Editor—The concept of an intubation box to contain aerosols has been proposed to address the risk of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission to healthcare professionals during airway management.1, 2, 3, 4 This barrier enclosure method has been widely promoted in the popular media.5 , 6 Although there is a need for innovation, it remains important to fully assess new concepts to ensure their fitness for purpose. To date, the intubation box has only been tested using a vertical cough model using a Sim-man1 mannikin (Laerdal Medical, Stavenger, Norway). We subjected such a box to objective airflow analysis of its performance with a human volunteer (more relevant to how it would be clinically deployed). We also collated perspectives from potential users in anaesthesia.
For airflow dynamic analysis, a barrier enclosure box of similar dimension and design to that proposed was placed over the head and upper torso of a healthy volunteer laying on an operating table in our simulation theatre (see Supplementary Fig. S1).1 Schlieren imaging (a passive imaging method for direct visualisation of refractive index changes) was performed around the box during both normal and deep exhalation and during coughing. The imaging focused on both the user side of the box (where there are two apertures for insertion of the healthcare professional's hands) and on the opposite side (which is open to allow positioning over the patient). A high-speed monochromatic camera (Phantom version 311 capable of 10,000 image s−1 frame rate with 1920×1080 pixel resolution; Bell Labs, Wayne, NJ, USA) was used to capture images and allow analysis. Testing was repeated three times.
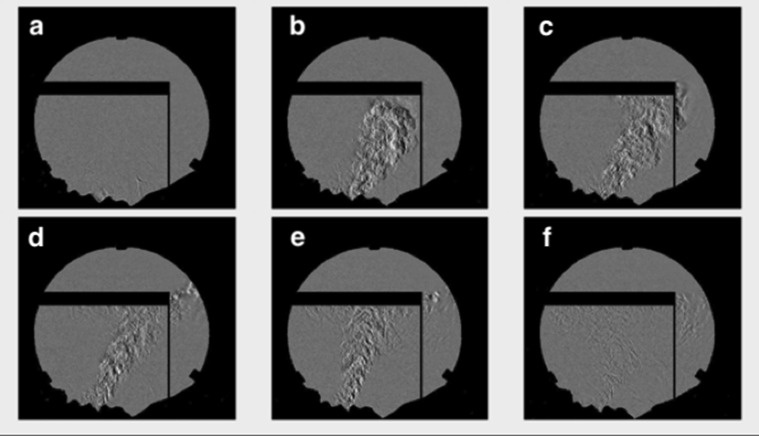
This assessment showed that substantial amounts of air moved out of the box and into the operating room during coughing (Fig. 1 ). This could be eliminated by placing a drape over this open side of the box such that, on repeat assessment, no airflow escaped the enclosure on that side. The analysis also identified some movement of air out of the box via the holes on the user side during deep exhalation by the volunteer but not during coughing.
Fig. 1.
Composite figure composed of stills from high-speed videography of schlieren imaging of a cough from a healthy volunteer lying on operating table with head within a barrier enclosure. (a) Still image immediately before cough with further images taken in series at (b) 5%, (c) 10%, (d) 40%, and (e) 75% of total cough duration, and (f) immediately upon cessation of air expiration as air continues to move around and out of the box.
User feedback from anaesthesiologists resulted in a clear consensus that the box, even with modification, did not add advantage over our current practice. Since the onset of the pandemic in Ireland, we have performed intubation only on patients under full neuromuscular blockade such that coughing is prevented at tracheal intubation. Tracheal extubation is done slowly and carefully under a simple plastic covering placed over the patient's face. The box was considered to create new complexity around procedures that ideally should be done quickly. There was also some concern that the box would concentrate infectious material confined within the box bringing added risk at the time of glove doffing and box cleaning.
There are differences in opinion regarding the use of rigid box constructs for airway management.7 Our analysis identified an easily implemented modification to the original design that might better protect the operating room and other staff from contamination. Although our imaging method does not measure droplet movement per se, it does show the air currents that carry particles. Our test method is closer to real-world conditions compared with previous methods used. The airflow dynamics associated with airway interventions (especially with infected patients and with positioning involving greater neck flexion8) are likely to be greater in magnitude and more variable in direction than with our healthy volunteer. Aside from rigid boxes and other solutions, there are other barrier constructs available commercially that more fully enclose the patient's head and upper torso (e.g. AerosolShield; Campbell Hill Ltd, Melksham, Wiltshire, UK). Disposable systems eliminate the need for cleaning and storage for reuse, an advantage for contagious patients. However, all designs compromise the movements of the healthcare provider such that specific training is likely necessary.9, 10, 11
Declarations of interest
The authors declare that they have no conflicts of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bja.2020.05.006.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Supplementary Fig S1.
Experimental set-up with (a) healthy volunteer positioned on an operating table with head and upper torso within the aerosol-containing box, and (b) alignment of schlieren imaging equipment to capture airflow characteristics
Dynamic schlieren imaging of footage related to the figure. If reading the pdf online, click on the image to view the video1
Dynamic schlieren imaging related to the figure. If reading the pdf online, click on the image to view the video2
References
- 1.Canelli R., Connor C.W., Gonzalez M., Nozari A., Ortega R. Barrier enclosure during endotracheal intubation. N Engl J Med. 2020;382:1957–1958. doi: 10.1056/NEJMc2007589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leyva Moraga F.A., Leyva Moraga E., Leyva Moraga F. Aerosol box, an operating room security measure in COVID-19 pandemic. World J Surg. 2020 doi: 10.1007/s00268-020-05542-x. Adv Access published on April 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Everington K. Taiwan News; 2020. Taiwanese doctor invents device to protect US doctors against coronavirus.https://www.taiwannews.com.tw/en/news/3902435 Available from: [Google Scholar]
- 4.Cubillos J., Querney J., Rankin A., Moore J., Armstrong K. A multipurpose portable negative air flow isolation chamber for aerosol-generating procedures during the COVID-19 pandemic. Br J Anaesth. 2020;27 doi: 10.1016/j.bja.2020.04.059. Adv Access Published April. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.News B. Coronavirus: NI firm helps develop shield for healthcare staff 2020. https://www.bbc.com/news/uk-northern-ireland-52303738 Available from:
- 6.Sampson C., Beckett A. Novel, inexpensive portable respiratory protection unit (PRPU) for healthcare workers. Clin Pract Cases Emerg Med. 2020;4:2. doi: 10.5811/cpcem.2020.4.47443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ortega R., Nozari A., Canelli R. More on barrier enclosure during endotracheal intubation. Reply N Engl J Med. 2020:382. doi: 10.1056/NEJMc2012960. Adv Access published on May 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Semler M.W., Janz D.R., Russell D.W. A multicenter, randomized trial of ramped position vs sniffing position during endotracheal intubation of critically ill adults. Chest. 2017;152:712–722. [Google Scholar]
- 9.Cook T., El-Boghdadly K., McGuire B. Consensus guidelines for managing the airway in patients with COVID-19: guidelines from the difficult airway society, the association of anaesthetists the intensive care society. The Fac Intensive Care Med Royal Coll Anaesthetists Anaesth. 2020;75:785–799. doi: 10.1111/anae.15054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kearsley R. Intubation boxes for managing the airway in patients with COVID-19. Anaesth Adv Access. 2020 doi: 10.1111/anae.15081. published on April 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Au Yong PS., Chen X. Reducing droplet spread during airway manipulation: lessons from the COVID-19 pandemic in Singapore. Br J Anaesth. 2020 doi: 10.1016/j.bja.2020.04.007. Adv Access published on April 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Dynamic schlieren imaging of footage related to the figure. If reading the pdf online, click on the image to view the video1
Dynamic schlieren imaging related to the figure. If reading the pdf online, click on the image to view the video2