Abstract
Background: Irrational prescribing results produce a negative impact on health and economy of both individuals and society, leading to wastage of resources and widespread health hazards.
Method: Outpatients with mild, moderate, and severe COPD were included. Several parameters were noted: patient’s age and gender, outpatient (OPD) ID number, date of admission, occupation, h/o smoking, alcohol consumption, etc, disease condition details (duration, gradation as mild, moderate and severe, and co-existing diseases), prescribed medication details (dose, frequency, route of administration, and duration). Drug selection was assessed as per GOLD guidelines, the severity of disease was categorized according to the same guidelines, and medication efficacy was evaluated by treatment outcome according to the modified MRC dyspnoea scale.
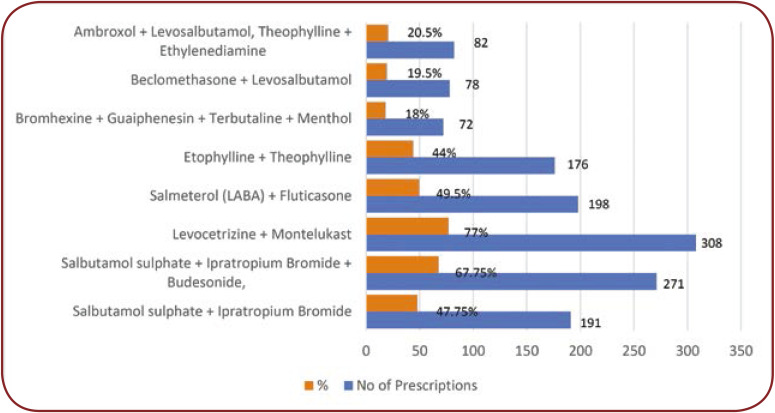
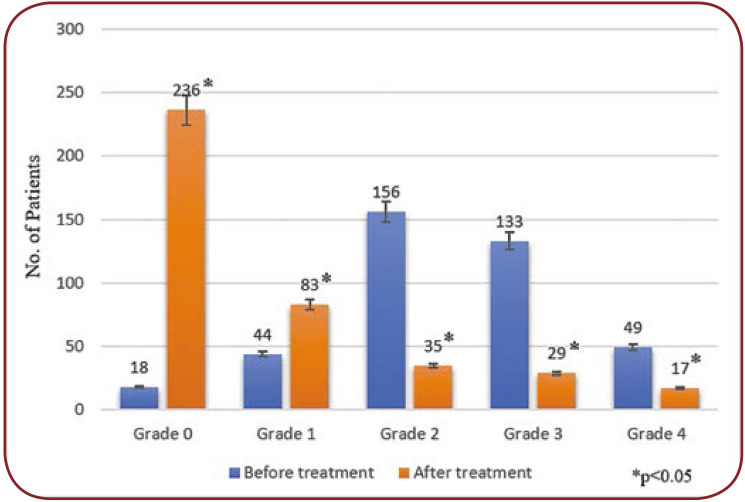
Results: Inhalation route (36.95%) was the most preferred route of drug administration in this study, followed by the parenteral route (34.34%), and enteral route (28.71%). Adherence to GOLD 2015: All patients (n=400) were categorized to Gold stages I to IV based on the severity of COPD. Amongst these patients, 11 were in stage I, 146 in stage II, 184 in stage III, and 59 in stage IV. The majority of subjects received fixed-dose combination therapy: levocetirizine + montelukast (77%) and least bromhexine + guaiphenesin + terbutaline + menthol (18%). Dyspnoea status was graded from 0 to 4 according to the modified MRC dyspnea scale. Out of the 400 patients, 18 had grade 0, 44 grade 1, 156 grade 2, 133 grade 3, and 49 grade 4.
Conclusion: Overall, data from this analysis suggest that adherence to GOLD guidelines does not have a perceivable impact on symptom prevalence, exacerbation rate or lung function. Male sex, asthma and severe co-morbidities as a cerebrovascular insult could be associated with a risk for frequent exacerbations.
Keywords:chronic obstructive pulmonary disease, prescription pattern, GOLD guidelines, modified MRC dyspnoea scale.
INTRODUCTION
All over the world, inappropriate/irrational prescribing pattern is a significant problem of healthcare delivery, especially in developing countries (1). Irrational prescribing has a negative impact on health and economy of both individuals and society, leading to wastage of resources and widespread health hazards (2).
Drug utilization studies are powerful tools to explore and ascertain the role of drugs in society. These studies contribute to sound sociomedical and health economic basis for healthcare decision making. Despite the complexity of drug use, several indicators have been developed, standardised and evaluated by the World Health Organization (WHO) (3). These indicators are used not only to measure drug use in outpatient facilities and provide measures of the optimal resource use in those facilities, but also to help correcting deviations from expected standards and planning.
The National Heart Lung and Blood Institute reports that there are 24 milion people with chronic obstructive pulmonary disease (COPD), of which only 10 milion adults are estimated to have been diagnosed with COPD, while the remaining 12 milion individuals are undiagnosed (4). COPD requires long-term treatment, which may lead to irrational drug use and certain sequela.
In COPD, pharmacotherapy aims to reduce symptoms, decrease the frequency and severity of exacerbations, improve health status and exercise tolerance. Bronchodilators represent the mainstay of pharmacological management of COPD. Short-acting bronchodilators are given for immediate symptom relief, one or more long-acting bronchodilators (long-acting beta 2 agonists (LAβAs) or long-acting muscarinic antagonist (LAMAs) are used for long term maintenance treatment in subjects with moderate to severe disease. Inhaled corticosteroids (ICS) are central to the treatment of asthma, but their role is controversial in the management of COPD. In COPD, ICS are primarily given to decrease the risk of exacerbations. The new Global Initiative for Chronic Obstructive Lung Disease (GOLD) strategy recommends the addition of a second bronchodilator in patients with moderate airflow obstruction, reserving the ICS use along with a LABA and/or LAMA for those with severe or very severe airflow obstruction and/or two or more exacerbations of COPD per year (5).
But there is evidence that prescriptions are not always written according to GOLD recommendations or other national guidelines (6), resulting in a high proportion of patients being unnecessarily treated with ICS and exposed to the risk of side effects in an undue manner.
A few studies have evaluated the patterns of drug therapy use relative to GOLD guidelines and have identified several gaps in the pharmacological management of COPD (7, 8).
Screening of prescriptions and evaluation of drug utilization can identify the issues regarding drug use and helps in contributing feedback to prescribers to create awareness about irrational drug use. Drug utilization studies provide useful insights into current prescribing practices and can thus help to reform and update practices in clinical medicine and pharmacotherapy (9). Keeping this in the background, the present study is undertaken to analyze the prescribing pattern, extent, rationality, frequency of drug use in COPD and adherence to GOLD guidelines (10) in the treatment of COPD.
METHODOLOGY
This was an observational prospective sampling study, conducted on 400 consecutive cases of COPD between January – December 2017 in the Medicine Department OPD after taking consent from each patient or patient’s guardian/ relative as well as permission from the Institutional Ethics Committee (Ref No: BRIMS/Ethical Committee/ 57/2015). Relevant data were personally collected by the investigator from all patients, as indicated in a specially designed performa.
Inclusion criteria: patients with mild, moderate, and severe COPD attending the outpatient Department of Medicine.
Exclusion criteria: patients with tuberculosis or bronchial asthma, terminally ill cancer patients, patients in intensive care unit (ICU), and pregnant and lactating women.
Relevant data were collected, including the following details:
- demographic data: patient age, gender, OPD ID number, date of admission, occupation, h/o smoking, alcoholic, etc;
- disease condition details: duration, gradation and co-existing diseases, if any;
- prescribed drug details: dose, frequency, route of administration, and duration.
Drug selection was assessed as per GOLD guidelines (11), disease severity was categorized according to guidelines (12), and medication efficacy was evaluated by treatment outcome according to modified MRC dyspnoea scale (13). The methodology used by us is shown in the flow chart presented in Figure 1.
Drugs used in COPD were categorized into three categories: bronchodilators, anticholinergics, and steroids. Fixed drug combinations were calculated separately. Adherence to GOLD guidelines (10) was studied by assuming that drugs recommended as the first line should be the most frequently prescribed ones with the highest utilization.
RESULTS
In the current study we analysed prescription data of 400 patients [278 males (69.5%) and 122 females (30.5%)], with a mean age of 42.7±13.7 years (42.8±13.6 for males and 42.6±13.9 for females).
Smoking and alcohol consumption history. The 400 patients were divided based on their addictive habits such as smoking and alcohol consumption. Thus, 158 (39.5%) patients were smokers and 62 (15.5%) alcoholics, 222 (55.5%) were non-smokers and 322 (80.5%) non-alcoholics, and 20 (5%) were ex-smokers and 16 (4%) ex-alcoholics.
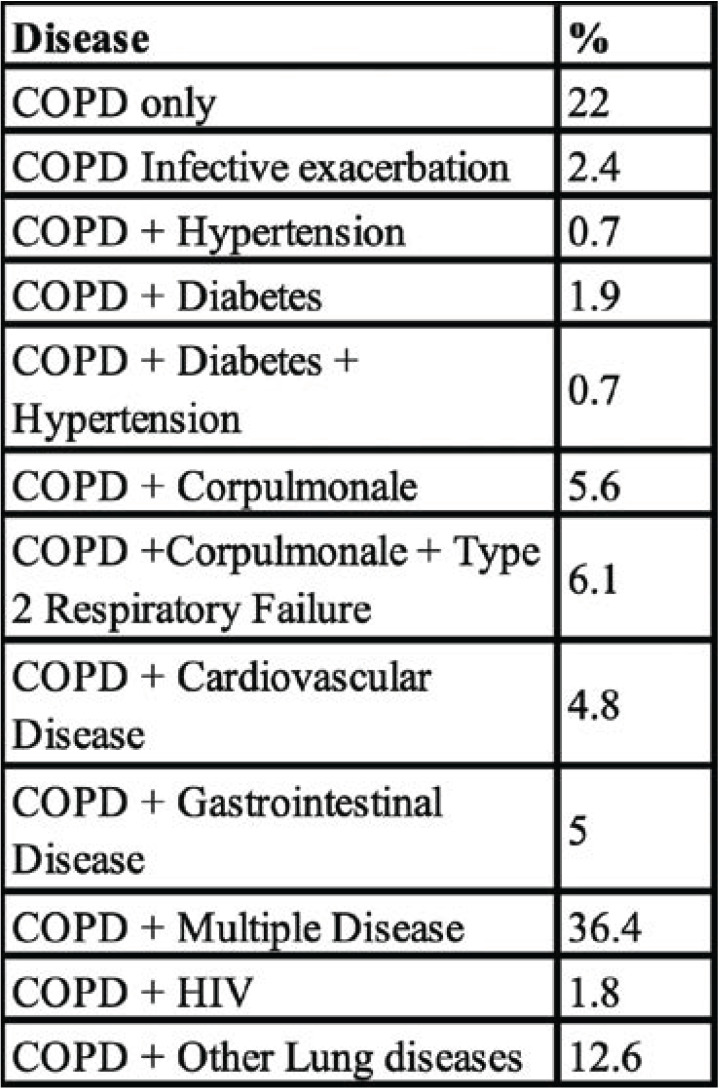
Disease comorbid status. The majority of patients were suffering from comorbid conditions. Among the 400 COPD cases, 22% of patients had only COPD and 78% comorbid conditions (Table 1).
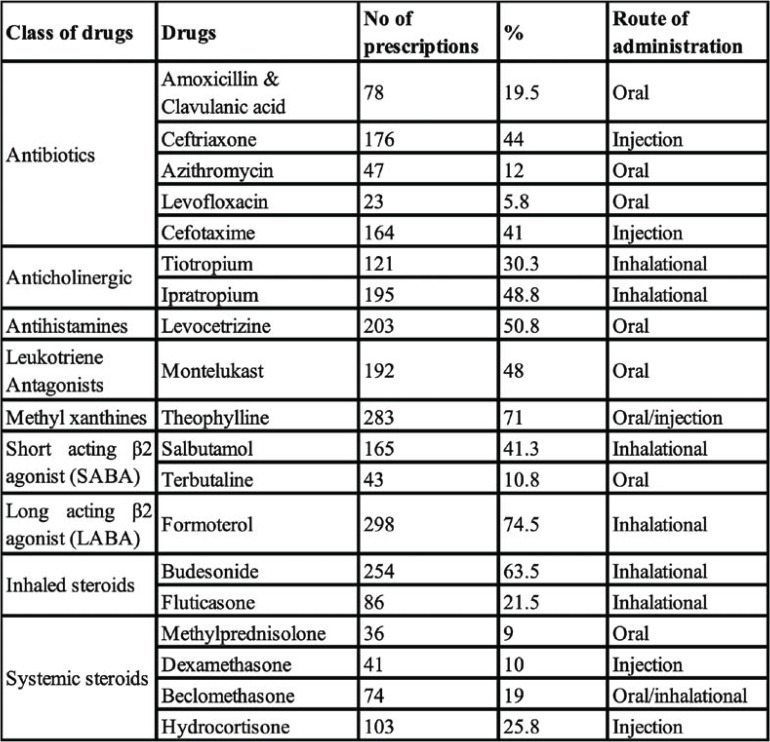
Dosage forms/routes of administration. Inhalation route (36.95%) was the most common route of drug administration in this study, followed by the parenteral route (34.34%) and enteral route (28.71%) (Table 2).
Drugs used by class. Antibiotics were given to all included patients, followed by bronchodilators, anticholinergic, short-acting b2 agonist and disease controlling drugs such as inhaled steroids and methylxanthine group drugs (Table 2).
The modified Medical Research Council (mMRC) scale. Before treatment, patients were interviewed for dyspnoea status, which was graded from 0 to 4, according to the modified MRC dyspnea scale (Figure 3).
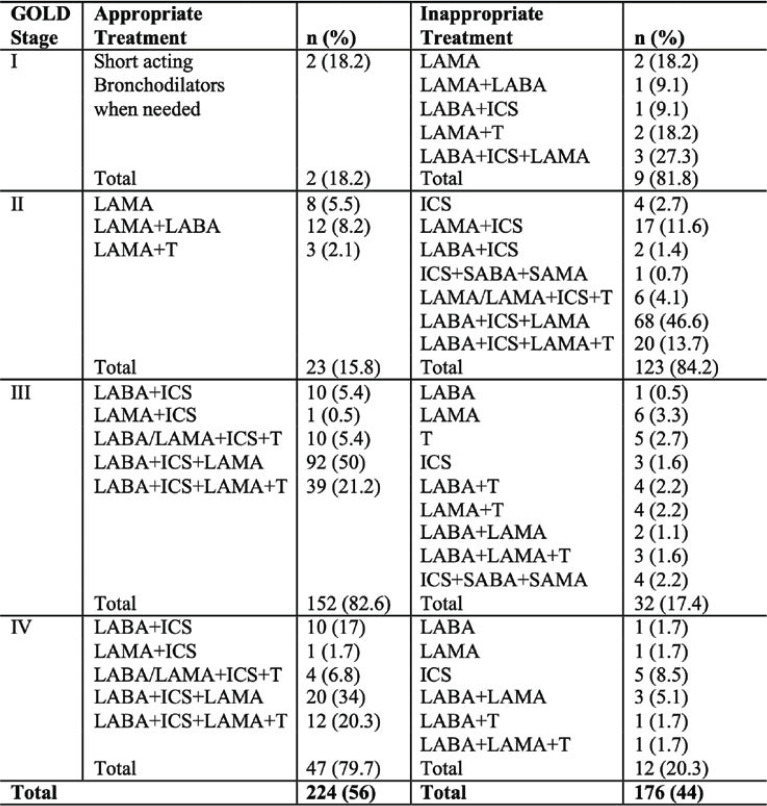
Adherence to GOLD 2015. All the 400 patients were categorized to GOLD stages I to IV based on COPD severity. Amongst these patients, 11 were in stage I, 146 in stage II, 184 in stage III, and 59 in stage IV. Appropriate and inappropriate treatment approaches in different stages are presented in Table 3.
DISCUSSION
Effect of gender. In our study, the incidence of COPD was higher in males than females, which was in accordance with the reports of Niffy A. et al (13) and Gigi A. et al. (14).
Effect of the season. The COPD patient inflow was the highest in October (14.5%) and the lowest in May (2%). The American Journal of Respiratory and Critical Care Medicine published an article showing that individuals with COPD and seasonal allergies were more likely to exhibit symptoms of wheezing and chronic coughing (15). A new study at Johns Hopkins University suggested that individuals with COPD and allergic disease are at higher risk for COPD exacerbations (16).
Effect of smoking. The present study results were in accordance with those of Niffy A. et al. (13). Tobacco smoking affects multiple organ systems, resulting in numerous so-called tobacco- related diseases, including various chronic respiratory diseases, mainly chronic obstructive pulmonary disease (COPD) as well as enhanced levels of carbohydrate deficient transferrin (CDT), an increased number of T lymphocytes and macrophages, and oxidants–antioxidants imbalance (17).
Effect of alcohol consumption on COPD. The present study results were in accordance with those of Niffy A et al. (13). Garshick E et al. (18) reported that lifetime alcohol consumption was a significant predictor of chronic cough and chronic phlegm but no symptoms. Smoking and alcohol consumption interactions were inversely correlated to the independent effects of alcohol. Frantz S et al. (19) showed an association between increased CDT and T lymphocytes and lower FEV1 as well as a diffusing capacity for carbon monoxide (DL, CO) in subjects drinking alcohol, also after adjustments for potential confounders. No such associations were observed in never-smokers.
Drug therapy. All the 400 prescriptions for subjects of our study contained more than three drugs, which is in accordance with the previous studies of Unni A. et al. (20) and Niffy A. et al. (13). The prescription of more than three drugs (multidrug therapy) for one patient may suggest the possibility of some patients presenting with an acute and chronic exacerbation of COPD and bronchial asthma with or without co-morbid conditions, which requires antibiotic and corticosteroid treatment.
Route of administration. Maintenance therapy with nebulizers should be employed in elderly patients as well as in those with severe disease and frequent exacerbations. For some patients, using both nebulizers and pressurized metered-dose inhalers provided the best combination in terms of efficacy and convenience. Our study results are supported by those of Dhand R. et al. (21). Aerosol therapy is an important administration route in the treatment of COPD to assure drug delivery to the lungs. Virchow J. C. et al. (22) suggested that the inhaler technology has the potential to improve asthma and COPD management.
Drugs. It was found that antibiotics were given to all patients, while the second most commonly prescribed drugs included anticholinergics, short-acting β2 agonists and disease controlling drugs such as inhaled steroids and methylxanthine group drugs. Our study results are in correlation with those of Vikneswari et al. (23).
In a study by Sharon Sunil et al. (24), 45% of patients received combination therapy, in which salbutamol + ipratropium bromide + budesonide (40%) was the preferred combination, followed by etophylline + theophylline (22%) and budesonide + formoterol (14%).
In the study of Faheemuddin M. D. et al. (25), COPD patients received a combination of bronchodilators consisting in an β2 agonist and an anticholinergic (salbutamol + ipratropium bromide).
In the present study, the most used combinations included levocetirizine + montelukast (77%), salbutamol sulphate + ipratropium bromide + budesonide (67.75%), and salmeterol (LABA) + fluticasone (49.5%) (Figure 2). Drug combinations were used to decrease COPD symptoms, increase drug effectiveness and decrease the medication dose. Mir S. Adil et al. (26) reported that LABA/SABA-ICS combination therapy was far better than LABA/SABA monotherapy in controlling COPD, because it not only reduced the risk of exacerbations but also improved QOL and airflow measures. Due to its antiinflammatory activity, combination therapy may help in reducing the risks of re-hospitalization or death.
According to Basavaraju Thejur Jayadeva et al. (27), short-acting β2 agonists (i.e., salbutamol) are so commonly prescribed due to their rapid onset and low cost. In our study, injection hydrocortisone (61%) was also used in managing an acute asthma attack. It prevents the side effect of inhaled medication, which irritates the respiratory tract.
In a study conducted by Niffy Abraham et al. (13), the majority of patients received a fixed dose combination therapy, including salbutamol sulphate + ipratropium bromide (23.19%) and salbutamol sulphate + ipratropium bromide + budesonide (42.23%). In another study (28), most of the patients were given the same combination therapy, consisting in salbutamol sulphate + ipratropium bromide (23.19%) and salbutamol sulphate + ipratropium bromide + budesonide (42.23%).
Efficacy of COPD medication as per the mMRC scale. The modified MRC score was >2 in the majority of COPD subjects before treatment. After receiving specific COPD medication, the score was improved in a significant number of patients, proving the efficacy of drugs used for the treatment of COPD.
Adherence to GOLD 2015. Our study results showed that the overall adherence to GOLD guideline treatment recommendations for different stages of COPD was 56%. Appropriate and inappropriate treatment approaches in different stages are presented in Table 3.
In stage I (n=11), only one patient (18.18%) was treated with an appropriate regimen, and others were overtreated with regular long-acting bronchodilators or combination of bronchodilators and ICSs. The common treatment option was LABA-ICS-LAMA (27.27%).
In stage II (n=146), adherence to GOLD recommendations was 15.75%, and this group was also overtreated by a combination of bronchodilators and ICSs. In this stage, frequently preferred treatment options included LABA-ICS-LAMA (46.6%), LABA-ICS-LAMA theophylline (T) (13.7%), and LABA-ICS (11.6%). Of all stage II patients (n=146), 84.3% received an ICS-based treatment.
In stage III (n=184), adherence to guidelines increased to 82.6% due to the wide use of bronchodilator ICS combinations. The most preferred drug combination consisted in LABA-ICS-LAMA (50%), followed by LABA-ICS-LAMA-T (21.2%). Undertreatment was due to inappropriate treatment with regular long-/short-acting bronchodilators without ICS use, 1.6% of patients receiving ICS alone without any bronchodilators.
In stage IV (n=59), the appropriate treatment rate was also high, as 79.7% of subjects were given dual, triple, and quadruple therapies with bronchodilators and ICSs. The most preferred regimens were LABA-ICS-LAMA (34%) and LABA-ICS-LAMA-T (20.3%) combinations. Of all stage IV patients, 88.1% received an ICS-based medication. Inappropriate treatment approaches were represented by administering one or more long-acting bronchodilators without ICS or using only ICS (8.5%).
Stage I patients were overtreated with regular long-acting bronchodilators or combination of bronchodilators and ICSs, while guidelines recommended short-acting bronchodilators as initial therapy. Only 15.8% of stage II patients received an appropriate treatment, and this was mainly due to overtreatment, which was combined with long-acting bronchodilators and ICS in 84.3% of subjects. The ICS-based medication was frequently used for patients in all stages (36.4% in stage I, 84.3% in stage II, 84.7% in stage III, and 88.1% in stage IV), mostly as a part of combination therapy (Table 3).
Overall, 56% of patients were treated according to guideline recommendations. Most of the provider’s guideline adherence studies have described the current practices of general practitioners. Two studies have also reported similar rates of adherence to guideline recommendations for COPD patients (37.9%–54.7%) among pulmonologists in other countries (29, 30).
CONCLUSION
Our study showed that COPD treatment had low rates of adherence to GOLD guidelines. Overall, data provided by this analysis suggest that adherence to GOLD guidelines does not have a perceivable impact on symptom prevalence, exacerbation rate or lung function. Male sex, asthma and severe co-morbidities as a cerebrovascular insult could be associated with a risk for frequent exacerbations.
We suggest that new strategies are needed to achieve a standardized approach for the treatment of COPD, aiming to improve adherence to guideline recommendations, with particular focus on therapeutic indications and overtreatment.
Conflict of interests: none declared
Financial support: none declared.
Acknowledgments: My sincere thanks to Dr. Channanna C, Director, Bidar Institute of Medical Sciences, Bidar, for permitting me to undertake this research work as a part of my M.D. curriculum. Also, I would like to express my gratitude and thanks to Dr. Gajanan P Kulkarni, Head, Department of Pharmacology, staff, fellow colleagues, friends and family members for their constant support and encouragement throughout my entire career, and for making me who I am today.
FIGURE 1.
Flow chart of methodology
TABLE 1.
Disease comorbid status
TABLE 2.
Drug utilisation pattern
FIGURE 2.
Drugs prescribed in fixed dose combinations
FIGURE 3.
Efficacy of drugs as per the mMRC scale
TABLE 3.
Treatment adherence to GOLD 2015
Contributor Information
DB JYOTHI, Vijayanagar Institute of Medical Sciences (VIMS), Bellary, Karnataka, India.
S VIJAY PRASAD, Department of Pharmacology, Govt Medical College, SHIVPURI, Madhya Pradesh, India.
Yakaiah VANGOORI, Sri Ramachandra Institute of Higher Education and Research (SRIHER) Chennai and Santhiram Medical College, Nandyal, AP, India.
Ambadasu BHARATHA, Faculty of Medical Sciences, The University of the West Indies, Cave Hill Campus, Barbados, WI.
References
- 1.Enato EFO, Madadi P, Souny AA. Assessment of disease profiles and drug prescribing patterns of healthcare facilities in Edo state, Nigeria. J Public Health Africa. 2012;e25:101–106. [Google Scholar]
- 2.Ghimire S, Nepal S, Bhandari S, et al. A prospective surveillance of drug prescribing and dispensing in a teaching hospital in western Nepal. J Pak Med Assoc. [Internet] 2009 [cited 2019 Jul 9];10:726-731. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19813695. [PubMed]
- 3.Ghei P. How to investigate drug use in health facilities. Selected drug use indicators. Health Policy. [Internet] 2004;1:73. Available from: https://apps.who.int/iris/handle/10665/60519.
- 4.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006. [DOI] [PMC free article] [PubMed]
- 5.Mazher Maqusood, Farhan Ahmad, Khan MK. A Study of Prescription Pattern in the Management of COPD in a Tertiary Care Hospital. Ann Int Med Dent Res. 2016;3:159–163. [Google Scholar]
- 6.Lucas AEM, Smeenk FWJM, Smeele IJ, van Schayck CP. Overtreatment with inhaled corticosteroids and diagnostic problems in primary care patients, an exploratory study. Fam Pract. [Internet] 2008 [cited 2019 Jul 9];2:86-91. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18304973. [DOI] [PubMed]
- 7.Diette GB, Dalal AA, D’souza AO, et al. Treatment patterns of chronic obstructive pulmonary disease in employed adults in the United States. Int J COPD. 2015. [DOI] [PMC free article] [PubMed]
- 8.Make B, Dutro MP, Paulose-Ram R, et al. Undertreatment of COPD: a retrospective analysis of US managed care and Medicare patients. Int J Chron Obstruct Pulmon Dis. [Internet]. 2012 [cited 2019 Jul 9];7:1-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22315517. [DOI] [PMC free article] [PubMed]
- 9.Melinda Ratini. A Newsletter on obstructive and restrictive lung disease. Reviewed by Melinda Ratini. WebMD. 2015.
- 10.Buist AS, Anzueto A, Calverley P, et al. GOLD – Global Initiative for Chronic Obstructive Lung Disease [Internet]. GOLD 2017 global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. http://goldcopd.org/gold-2017-globalstrategy- diagnosis-managementprevention- copd/ 2017.
- 11.Sin DD, Man SFP. Why are patients with chronic obstructive pulmonary disease at increased risk of cardiovascular diseases? The potential role of systemic inflammation in chronic obstructive pulmonary disease. Circulation. [Internet]. 2003 Mar 25 [cited 2019 Jul 9];11:1514-1519. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12654609. [DOI] [PubMed]
- 12.Barnes PJ. Chronic Obstructive Pulmonary Disease | Overview. 17th ed., Anthony S. Fauci, editor, Encyclopedia of Respiratory Medicine. Mc Graw Hill. 2006. pp. 429–439.
- 13.Niffy A, Vikneswari A, Sunny N, Sherlet G. Analysis of Prescribing Pattern Of Drugs In Obstructive Lung Diseases. EJPMR. 2017;2:710–714. [Google Scholar]
- 14.Gigi A, Sunil S, Hepzhiba P, et al. Assessment of Drug Prescribing Pattern in Chronic Obstructive Pulmonary Disease Patients at a Tertiarycare Hospital. J Pharm Res. 2015;0:45. [Google Scholar]
- 15. . COPD and Seasonal Allergies Related Lung Conditions. [Internet]. [cited 2017 Aug 19]. Available from: https://lunginstitute.com/lung-diseases/ copd/copd-and-seasonal-allergies/ 16. American Thoracic Society (ATS).
- 16.American Thoracic Society (ATS). Allergic disease worsens COPD symptoms and exacerbations. [Internet]. Science Daily.[cited 2016 May 10]. Available from: www.sciencedaily.com/releases/2013/05/130510075331.htm.
- 17.Adams SG, Pugh JA, Kazis LE, et al. Characteristics Associated with Sustained Abstinence from Smoking Among Patients with COPD. Am J Med. 2006;5:441–447. doi: 10.1016/j.amjmed.2005.09.055. [DOI] [PubMed] [Google Scholar]
- 18.Garshick E, Segal MR, Worobec TG, et al. Alcohol consumption and chronic obstructive pulmonary disease. Am Rev Respir Dis. [Internet] 1989 [cited 2019 Jul 9];2:373-378. Available from: http://www.ncbi.nlm.nih.gov/pubmed/2764374. [DOI] [PubMed]
- 19.Frantz S, Wollmer P, Dencker M, et al. Associations between lung function and alcohol consumption – assessed by both a questionnaire and a blood marker. Respir Med. [Internet] 2014 [cited 2019 Jul 9];1:114-121. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24064346. [DOI] [PubMed]
- 20.Unni A, et al. Drug utilization pattern in chronic obstructive pulmonary disease in patients at a tertiary care hospital. Int J Pharm Pharm Sci. [Internet] 2015;11:389-391. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L606756610%0Ahttp://sfx.hul.harvard.edu/sfx_local?sid=EMBASE&issn=09751491&id=doi:&atitle=Drug+utilization+pattern+in+chronic+obstructive+pulmonary+disease+inpatients+at+a+tertiary+c.
- 21.Dhand R, Dolovich M, Chipps B, et al. The role of nebulized therapy in the management of COPD: Evidence and recommendations. COPD J Chronic Obstr Pulm Dis. [Internet] 2012 [cited 2019 Jul 9];1:58-72. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22292598. [DOI] [PubMed]
- 22.Virchow JC, Crompton GK, Dal Negro R, et al. Importance of inhaler devices in the management of airway disease. Respir Med. [Internet] 2008 [cited 2019 Jul 9];1:10-19. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17923402. [DOI] [PubMed]
- 23.Vikneswari TTM. Drug Utilisation Pattern in Chronic Obstructive Pulmonary Disease in a Tertiary Care Teaching Hospital. Indo Am J Pharm Res. 2016;7:1. [Google Scholar]
- 24.Sunil S, Gigi A, Hepzhiba P, et al. Drug Utilization Evaluation in Chronic Obstructive Pulmonary Disease Patients – A Prospective Study. WJPPS. 2016;1:1133–1143. [Google Scholar]
- 25.Faheemuddin MD, Ramaiah B, Kiran SS. Evaluation of Medication-Adherence in COPD Patients and their Drug Utilization pattern. Chronic Obstr Pulm Dis. 2016;17:1–9. [Google Scholar]
- 26.Adil MS, Amer Khan M, Nematullah Khan M, et al. EMPADE study: Evaluation of medical prescriptions and adverse drug events in COPD patients admitted to intensive care unit. J Clin Diagnostic Res. 2015. [DOI] [PMC free article] [PubMed]
- 27.Basavaraju Thejur Jayadeva PP. A retrospective study on drug utilization in patients with acute exacerbation of bronchial asthma in adults at a tertiary teaching hospital in Bengaluru. Egypt J Chest Dis Tuberc. 2016;1:19–22. [Google Scholar]
- 28.Tanaka KI, Kurotsu S, Asano T, et al. Superiority of pulmonary administration of mepenzolate bromide over other routes as treatment for chronic obstructive pulmonary disease. Sci Re. 2014. [DOI] [PMC free article] [PubMed]
- 29.Corrado A, Rossi A. How far is real life from COPD therapy guidelines? An Italian observational study. Respir Med. [Internet] 2012 [cited 2019 Jul 9];7:989-997. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22483189. [DOI] [PubMed]
- 30.Sharif R, Cuevas CR, Wang Y, et al. Guideline adherence in management of stable chronic obstructive pulmonary disease. Respir Med. [Internet] 2013 [cited 2019 Jul 9];7:1046-1052. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23639271. [DOI] [PubMed]