Fig. 1. More than a quarter of the respondents have currently no physical activity, corresponding to another quarter feeling that they lost control of their usual alimentation habits. Additionally, stress, feeling of emptiness, and boredom are managed with food consumption in 37.4, 36.7, and 43% of individuals, respectively. Furthermore, and more importantly, the latter three emotional eating habits show a low though significant positive correlation with lower physical activity (lowest Spearman’s Rho = 0.10, p value < 0.001) and a high positive correlation with loss of control of usual alimentation (lowest Spearman’s Rho = 0.32, p value < 0.001).
Fig. 1.
Stacked bar chart representing the percentage of answer for each item asked
Although such survey does not have the same merits of traditional scientific comparative studies, the results are striking as they were obtained only 3 weeks after the beginning of mass quarantine. From the viewpoint of the psychiatrist, it is clear that any addictions, from tobacco consumption to online shopping, would dramatically increase during such period. Quarantine and isolation lead to impatience and risk-seeking behavior that in turn have been recently found to increase the likelihood to become obese [2]. In line with those intuitions, our poll shows that a considerable part of the population finds comfort and consolation through food consumption. Doing so, we can anticipate that unhealthy dietary might settle, leading to substantial weight gain and worsening of eating disorders such as bulimia or bing-eating. Similarly, following a prolonged shelter-in-place, doctors might encounter an increase in the incidence of obesity-related comorbidities. Thus, a group of individuals require our attention now. If not, patient care might be more complex as eating disorders often come along with depression, anxiety, or even psychotic decompensation in the vulnerable ones.
To provide sufficient health caregivers, authorities have logically mandated hospitals to cancel any surgical procedures, outside emergencies, and cancer surgeries that cannot be postponed. The exclusion of bariatric patients did not curtail their desire to be treated; instead, their concerns for bariatric surgery have grown consequently [3]. The waiting list has and will expand. In the meantime, multidisciplinary bariatric teams should not rest on their feet. Rather, the mobilization through alternative methods should intensify, with each speciality involved. Psychiatrists and nutritionists should follow up and carefully target sensitive patients, vulnerable to food misconduct. Endocrinologists and bariatric surgeons should work on temporary medical management and draw up action plans to efficiently provide care once routine establishes again.
Last but not least, it might be time for governmental prevention programs to boost their fight against obesity. Without mentioning once more the epidemic of obesity worldwide and its downfall, this disease finds itself to be a risk factor for other ones too often. Coronavirus infection did not differ: obese patients have been associated with a higher risk of morbidity and mortality. Several reasons for the increased lethality of COVID-19 infection have been advanced going from the uncontrolled inflammatory cascade leading to and/or aggravating acute respiratory failure, the overexpression of ACE2—at the heart of the debate on the COVID-19 pandemic [4]— in adipose tissue, and the metabolic obesity-related comorbidities, namely type 2 diabetes and hypertension that have been shown to be associated with increased disease severity and mortality [5, 6]. However, deregulation of the renin/angiotensin system in obese patients warrants some consideration. Angiotensinogen is mostly produced by the liver in normal physiology, whereas in obese individuals, white adipose tissues take over a major part of its production, with a subsequent abnormal increase of local and circulating levels of the vasoconstrictor Angiotensin II [7]. In case of COVID-19 infection, the renin/angiotensin counterregulatory axis, also known as ACE2/Ang-(1–7)/Mas, cannot counteract the deleterious effect of Angiotensin II on pulmonary and cardiac structures and functionalities, due to a loss of function of ACE2 by massive viral binding and internalization. In comparison to this physiopathology understood by doctors, global awareness of obesity and its risks starts to expand among the population.
In conclusion, concerns for food disorder and weight gain are slowly gaining ground in our isolated populations. Awareness among multidisciplinary bariatric teams has never been more needed and effective health measures must be taken, to avoid uncontrolled obesity and obesity-related comorbidity growth, and to prepare the aftermath following the resumption of our routine. Once more, bariatric surgeons must be in the center of the battle and stand ready to offer the right care.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent does not apply.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lippi G, Henry BM, Bovo C, et al. Health risks and potential remedies during prolonged lockdowns for coronavirus disease 2019 (COVID-19). Diagnosis. 2020;2:85–90. [DOI] [PubMed]
- 2.de Oliveira ACM, Leonard TCM, Shuval K, Skinner CS, Eckel C, Murdoch JC. Economic preferences and obesity among a low-income African American community. J Econ Behav Organ. 2016;131:196–208. doi: 10.1016/j.jebo.2015.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tyagi S, Singhal R. Bariatric surgery in the times of corona. Obes Surg. 2020. [DOI] [PMC free article] [PubMed]
- 4.Alifano M, Alifano P, Forgez P, et al. Renin-angiotensin system at the heart of COVID-19 pandemic. Biochimie. 2020;174:30–33. [DOI] [PMC free article] [PubMed]
- 5.Guan W, Ni Z, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. [DOI] [PMC free article] [PubMed]
- 6.Drucker DJ. Coronavirus infections and type 2 diabetes-shared pathways with therapeutic implications. Endocr Rev. 2020;41. [DOI] [PMC free article] [PubMed]
- 7.Giacchetti G, Faloia E, Mariniello B, Sardu C, Gatti C, Camilloni MA, Guerrieri M, Mantero F. Overexpression of the renin-angiotensin system in human visceral adipose tissue in normal and overweight subjects. Am J Hypertens. 2002;15:381–388. doi: 10.1016/S0895-7061(02)02257-4. [DOI] [PubMed] [Google Scholar]