Abstract
Background:
The number of citations a scientific paper has received indicates its impact within any medical field. We performed a bibliometric analysis to highlight the key topics of the most frequently cited 100 articles on perianal fistula to determine the advances in this field.
Methods:
The Scopus database was searched from 1960 to 2018 using the search terms “perianal fistula” or “anal fistula” or “fistula in ano” or “anal fistulae” or “anorectal fistulae” including full articles. The topic, year of publication, publishing journal, country of origin, institution, and department of the first author were analyzed.
Results:
The median number of citations for the top 100 of 3431 eligible papers, ranked in order of the number of citations, was 100 (range: 65–811), and the number of citations per year was 7.5 (range: 3.8–40.1). The most-cited paper (by Parks et al in 1976; 811citations) focused on the classification of perianal fistula. The institution with the highest number of publications was St Mark's Hospital, London, UK. The most-studied topic was surgical management (n = 47). The country and the decade with the greatest number of publications in this field were the USA (n = 34) and the 2000s (n = 50), respectively.
Conclusion:
The 100 most frequently cited manuscripts showed that surgical management had the greatest impact on the study of perianal fistula. This citation analysis provides a reference of what could be considered the most classic papers on perianal fistula, and may serve as a reference for researchers and clinicians as to what constitutes a citable paper in this field.
Keywords: bibliometric analysis, citations, hot topics, perianal fistula, surgery
1. Introduction
Perianal fistula is one of the most difficult surgical disorders. Protecting anal function and preventing anal incontinence are very difficult for surgeons, especially complex perianal fistulas (high, Crohn diseases and low fistulas with compromised sphincters). Although new minimally invasive surgical procedures continue to be developed, the problems of postoperative recurrence and incontinence have yet to be resolved. For more than a century, the study of perianal fistula has produced a large body of clinical and scientific papers, which have led to a greater understanding of the etiology and pathology of the disease and advances in its surgical treatment and imaging examinations. In particular, treatment of perianal fistula in the presence of Crohn disease has also made many new advances, such as the use of stem cells. Since scientists Cole and Eales in 1917 proposed a quantitative comparison of the anatomical literature, bibliometric citation analysis, which examines the citation history of individual papers on a topic of interest, has developed gradually. A citation is received when a publication is referenced by another peer-reviewed paper. As a high number of citations is a proxy for a manuscript's contribution to the current body of knowledge on a subject, the 100 most-cited articles represent the core works of the understanding and treatment of a given disease. Eigenfactor scores are used to determine a journal's impact, which are listed in Thomson's Journal Citation Reports (JCR).
Many medical and surgical specialties have utilized the citation rank analysis to identify the most influential papers in their field, which include burns,[1] cardiac surgery,[2] laparoscopic surgery,[3] abdominal surgery,[4] and cardiovascular medicine.[5] To date, there have been no studies undertaken to determine the most influential papers in the field of perianal fistula. We aim to analyze the 100 most-cited papers on perianal fistula to provide a unique insight into how our understanding of perianal fistula has developed and changed the management of this disease.
2. Materials and methods
The Scopus database was searched to identify the top 100 most-cited manuscripts on perianal fistula using “perianal fistula” or “anal fistula” or “fistula in ano” or “anal fistulae” or “anorectal fistulae” as advanced search terms. The search was limited to full papers in all languages, and the results were ranked by citation number in descending order. Considering the potential bias of increased numbers of citations in older papers, we also calculated the citation rate to reflect the annual reference rate. Articles with the same number of citations were sorted by the citation rate. The number of citations obtained from each study was also evaluated using the Google Scholar database for a comparative analysis.
The title, first and senior author, institution and department of the first author, date of publication, topic, and the country of origin of each paper were recorded for further analysis. The 5-year impact factors and Eigenfactors of each journal publishing the manuscripts were recorded.
3. Results
The Scopus database search returned 3431 full-length, English and non-English language papers. The 100 most-cited articles are listed in Table 1 [6–105]. The number of citations in these 100 papers ranged from 811 to 865, with a median number of 100; with Google Scholar (GS), the median was 159 (range: 1364–1389). The most cited paper, by Parks et al in 1976 focused on the classification of perianal fistula, which was published in 1976 and cited 811 times.[6] The oldest paper in the top 100 most-cited articles was by Milligan and Morgan[69] and was published in the Lancet in 1934. The most recent paper in the top 100 most-cited papers by Panés et al was published in the Lancet and studied stem cell treatment of complex perianal fistulas in Crohn disease, which was cited 101 times.[54] The 2000s yielded the highest number of influential papers (n = 50; 704 citations).
Table 1.
The top 100 most-cited papers on perianal fistula.
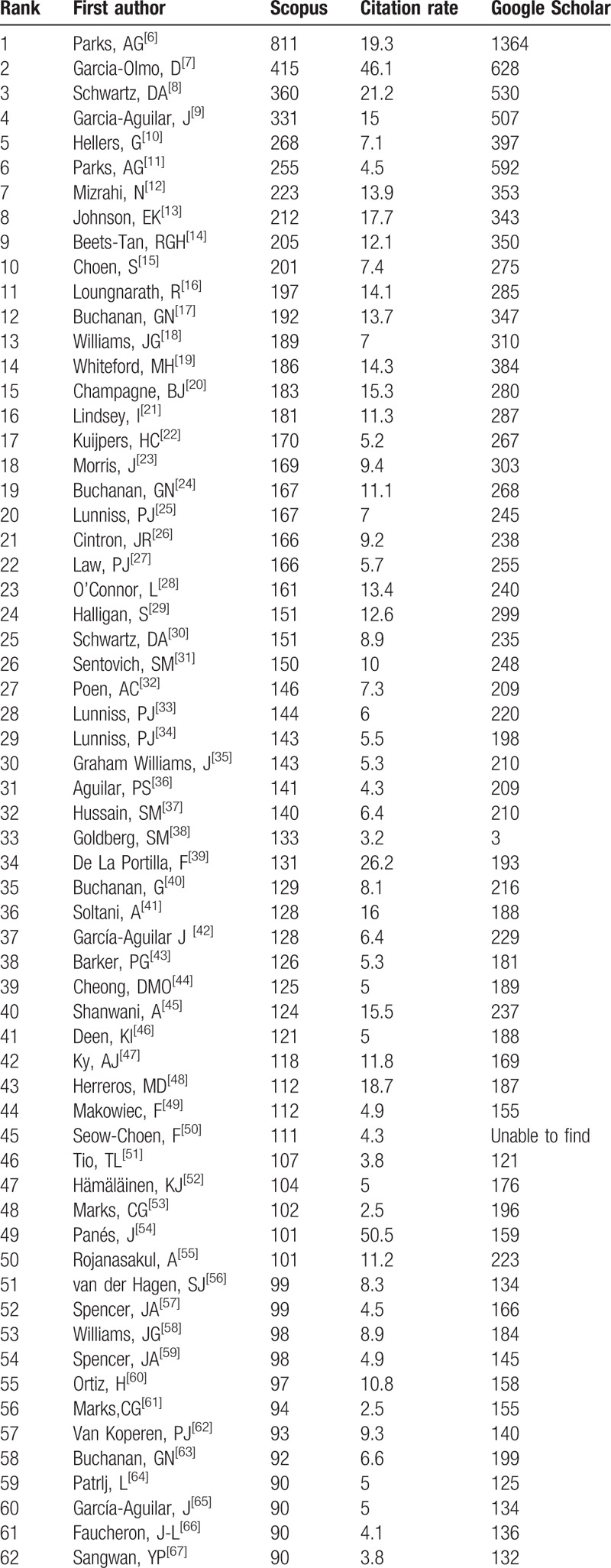
Table 1 (Continued).
The top 100 most-cited papers on perianal fistula.
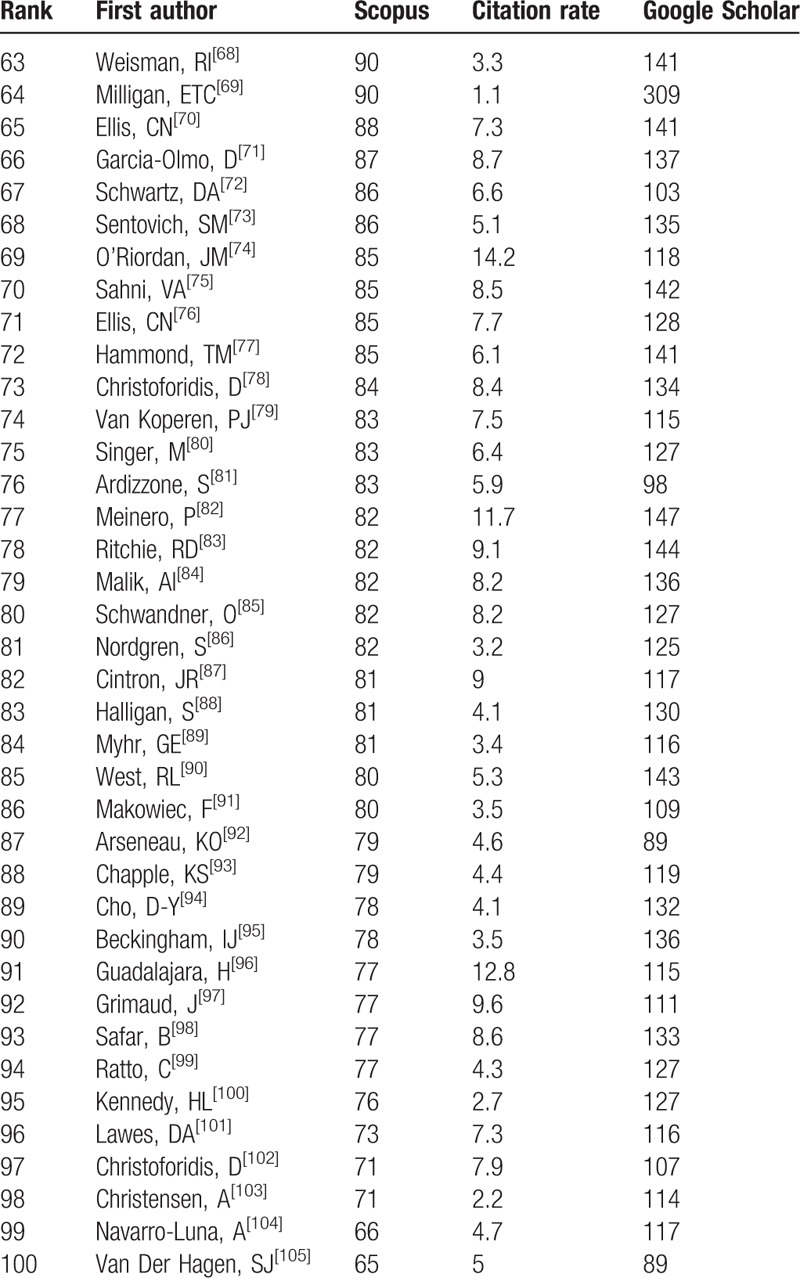
The 100 most-cited papers were published in 22 journals, with the number of manuscripts per journal ranging from 1 to 44. Impact factors of the 22 journals ranged from 53.254 (Lancet) to 2.031 (Digestive Surgery). The Journal of the Diseases of the Colon and Rectum published most papers (n = 44; 5804 citations). The Lancet also had the highest 5-year impact factor (52.665) and Eigenfactor (0.40).
The 100 most-cited papers were from 18 countries, including 13 non-English-speaking countries. The greatest number of publications was from the USA (n = 34; 4613 citations) (Fig. 1). The UK and Netherlands were responsible for 27 (4099 citations) and 10 papers (1188 citations), respectively. St. Mark's Hospital, London, UK had the highest number of papers in the top 100 with 14 papers generating 2598 citations. Professor Buchanan GN, from St Mark's Hospital, had the highest number of first authorships in the top 100 most-cited papers with a total of 4 manuscripts,[17,24,40,63] one of which was published in the Lancet (impact factor 53.254). Three authors had 3 publications each in which they were first author, namely Schwartz et al,[8,30,72] Williams et al,[18,35,58] and Lunniss et al.[25,33–34]
Figure 1.
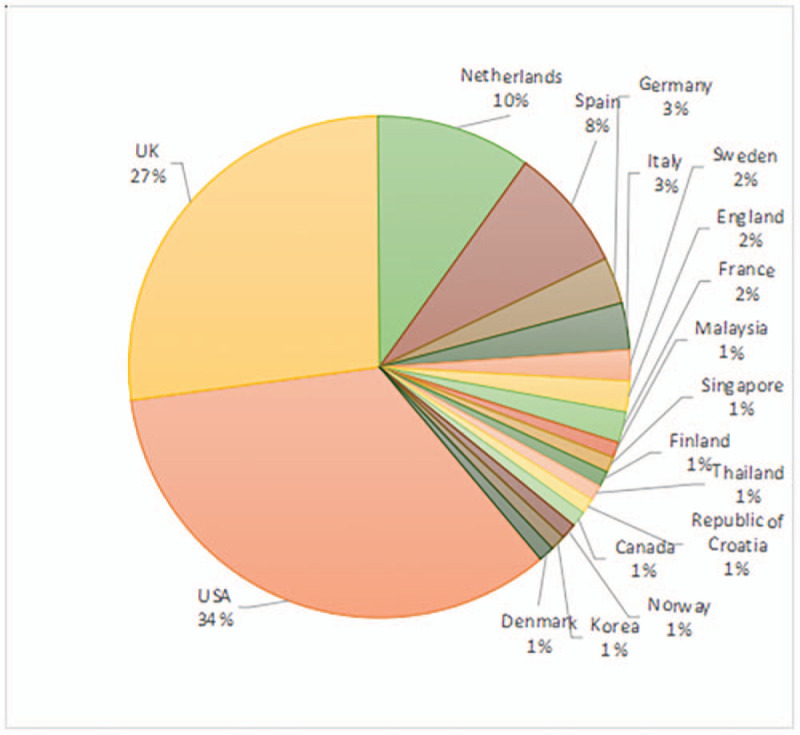
Countries of origin of the top 100 most-cited papers. Numbers of papers in the top 100 are shown as percentages.
The citation rate for the top 10 most-cited manuscripts ranged from 50.5 for Panés et al in 2016 (“Expanded allogeneic adipose-derived mesenchymal stem cells (Cx601) for complex perianal fistulas in Crohn disease: a phase 3 randomized, double-blind controlled trial”)[54] to 14.3 for Whiteford et al in 2005 (“Practice parameters for the treatment of perianal abscess and fistula-in-ano (revised)”).[19] The USA had the highest number of papers in the top 10 according to citation rate with 5, followed by Spain with 4 and the UK with 1. Interestingly, 3 in the top 10 papers according to citation rate were from Spain, which investigated stem cell therapy.
The topics covered in the top 100 most-cited papers were wide-ranging. Surgical management was the topic with the highest number of publications in the top 100 (n = 47), followed by imaging examinations (n = 28). Twenty-six papers on anal fistula were related to Crohn disease, while 5 papers were dedicated to stem cells, 2 papers focused on Infliximab, 2 articles studied the etiology and pathology of perianal fistula, and 1 focused on the classification of perianal fistula.
4. Discussion
The treatment of anal fistula is difficult as recurrent or unhealed events occur, which seriously influence patient quality of life. Although surgery is the only treatment to cure perianal fistula, surgical problems such as protecting anal function, and preventing recurrence and incontinence have confused clinicians for centuries. Research on these aspects is constantly developing. Lundqvist et al[106] carried out the first study on resource use, costs and sick leave related to anal fistulas in Sweden, and showed that anal fistula is a costly social disease, especially in patients undergoing multiple surgeries which results in a heavy social burden.
Unsurprisingly, according to the results of this bibliometric analysis, surgical management is the most discussed topic and was represented in 47 of the 100 most-cited papers. Research contents included “fistula fibrin glue” (11 articles, 1270 citations),[15,24,26,31,64,72,73,75,82,87,97] “perianal fistula plug” (10 articles, 1031 citations),[20,28,47,74,75,78,79,85,98,101] “setontreatment” (6 articles, 628 citations),[18,52,63,66,83,103] “advancement flap” (5 articles),[12,36,41,49,62] “fistulotomy” (2 articles),[62,100] “ligation-of-intersphincteric-fistula-tract” (2 articles),[45,55] “video-assisted-anal-fistula-treatment” (1 article),[82] comparison of operations (6 articles), and others (4 articles). The comparisons between operations were as follows: “perianal fistula plug” versus “fistula fibrin glue,” [13] “fistula fibrin glue” versus “seton treatment” and “fistulotomy,” [21] “seton treatment” versus “fistulotomy,”[35,42] and “perianal fistula plug” versus “advancement flap.”[60,102] Fistula fibrin glue was the most frequently studied form of surgical treatment. In the early 1980s, Kirkegaard and Madsen[107] reported the successful closure of various fistulas with fibrin sealant. It is suitable for both cryptoglandular perianal fistula and perianal fistula with Crohn disease, and is safe, simple, and easy to perform by the surgeon. Although the reported success rates vary, should this operation fail, it can be repeated or changed to another type of sphincter retention surgery. All the studies on surgery lacked randomized controlled trials, which will be the focus of future research by clinicians.
With regard to perianal fistula with Crohn disease, this represents a greater challenge to surgeons due to poor healing, risk of incontinence, and the need for fecal diversion or proctectomy in some patients.[108] There were 26 papers in the 100 most-cited manuscripts on this topic, 4 of these articles focusing on stem cell treatment, including 2 randomized controlled trials, which received 415 citations (Garcia-Olmo et al[7]) and 101 citations (Panés et al[54]), respectively. Therefore, this novel stem cell treatment of perianal fistula with Crohn disease is a hot research topic. Professor Dryden[109] stated that Crohn disease remains a life-long disease, and mesenchymal stem cells may serve as a candidate therapy for patients who have failed to respond to biological therapy.
With regard to the topics covered in the 100 most-cited papers, imaging examinations were also well studied, with 28 articles in total, which included magnetic resonance imaging (MRI), endorectal ultrasonography (ERUS), and fistulography. Of these, MRI was the most studied. It is universally acknowledged that MRI has advantages in aspects such as accuracy, preoperative staging, and evaluation of the primary tract, location of the internal opening, and predicting postoperative recurrence. Yildirim et al[110] conducted a study to assess the contribution of various MRI sequences, compared with readers with varying levels of experience. The results showed that there was statistically significant agreement between the readers for fistula classification, internal opening location, and the presence of sinus tracts, abscess, a horseshoe componentand inflammation. ERUS has some advantages in perianal fistula staging. However, fistulography is inaccurate and unreliable, and is not recommended for the diagnosis of perianal fistula.
Scopus, Web of Science (WOS), Google Scholar (GS), and PubMed are the main databases for academic information sources. Scopus includes a broader spectrum of journals than PubMed and WOS, and its citation analysis is faster and includes more articles than the citation analysis of WOS.[111] Moed et al[112] demonstrated that the linear correlation between GS and Scopus citation counts at the article level is high, with Pearson correlation coefficient being in the range 0.8 to 0.9. Therefore, GS was also chosen to reflect the citation frequency of the top 100 most-cited papers listed in Scopus.
The main limitation of this study is that the Scopus database was used to search for the most-cited articles, as the number of citations is known to differ between GS and WOS. In this paper, although all studies were also evaluated based on the number of citations identified by GS, they were not sorted accordingly. Also the search strategy may not have included all articles on perianal fistula. Furthermore, as suggested by Schoonbaer and Roelants,[113] the use of citation analysis and journal impact is controversial, due to technical limitations, database selectivity, time and discipline-related biases, language and publication-type biases, multiple authorship merits, and citing motivations. With regard to self-citation, several of the manuscripts in the top 100 are authored by multiple researchers (such as “Fibringlue is effective healing perianal fistulas in patients with Crohn Disease”[97] which is authored by 20 coauthors), making it difficult to accurately track and calculate self-citations. Another limitation is that older manuscripts have a greater opportunity for citation than more recent manuscripts. In addition, the names of only the first and senior authors and the institution of only the first author are captured. Thus, several authors in the top 100 may in fact have contributed toward multiple papers, although in a lesser role than the first or senior authors.
5. Conclusions
The most-cited papers highlighted in the current work can be considered the classic works in the field of perianal fistula study, which describe surgical techniques, imaging examinations, basic science, drug therapy (stem cells, Infliximab), and other topics. The majority of papers were published in journals with an impact factor of less than 10. This article may serve as a reference for researchers and clinicians as to what constitutes a citable paper in this field. A few of the more recent papers now have higher rates of citation than those mentioned in this study. The topics covered in these papers can expect significant developments in the next 10 years.
Acknowledgments
The author thank International Science Editing (http://www.internationalscienceediting.com) for editing this manuscript.
Author contributions
Data curation: Qin Chen, Yufei Li.
Methodology: Xiaofeng Wang, Huashan Li.
Supervision: Huashan Li.
Writing – original draft: Qin Chen, Yufei Li.
Writing – review & editing: Qin Chen, Yufei Li.
Footnotes
Abbreviations: ERUS = endorectal ultrasonography, GS = Google Scholar, JCR = Journal Citation Reports, MRI = magnetic resonance imaging, WOS = Web of Science.
How to cite this article: Chen Q, Li Y, Wang X, Li H. Hot topics in global perianal fistula research: A scopus-based bibliometric analysis. Medicine. 2020;99:17(e19659).
QC and YL contributed equally to this work and are co-first authors.
Grant Support for the research is reported.
This paper is a bibliometric article and does not involve human studies or animal experiments. Therefore, approval from the ethics committee is not necessary.
The authors have no conflicts of interest to disclose.
References
- [1].Joyce CW, Kelly JC, Sugrue C. A bibliometric analysis of the 100 most influential papers in burns. Burns 2014;40:30–7. [DOI] [PubMed] [Google Scholar]
- [2].O'Sullivan KE, Kelly JC, Hurley JP. The 100 most cited publications in cardiac surgery: a bibliometric analysis. Ir J Med Sci 2015;184:91–9. [DOI] [PubMed] [Google Scholar]
- [3].Mellor KL, Powell AGMT, Lewis WG. Laparoscopic surgery's 100 most influential manuscripts: a bibliometric analysis. Surg Laparosc Endosc Percutan Tech 2018;28:13–9. [DOI] [PubMed] [Google Scholar]
- [4].Ellul T, Bullock N, Abdelrahman T, et al. The 100 most cited manuscripts in emergency abdominal surgery: a bibliometric analysis. Int J Surg 2017;37:29–35. [DOI] [PubMed] [Google Scholar]
- [5].Shuaib W, Khan MS, Shahid H, et al. Bibliometric analysis of the top 100 cited cardiovascular articles. Am J Cardiol 2015;115:972–81. [DOI] [PubMed] [Google Scholar]
- [6].Parks AG, Gordon PH, Hardcastle JD. A classification of fistula-in-ano. Br J Surg 1976;63:1–2. [DOI] [PubMed] [Google Scholar]
- [7].Garcia-Olmo D, Herreros D, Pascual I, et al. Expanded adipose-derived stem cells for the treatment of complex perianal fistula: a phase ii clinical trial. Dis Colon Rectum 2009;52:79–86. [DOI] [PubMed] [Google Scholar]
- [8].Schwartz DA, Wiersema MJ, Dudiak KM, et al. A comparison of endoscopic ultrasound, magnetic resonance imaging, and exam under anesthesia for evaluation of Crohn's perianal fistulas. Gastroenterology 2001;121:1064–72. [DOI] [PubMed] [Google Scholar]
- [9].Garcia-Aguilar J, Belmonte C, Douglas Wong W, et al. Anal fistula surgery: factors associated with recurrence and incontinence. Dis Colon Rectum 1996;39:723–9. [DOI] [PubMed] [Google Scholar]
- [10].Hellers G, Bergstrand O, Ewerth S, et al. Occurrence and outcome after primary treatment of anal fistulae in Crohn's disease. Gut 1980;21:525–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Parks AG. Pathogenesis and treatment of fistula-in-ano. BMJ 1961;1:463–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Mizrahi N, Wexner SD, Zmora O, et al. Endorectal advancement flap: are there predictors of failure? Dis Colon Rectum 2002;45:1616–21. [DOI] [PubMed] [Google Scholar]
- [13].Johnson EK, Gaw JU, Armstrong DN. Efficacy of anal fistula plug vs. fibrin glue in closure of anorectal fistulas. Dis Colon Rectum 2006;49:371–6. [DOI] [PubMed] [Google Scholar]
- [14].Beets-Tan RG, Beets GL, Van der Hoop AG, et al. Preoperative MR imaging of anal fistulas: does it really help the surgeon? Radiology 2001;218:75–84. [DOI] [PubMed] [Google Scholar]
- [15].Choen S, Burnett S, Bartram CI, et al. Comparison between anal endosonography and digital examination in the evaluation of anal fistulae. Br J Surg 1991;78:445–7. [DOI] [PubMed] [Google Scholar]
- [16].Loungnarath R, Dietz DW, Mutch MG, et al. Fibrin glue treatment of complex anal fistulas has low success rate. Dis Colon Rectum 2004;47:432–6. [DOI] [PubMed] [Google Scholar]
- [17].Buchanan GN, Halligan S, Bartram CI, et al. Clinical examination, endosonography, and MR imaging in preoperative assessment of fistula in ano: comparison with outcome-based reference standard. Radiology 2004;233:674–81. [DOI] [PubMed] [Google Scholar]
- [18].Williams JG, MacLeod CA, Rothenberger DA, et al. Seton treatment of high anal fistulae. Br J Surg 1991;78:1159–61. [DOI] [PubMed] [Google Scholar]
- [19].Whiteford MH, x Kilkenny J, III, Hyman N, et al. Practice parameters for the treatment of perianal abscess and fistula-in-ano (revised). Dis Colon Rectum 2005;48:1337–42. [DOI] [PubMed] [Google Scholar]
- [20].Champagne BJ, O’Connor LM, Ferguson M, et al. Efficacy of anal fistula plug in closure of cryptoglandular fistulas: long-term follow-up. Dis Colon Rectum 2006;49:1817–21. [DOI] [PubMed] [Google Scholar]
- [21].Lindsey I, Smilgin-Humphreys MM, Cunningham C, et al. A randomized, controlled trial of fibrin glue vs. conventional treatment for anal fistula. Dis Colon Rectum 2002;45:1608–15. [DOI] [PubMed] [Google Scholar]
- [22].Kuijpers HC, Schulpen T. Fistulography for fistula-in-ano: is it useful? Dis Colon Rectum 1985;28:103–4. [DOI] [PubMed] [Google Scholar]
- [23].Morris J, Spencer JA, Ambrose NS. MR imaging classification of perianal fistulas and its implications for patient management. Radiographics 2000;20:623–35. [DOI] [PubMed] [Google Scholar]
- [24].Buchanan GN, Bartram CI, Phillips RK, et al. Efficacy of fibrin sealant in the management of complex anal fistula: a prospective trial. Dis Colon Rectum 2003;46:1167–74. [DOI] [PubMed] [Google Scholar]
- [25].Lunniss PJ, Barker PG, Sultan AH, et al. Magnetic resonance imaging of fistula-in-ano. Dis Colon Rectum 1994;37:708–18. [DOI] [PubMed] [Google Scholar]
- [26].Cintron JR, Park JJ, Orsay CP, et al. Repair of fistulas-in-ano using fibrin adhesive: long-term follow-up. Dis Colon Rectum 2000;43:944–50. [DOI] [PubMed] [Google Scholar]
- [27].Law PJ, Talbot RW, Bartram CI, et al. Anal endosonography in the evaluation of perianal sepsis and fistula in ano. Br J Surg 1989;76:752–5. [DOI] [PubMed] [Google Scholar]
- [28].O’Connor L, Champagne BJ, Ferguson MA, et al. Efficacy of anal fistula plug in closure of crohn's anorectal fistulas. Dis Colon Rectum 2006;49:1569–73. [DOI] [PubMed] [Google Scholar]
- [29].Halligan S, Stoker J. Imaging of fistula in ano. Radiology 2006;239:18–33. [DOI] [PubMed] [Google Scholar]
- [30].Schwartz DA, Pemberton JH, Sandborn WJ. Diagnosis and treatment of perianal fistulas in Crohn disease. Ann Intern Med 2001;135:906–18. [DOI] [PubMed] [Google Scholar]
- [31].Sentovich SM. Fibrin glue for anal fistulas: long-term results. Dis Colon Rectum 2003;46:498–502. [DOI] [PubMed] [Google Scholar]
- [32].Poen AC, Felt-Bersma RJF, Eijsbouts QAJ, et al. Hydrogen peroxide-enhanced transanal ultrasound in the assessment of fistula-in-ano. Dis Colon Rectum 1998;41:1147–52. [DOI] [PubMed] [Google Scholar]
- [33].Lunniss PJ, Kamm MA, Phillips RKS. Factors affecting continence after surgery for anal fistula. Br J Surg 1994;81:1382–5. [DOI] [PubMed] [Google Scholar]
- [34].Lunniss PJ, Armstrong P, Barker PG, et al. Magnetic resonance imaging of anal fistulae. Lancet 1992;340:394–6. [DOI] [PubMed] [Google Scholar]
- [35].Williams JG, Rothenberger DA, Nemer FD, et al. Fistula-in-ano in Crohn's disease results of aggressive surgical treatment. Dis Colon Rectum 1991;34:378–84. [DOI] [PubMed] [Google Scholar]
- [36].Aguilar PS, Plasencia G, Hardy TG, Jr, et al. Mucosal advancement in the treatment of anal fistula. Dis Colon Rectum 1985;28:496–8. [DOI] [PubMed] [Google Scholar]
- [37].Hussain SM, Stoker J, Schouten WR, et al. Fistula in ano-endoanal sonography versus endoanal MR imaging in classification. Radiology 1996;200:475–81. [DOI] [PubMed] [Google Scholar]
- [38].Goldberg SM, Parks AG, Golicher JC, et al. The treatment of high fistula-in-ano. Dis Colon Rectum 1976;19:487–99. [DOI] [PubMed] [Google Scholar]
- [39].De La Portilla F, Alba F, García-Olmo D, et al. Expanded allogeneic adipose-derived stem cells (eASCs) for the treatment of complex perianal fistula in Crohn's disease: results from a multicenter phase I/IIa clinical trial. Int J Colorectal Dis 2013;28:313–23. [DOI] [PubMed] [Google Scholar]
- [40].Buchanan G, Halligan S, Williams A, et al. Effect of MRI on clinical outcome of recurrent fistula-in-ano. Lancet 2002;360:1661–2. [DOI] [PubMed] [Google Scholar]
- [41].Soltani A, Kaiser AM. Endorectal advancement flap for cryptoglandular or Crohn's fistula-in-ano. Dis Colon Rectum 2010;53:486–95. [DOI] [PubMed] [Google Scholar]
- [42].García-Aguilar J, Belmonte C, Wong DW, et al. Cutting seton versus two-stage seton fistulotomy in the surgical management of high anal fistula. Br J Surg 1998;85:243–5. [DOI] [PubMed] [Google Scholar]
- [43].Barker PG, Lunniss PJ, Armstrong P, et al. Magnetic resonance imaging of fistula-in-ano: technique, interpretation and accuracy. Clin Radiol 1994;49:7–13. [DOI] [PubMed] [Google Scholar]
- [44].Cheong DMO, Nogueras JJ, Wexner SD, et al. Anal endosonography for recurrent anal fistulas: image enhancement with hydrogen peroxide. Dis Colon Rectum 1993;36:1158–60. [DOI] [PubMed] [Google Scholar]
- [45].Shanwani A, Nor AM, Nil Amri MK. Ligation of the intersphincteric fistula tract (LIFT): a sphincter-saving technique for fistula-in-ano. Dis Colon Rectum 2010;53:39–42. [DOI] [PubMed] [Google Scholar]
- [46].Deen KI, Williams JG, Hutchinson R, et al. Fistulas in ano: endoanal ultrasonographic assessment assists decision making for surgery. Gut 1994;35:391–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Ky AJ, Sylla P, Steinhagen R, et al. Collagen fistula plug for the treatment of anal fistulas. Dis Colon Rectum 2008;51:838–43. [DOI] [PubMed] [Google Scholar]
- [48].Herreros MD, Garcia-Arranz M, Guadalajara H, et al. Autologous expanded adipose-derived stem cells for the treatment of complex cryptoglandular perianal fistulas: a phase iii randomized clinical trial (FATT 1 fistula advanced therapy trial 1) and long-term evaluation. Dis Colon Rectum 2012;55:762–72. [DOI] [PubMed] [Google Scholar]
- [49].Makowiec F, Jehle EC, Becker HD, et al. Clinical course after transanal advancement flap repair of perianal fistula in patients with Crohn's disease. Br J Surg 1995;82:603–6. [DOI] [PubMed] [Google Scholar]
- [50].Seow-Choen F, Nicholls RJ. Anal fistula. Br J Surg 1992;79:197–205. [DOI] [PubMed] [Google Scholar]
- [51].Tio TL, Mulder CJ, Wijers OB, et al. Endosonography of peri-anal and peri-colorectal fistula and/or abscess in Crohn's disease. Gastrointest Endosc 1990;36:331–6. [DOI] [PubMed] [Google Scholar]
- [52].Hämäläinen KJ, Sainio AP. Cutting seton for anal fistulas: high risk of minor control defects. Dis Colon Rectum 1997;40:1443–7. [DOI] [PubMed] [Google Scholar]
- [53].Marks CG, Ritchie JK. Anal fistulas at St Mark's Hospital. Br J Surg 1977;64:84–91. [DOI] [PubMed] [Google Scholar]
- [54].Panés J, García-Olmo D, Van Assche G, et al. Expanded allogeneic adipose-derived mesenchymal stem cells (Cx601) for complex perianal fistulas in Crohn's disease: a phase 3 randomised, double-blind controlled trial. Lancet 2016;388:1281–90. [DOI] [PubMed] [Google Scholar]
- [55].Rojanasakul A. LIFT procedure: a simplified technique for fistula-in-ano. Tech Coloproctol 2009;13:237–40. [DOI] [PubMed] [Google Scholar]
- [56].van der Hagen SJ, Baeten CG, Soeters PB, et al. Long-term outcome following mucosal advancement flap for high perianal fistulas and fistulotomy for low perianal fistulas Recurrent perianal fistulas: failure of treatment or recurrent patient disease? Int J Colorectal Dis 2006;21:784–90. [DOI] [PubMed] [Google Scholar]
- [57].Spencer JA, Ward J, Beckingham IJ, et al. Dynamic contrast-enhanced MR imaging of perianal fistulas. Am J Roentgenol 1996;167:735–41. [DOI] [PubMed] [Google Scholar]
- [58].Williams JG, Farrands PA, Williams AB, et al. The treatment of anal fistula: ACPGBI position statement. Colorectal Dis 2007;9: suppl. 4: 18–50. [DOI] [PubMed] [Google Scholar]
- [59].Spencer JA, Chapple K, Wilson D, et al. Outcome after surgery for perianal fistula: predictive value of MR imaging. Am J Roentgenol 1998;171:403–6. [DOI] [PubMed] [Google Scholar]
- [60].Ortiz H, Marzo J, Ciga MA, et al. Randomized clinical trial of anal fistula plug versus endorectal advancement flap for the treatment of high cryptoglandular fistula in ano. Br J Surg 2009;96:608–12. [DOI] [PubMed] [Google Scholar]
- [61].Marks CG, Ritchie JK, Lockhart-Mummery HE. Anal fistulas in Crohn's disease. Br J Surg 1981;68:525–7. [DOI] [PubMed] [Google Scholar]
- [62].Van Koperen PJ, Wind J, Bemelman WA, et al. Long-term functional outcome and risk factors for recurrence after surgical treatment for low and high perianal fistulas of cryptoglandular origin. Dis Colon Rectum 2008;51:1475–81. [DOI] [PubMed] [Google Scholar]
- [63].Buchanan GN, Owen HA, Torkington J, et al. Long-term outcome following loose-seton technique for external sphincter preservation in complex anal fistula. Br J Surg 2004;91:476–80. [DOI] [PubMed] [Google Scholar]
- [64].Patrlj L, Kocman B, Martinac M, et al. Fibrin glue-antibiotic mixture in the treatment of anal fistulae: experience with 69 cases. Dig Surg 2000;17:77–80. [DOI] [PubMed] [Google Scholar]
- [65].García-Aguilar J, Davey CS, Le CT, et al. Patient satisfaction after surgical treatment for fistula-in-ano. Dis Colon Rectum 2000;43:1206–12. [DOI] [PubMed] [Google Scholar]
- [66].Faucheron J-L, Saint-Marc O, Guibert L, et al. Long-term seton drainage for high anal fistulas in crohn's disease—a sphincter-saving operation? Dis Colon Rectum 1996;39:208–11. [DOI] [PubMed] [Google Scholar]
- [67].Sangwan YP, Rosen L, Riether RD, et al. Is simple fistula-in-ano simple? Dis Colon Rectum 1994;37:885–9. [DOI] [PubMed] [Google Scholar]
- [68].Weisman RI, Orsay CP, Pearl RK, et al. The role of fistulography in fistula-in-ano: report of five cases. Dis Colon Rectum 1991;34:181–4. [DOI] [PubMed] [Google Scholar]
- [69].Milligan ETC, Morgan CN. Surgical anatomy of the anal canal with special reference to anorectal fistulae. Lancet 1934;224:1150–6. [Google Scholar]
- [70].Ellis CN, Clark S. Fibrin glue as an adjunct to flap repair of anal fistulas: a randomized, controlled study. Dis Colon Rectum 2006;49:1736–40. [DOI] [PubMed] [Google Scholar]
- [71].Garcia-Olmo D, Garcia-Arranz M, Herreros D. Expanded adipose-derived stem cells for the treatment of complex perianal fistula including Crohn's disease. Expert Opin Biol Ther 2008;8:1417–23. [DOI] [PubMed] [Google Scholar]
- [72].Schwartz DA, White CM, Wise PE, et al. Use of endoscopic ultrasound to guide combination medical and surgical therapy for patients with Crohn's perianal fistulas. Inflamm Bowel Dis 2005;11:727–32. [DOI] [PubMed] [Google Scholar]
- [73].Sentovich SM. Fibrin glue for all anal fistulas. J Gastrointest Surg 2001;5:158–61. [DOI] [PubMed] [Google Scholar]
- [74].O’Riordan JM, Datta I, Johnston C, et al. A systematic review of the anal fistula plug for patients with Crohn's and non-Crohn's related fistula-in-ano. Dis Colon Rectum 2012;55:351–8. [DOI] [PubMed] [Google Scholar]
- [75].Sahni VA, Ahmad R, Burling D. Which method is best for imaging of perianal fistula? Abdom Imaging 2008;33:26–30. [DOI] [PubMed] [Google Scholar]
- [76].Ellis CN. Bioprosthetic plugs for complex anal fistulas:an early experience. J Surg Educ 2007;64:36–40. [DOI] [PubMed] [Google Scholar]
- [77].Hammond TM, Grahn MF, Lunniss PJ. Fibrin glue in the management of anal fistulae. Colorectal Dis 2004;6:308–19. [DOI] [PubMed] [Google Scholar]
- [78].Christoforidis D, Etzioni DA, Goldberg SM, et al. Treatment of complex anal fistulas with the collagen fistula plug. Dis Colon Rectum 2008;51:1482–7. [DOI] [PubMed] [Google Scholar]
- [79].Van Koperen PJ, D’Hoore A, Wolthuis AM, et al. Anal fistula plug for closure of difficult anorectal fistula: a prospective study. Dis Colon Rectum 2007;50:2168–72. [DOI] [PubMed] [Google Scholar]
- [80].Singer M, Cintron J, Nelson R, et al. Treatment of fistulas-in-ano with fibrin sealant in combination with intra-adhesive antibiotics and/or surgical closure of the internal fistula opening. Dis Colon Rectum 2005;48:799–808. [DOI] [PubMed] [Google Scholar]
- [81].Ardizzone S, Maconi G, Colombo E, et al. Perianal fistulae following infliximab treatment clinical and endosonographic outcome. Inflamm Bowel Dis 2004;10:91–6. [DOI] [PubMed] [Google Scholar]
- [82].Meinero P, Mori L. Video-assisted anal fistula treatment (VAAFT): a novel sphincter-saving procedure for treating complex anal fistulas. Tech Coloproctol 2011;15:417–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [83].Ritchie RD, Sackier JM, Hodde JP. Incontinence rates after cutting seton treatment for anal fistula. Colorectal Dis 2009;11:564–71. [DOI] [PubMed] [Google Scholar]
- [84].Malik AI, Nelson RL. Surgical management of anal fistulae: a systematic review. Colorectal Dis 2008;10:420–30. [DOI] [PubMed] [Google Scholar]
- [85].Schwandner O, Stadler F, Dietl O, et al. Initial experience on efficacy in closure of cryptoglandular and Crohn's transsphincteric fistulas by the use of the anal fistula plug. Int J Colorectal Dis 2008;23:319–24. [DOI] [PubMed] [Google Scholar]
- [86].Nordgren S, Fasth S, Hultén L. Anal fistulas in Crohn's disease: incidence and outcome of surgical treatment. Int J Colorectal Dis 1992;7:214–8. [DOI] [PubMed] [Google Scholar]
- [87].Cintron JR, Park JJ, Orsay CP, et al. Repair of fistulas-in-ano using autologous fibrin tissue adhesive. Dis Colon Rectum 1999;42:607–13. [DOI] [PubMed] [Google Scholar]
- [88].Halligan S, Bartram CI. MR imaging of fistula in ano: are endoanal coils the gold standard? Am J Roentgenol 1998;171:407–12. [DOI] [PubMed] [Google Scholar]
- [89].Myhr GE, Myrvold HE, Nilsen G, et al. Perianal fistulas: use of MR imaging for diagnosis. Radiology 1994;191:545–9. [DOI] [PubMed] [Google Scholar]
- [90].West RL, Zimmerman DDE, Dwarkasing S, et al. Prospective comparison of hydrogen peroxide-enhanced three-dimensional endoanal ultrasonography and endoanal magnetic resonance imaging of perianal fistulas. Dis Colon Rectum 2003;46:1407–15. [DOI] [PubMed] [Google Scholar]
- [91].Makowiec F, Jehle EC, Starlinger M. Clinical course of perianal fistulas in Crohn's disease. Gut 1995;37:696–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [92].Arseneau KO, Cohn SM, Cominelli F, et al. Cost-Utility of initial medical management for Crohn's disease perianal fistulae. Gastroenterology 2001;120:1640–56. [DOI] [PubMed] [Google Scholar]
- [93].Chapple KS, Spencer JA, Windsor ACJ, et al. Prognostic value of magnetic resonance imaging in the management of fistula-in-ano. Dis Colon Rectum 2000;43:511–6. [DOI] [PubMed] [Google Scholar]
- [94].Cho D-Y. Endosonographic criteria for an internal opening of fistula-in-ano. Dis Colon Rectum 1999;42:515–8. [DOI] [PubMed] [Google Scholar]
- [95].Beckingham IJ, Spencer JA, Ward J, et al. Prospective evaluation of dynamic contrast enhanced magnetic resonance imaging in the evaluation of fistula in ano. Br J Surg 1996;83:1396–8. [DOI] [PubMed] [Google Scholar]
- [96].Guadalajara H, Herreros D, De-La-Quintana P, et al. Long-term follow-up of patients undergoing adipose-derived adult stem cell administration to treat complex perianal fistulas. Int J Colorectal Dis 2012;27:595–600. [DOI] [PubMed] [Google Scholar]
- [97].Grimaud J, Munoz-Bongrand N, Siproudhis L, et al. Fibrin glue is effective healing perianal fistulas in patients with Crohn's disease. Gastroenterology 2010;138:2275–81. [DOI] [PubMed] [Google Scholar]
- [98].Safar B, Jobanputra S, Sands D, et al. Anal fistula plug: initial experience and outcomes. Dis Colon Rectum 2009;52:248–52. [DOI] [PubMed] [Google Scholar]
- [99].Ratto C, Gentile E, Merico M, et al. How can the assessment of fistula-in-ano be improved? Dis Colon Rectum 2000;43:1375–82. [DOI] [PubMed] [Google Scholar]
- [100].Kennedy HL, Zegarra JP. Fistulotomy without external sphincter division for high anal fistulae. Br J Surg 1990;77:898–901. [DOI] [PubMed] [Google Scholar]
- [101].Lawes DA, Efron JE, Abbas M, et al. Early experience with the bioabsorbable anal fistula plug. World J Surg 2008;32:1157–9. [DOI] [PubMed] [Google Scholar]
- [102].Christoforidis D, Pieh MC, Madoff RD, et al. Treatment of transsphincteric anal fistulas by endorectal advancement flap or collagen fistula plug: a comparative study. Dis Colon Rectum 2009;52:18–22. [DOI] [PubMed] [Google Scholar]
- [103].Christensen A, Nilas L, Christiansen J. Treatment of transsphincteric anal fistulas by the seton technique. Dis Colon Rectum 1986;29:454–5. [DOI] [PubMed] [Google Scholar]
- [104].Navarro-Luna A, García-Domingo MI, Rius-Macías J, et al. Ultrasound study of anal fistulas with hydrogen peroxide enhancement. Dis Colon Rectum 2004;47:108–14. [DOI] [PubMed] [Google Scholar]
- [105].Van Der Hagen SJ, Baeten CG, Soeters PB, et al. Anti-TNF-a (Infliximab) used as induction treatment in case of active proctitis in a multistep strategy followed by definitive surgery of complex anal fistulas in Crohn's disease: a preliminary report. Dis Colon Rectum 2005;48:758–67. [DOI] [PubMed] [Google Scholar]
- [106].Lundqvist A, Ahlberg I, Hjalte F, et al. Direct and indirect costs for anal fistula in Sweden. Int J Surg 2016;35:129–33. [DOI] [PubMed] [Google Scholar]
- [107].Kirkegaard P, Madsen PV. Perineal sinus after removal of the rectum: occlusion with fibrin adhesive. Am J Surg 1983;145:791–4. [DOI] [PubMed] [Google Scholar]
- [108].Nasseri Y, Cassella L, Berns M, et al. The anal fistula plug in Crohn's disease patients with fistula-in-ano: a systematic review. Colorectal Dis 2016;18:351–6. [DOI] [PubMed] [Google Scholar]
- [109].Dryden GW. Overview of stem cell therapy for Crohn's disease. Expert Opin Biol Ther 2009;9:841–7. [DOI] [PubMed] [Google Scholar]
- [110].Yildirim N, Gökalp G, Öztürk E, et al. Ideal combination of MRI sequences for perianal fistula classification and the evaluation of additional findings for readers with varying levels of experience. Diagn Interv Radiol 2012;18:11–9. [DOI] [PubMed] [Google Scholar]
- [111].Falagas ME, Pitsouni EI, Malietzis GA, et al. Comparison of PubMed, Scopus, Web of Science, and Google Scholar: strengths and weaknesses. Faseb J 2008;22:338–42. [DOI] [PubMed] [Google Scholar]
- [112].Moed HF, Bar-Ilan J, Halevi G. A new methodology for comparing Google Scholar and Scopus. J Informetr 2016;10:533–51. [Google Scholar]
- [113].Schoonbaer D, Roelants G. Citation analysis for measuring the value of scientific publications: quality assessment tool or comedy of errors? Trop Med Int Health 1996;1:739–52. [DOI] [PubMed] [Google Scholar]


