Abstract
The twin pregnancy is a risk pregnancy, being associated with a series of fetal and neonatal complications when compared to singleton pregnancies.
Ultrasound assessment of the fetal brain is mandatory in the prenatal screening for fetal, congenital and acquired anomalies. Fetal neurosonography is useful in the prenatal diagnosis of cerebral anomalies, combining ultrasonography with fetal ultrasound.
In this study, we assessed the Kanet score in two populations of pregnant women with dichorionic twin pregnancies (DC twin) (n=67) and monochorionic twin pregnancies (MC twin) (n=24). In the two groups we included pregnancies with normal fetal growth and pregnancies with discordant fetal growth (DC twin) and selective intrauterine reatriction (MC twin). For both groups, we assessed the antenatal Kanet score during three visits and compared the results with the neurodevelopment immediately after birth up to the two-year-old children.
The calculation of the average values of the Kanet score for dichorionic pregnancies revealed normal, maximal average values at all three visits, for all fetuses, no matter if they had normal growth or discordant growth. At the first and third visit, we observed statistically significant differences between the average Kanet scores in DC twins with discordant growth vs. DC twins with normal growth.
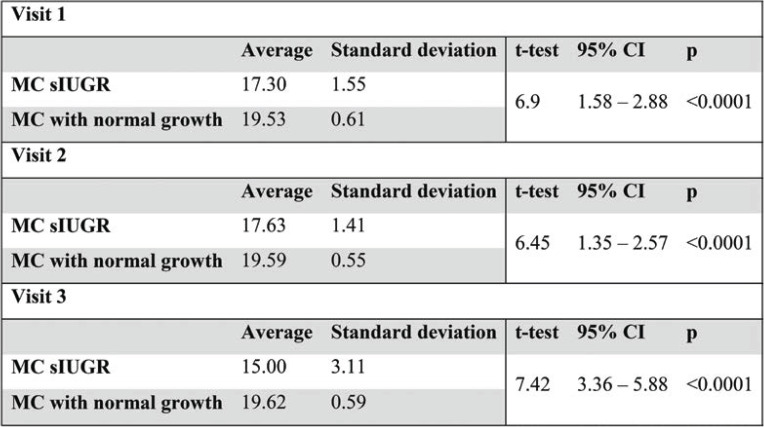
The analysis of average values of the Kanet score in the group of MC twin pregnancies revealed statistically significant differences between monochorionic twins with discordant growth vs. twins with normal growth at all three visits (p=0.0001), with average values between 17.30 and 19.62 being deemed normal.
Amiel-Tison score was used as a standard tool for the neurological assessment both immediately after birth and for children up to two years of age.
Keywords:Kanet score, dichorionic twin pregnancy, monochorionic twin pregnancy, discordant growth, selective intrauterine growth restriction, Prader Willi syndrome, neurodevelopment.
INTRODUCTION
It is widely recognized that twin pregnancy is a risk pregnancy, being associated with a series of fetal and neonatal complications (1).
Zygosity is very important when discussing the vascular consequences and neurological development of twins. All dizygotic twins and about one-third of monozygotic twins are dichorionic and have a low mortality and perinatal morbidity risk (2). Risks are greatly increased in monochorionic placentas, being present in about 20% of all twin pregnancies. Monochorionic placentation through inter-twin arterial anastomoses can have a number of important pathogenic implications for one or both of the fetuses (3). Twin pregnancies are more frequently associated with congenital anomalies when compared to singleton pregnancies. Most cases of cerebral palsy have their pathogenesis during fetal development and are thus a form of congenital anomaly, the etiology of which is uncertain (4). Congenital anomalies with cerebral palsy are an important cause of neurological disability in the newborn and infant from a twin pregnancy.
Ultrasound assessment of fetal brain is mandatory in the prenatal screening for fetal, congenital and acquired anomalies. Fetal neurosonography is useful in the prenatal diagnosis of cerebral anomalies, combining ultrasonography with fetal ultrasound (5).
Diagnosis of cerebral palsy remains one of the most difficult and challenging clinical situations in obstetrics and fetal ultrasonography. These difficulties could be overcome using 3D/4D ultrasound technology. This type of ultrasound has been imported in everyday practice of fetal ultrasound and offers higher quality images and information. Real-time images allow us not only to study fetal anatomy, but also to assess fetal movements and behaviour (6).
4D ultrasound provides real-time spatial images and enables the collection of information about mimics, gestures and facial expressions, making it possible to distinguish between normal and abnormal behavioral patterns (7). It is thus an extremely useful tool in early diagnosis of fetal brain impairment (8, 9).
Aim
The aim of this study is to assess neurodevelopment using the Kanet test (called Kurjak’s antenatal neurodevelopmental test) in monochorionic and dichorionic twin pregnancies, starting from the 28th week of amenorrhea. We also aim to correlate these results with the neonatal and follow-up assessments of the infant and child up to two years of age with the Amiel-Tison test in order to determine the degree of neonatal neurological impairment and especially the neurodevelopmental process during the first two years of life.
4D ultrasound assessment of fetal behavior and facial expressions, as well as the analysis of the usefulness of this test represent a diagnosis criterion for prenatal brain injury. Assessing twin pregnancies with normal and complicated evolution enables us to prenatally diagnose neurological impairment and confirm the cases that had been under suspicion from the antenatal period. This assessment can make the difference between normal and abnormal behavioral patterns (10).
Amiel-Tison neurological assessment at term age (11) is an important tool in the clinical assessment of the central nervous system. It enables us to identify a group of children with different degrees of neurological impairment right from the neonatal period, being of real use in both daily practice and research (12). It is valid for all full-term neonates or at 40 weeks corrected age and can be used up to the age of six years.
MATERIAL AND METHOD
This prospective-descriptive study was carried out over a period of 36 months, between February 2015 and January 2018, in the maternal- fetal medicine departments of three university hospitals: Elias Emergency University Hospital Bucharest, Panait Sârbu Clinical Hospital and Bucur Maternity Hospital (Sf. Ioan Emergency Clinical Hospital).
The study population consisted of 91 cases of twin pregnancy, 28 cases from Elias Emergency University Hospital, 37 from Panait Sârbu Clinical Hospital and 26 from Bucur Maternity Hospital. Twenty four (26.37%) pregnancies were twin monochorionic-diamniotic (MC) pregnancies, and 67 (73.63%) dichorionic (DC).
The initial study design consisted in the ultrasound assessment of pregnant women starting from the 28th week of gestation (first visit). We performed an assessment of both fetuses’ biometry, Doppler velocimetry of the middle cerebral artery with the measurement of pulsatility index (IP-MCA), peak-systolic velocity (PSV- MCA), umbilical artery pulsatility index (IP-UA) and ductus venosus, AFI measurement in both amniotic bags, and the Kanet score. Pregnant women were reassessed at the second visit, according to the associated pathology, at an interval of 2-4 weeks (30-32 weeks of amenorrhea). The third visit was at 34-36 weeks of amenorrhea. Additional Doppler ultrasound assessments were performed whenever the particular situation required it. They were absolutely necessary in choosing the optimum time of delivery in case of complicated twin pregnancies which could not go through all three stages of ultrasound follow- up, thus changing the initial design (13).
The ultrasound assessments were performed by five different operators with maternal-fetal medicine certification, who entered data into a common database.
All pregnant women had the first trimester screening and the screening for structural anomalies at 20-24 weeks of amenorrhea in the maternal-fetal medicine departments of the three clinics but also in independent centers. We were thus sure that the pregnancies were not complicated with chromosomal abnormalities or fetal structural abnormalities.
Ultrasound examination for the KANET antenatal neurological evaluation test should last between 15-20 minutes, and fetuses should be examined while they are awake. If the fetus is sleeping, the examination is postponed for 30 minutes or for the following day, for a minimum period of 14 to 16 hours. Certain parameters are observed during examination, each receiving 0/1/2 points (10). A normal KANET score is between 14-20 points, a borderline score between 6 and 13 points, and an abnormal one between 0-5 points.
When the test is abnormal or the score is borderline, it should be repeated every two weeks until delivery. Facial movements and the eye blinking are the most important parameters that are being observed, as a reflection of the general belief that ‘the face is the mirror of the brain’.
All pregnant women were admitted and gave birth in the clinics mentioned above. Newborns were assessed in order to identify a possible neonatal neurological impairment by means of: APGAR score at 5, 10, 20 minutes, fetal acid-base status – determination of arterial pH and base excess in a segment of umbilical cord clamped immediately after birth – neurological clinical examination of the newborn (vital signs, level of alertness, examination of the teguments, head and spine, motor functions, cranial nerves, reflexes, sensitive examination and behavioral assessment) and Amiel-Tison neurological assessment.
Amiel-Tison neurological assessment at term age (12) is an important tool in the clinical assessment of the central nervous system. It enables us to identify right from the neonatal period a group of children with different degrees of neurological impairment, being of real use in both daily practice and research. It is valid for all full-term neonates or at 40 weeks corrected age and can be used up to the age of six years. This assessment system includes 35 items clustered into 10 domains. The neuro-psychologically elements include alertness degree, passive tone in the trunk and limbs, active tone, primitive reflexes.
The scoring system used to describe normality or the degree of severity in case of abnormal response is:
• 0 – the typical full-term aspect, 40 weeks of amenorrhea, within normal limits
• 1 – it indicates an intermediate area, moderately deviated from normal
• 2 – a clear pathological result
• X – we should keep in mind the result obtained whenever a score seems inappropriate, especially if the results obtained cannot be classified neither normal nor pathological at that age.
This assessment uses a relatively simple method, which takes about 5 minutes to complete and includes a system of granting 0, 1, 2 points. It does not have a quantitative coding system, but because the assessment can be repeated at different time intervals, it enables us to establish a clinical profile of the child and thus to detect an early brain damage.
RESULTS
For data processing and systematization, we used Microsoft Office 365 Excel program. Graphic representations as well as statistical analysis of data were performed using the same program, along with add-ins such as WinStat and XLstat. For calculation of the statistical significance of the results obtained, we benefitted from the online support provided by Prof. Richard Lowry, Vassar College Poughkeepsie, NY USA, via www.vassarstats.net.
Following the statistical analysis of the group of pregnant women with dichorionic twin pregnancy (n = 67), 10 cases evolved towards discordant fetal growth (14.93%). We found statistically significant differences between the average weight of discordant DC twins and DC twins with normal growth at all three visits (p between 0.0001 and 0.02). The average weight is always higher in the dichorionic twins with normal growth (t-test).
Kanet score distribution analysis of the group of pregnant women with normal growth DC pregnancy after all three visits revealed that in all cases the Kanet score was normal for both fetuses, usually with maximum values. A single case (presented as case X) had Kanet score borderline values (score 13), for only one of the twins, at the first two visits; at the third visit, the twin had an abnormal Kanet score (score 5) (Tables 2, 3 and 4).
Regarding the Kanet score distribution in the group of twin pregnancies with discordant growth, we found normal values of the Kanet score in all cases, for both fetuses, at all three visits (Tables 2, 3 and 4).
For the calculation of the average values of the Kanet score in the group of dichorionic pregnancies, we used the student test (t-test) and found normal, maximal average values at all three visits for all fetuses, no matter if they had normal growth or discordant growth. We observed statistically significant differences between the average Kanet scores in DC twins with discordant growth vs. DC twins with normal growth, at the first and third visit (Table 5).
Out of the 24 cases of diamniotic-monochorionic twin pregnancies, seven evolved with abnormal fetal growth. Out of these, five cases (20.83%) progressed to selective intrauterine growth restriction (sIUGR) (without associative signs of twin-to-twin transfusion syndrome – TTTS), with progressive development starting from the end of the second trimester and the beginning of the third trimester.
Pregnancies were further evaluated by fetal Doppler velocimetry at one-week intervals, when the growth difference between the two fetuses exceeded 20%, according to international protocols (2).
When analyzing the average weight in the monochorionic sIUGR fetuses vs those with normal growth, statistically significant differences between the average weight of MC twins with sIUGR compared with MC twins with normal growth were observed by us in all three visits. At the first visit, the average weight of the sIUGR MC twins was significantly higher (p=0.04), while at the other two visits their average weight was significantly lower (p=0.004 / p=0.0001).
Regarding the distribution of the Kanet score in the group of MC pregnancies, we found normal values in 100% of cases, at all three visits, for pregnancies with normal growth as well as for those with sIUGR. Analysis of Kanet score average values in the group of MC twin pregnancies revealed statistically significant differences between the MC twins with discordant growth vs. twins with normal growth at all three visits (p=0.0001), with average values between 17.30 and 19.62 being deemed normal (Table 6).
We did not find significant correlations between the Kanet score and the weight of the MC twins at the three visits (p between 0.12 and 0.67).
In both groups analyzed by us, the calculated Amiel-Tison score was normal for all newborns, with four exceptions: one fetus in the group of DC twins (case X) and three fetuses with intrauterine growth restriction in the group of MC twins. The small number of exceptions did not allow for a statistical analysis of the variations of this score.
Descriptive study – clinical cases
A single case of dichorionic pregnancy (case X) was enrolled in the present study, the 34-year-old primipara pregnant woman being under observation in the hospital. We found concordant normal fetal growth of both fetuses, with normal Doppler velocimetry at all three visits.
Regarding the Kanet score, there were abnormal and rare movements of the limbs, blinking and yawning since the first visit in case of a twin (borderline score 13). The pregnancy was reassessed every two weeks according to recommendations (2). During the second visit, we found that the Kanet borderline score did not change for the twin with score 13, while on the third visit, the score decreased to 5. Biologically, we found an elevated à jeun glycemia followed by a normal glucose tolerance test. During the third trimester, the mother claimed she felt low fetal movements. The non-stress test was reactive. Middle cerebral artery and umbilical artery (UA) blood flow velocities and pulsatility indices were normal. An abnormal Kanet score (score 5) showed:
• isolated head anteflexion: 1
• cranial sutures and head circumference: 0
• isolated eye blinking: 1
• facial alterations: 1
• mouth opening (yawning or mouthing): 1
• isolated hand movements: 1
• leg movements: 0
• hand to face movements: 0
• fingers movements: 0
• gestalt perception of general movements: 0
A caesarean section was performed at term, with extraction of two live neonates: the first male neonate 2790 g, Apgar score 9, and the second male neoante 2710 g, Apgar score 9. Clinical examination at birth of case X revealed moderate hypotonia, low reactivity. During admission, he had persistent hypotonia, predominantly axial, low presence of reactivity, present ROT, sucking reflex, present swallowing, bottle- feeding difficult, slow weight ascending curve. The neurological exam revealed a hypotonic baby, ROT very hard to get, batrachian position, low tonus, low power, reactivity: difficult awakening, does not cry, gets tired while feeding, short staring. Other paraclinic investigations were normal (blood, transfontanellar ultrasound, genetic testing). The result of Methylation – Specific MLPA – indicates a Prader Willi syndrome.
The Amiel-Tison test at birth was 2, which persisted for up to 18 months. Assessment at 24 months revealed an improvement in hypotonia and other neurological anomalies (score 1).
The five cases of MC pregnancies with sIUGR evolved as described below.
Case 1. Enrolled in the study at 28 weeks of amenorrhea, with one of the fetuses with a 15% sIUGR compared to the second fetus, a positive end-diastolic flow in the UA (sIUGR Type I) (14), AFI 3. The Kanet score of the fetus with growth restriction was 17 (normal score). At the second visit, it was found that the difference between the estimated fetal weights of both fetuses increased, with a twin’s aggravation of growth restriction (a difference of 23%), with end-diastolic flow present in the UA (type I), Kanet score 14 – normal. At the third visit, there was a 24% difference between the estimated fetal weights, with intermittent absent end-diastolic flow in the UA (type III) (15), Kanet score 13 (borderline) of the sIUGR fetus. A caesarean section was performed at 34 weeks. The postnatal neurological assessment of both neonates was within normal parameters, corresponding to the gestational age. Amiel-Tison score was normal (40 weeks corrected age), a score that continued to be normal throughout the follow-up.
Case 2.sIUGR diagnosed at 26 weeks (with a 15% growth difference between the two fetuses) and enrolled in the study at 28 weeks. During the first visit, Doppler ultrasound assessment was normal, Kanet score 19. At the second visit, the growth difference between the two fetuses was still 15%, the Doppler ultrasound assessment was within normal parameters, Kanet score 17. The third visit revealed a growth difference between the two fetuses of 22% and ultrasound showed intermittent absent end-diastolic flow in the umbilical artery of the growth-restricted twin (sIUGR type III) (14). Kanet score was 12 – borderline. A caesarean section was performed after the third visit, at 34 weeks and three days, as dictated by Doppler ultrasound changes (16). Postnatal neurological assessment of both neonates was corresponding to the gestational age (prematurity). Subsequent neurological assessments and Amiel-Tison score at 40 weeks corrected age were normal. Assessments were normal throughout follow-up.
Case 3.Case enrolled at first visit with a 17% growth difference, normal Doppler ultrasound assessment, Kanet score 14 – borderline (assessment of 80 minutes, with 30 minutes break). The second visit showed a 25% growth difference between the two fetuses, with ultrasound showing reversed end-diastolic flow in the umbilical artery of the growth-restricted twin (sIUGR type II) (16). The Kanet score was 5 – low (assessment of 40 minutes, 30 minutes break). A caesarean section was performed after the second visit, at 32 weeks, due to Doppler ultrasound changes. The neurological assessment of the newborn with growth restriction revealed a discrete change in the neurological status, with axial hypotonia (accentuated by prematurity), the Amiel-Tison score at 40 weeks corrected age being moderately deviated from normal (1). The evolution was favorable, the neurological assessment from six months and later being normal (Amiel-Tison score 0)
Case 4.sIUGR diagnosed at 26 weeks (with a 20% growth difference between the two fetuses) and enrolled in the study at 28 weeks. At the first visit, the Doppler ultrasound assessment was normal, Kanet score 18. At the second visit, the growth difference between the two fetuses remained 20%, the Doppler ultrasound assessment was within normal parameters, Kanet score 17. The third visit revealed a growth difference between the two fetuses of 25%, end-diastolic flow positive in the UA (sIUGR type I) (14). Kanet score was 11 – borderline. A caesarean section was performed after the third visit, at 36 weeks, as dictated by SOGR guides and protocols of the clinics. The newborn with sIUGR evolved favorably from the neurological point of view, the Amiel-Tison score being normal at 40 weeks corrected age and later.
Case 5.Enrolled at the first visit with a growth difference between the two fetuses of 20%, diagnosed with sIUGR from 25 weeks. The ultrasound shows reversed end-diastolic flow in the umbilical artery of the growth-restricted twin (sIUGR Type II) (14), reversed a wave in the ductus venosus. The Kanet score of the fetus with growth restriction was 5 – abnormal. The case management consisted in daily Doppler and NST monitoring, with respiratory distress prophylaxis with dexamethasone 6 mg, four doses. A caesarean section was performed at 29 weeks and three days. Postnatal neurological assessment revealed moderate global neurological deficit, determined by prematurity and etiopathogenesis of the underlying disease (for the sIUGR newborn).
DISCUSSION
Kanet score analysis in the group of pregnant women with normal growth dichorionic pregnancy after all three visits revealed that the Kanet score was normal for both fetuses in all cases. Case X in discussion, from a dichorionic pregnancy and postnatally diagnosed with Prader Willi syndrome, presented borderline values of Kanet score (score 13) at the first two visits and an abnormal Kanet score of 5 at the third visit. In that case, there was a correspondence between the antenatal assessment by the Kanet test and the postnatal neurological one. However, the origin of neurological disorders is in the genetic anomalies postnatally revealed. Prader- Willi syndrome is an imprinting disorder that can occur via three main genetic mechanisms: maternal uniparental disomy, paternal deletion of genes within the 15q11.2-q13 region and an imprinting center defect (17, 18).
Both healthy parents with non-genetic anomalies and a methylation-specific multiplex ligation- dependent probe amplification (MS-MLPA) and array-based comparative genome hybridization (aCGH) analyses test positive for a de novo microdeletion involving BP2 and BP3 (type 2) at 15q11.2-q13, a very rare finding (19).
Regarding the distribution of the Kanet score in the group of DC twin pregnancies with discordant growth, we found normal values of the Kanet score in all cases, during all three visits, for both fetuses, and normal postnatal neurological assessment. Follow-up visits were also normal, demonstrating and strengthening the correlation between the normal values of this score and the normal postnatal neurological status in infants and children up to two years. The same correlation was found in normal growth MC pregnancies.
A special note is the study of fetal behavior and the clinical integration of the Kanet neurological score in an attempt to make possible correlations between abnormal values of this score and certain postpartum complications in MC pregnancies complicated with sIUGR. In hindsight, even if we found abnormal Kanet scores, the association with postpartum neurological anomalies was unclear. Although the antenatal Kanet score was borderline or abnormal for sIUGR fetuses from MC pregnancies, the postnatal neurological evolution of these children was favorable, either progressively or slowly due to prematurity and IUGR etiopathogenesis.
While an abnormal Kanet score seems to be largely associated with the occurrence of cerebral palsy at two years postpartum, we did not find any case of cerebral palsy in our study. The results are obviously limited by the small number of subjects and the subjectivity involved in the ultrasound examination performed by several operators.
CONCLUSION
The antenatal diagnosis of neurological impairment is very difficult. Usually, neurological impairment is postnatally diagnosed, within a few months or years after birth. It is useful to diagnose neurological impairments with genesis during intrauterine life before birth, in order to enable an efficient early postnatal intervention, thus improving the neurological outcome of such children (20).
In conclusion, the advantages of technological progress of the fetal ultrasound reside in the possibility of a complete neurological and neurobehavioural assessment of the fetus (21), thus identifying right from the antenatal period the abnormal behavioural profile and anticipating any postnatal neurological anomalies, others than the cerebral palsy, which has already been diagnosed (22).
Although neuroimaging techniques have increasingly improved, prenatal counselling remains a major challenge, as the prediction of brain function and neurological prognosis are often uncertain. Prenatal ultrasound examination, including the Kanet test and a postnatal assessment enable the process of communication with parents, offering them the medical, psychological and social support to facilitate an optimal development of children with neurological impairment.
Conflicts of interest: none declared.
Financial support: none declared.
TABLE 1.
KANET score interpretation, with permission, Kurjak et al. (8, 11)
TABLE 2.
Kanet score distribution in dichorionic twins at the first visit
TABLE 3.
Kanet score distribution in dichorionic twins at the second visit
TABLE 4.
Kanet score distribution in dichorionic twins at the third visit
TABLE 5.
Comparisons between Kanet score average values in the dichorionic twins at the three visits
TABLE 6.
Comparisons between average values of the Kanet score in MC twins at the three visits
Contributor Information
Mihaela BOT, Department of Obstetrics-Gynecology and Neonatology, Elias Emergency Hospital Bucharest, Bucharest, Romania.
Radu VLADAREANU, Department of Obstetrics-Gynecology and Neonatology, Elias Emergency Hospital Bucharest, Bucharest, Romania.
Anca BURNEI, Department of Obstetrics-Gynecology and Neonatology, Elias Emergency Hospital Bucharest, Bucharest, Romania.
Alexandra MUNTEANU, University of Medicine and Pharmacy Carol Davila, Bucharest, Romania.
Ioana CALO, Department of Obstetrics-Gynecology and Neonatology, Elias Emergency Hospital Bucharest, Bucharest, Romania.
Simona VLADAREANU, Department of Obstetrics-Gynecology and Neonatology, Elias Emergency Hospital Bucharest, Bucharest, Romania.
References
- 1.Bot M, Burnei-Rusu A, Zamfirescu V, et al. Hemodynamic And Neurological Changes In Twin-to-Twin Transfusions. Proceedings of the 5th Congres of SRUOG 2017, FiLOdiritto Editore 2017. 2017.
- 2.Royal College of Obstetricians and Gynaecologists. Management of Monochorionic Twin Pregnancy. BJOG. 2016.
- 3.Chauhan SP, Scardo JA, Hayes E, et al. Twins: prevalence, problems, and preterm births. Am J Obstet Gynecol. 2010;203:305. doi: 10.1016/j.ajog.2010.04.031. [DOI] [PubMed] [Google Scholar]
- 4.Pharoah POD. Dundar Y. Monozygotic twinning, cerebral palsy and congenital anomalies. Human Reproduction Update. 2009;6:639–648. doi: 10.1093/humupd/dmp019. [DOI] [PubMed] [Google Scholar]
- 5.Merz E, Abramowicz JS. 3D/4D Ultrasound in Prenatal Diagnosis: Is it Time for Routine Use? Clin Obstet Gynecol. 2012;1:336–351. doi: 10.1097/GRF.0b013e3182446ef7. [DOI] [PubMed] [Google Scholar]
- 6.Kurjak A, Pooh R, Tikvica A, et al. Assessment of fetal neurobehaviour by 3D/4D ultrasound. Fetal Neurology. 2009. pp. 220–250.
- 7.Kurjak A, Carrera J, Medic M, et al. The antenatal development of fetal behavioral patterns assessed by four-dimensional sonography. J Matern Fetal Neonatal Med. 2005;6:401–416. doi: 10.1080/14767050400029657. [DOI] [PubMed] [Google Scholar]
- 8.Kurjak A, Miskovic B, Andonotopo W, et al. How useful is 3D and 4D ultrasound in perinatal medicine? J Perinat Med. 2007;1:10–27. doi: 10.1515/JPM.2007.002. [DOI] [PubMed] [Google Scholar]
- 9.Stanoevici M, et al. An Attempt to Standardize Kurjak’s Antenatal Neurodevelopmental Test: Osaka Consensus Statement. Donald School. Journal of Ultrasound in Obstetrics and Gynecology. 2011;4 [Google Scholar]
- 10.Gosselin J, Gahagan S, Amiel-Tison C. The Amiel-Tison neurological assessment at term: Conceptual and methodological continuity in the course of follow-up. Ment Retard Dev Disabil Res Rev. 2005;1:34–51. doi: 10.1002/mrdd.20049. [DOI] [PubMed] [Google Scholar]
- 11.Kurjak A, Antsaklis P, Stanojevic M, Vladareanu R, et al. Multicentric studies of the fetal neurobehavior by KANET test. J Perinat Med. 2017;6:717–727. doi: 10.1515/jpm-2016-0409. [DOI] [PubMed] [Google Scholar]
- 12.Paro-Panjan D, Neubauer D, Kodric J, Bratanic B. Amiel-Tison Neurological Assessment at term age: Clinical application, correlation with other methods, and outcome at 12 to 15 months. Developmental Medicine & Child Neurology. 2005;1:19–26. doi: 10.1017/s0012162205000046. [DOI] [PubMed] [Google Scholar]
- 13.Buca D, Pagani G, Rizzo G, et al. Outcome of monochorionic twin pregnancy with selective intrauterine growth restriction according to umbilical artery Doppler flow pattern of smaller twin: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2017;5:559. doi: 10.1002/uog.17362. [DOI] [PubMed] [Google Scholar]
- 14.Gratacós E, Lewi L, Muñoz BA, et al. A classification system for selective intrauterine growth restriction in monochorionic pregnancies according to umbilical artery Doppler flow in the smaller twin. Ultrasound in obstetrics & gynecology: the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2007;1:28–34. doi: 10.1002/uog.4046. [DOI] [PubMed] [Google Scholar]
- 15.Petca A, Bot A. IUGR – Improving the outcomes. Obstetrica si Ginecologia. 2012;4:261–266. [Google Scholar]
- 16.Bot M, Petca A. Doppler changes in the fetuses with intrauterine growth restriction. What is new? Current Health Sciences Journal. 2013;39:62–67. [Google Scholar]
- 17.Cassidy SB, Driscoll DJ. Prader-Willi syndrome. Eur J Hum Genet. 2009;17:3–13. doi: 10.1038/ejhg.2008.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Horsthemke B, Wagstaff J. Mechanisms of imprinting of the Prader-Willi/Angelman region. Am J Med Genet A. 2008;146A:2041–2052. doi: 10.1002/ajmg.a.32364. [DOI] [PubMed] [Google Scholar]
- 19.Han JY, Park J, Jang W, et al. A twin sibling with Prader-Willi syndrome caused by type 2 microdeletion following assisted reproductive technology: A case report. Biomed Rep. 2016;1:18–22. doi: 10.3892/br.2016.675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vladareanu S, Vladareanu R, Bot M. Neurological outcomes in twins. Chapter in The Fetus as a Pacient – Current Perspectives – Frank A. Chervenak, Sanja Kupesic Plavsic, Asim Kurjak. . Jaypee Brothers Medical Publishers. 2020.
- 21.Turan OM, Turan S, Gungor S, et al: Progression of Doppler abnormalities in intrauterine growth restriction. Ultrasound Obstet Gynecol. 2008;32:160–167. doi: 10.1002/uog.5386. [DOI] [PubMed] [Google Scholar]
- 22.Kurjak A, Predojevic M, Stanojevic M, et al. Intrauterine growth restriction and cerebral palsy. Acta Inform Med. 2012;2:64–82. doi: 10.5455/aim.2010.18.64-82. [DOI] [PMC free article] [PubMed] [Google Scholar]