Abstract
Objective
To compare and correlate the efficacy of the NOSE score & the VAS score in determining the symptomatic benefit in patients undergoing septoplasty.
Materials and methods
Eighty patients with deviated nasal septum undergoing septoplasty were included in the study. NOSE score & VAS score (out of 100) was documented before and after surgery. Results were correlated and compared statistically.
Results
In the NOSE score, the most bothersome symptom was trouble breathing through the nose (85.83); followed by Nasal obstruction or blockage (82.50). Wilcoxon test showed significant improvement with NOSE score and VAS score in all patients at 1 month and 3 months. Spearman's coefficient showed a positive correlation between the two, though the score improvement and patient satisfaction rate was significantly high with NOSE score.
Conclusions
NOSE score and the VAS score both provide effective framework for evaluating treatment responses after septoplasty. However, the NOSE score showed higher improvement and better patient satisfaction rate when used to measure of nasal obstruction as compared to the VAS score.
Keywords: Deviated nasal septum, Septoplasty, NOSE score, VAS score
Introduction
Nasal obstruction is a significant health problem associated with poor sleep and a decreased health-related quality of life. Septoplasty is the recommended surgical procedure to relieve nasal obstruction due to a deviated nasal septum and it is also one of the most common operations to be performed by Rhinologist.1 There are many subjective and objective methods for assessing nasal obstruction. Of the subjective methods, health-related quality of life questionnaires are among the most recent tools for assessing changes in symptoms, the impact of disease on the quality of life and effectiveness of the treatment of chronic diseases. These questionnaires were developed either for gauging general health status or assessing a specific clinical problem. In the Rhinology field, there are several questionnaires, one of which is the NOSE score. In 2004, Stewart et al2 introduced the NOSE score as a valid, reliable, and responsive self-report instrument to quantify the subjective burden related to nasal obstruction. In our clinical practice, we have chosen this questionnaire because it is brief, easy to complete for the patient and specific for nasal obstruction. Also, the NOSE score can be further applied for outcome analysis after septoplasty.3 Another subjective method for analysis of symptoms is the VAS. VAS is a psychometric response scale used to measure subjective characteristics or attitudes and have been used in the past for a multitude of disorders, as well as in market research and social science investigations, among others.4 The VAS has been used in this study to determine the severity of nasal obstruction pre- and post-operatively after septoplasty. This study aims to compare the efficacy of the NOSE and VAS score in determining the symptomatic benefit in patients of septoplasty.
Materials and methods
This is a prospective study done at our Institute during 2017–2018. Institutional Review Board approval was taken and the study was performed according to the guidelines and ethical standards of the Helsinki Declaration. The approval number is SKNMC/Ethics/App/2018/420. Eighty patients aged between 18 and 65 years, with symptomatic deviated nasal septum having nasal obstruction as primary complaint, were included in this study. Patients with previous nasal septal surgery, acute or chronic rhino sinusitis, inferior turbinate hypertrophy, perforation of the nasal septum, allergic rhinitis, granulomatous diseases of nose and sinuses, craniofacial malformation and pregnancy were excluded from the study. Detailed history of present illness was taken with special note of presence or absence of symptoms, like nasal obstruction, headache, nasal discharge, nasal bleeding, loss of smell and other associated manifestations. A detailed general physical examination and ENT examination was performed. After taking informed consent, patients were asked to fill questionnaires relating to severity of their symptoms using NOSE score (Table 1) and the VAS scale (Fig. 1). For the VAS score, patients were instructed to indicate the point on the scale (1–10) that best corresponds to their status for severity of nasal obstruction.” Higher score indicates worse obstruction.
Table 1.
NOSE score.
| Symptom | Not a problem (A) | Very mild problem (B) | Moderate problem (C) | Fairly bad problem (D) | Severe problem (E) |
|---|---|---|---|---|---|
| Nasal stuffiness | 0 | 1 | 2 | 3 | 4 |
| Nasal Blockage or obstruction | 0 | 1 | 2 | 3 | 4 |
| Trouble breathing through my nose | 0 | 1 | 2 | 3 | 4 |
| Trouble sleeping | 0 | 1 | 2 | 3 | 4 |
| Unable to get enough air through my nose during exertion or exercise | 0 | 1 | 2 | 3 | 4 |
Total score = A+B+C+D+E (Maximum score 20). Score out of 20×5 = Score out of 100.
Fig. 1.
Visual analogue scale (VAS). VAS score out of 10 × 10 = VAS score out of 100.
After preoperative evaluation, septoplasty surgery was performed in all patients under general anaesthesia by the same team of surgeons, namely the authors. Infiltration of the septum was done with 2% lignocaine with adrenaline, 1:100 000. A hemitransfixion (Freer's) incision was made at the caudal border of nasal septum. The mucoperichondrial and mucoperiosteal flaps were elevated. The osseocartilaginous junction was dislocated. The bony septum was corrected by removing the deviated portion of the septum. Inferior cartilaginous strip was removed if necessary. The incision was sutured with 3.0 catgut. Bilateral nasal packing was done. Patient received intravenous antibiotics and anti-inflammatory analgesics for 3 days. Nasal pack was removed on 3rd post operative day and the patient was discharged. Follow up was done after 1 week and the monthly thereafter. Post-operative symptoms were evaluated using NOSE score and the VAS score (out of 100) at 1 and 3 months. Data was analyzed using tables, graph and percentage and test of significance. For comparative analysis between preoperative and postoperative score, Wilcoxon test was used. Score improvement was compared withChi square test with Yate's correction and Fisher's exact probability test. A p value < 0.05 was considered to be significant. The odds ratios (OR) and 95% confidence intervals (CI) were added, if p values were less than 0.05. Correlation between NOSE score and VAS score was done through the Spearman's coefficient correlation. This coefficient varies between −1 and 1. The closer it is to −1 or 1, stronger is the association and closer it is to 0, weaker is the association. If it is closer to −1, it suggests inverse association between the variables. Patients with total score 25/100 or less at 3 months were considered as extremely satisfied. Patient satisfaction rate was compared between NOSE score and VAS score.
Results
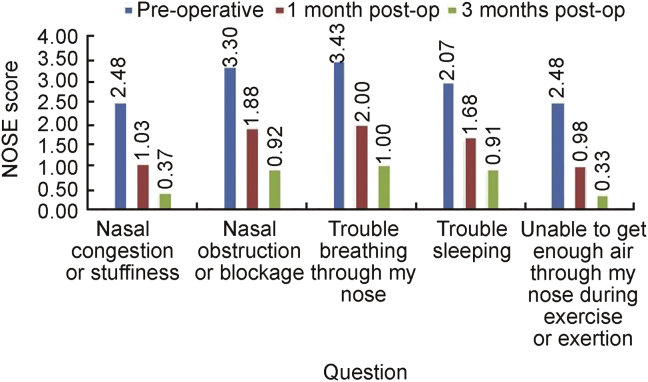
The average age of the participant was 29.96 years, youngest being 18 years of age and oldest being 60 years of age. Male to female ratio was 2.33:1. The average preoperative NOSE score was 73.33. It was observed that the most bothersome symptom was trouble breathing through the nose (85.83), the second being Nasal obstruction or blockage (82.50). The average postoperative NOSE score was 37.92 and 17.67 at 1 month and 3 months respectively (Table 2, Fig. 2), thus showing a consistent improvement. Wilcoxon test applied for graded improvement of the score showed statistically significant improvement with Z value 3.290 and p value 0.001 (95% confidence interval) in Table 2.
Table 2.
Average NOSE score.
| Question | Pre-operatively | 1 month after surgery | 3 months after surgery |
|---|---|---|---|
| Nasal Congestion or Stuffiness | 2.48 | 1.03 | 0.37 |
| Nasal Obstruction or Blockage | 3.30 | 1.88 | 0.92 |
| Trouble breathing through my nose | 3.43 | 2.00 | 1.00 |
| Trouble sleeping | 2.97 | 1.68 | 0.92 |
| Unable to get enough air through my nose during exercise or exertion | 2.48 | 0.98 | 0.33 |
| Total NOSE score (out of 20) | 14.67 | 7.58 | 3.53 |
| % NOSE score (OUT OF 100) | 73.33 | 37.92 | 17.67 |
| Wilcoxon Z value | 3.290 | ||
| Wilcoxon p value | 0.001 | ||
Fig. 2.
NOSE score.
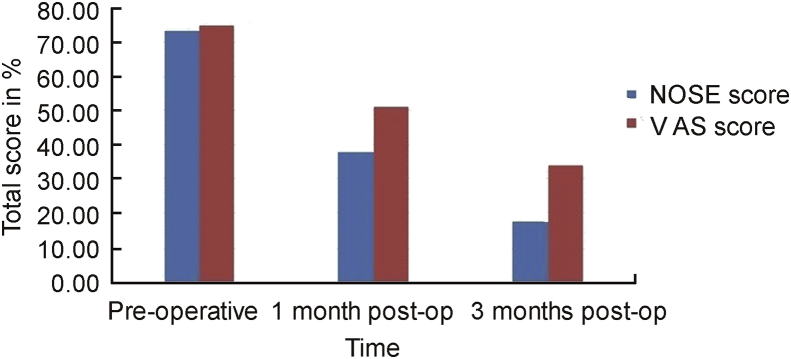
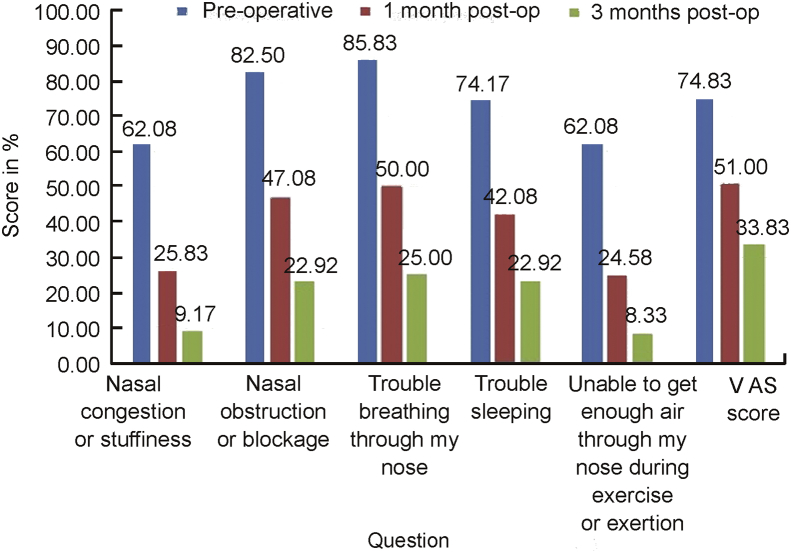
The average preoperative VAS score was 74.83. The average postoperative VAS score was 51.0 and 33.83 at 1 month and 3 months respectively (Table 3, Fig. 3). Wilcoxon test applied for graded improvement of the score showed statistically significant improvement with Z value 3.251 and p value 0.001 (95% confidence interval) in Table 3 (see Fig. 4, Fig. 5).
Table 3.
VAS score for nasal obstruction.
| VAS score for nasal obstruction | pre-operatively | 1 month after surgery | 3 months after surgery |
|---|---|---|---|
| Average of total (out of 10) | 7.48 | 5.10 | 3.38 |
| Average percentage (out of 100) | 74.83 | 51.00 | 33.83 |
| Wilcoxon Z value | 3.251 | ||
| Wilcoxon p value | 0.001 | ||
Fig. 3.
VAS score.
Fig. 4.
Comparison between NOSE score and VAS score.
Fig. 5.
Comparison between NOSE score and VAS score in %.
According to the Spearman's relation coefficient, we observed that there is a significant correlation between NOSE and VAS (rs = 0.548; p = 0.0001; n = 80). Thus, the higher the NOSE score, the higher is VAS score. Comparative analysis of score improvement revealed statistically significant difference, with NOSE score showing more improvement as compared to VAS score.Chi square value was 5.847 with p value 0.0156. Fisher's exact probability showed p value 0.0151.
Patient satisfaction rate was 88% with NOSE score and 62% with VAS score, showing statistically significant difference with Fisher's exact probability test (p value 0.0001).
Discussion
Nasal obstruction is one of the most common complaints that a Rhinologist faces in the day to day practice. Deviated nasal septum is one of the most common causes for the nasal obstruction. Various surgeries have been proposed for the correction of deviated nasal septum. It has undergone several modifications since its inception. Initially submucous resection of septum was done which was a radical surgery and was associated with complications. Later septoplasty was developed as it had advantages of minimal resection of septum and hence less complications.2
In the past, the attempt has frequently been made to prove clinical relevant improvement of nasal breathing after septal surgery by active anterior rhinomanometry, acoustic rhinometry, or peak nasal inspiratory flow (PNIF). Only three out of 982 studies fulfilled the stringent criteria of a meta-analysis by Singh et al. However, the utilizable data showed a significant reduction of nasal resistance after septal surgery.5
The application of validated disease-specific measures in prospective studies is required to achieve a high level of Evidence-Based Medicine (EBM). Stewart et al2 addressed themselves to this task and developed the NOSE score within the scope of a multicenter study. A team of experts developed an alpha-version of the instrument with 10 obstruction-specific items that were scored using a 5-point Likert scale. This measure was validated by the assessment and calculation of reliability (test-retest reliability, internal consistency), validity (content validity, construct validity, discrimination validity, concurrent validity) and response sensitivity (standardized response mean, effect size). During this process the measure was reduced to 5 items which are the following: nasal congestion or stuffiness, nasal blockage or obstruction, trouble breathing through the nose, trouble sleeping, unable to get enough air through the nose during exercise or exertion.2
The study by Stewart et al6 also has used NOSE score for subjective evaluation, as was used in our study and they concluded, in patients with septal deformity, septoplasty results in significant improvement in disease-specific quality of life, high patient's satisfaction, and decreased medication use. Similar to our study, according to Stewart et al6 NOSE score can be used for subjective evaluation of nasal obstruction, which can be used for pre to post operative evaluation and also for comparison among different nasal surgeries.
The NOSE score was then subsequently used in a prospective study with 59 patients addressing outcome evaluation after septoplasty, the multicenter NOSE score Study.6 Data revealed a significant improvement of the mean NOSE score from 67 to 23 points (p<0.001) on a 0–100 scale after 3 months which was also detectable after 6 months. Patient satisfaction was high with 63% of the patients being very or extremely satisfied. Furthermore, reduced use of medication was observed. Another study with 12 patients treated with extracorporeal septoplasty detected an improvement of the NOSE score from 77 to 13 points.7 In our study it was observed that the most bothersome symptom was trouble breathing through the nose (85.83), the second being nasal obstruction or blockage (82.50). There was a consistent improvement in all patients at 1 month as well as 3 months (Table 2, Table 4). We found patient satisfaction rate 88% and the improvement of NOSE score from 73.33 to 17.67 at the end of 3 months.
Table 4.
Comparison of NOSE score & VAS score.
| Pre-operatively | Pre-op score (out of 100) | 1 month after surgery | 1 month post-op score (out of 100) | 3 months after surgery | 3 months post-op score (out of 100) | |
|---|---|---|---|---|---|---|
| Nasal Congestion or Stuffiness | 2.48 | 62.08 | 1.03 | 25.83 | 0.37 | 9.17 |
| Nasal Obstruction or Blockage | 3.30 | 82.50 | 1.88 | 47.08 | 0.92 | 22.92 |
| Trouble breathing through my nose | 3.43 | 85.83 | 2.00 | 50.00 | 1.00 | 25.00 |
| Trouble sleeping | 2.97 | 74.17 | 1.68 | 42.08 | 0.92 | 22.92 |
| Unable to get enough air through my nose during exercise or exertion | 2.48 | 62.08 | 0.98 | 24.58 | 0.33 | 8.33 |
| Total NOSE score | 14.67 | 73.33 | 7.58 | 37.92 | 3.53 | 17.67 |
| VAS score | 7.48 | 74.83 | 5.10 | 51.00 | 3.38 | 33.83 |
VAS has been used repeatedly for the assessment of septoplasty results as disease-specific Quality of life instruments were not available. Compared with assessment of satisfaction they stand for methodic progress.8 A retrospective long-term evaluation 2–10 years after septoplasty yielded a mean satisfaction of 6 on a 1–10-scale.8 Furthermore, the authors stated a significant correlation between anterior septal deviation and satisfaction with the result of surgery. In a comparison of conventional versus endoscopic septoplasty subjective assessment of obstruction by VAS did not detect a difference between the two techniques.9 In our study, the VAS score showed a consistent improvement from preoperative assessment score 74.8 to 51.0 at 1 month and 33.8 at 3 months. We found patient satisfaction rate 62%.
Benefits of septoplasty, as perceived by the patient, widely vary over different grades of satisfaction, ranging from complete alleviation of symptoms to a total failure. For accurate assessment of the benefit, we need a disease specific questionnaire. In addition to high sensitivity and reliability, VAS is easy and simple to use by patients and health care providers.9 But it is not a disease specific and does not include various aspects of nasal obstruction. On comparing the results of the NOSE and VAS scale, it was found that, though the total NOSE score pre-operatively was very similar to the VAS scale, there was more improvement seen on the NOSE score rather than the VAS scale at both 1 and 3 months respectively. Patient satisfaction rate was also significantly high with NOSE score. NOSE score is a detailed questionnaire including 5 aspects related to nasal obstruction. It provides a valuable context and gives our patients a foundation to better understand their symptoms. Structuring the NOSE score of patients in classification system gives them a better understanding of severity of their condition. We found NOSE score to be a brief, reliable, responsive survey to measure disturbances in quality of life specific to nasal obstruction.
Conclusion
Surgeries for nasal obstruction are among the most common in otorhinolaryngology practices. Quality of life questionnaire is easy and effective tool in estimating the amount of improvement in nasal obstruction for patients undergoing septoplasty. Both the NOSE and VAS score provide effective framework for evaluating treatment responses. However, the NOSE score showed higher improvement and better patient satisfaction rate when used to measure of nasal obstruction as compared to the VAS score.
Declaration of Competing Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Edited by Yi Fang
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Moore M., Eccles R. Objective evidence for the efficacy of surgical management of the deviated septum as a treatment for chronic nasal obstruction: a systematic review. Clin Otolaryngol. 2011;36:106–113. doi: 10.1111/j.1749-4486.2011.02279.x. [DOI] [PubMed] [Google Scholar]
- 2.Stewart M.G., Witsell D.L., Smith T.L., Weaver E.M., Yueh B., Hannley M.T. Development and validation of the nasal obstruction symptom evaluation (NOSE) scale. Otolaryngol Head Neck Surg. 2004;130:157–163. doi: 10.1016/j.otohns.2003.09.016. [DOI] [PubMed] [Google Scholar]
- 3.Rhee J.S., Sullivan C.D., Frank D.O., Kimbell J.S., Garcia G.J. A systematic review of patient-reported nasal obstruction scores: defining normative and symptomatic ranges in surgical patients. JAMA Facial Plast Surg. 2014;16:219–225. doi: 10.1001/jamafacial.2013.2473. quiz 232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Flynn D., van Schaik P., van Wersch A. A comparison of multi-item Likert and Visual Analogue Scales for the assessment of transactionally defined coping function. Eur J Psychol Assess. 2004;20:49–58. [Google Scholar]
- 5.Singh A., Patel N., Kenyon G., Donaldson G. Is there objective evidence that septal surgery improves nasal airflow. J Laryngol Otol. 2006;120:916–920. doi: 10.1017/S0022215106003410. [DOI] [PubMed] [Google Scholar]
- 6.Stewart M.G., Smith T.L., Weaver E.M. Outcomes after nasal septoplasty: results from the nasal obstruction septoplasty effectiveness (NOSE) study. Otolaryngol Head Neck Surg. 2004;130:283–290. doi: 10.1016/j.otohns.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 7.Most S.P. Anterior septal reconstruction: outcomes after a modified extracorporeal septoplasty technique. Arch Facial Plast Surg. 2006;8:202–207. doi: 10.1001/archfaci.8.3.202. [DOI] [PubMed] [Google Scholar]
- 8.Dinis P.B., Haider H. Septoplasty: long-term evaluation of results. Am J Otolaryngol. 2002;23:85–90. doi: 10.1053/ajot.2002.30987. [DOI] [PubMed] [Google Scholar]
- 9.Bothra R., Mathur N.N. Comparative evaluation of conventional versus endoscopic septoplasty for limited septal deviation and spur. J Laryngol Otol. 2009;123:737–741. doi: 10.1017/S0022215108004192. [DOI] [PubMed] [Google Scholar]