Abstract
Objective
To assess the effectiveness of hydroxychloroquine in patients admitted to hospital with coronavirus disease 2019 (covid-19) pneumonia who require oxygen.
Design
Comparative observational study using data collected from routine care.
Setting
Four French tertiary care centres providing care to patients with covid-19 pneumonia between 12 March and 31 March 2020.
Participants
181 patients aged 18-80 years with documented severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pneumonia who required oxygen but not intensive care.
Interventions
Hydroxychloroquine at a dose of 600 mg/day within 48 hours of admission to hospital (treatment group) versus standard care without hydroxychloroquine (control group).
Main outcome measures
The primary outcome was survival without transfer to the intensive care unit at day 21. Secondary outcomes were overall survival, survival without acute respiratory distress syndrome, weaning from oxygen, and discharge from hospital to home or rehabilitation (all at day 21). Analyses were adjusted for confounding factors by inverse probability of treatment weighting.
Results
In the main analysis, 84 patients who received hydroxychloroquine within 48 hours of admission to hospital (treatment group) were compared with 89 patients who did not receive hydroxychloroquine (control group). Eight additional patients received hydroxychloroquine more than 48 hours after admission. In the weighted analyses, the survival rate without transfer to the intensive care unit at day 21 was 76% in the treatment group and 75% in the control group (weighted hazard ratio 0.9, 95% confidence interval 0.4 to 2.1). Overall survival at day 21 was 89% in the treatment group and 91% in the control group (1.2, 0.4 to 3.3). Survival without acute respiratory distress syndrome at day 21 was 69% in the treatment group compared with 74% in the control group (1.3, 0.7 to 2.6). At day 21, 82% of patients in the treatment group had been weaned from oxygen compared with 76% in the control group (weighted risk ratio 1.1, 95% confidence interval 0.9 to 1.3). Eight patients in the treatment group (10%) experienced electrocardiographic modifications that required discontinuation of treatment.
Conclusions
Hydroxychloroquine has received worldwide attention as a potential treatment for covid-19 because of positive results from small studies. However, the results of this study do not support its use in patients admitted to hospital with covid-19 who require oxygen.
Introduction
The World Health Organization declared pandemic of coronavirus disease 2019 (covid-19) due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is resulting in fatal pneumonia. Treatments are urgently needed to prevent hypoxaemic respiratory failure and death.1 Hydroxychloroquine has received worldwide attention after an in vitro study reported its potential activity against SARS-CoV-2,2 and small studies have released promising results. However, the effectiveness of hydroxychloroquine for treating covid-19 is the subject of serious debate.3 One uncontrolled French study included 26 hospital inpatients who were positive for SARS-CoV-2 PCR (polymerase chain reaction) on a nasopharyngeal swab. The study suggested that 600 mg/day of hydroxychloroquine was associated with a decrease in SARS-CoV-2 shedding and when combined with azithromycin it was more efficacious.4 However, another uncontrolled French study found no evidence of antiviral clearance with hydroxychloroquine and azithromycin in 11 patients admitted to hospital.5 A recent study randomised 62 patients into two parallel groups: a control group and a group receiving hydroxychloroquine (400 mg/day for five days). The study reported a shorter time to clinical recovery in the hydroxychloroquine group.6 However, these patients were not severely ill, the clinical endpoints were not clearly defined, and there was no stratification for comorbidities known to be associated with a poor outcome.6
Based on the results of these studies and the negligible cost and known safety profile of hydroxychloroquine in treating rheumatic conditions, this drug has been considered to be potentially useful in treating patients with covid-19. Hydroxychloroquine has attracted attention in social and mass media, and has also received US Food and Drug Administration approval for patients with severe covid-19.7 However, fears have increased about a shortage of this essential treatment for patients with rheumatic diseases, including systemic lupus erythematus,8 and questions have been raised about its safety in patients with covid-19.
Because of the lack of unbiased data and the urgency of determining the clinical efficacy of hydroxychloroquine to treat covid-19, we used observational data collected in a real world setting in patients admitted to hospital with covid-19 who required oxygen. We evaluated the clinical effectiveness of oral hydroxychloroquine at a daily dose of 600 mg on admissions to the intensive care unit or death by any cause. Secondary outcomes included the effectiveness of hydroxychloroquine in preventing acute respiratory distress syndrome, and in reducing the duration of oxygen requirement.
Methods
Study design and population
We used data collected from routine care to assess the effectiveness of hydroxychloroquine in patients admitted to hospital with covid-19 and who required oxygen.9 Physicians screened the electronic health records of all patients with covid-19 pneumonia admitted to four French tertiary hospitals between 12 March and 31 March 2020. Patients were eligible for this study if they were aged 18-80 years, had PCR confirmed SARS-CoV-2 infection (supplementary data 1), and required oxygen by mask or nasal prongs (corresponding to a WHO progression score of 5).
Exclusion criteria were the presence of a contraindication to hydroxychloroquine at 600 mg/day (including patients receiving dialysis); hydroxychloroquine treatment started before admission to hospital; treatment with another experimental drug for covid-19 (tocilizumab, lopinavir-ritonavir, or remdesivir) within 48 hours after admission; organ failure that required immediate admission to the intensive care unit or continuous care unit; acute respiratory distress syndrome at admission (defined by the need for non-invasive ventilation with provision of continuous positive airway pressure or invasive mechanical ventilation)10; discharge from the intensive care unit to standard care; decision to limit and stop active treatments prescribed at admission; and opposition to data collection by patients or their legal representative.
The study was performed in accordance with the declaration of Helsinki, as amended, and received approval by the appropriate IRB, which included an amendment for the extension of follow-up (No 2020_060, Hôpitaux Universitaires Henri-Mondor, AP-HP).
Treatment strategies
We compared two treatment strategies: starting hydroxychloroquine at a dose of 600 mg/day (treatment group) and no hydroxychloroquine treatment (control group). The dose was chosen after publication of the first study on hydroxychloroquine for treating covid-19.4 Patients in the treatment group could start treatment within a grace period of 48 hours after admission. The decision of whether or not to treat patients with hydroxychloroquine was based on local medical consensus and the clinicians’ own opinion of its effectiveness. The decision was made before patients were admitted to hospital and so their characteristics played no part. Supplementary data 1 provides additional information about the number of patients in each group in each hospital.
Start and end of follow-up
The start of follow-up (baseline or time zero) for each patient was the time of admission to hospital. All patients were followed up from baseline until death, loss to follow-up, or end of follow-up on 24 April 2020, whichever occurred first.
Outcomes
The primary outcome was survival without transfer to the intensive care unit at day 21. Secondary outcomes were overall survival, survival without acute respiratory distress syndrome, weaning from oxygen, and discharge from hospital to home or rehabilitation (all at day 21). Patients who received hydroxychloroquine had QT prolongation assessed by a 12 lead electrocardiogram and corrected for heart rate by Bazett’s or Fredericia’s formula at the start of treatment and for three to five days after.
Statistical analysis
An inverse probability of treatment weighting approach was used to balance the differences in baseline variables between treatment groups.11 12 A non-parsimonious multivariable logistic regression model was constructed to estimate each patient’s probability of receiving hydroxychloroquine given their baseline covariates (that is, the propensity score). Variables of the propensity score model were planned and prespecified before outcome analyses. Several variables were included: age, sex, comorbidities (presence of chronic respiratory insufficiency during oxygen treatment, or asthma, cystic fibrosis, or any chronic respiratory disease likely to result in decompensation during a viral infection; heart failure (New York Heart Association class III or IV); chronic kidney disease; liver cirrhosis with Child-Pugh class B or more; personal history of cardiovascular disease (hypertension, stroke, coronary artery disease, or cardiac surgery); insulin dependent diabetes mellitus, or diabetic microangiopathy or macroangiopathy; treatment with immunosuppressive drugs, including anticancer chemotherapy; uncontrolled HIV infection or HIV infection with CD4 cell counts <200/µL; or a haematological malignancy); body mass index (≥30 or not); third trimester of pregnancy; treatment by angiotensin converting enzyme inhibitors or angiotensin receptor blockers13; time since symptom onset; and severity of condition at admission (percentage of lung affected: ≥50% or not; presence of confusion; respiratory frequency; oxygen saturation without oxygen; oxygen flow; systolic blood pressure; and C reactive protein level).
All variables included in the propensity score model reflected knowledge available at baseline. Standardised differences were examined to assess balance, with a threshold of 10% designated to indicate clinically meaningful imbalance.14
Crude survival rates were computed by using the Kaplan-Meier method. Cox proportional hazards models were used to compute inverse probability of treatment weighting hazard ratios. Inverse probability of treatment weighting estimates of the relative risk were computed for binary outcomes. Outcomes are presented in the total population and in the subgroup of patients with a better prognosis at admission, estimated by a quick sepsis related organ failure assessment score less than 2.15 16
Our causal contrast of interest was the per protocol effect, and we compared participants who received hydroxychloroquine within 48 hours of admission with those who did not receive the drug. Because some patients subsequently received hydroxychloroquine after 48 hours, we specified two additional comparisons. Firstly, mimicking an intention-to-treat analysis: all patients eligible for the study were analysed, and those who received hydroxychloroquine after 48 hours were analysed in the control group. Secondly, mimicking an as-treated analysis: patients who received hydroxychloroquine after 48 hours were analysed in the treatment group.
We performed sensitivity analyses to assess the robustness of findings. Firstly, we conducted a trimmed analysis that was truncated at the region of common support, defined as the overlap between the range of propensity scores in the treatment group and the control group. Patients with propensity scores outside the region of common support were excluded from this analysis. Secondly, to account for time dependent bias, we performed an analysis in which all patients from the control group who reached the primary outcome (transfer to intensive care unit or death) during the grace period were randomly assigned to one of the two groups, given that their observational data were compatible with both groups at the time of the event.17
Missing baseline variables were handled by multiple imputation by chained equations using the other variables available. All statistical analyses were performed with the R statistical package version 3.6.1 or later (R Foundation for Statistical Computing, https://www.R-project.org/).
Patient and public involvement
Neither patients nor the public were involved in the conception or conduct of the study.
Results
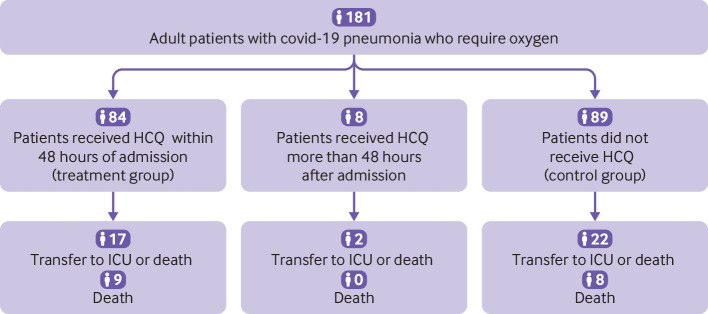
Among the 181 patients eligible for analysis, 84 received hydroxychloroquine within 48 hours of admission, eight received hydroxychloroquine more than 48 hours after admission, and 89 did not receive hydroxychloroquine (fig 1). To assess a per protocol effect, our main analysis compared the 84 participants who received hydroxychloroquine within 48 hours (treatment group) with the 89 who did not receive the drug (control group). The median age of patients was 60 years (interquartile range 52-68 years), and 72% were men. Patients in the treatment group had fewer comorbidities, except for liver cirrhosis. The median interval between symptom onset and admission to hospital was 7 days (interquartile range 5-10 days). Overall, initial severity was well balanced between the groups, except for confusion on admission (0 in the treatment group v 6 (7%) in the control group). Azithromycin was administered to 18% of the participants in the treatment group versus 29% in the control group; amoxicillin and clavulanic acid was given to 52% versus 28%, respectively (excluding cointerventions in patients transferred to the intensive care unit; table 1). No patients received antiviral or anti-inflammatory treatments, including steroids or non-steroidal anti-inflammatory drugs (non-steroidal anti-inflammatory drugs are not used as antipyretics in adults in France and are considered to be contraindicated for covid-19) before transfer to the intensive care unit. Supplementary data 1 details hydroxychloroquine use in the four French study hospitals.
Fig 1.
Study flowchart. Covid-19=coronavirus disease 2019; HCQ=hydroxychloroquine; ICU=intensive care unit
Table 1.
Baseline personal and clinical characteristics of patients with coronavirus disease 2019 assigned to hydroxychloroquine (treatment group) or no hydroxychloroquine (control group). Values are percentages (absolute numbers) unless stated otherwise
| Characteristics | Total (n=173) | Treatment group (n=84) | Control group (n=89) |
|---|---|---|---|
| Personal and clinical data | |||
| Median (interquartile range) age (years; n=173) | 60 (52-68) | 59 (48-67) | 62 (54-69) |
| Men (n=173) | 72 (125) | 77 (65) | 67 (60) |
| Comorbidities (n=173 except as otherwise specified): | |||
| Chronic respiratory disease (including asthma) | 11 (19) | 6 (5) | 16 (14) |
| Chronic heart failure (NYHA class III or IV) | 4 (6) | 1 (1) | 6 (5) |
| Cardiovascular diseases (including hypertension) | 51 (89) | 45 (38) | 57 (51) |
| Diabetes requiring insulin (n=172) | 9 (15) | 5 (4) | 12 (11) |
| Chronic kidney failure | 5 (9) | 1 (1) | 9 (8) |
| Liver cirrhosis (Child-Pugh class B or more) | 1 (1) | 1 (1) | 0 |
| Immunosuppression | 12 (20) | 10 (8) | 14 (12) |
| Body mass index >30 (n=167) | 26 (44) | 25 (21) | 27 (23) |
| Treatment with ACEIs or ARBs (n=173) | 30 (52) | 31 (26) | 29 (26) |
| Covid-19 data | |||
| Median (interquartile range) time from symptom onset to admission (days; n=173) | 7 (5-10) | 8 (6-10) | 7 (3-10) |
| Confusion on admission (n=171) | 4 (6) | 0 (0) | 7 (6) |
| Median (interquartile range) respiratory rate (per min; n=165) | 26 (22-30) | 26 (24-32) | 26 (20-30) |
| Median (interquartile range) oxygen saturation (without oxygen; n=170) | 92 (89-94) | 92 (89-94) | 92 (90-94) |
| Median (interquartile range) oxygen flow at admission (L/min; n=173) | 2 (2-4) | 3 (2-4) | 2 (2-3) |
| Median (interquartile range) systolic blood pressure (mm Hg; n=172) | 128 (114-142) | 124 (112-138) | 130 (116-146) |
| Neutrophil count >8000/mm3 (n=172) | 14 (24) | 21 (17) | 8 (7) |
| Lymphocyte count <500/mm3 (n=172) | 9 (16) | 7 (6) | 11 (10) |
| C reactive protein >40 mg/L (n=170) | 85 (145) | 91 (76) | 80 (69) |
| Percentage of lung affected on CT scan >50% (n=135*) | 16 (22) | 22 (14) | 11 (8) |
| Azithromycin treatment (n=173) | 24 (41) | 18 (15) | 29 (26) |
| Amoxicillin-clavulanic acid treatment (n=173) | 40 (69) | 52 (44) | 28 (25) |
ACEI=angiotensin converting enzyme inhibitor; ARB=angiotensin receptor blocker; CT=computed tomography; NYHA=New York Heart Association.
Thirty eight patients did not have computed tomography at admission.
Propensity score model development
Propensity scores ranged from 0.09 to 0.95 in the treatment group and from 0.01 to 0.91 in the control group, with 96% in the region of common support (propensity scores 0.09-0.91; supplementary data 2). After inverse probability of treatment weighting was applied, 15 of the 19 covariates in the planned propensity score had weighted standardised differences below 10%; four covariates (confusion on admission, chronic kidney disease, chronic heart failure (New York Heart Association class III or IV), and liver cirrhosis (Child-Pugh class B or more)) exceeded the threshold (supplementary data 3). These results were owing to the absence of confusion on admission in the treatment group (compared with six patients with confusion in the control group); only one patient had chronic kidney disease in the treatment group (compared with eight in the control group); only one patient had chronic heart failure in the treatment group (compared with five in the control group); and only one patient had liver cirrhosis in the treatment group (compared with no patients in the control group). These four variables were therefore not included in the final propensity score model (supplementary data 4).
Follow-up and outcomes
Median follow-up for surviving patients was 32.5 days; three patients (one in the treatment group and two in the control group; 2%) were lost to follow-up after being discharged in good health and without oxygen. Two other patients had a follow-up of only 20 days. At day 21, 17 of 173 (10%) patients had died (nine in the treatment group and eight in the control group).
In the non-weighted analyses, among the 173 patients in the two treatment groups, the rate of survival without transfer to intensive care at 21 days was 80% in the treatment group compared with 75% in the control group (hazard ratio 0.8, 95% confidence interval 0.4 to 1.5; fig 2). The overall survival rate at 21 days was 89% in the treatment group and 91% in the control group (1.2, 0.5 to 3.0). The rate of survival without acute respiratory distress syndrome was 70% in the treatment group and 74% in the control group (1.2, 0.7 to 2.2; table 2, supplementary data 5 and 6).
Fig 2.
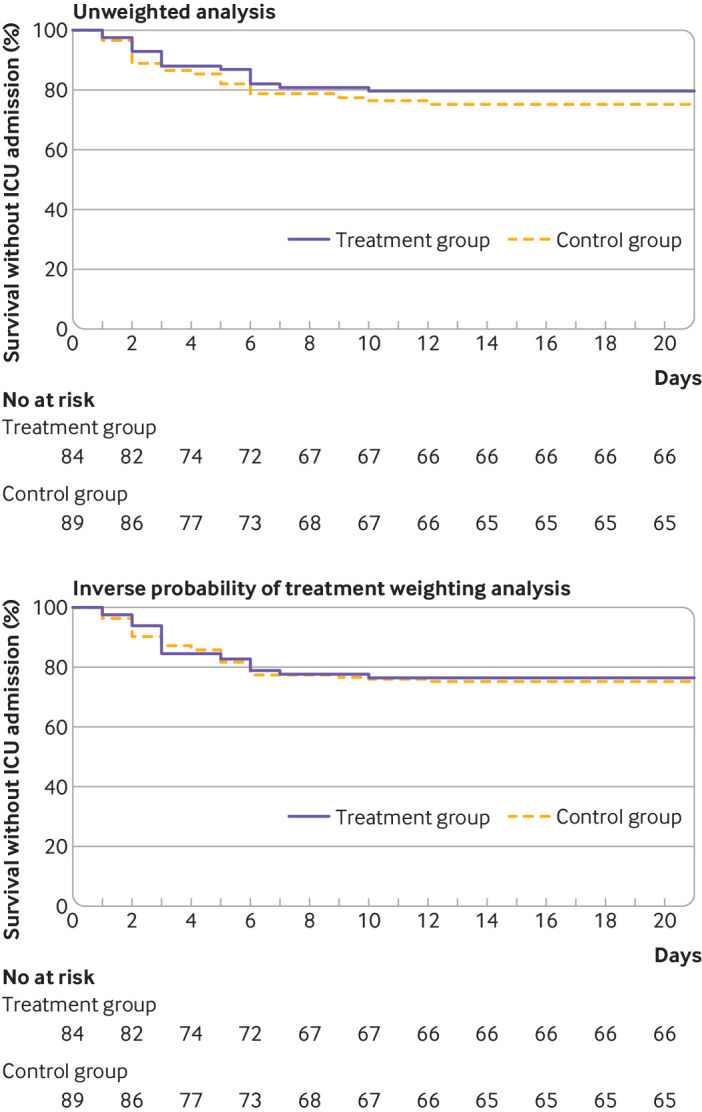
Kaplan-Meier curves for survival without transfer to intensive care in unweighted sample (top panel) and sample used for inverse probability of treatment weighting (bottom panel). A multivariable logistic regression model was constructed to estimate each patient’s probability of receiving hydroxychloroquine given their baseline covariates (that is, the propensity score: variables in model included age, sex, and comorbidities). ICU=intensive care unit
Table 2.
Primary and secondary outcomes at day 21 in patients with coronavirus disease 2019 assigned to hydroxychloroquine (treatment group) or no hydroxychloroquine (control group)
| Outcomes | No of events | Ratio (95% CI) | IPTW ratio (95% CI)* | |
|---|---|---|---|---|
| Treatment group (n=84) | Control group (n=89) | |||
| Survival without transfer to intensive care unit | 17 | 22 | HR 0.8 (0.4 to 1.5) | wHR 0.9 (0.4 to 2.1) |
| Overall survival (No of deaths) | 9 | 8 | HR 1.2 (0.5 to 3.0) | wHR 1.2 (0.4 to 3.3) |
| Survival without acute respiratory distress syndrome | 25 | 23 | HR 1.2 (0.7 to 2.2) | wHR 1.3 (0.7 to 2.6) |
| Oxygen weaning | 66 | 66 | RR 1.1 (0.9 to 1.3) | wRR 1.1 (0.9 to 1.3) |
| Discharge from hospital to home or rehabilitation | 67 | 71 | RR 1.0 (0.9 to 1.2) | wRR 0.9 (0.8 to 1.2) |
HR=hazard ratio; IPTW=inverse probability of treatment weighting; RR=relative risk; wHR=weighted hazard ratio; wRR=weighted relative risk.
Weighted hazard ratios, weighted relative risks, and 95% confidence intervals were obtained by inverse probability treatment weighting. A multivariable logistic regression model was constructed to estimate each patient’s probability of receiving hydroxychloroquine given their baseline covariates (that is, the propensity score: variables in model included age, sex, and comorbidities)
At day 21, 79% of patients in the treatment group had been weaned from oxygen compared with 74% in the control group (relative risk 1.1, 95% confidence interval 0.9 to 1.3). Furthermore, 80% of patients in both groups had been discharged to home or rehabilitation (1.0, 0.9 to 1.2; table 2). None of the 15 patients who received a combination of hydroxychloroquine and azithromycin was transferred to intensive care and none died. Additionally, these patients had fewer severe signs at admission compared with patients who received hydroxychloroquine without azithromycin (oxygen flow: 2 L/min, interquartile range 1.25-4 v 3 L/min, 2-6; respiratory frequency: 25 per min, interquartile range 22-33 v 28 per min, 24-32; percentage of lung affected >50%: 13% v 17%). Finally, 26 patients received azithromycin without hydroxychloroquine. Among these patients, six were admitted to the intensive care unit and five died.
In the inverse probability of treatment weighting analyses that took imbalance at baseline into account, among the 173 patients in the two groups, the survival rate without transfer to the intensive care unit at day 21 was 76% in the treatment group and 75% in the control group (weighted hazard ratio 0.9, 95% confidence interval 0.4 to 2.1; fig 2). The overall survival rate at day 21 was 89% in the treatment group and 91% in the control group (1.2, 0.4 to 3.3). The rate of survival without acute respiratory distress syndrome at day 21 was 69% in the treatment group compared with 74% in the control group (1.3, 0.7 to 2.6; table 2, supplementary data 5 and 6).
At day 21, 82% of patients in the treatment group had been weaned from oxygen compared with 76% in the control group (weighted relative risk 1.1, 95% confidence interval 0.9 to 1.3). Furthermore, 76% of patients in the treatment group had been discharged to home or rehabilitation compared with 82% in the control group (0.9, 0.8 to 1.2; table 2). All sensitivity analyses were consistent with the principal analysis and found that hydroxychloroquine had no effect on any outcome (supplementary data 7).
Our results also suggested that patients with fewer symptoms and better prognosis at admission did not respond to hydroxychloroquine (quick sepsis related organ failure assessment score less than 2: n=73 in the treatment group and n=76 in the control group): weighted hazard ratio 1.1 (95% confidence interval 0.5 to 2.6) for survival without transfer to intensive care unit; weighted hazard ratio 1.8 (0.6 to 5.9) for overall survival; weighted hazard ratio 1.6 (0.7 to 3.3) for survival without acute respiratory distress syndrome; weighted relative risk 1.0 (0.9 to 1.2) for oxygen weaning; weighted relative risk 0.9 (0.7 to 1.1) for discharge to home or rehabilitation.
Finally, adding the eight patients who received hydroxychloroquine treatment more than 48 hours after admission (for a population of 181) and including them in the treatment group (mimicking an as-treated analysis) or in the control group (mimicking an intention-to-treat analysis) did not change the results (weighted hazard ratio 1.0 (95% confidence interval 0.4 to 2.1), and 0.9 (0.5 to 1.9) for the primary outcome, respectively; supplementary data 8 and 9).
Safety
Of the 84 patients who received hydroxychloroquine within the first 48 hours, eight (10%) experienced electrocardiographic modifications that required discontinuation of hydroxychloroquine at a median of 4 days (interquartile range 3-9 days) after it began, which is in accordance with French national guidelines. Among these patients, seven had a corrected QT interval prolongation of more than 60 ms (including one patient with corrected QT interval prolongation >500 ms). One patient who received no other drugs that might have interfered with cardiac conduction presented a first degree atrioventricular block after two days of hydroxychloroquine treatment. One patient in whom hydroxychloroquine was started five days after admission (control group) was transferred to intensive care two days later. This patient was then prescribed lopinavir and ritonavir and developed left bundle branch block on day 8. None of these patients was concomitantly treated with azithromycin.
Discussion
We report a comparative study that uses real world data collected from routine care to assess the efficacy and safety of hydroxychloroquine in a population of 181 patients admitted to hospital with covid-19 hypoxaemic pneumonia. We found that hydroxychloroquine treatment at 600 mg/day added to standard care was not associated with a reduction of admissions to the intensive care unit or death 21 days after hospital admission compared with standard care alone. Additionally the rate of survival without acute respiratory distress syndrome did not increase. These results were unchanged when the eight patients who received hydroxychloroquine after 48 hours were included in the analysis, regardless of whether they were analysed in the treatment group (mimicking an as-treated analysis) or in the standard of care (control) group (mimicking an intention-to-treat analysis).
Our population of patients admitted to hospital because they required oxygen is similar to that reported by other studies, and the proportion of patients transferred to the intensive care unit was similar to that reported in a Chinese cohort of 138 patients admitted to hospital with covid-19 pneumonia.18 The clinical features of included patients were also consistent with other reports, with a predominance of men and patients with cardiovascular comorbidities or obesity.18 19 Apart from azithromycin, the patients in this study did not receive any other drugs; in particular, potential confounders such as antiviral and anti-inflammatory treatments, including steroids, before admission to intensive care.
It could be argued that the timing of antiviral treatment initiation might be critical in reducing SARS-Cov-2 viral load.20 In the recent lopinavir-ritonavir trial, a post hoc subgroup analysis suggested that lopinavir-ritonavir might have a clinical benefit when started earlier than 12 days after symptom onset.21 In our study, however, patients had a short median time from symptom onset to inclusion (seven days) and were treated with hydroxychloroquine within 48 hours of admission. We also found that viral ribonucleic acid for SARS-CoV-2 was detectable among all patients at inclusion, showing active viral shedding. Nevertheless, we cannot rule out the possibility that hydroxychloroquine could be beneficial at symptom onset; this question must be assessed in future trials.
A previous report4 indicates that hydroxychloroquine should have been expected to show some antiviral efficacy. We did not check the results of subsequent SARS-Cov-2 PCR in this study and therefore cannot reach a conclusion about its potential efficacy for decreasing viral shedding. Although this might seem to be a limitation, we used robust clinical outcomes; that is, death, admission to the intensive care unit, acute respiratory distress syndrome, and oxygen requirement, which are substantially more clinically relevant.
Progression of covid-19 pneumonia in the second week of illness is associated with a so called cytokine storm,19 22 which is thought to be responsible for the clinical worsening of many patients. Most of the patients included in this study had an inflammatory syndrome defined by a C reactive protein level higher than 40 mg/L, which suggests that a cytokine storm syndrome had already begun.23 Therefore, drugs that decrease virus shedding could be inadequate at this stage, which is why many anti-inflammatory drugs are currently being tested, such as tocilizumab and corticosteroids. However, hydroxychloroquine could still be effective in this setting because of its immunomodulatory properties, which include regulation of the production of proinflammatory cytokines such as interleukin 2, interleukin 1, interleukin 6, and tumour necrosis factor α,24 and endosomal inhibition of toll-like receptors, which have a major role in innate immune response.25 Nonetheless, hydroxychloroquine treatment showed no effectiveness in this specific population.
Finally, hydroxychloroquine blocks the KCNH2 encoded hERG/Kv11.1 potassium channel and can potentially prolong the corrected QT interval, with potentially severe consequences, such as sudden cardiac death and cardiac arrhythmia in patients with covid-19.26 In addition to prolongations of corrected QT intervals, we observed two other major cardiac events in this study, and the French national drug agency has reported three deaths potentially related to hydroxychloroquine since its promotion as a potential treatment for covid-19. Although hydroxychloroquine is considered safe in the context of systemic lupus erythematosus, these adverse events might be explained by the use of high dose hydroxychloroquine in patients older than 75 years with renal impairment and frequent drug interactions. We cannot rule out the possibility that these cardiac effects attributed to hydroxychloroquine were caused by covid-19, especially given electrocardiograms were unavailable during follow-up in the control group. However, these possible side effects of hydroxychloroquine plus the negative clinical results of this study argue against the widespread use of hydroxychloroquine in patients with covid-19 pneumonia.
Limitations of this study
Our study has several limitations. Firstly, although we used robust methods and statistical techniques to draw causal inferences from observational data, treatment was not randomly assigned and potential unmeasured confounders could bias our results. Secondly, four potentially important prognostic variables could not be balanced in the propensity score model because none or only one patient in the treatment group presented with these variables. Accordingly, caution is required in interpreting these results, especially for overall mortality for which only a few events were observed. Nevertheless, this limitation did favour the hydroxychloroquine group and the absence of any difference between treated and untreated patients further strengthens our conclusions. Thirdly, we did not take a centre effect into account in the propensity score model because the number of patients treated with hydroxychloroquine in centres was unbalanced (some centres treated all their patients, whereas others did not). Nevertheless, that the decision to treat or not treat patients with hydroxychloroquine was based on local medical consensus rather than on their characteristics should reduce this bias. Fourthly, our sample was limited to the number of eligible patients available at the time of analysis; we cannot rule out the possibility that our findings are owing to a lack of power. Fifthly, because we included only patients admitted to hospital, we cannot reach a conclusion about the possible efficacy of hydroxychloroquine in preventing covid-19 or in preventing severe forms of the disease. Finally, our study was not designed to assess the efficacy of the association of hydroxychloroquine and azithromycin, and no conclusion about its efficacy can be reached. Further research is ongoing.
Conclusions
In patients admitted to hospital with covid-19 pneumonia who require oxygen, hydroxychloroquine treatment seemed to have no effect on reducing admissions to intensive care or deaths at day 21 after hospital admission. Additionally, hydroxychloroquine treatment did not have any effect on survival without acute respiratory distress syndrome at day 21 after hospital admission. These results do not support the use of hydroxychloroquine in these patients.
What is already known on this topic
Treatments are urgently needed to prevent respiratory failure and deaths from coronavirus disease 2019 (covid-19)
An in vitro study has reported potential activity by hydroxychloroquine against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) responsible for covid-19
Small studies of hydroxychloroquine treatment in patients with covid-19 have reported promising results
What this study adds
In patients admitted to hospital with covid-19 pneumonia who require oxygen, hydroxychloroquine seemed to have no effect on reducing admissions to intensive care or deaths at day 21 after hospital admission
Hydroxychloroquine treatment did not have any effect on survival without acute respiratory distress syndrome at day 21 after hospital admission
The results of this study do not support the use of hydroxychloroquine in these patients
Acknowledgments
We thank Ada Clarke, Moez Jallouli, Hicham Kardaoui, Kamil Chitour, Laetitia Languille, Mouhamed Dieng, Jean-Daniel Lelièvre, Chloé Delille, and Louise Mimville.
Web extra.
Extra material supplied by authors
Web appendix: Supplementary material
Contributors: VTT and MR contributed equally to the work. MMah conceptualised the paper. MMah, MR, AC, RP, CG, SG, RL, TAS, FS, MMat, MK, EC, BT, CM, PL, YS, MMic, EP, NC, NR, VdL, LM, FXL, EA, PM, EF, CO, SK, and NCC collected data. VTT, JD, EP, and PR analysed data. JMP performed SARS-Cov2 RT-PCR. MMah, VTT, PR, BG, and NCC interpreted the results and wrote the article. All authors contributed to revision of the final version of the manuscript, approved the final version submitted, and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. MMah acts as guarantor for the work. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: No funding received for the present study.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: no support from any organisation for the submitted work; EA reports personal fees from GBT, personal fees from Hemanext, outside the submitted work; NC reports non-financial support from Novartis, non-financial support from Mylan, non-financial support from Therakos, outside the submitted work; AC reports non-financial support from Sanofi, non-financial support from Janssen, outside the submitted work; NCC reports grants from GlaxoSmithKline (GSK), grants from UCB, outside the submitted work; EC has nothing to disclose; JD has nothing to disclose; SG reports personal fees and non-financial support from Gilead Sciences, personal fees and non-financial support from ViiV Healthcare SAS, other from Sanofi Aventis France, personal fees, non-financial support and other from Pfizer SAS, personal fees from Icomed, other from OVERCOME, personal fees and non-financial support from MSD France, non-financial support from Mylan Medical SAS, non-financial support from CSL Behring SA, personal fees and non-financial support from Janssen-Cilag, non-financial support from Longueur D’Ondes, non-financial support from Octapharma France, outside the submitted work; VdL reports non-financial support from Eumedica, non-financial support from Fresenuis Kabi, outside the submitted work; EF reports personal fees from Novartis, outside the submitted work; BG reports grants and personal fees from Amgen, personal fees from Novartis, grants and personal fees from Roche, personal fees from Grifols, personal fees from LFB, outside the submitted work; CG has nothing to disclose; SK reports personal fees from Accelerate Diagnostics, other from Astellas, grants, personal fees and other from bioMérieux, personal fees and other from MSD, other from Pfizer, personal fees from Menarini, outside the submitted work; MK has nothing to disclose; PL has nothing to disclose; FXL has received personal fees from Gilead and MSD; RL reports non-financial support from Eumedica SA, non-financial support from Gilead Sciences, non-financial support from MSD France, non-financial support from Pfizer PFE France, non-financial support from Sanofi Aventis France, non-financial support from Astellas Pharma, non-financial support from CSL Behring SA, non-financial support from Ipsen Pharma, outside the submitted work; MMah reports grants from GSK, other from GSK, other from Morphosys, personal fees from LFB, personal fees from Amgen, personal fees from Grifols, outside the submitted work; MMat reports personal fees from A+A, personal fees from CSL Behring, personal fees from ELIVIE, personal fees from Genzyme, personal fees from Vivactis, outside the submitted work; PM has nothing to disclose; MMic reports personal fees from Alexion, personal fees from Amgen, personal fees from Novartis, personal fees from Argenx, personal fees from Sanofi-Bioverativ, outside the submitted work; CM reports non-financial support from Novartis, outside the submitted work; LM reports personal fees from Janssen Cilag, non-financial support from Swedish orphan biovitrum, non-financial support from LFB, non-financial support from Shire, non-financial support from Grifols, outside the submitted work; CO reports non-financial support from MSD, non-financial support from Janssen, non-financial support from CSL Behring, non-financial support from Gilead, outside the submitted work; RP has nothing to disclose; JMP reports personal fees from Abbvie, personal fees from Gilead, personal fees from Merck, personal fees from Siemens Healthcare, outside the submitted work; EP has nothing to disclose; PR reports personal fees from Inato, outside the submitted work; NR reports grants and personal fees from Boehringer Ingelheim, grants and personal fees from Novartis, personal fees from Teva, personal fees from GSK, personal fees from AstraZeneca, personal fees from Chiesi, grants and personal fees from Pfizer, personal fees from Sanofi, personal fees from Zambon, outside the submitted work; MR reports personal fees from Novartis Pharma SAS, personal fees from Bristol Myers Squibb, personal fees from Swedish Orphan Biovitrum, outside the submitted work; FS reports personal fees from Gilead Sciences, outside the submitted work; YS reports non-financial support from AstraZeneca, non-financial support from Novartis Pharma, non-financial support from Bristol Myers Squibb, non-financial support from Sanofi Aventis France, non-financial support from Shire France, non-financial support from Chugai Pharma France, non-financial support from Pfizer SAS, non-financial support from Swedish Orphan Biovitrum, non-financial support from CSL Behring SA, outside the submitted work; TAS reports personal fees from Bayer, non-financial support from LFB, non-financial support from Medexact, non-financial support from Mundipharma, outside the submitted work; BT reports personal fees from AstraZeneca, personal fees from Roche Chugai, personal fees from GSK, grants from Bristol Myers Squibb, grants from Lilly, grants from Vifor Pharma, outside the submitted work; VTT has nothing to disclose; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: This study conformed to the ethical guidelines of the 1975 Declaration of Helsinki and was approved by the ethics committee of Henri-Mondor Hospital, AP-HP (No 2020_060). Patients were informed by letter of the use of their data.
Data sharing: The data are available on request.
Dissemination to related patient and public communities: We plan to issue a press release on official publication of this manuscript and disseminate our findings through social media outlets, to ensure the results of the study have a broad public outreach.
The lead author (MMah) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned have been explained.
References
- 1. Kupferschmidt K, Cohen J. Race to find COVID-19 treatments accelerates. Science 2020;367:1412-3. 10.1126/science.367.6485.1412. [DOI] [PubMed] [Google Scholar]
- 2. Yao X, Ye F, Zhang M, et al. In vitro antiviral activity and projection of optimized dosing design of hydroxychloroquine for the treatment of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Clin Infect Dis 2020. 10.1093/cid/ciaa237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kim AHJ, Sparks JA, Liew JW, et al. COVID-19 Global Rheumatology Alliance† A rush to judgment? Rapid reporting and dissemination of results and its consequences regarding the use of hydroxychloroquine for covid-19. Ann Intern Med 2020;30. 10.7326/M20-1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gautret P, Lagier J-C, Parola P, et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents 2020;105949:105949. 10.1016/j.ijantimicag.2020.105949. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 5. Molina JM, Delaugerre C, Goff JL, et al. No evidence of rapid antiviral clearance or clinical benefit with the combination of hydroxychloroquine and azithromycin in patients with severe covid-19 infection. Med Mal Infect 2020;S0399077X20300858 10.1016/j.medmal.2020.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chen Z, Hu J, Zhang Z, et al. Efficacy of hydroxychloroquine in patients with COVID-19: results of a randomized clinical trial. Epidemiology 2020. 10.1101/2020.03.22.20040758. [DOI] [Google Scholar]
- 7. Lenzer J. Covid-19: US gives emergency approval to hydroxychloroquine despite lack of evidence. BMJ 2020;369:m1335. 10.1136/bmj.m1335. [DOI] [PubMed] [Google Scholar]
- 8. Yazdany J, Kim AHJ. Use of hydroxychloroquine and chloroquine during the covid-19 pandemic: what every clinician should know. Ann Intern Med 2020;31. 10.7326/M20-1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hernán MA, Robins JM. Using big data to emulate a target trial when a randomized trial is not available. Am J Epidemiol 2016;183:758-64. 10.1093/aje/kwv254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ranieri VM, Rubenfeld GD, Thompson BT, et al. ARDS Definition Task Force Acute respiratory distress syndrome: the Berlin Definition. JAMA 2012;307:2526-33. 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 11. Lunceford JK, Davidian M. Stratification and weighting via the propensity score in estimation of causal treatment effects: a comparative study [correction in: Stat Med 2017;36:2320]. Stat Med 2004;23:2937-60. 10.1002/sim.1903. [DOI] [PubMed] [Google Scholar]
- 12. Robins JM, Hernán MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology 2000;11:550-60. 10.1097/00001648-200009000-00011. [DOI] [PubMed] [Google Scholar]
- 13. Patel AB, Verma A. Covid-19 and angiotensin-converting enzyme inhibitors and angiotensin receptor blockers: what is the evidence? JAMA 2020;24. 10.1001/jama.2020.4812. [DOI] [PubMed] [Google Scholar]
- 14. Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med 2015;34:3661-79. 10.1002/sim.6607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 2016;315:801-10. 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Freund Y, Lemachatti N, Krastinova E, et al. French Society of Emergency Medicine Collaborators Group Prognostic accuracy of sepsis-3 criteria for in-hospital mortality among patients with suspected infection presenting to the emergency department. JAMA 2017;317:301-8. 10.1001/jama.2016.20329. [DOI] [PubMed] [Google Scholar]
- 17. Hernán MA, Schisterman EF, Hernández-Díaz S. Invited commentary: composite outcomes as an attempt to escape from selection bias and related paradoxes. Am J Epidemiol 2014;179:368-70. 10.1093/aje/kwt283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020;7. 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497-506. 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gonçalves A, Bertrand J, Ke R, et al. Timing of antiviral treatment initiation is critical to reduce SARS-Cov-2 viral load. medRxiv [Preprint] 2020. 10.1101/2020.04.04.20047886 [DOI] [PMC free article] [PubMed]
- 21. Cao B, Wang Y, Wen D, et al. A trial of lopinavir-ritonavir in adults hospitalized with severe covid-19. N Engl J Med 2020;18. 10.1056/NEJMoa2001282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054-62. 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lescure F-X, Bouadma L, Nguyen D, et al. Clinical and virological data of the first cases of COVID-19 in Europe: a case series. Lancet Infect Dis 2020;27:S1473-3099(20)30200-0. 10.1016/S1473-3099(20)30200-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Costedoat-Chalumeau N, Dunogué B, Morel N, Le Guern V, Guettrot-Imbert G. Hydroxychloroquine: a multifaceted treatment in lupus. Presse Med 2014;43:e167-80. 10.1016/j.lpm.2014.03.007 [DOI] [PubMed] [Google Scholar]
- 25. Kuznik A, Bencina M, Svajger U, Jeras M, Rozman B, Jerala R. Mechanism of endosomal TLR inhibition by antimalarial drugs and imidazoquinolines. J Immunol 2011;186:4794-804. 10.4049/jimmunol.1000702. [DOI] [PubMed] [Google Scholar]
- 26.Giudicessi JR, Noseworthy PA, Friedman PA, Ackerman MJ. Urgent guidance for navigating and circumventing the QTc-prolonging and torsadogenic potential of possible pharmacotherapies for coronavirus disease 19 (COVID-19). Mayo Clin Proc 2020. 10.1016/j.mayocp.2020.03.024 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Web appendix: Supplementary material