Abstract
We examined the relationship between social isolation and health among parents and their adolescent children. Data came from the 2014 Family Life, Activity, Sun, Health, and Eating Study (FLASHE), a cross-sectional internet study from the National Cancer Institute. Parents and their adolescent children (ages 12–17) completed surveys about demographics, physical activity, and diet; analyses include all dyads in which at least one member provided information for any of the analyzed variables (N = 1851). Actor Partner Interdependence Models in Mplus with demographic covariates tested whether parent and adolescent perceived social isolation (2 items from the UCLA Loneliness Scale) were associated with each person’s self-reported health. Most dyads included a mother (38% mother–daughter, 36% mother–son). Most parents were non-Hispanic White (69%), married/partnered (77%), and reported household income below $100,000 (79%). Both social isolation and self-reported health were significantly correlated between parents and their adolescent children (Pearson correlation = .38 for isolation, .32 for health). There were negative associations between parent isolation and parent health, adolescent isolation and adolescent health, and parent isolation and adolescent health (all ps < .05), but no association between adolescent isolation and parent health. The finding that parents’ social isolation was linked to lower self-reported health not only for themselves but also for their adolescent children highlights the importance of addressing social isolation in clinical social work practice. Family interventions, or interventions to reduce adults’ negative social cognitions or promote social connections, may improve health for both adults and their adolescent children.
Keywords: Social isolation, Adolescents, Dyadic analysis, Actor Partner Interdependence Model, Family systems theory
Introduction
Eradicating social isolation is one of the Social Work Grand Challenges issued by the American Academy for Social Work and Social Welfare; their working paper begins with the blunt statement, “Social isolation is a potent killer” (Lubben et al. 2015, p. 3). Healthy People 2020, the blueprint of health goals for the United States, has as an overarching goal to “create social and physical environments that promote good health for all” (National Center for Health Statistics 2016, p. 3). These goals are based on substantial evidence linking social isolation to poor mental and physical health. Social isolation as a determinant of health and well-being has also gained attention in the popular press, with former U.S. Surgeon General Vivek Murthy taking on the “loneliness epidemic” as one of his signature issues (Murthy 2017).
The link between social relationships and health among adults has long been noted (House et al. 1988). A meta-analysis found that social isolation and loneliness were both associated with increased risk of mortality; effects were stronger in samples with an average age under 65 (Holt-Lunstad et al. 2015). The term social isolation is often used to reflect objective structural factors (e.g., living alone), whereas the term loneliness is used to reflect subjective perceptions (e.g., Jong-Gierveld et al. 2006); the commonly used UCLA Loneliness Scale (Russell et al. 1978) includes items measuring both feelings of loneliness and self-perceived isolation. Self-perceived social isolation has been linked to physical and mental health outcomes including higher blood pressure, poor sleep, and increased mortality risk (Cacioppo and Cacioppo 2014). Social isolation is also hypothesized to contribute to the opioid epidemic, one of the gravest public health threats facing the United States today (Dasgupta et al. 2018).
Most prior research on social isolation and loneliness has focused on older adults (Brody 2017; Poscia et al. 2018), but these issues are also problematic for younger people, including adolescents (Brody 2017; Heinrich and Gullone 2006; Qualter et al. 2010; Williams and Braun 2019; Bessaha et al. 2019). Especially given the intense role of peer, parent–adolescent, and romantic relationships in the social development of adolescents, feelings of loneliness or isolation can be especially difficult during this life stage (Arnett 2014; Laser and Nicotera 2011; Steinberg and Morris 2001). Understanding adolescents’ worldviews and interpretations of social interactions can be useful in clinical social work practice and promote mental health and well-being into adulthood (Korkiamäki 2014).
Experiencing social isolation or loneliness during adolescence has been associated with health consequences later in adult life (Caspi et al. 2006; Goosby et al. 2013). In a longitudinal cohort study following children for 20 years, Caspi et al. (2006) found that socially isolated children and adolescents had significantly poorer health outcomes in adulthood even after controlling for factors such as low childhood socioeconomic status and childhood overweight. These findings suggest that experiences of social isolation early in life has “persistent and cumulative effects” on poor health outcomes in adulthood (Caspi et al. 2006, p. 810). Additionally, Goosby et al. (2013) reported that adolescent loneliness is a risk factor for experiencing less-than-optimal self-rated health and cardiovascular disease in adulthood. Findings also revealed that having parental support can counteract the negative impacts of feeling lonely, which is consistent with family systems theory (Whitchurch and Constantine 2009) and demonstrates “linked lives between adolescents and their parents and peers” (Goosby et al. 2013, p. 9). Lonely adolescents who experienced higher levels of support were at greater risk of poorer self-rated health in early adulthood compared to non-lonely adolescents, which supports the notion that those who experience loneliness may find it more difficult to perceive social support as helpful (Goosby et al. 2013).
Social isolation and loneliness in adolescence have been associated with psychological health issues, including depression (Asher and Paquette 2003; Goosby et al., 2013; Qualter et al., 2010). Adolescents’ self-perceived experiences of peer exclusion, not being part of a peer group, or “being an outsider” have been associated with emotional stress, including loneliness, as well as hopelessness and sadness (Korkiamäki 2014). Research suggests that some types of social media use may increase social isolation and feelings of loneliness, especially in relation to experiences of cyberbullying and Facebook depression (O’Keeffe and Clarke-Pearson 2011) or passive social media use (e.g., scrolling through timelines and feeds, as opposed to active use creating face-to-face interactions) (Chatterjee 2018). At the same time, technology also offers the opportunity to forge or strengthen social relationships (Carvalho et al. 2015; Zilberstein 2015).
In clinical practice, it is important to understand how the social and physical health of family members are interconnected, and how intervening with one person may affect others (Van Hook 2008). Theories of family systems (Bowen 1993; Whitchurch and Constantine 2009) depict the health and wellbeing of family members as interconnected. According to Bowen’s family systems theory (1993), the emotional functioning of the family unit can influence the health of all family members. However, very little empirical work has explicitly tested the interrelatedness of social isolation and health within parent–adolescent dyads. The purpose of this study was to investigate the interrelationship between parent and adolescent social isolation and health. We hypothesized that self-reported health and social isolation measures would both be correlated between parents and their adolescent children. We hypothesized that each person’s social isolation would be associated with their own health, and that within dyads one person’s isolation would be associated with the other person’s health.
Methods
Data come from the 2014 Family Life, Activity, Sun, Health, and Eating (FLASHE) Study (Oh et al. 2017; Nebeling et al. 2017), a cross-sectional study conducted by the National Cancer Institute (NCI) in contract with Westat, Inc. Parents and their children ages 12–17 were recruited through a consumer opinion panel to complete online surveys about demographics, physical activity, and diet. Parents were eligible if they were 18 or older and had a child age 12–17 living with them 50% or more of the time. FLASHE was approved by the Westat, Inc. and NCI Special Studies institutional review boards. All procedures followed were in accordance with ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Parents provided consent for themselves and their adolescents; adolescents provided assent (Oh et al. 2017).
Of 5027 dyads screened, a total of 1945 enrolled. Participants were asked to complete two surveys, one focused on diet and the other focused on physical activity. The order of the two surveys was assigned randomly at the dyad level, and demographic information was collected as part of whichever survey was given first (Nebeling et al. 2017; Oh et al. 2017). Social isolation was assessed as part of the physical activity survey, and self-reported health was assessed as part of the demographic module. The current analyses include all dyads in which at least one member completed either demographic information or the physical activity survey (N = 1851).
Measures
Details about FLASHE survey development and testing are provided by Nebeling et al. (2017). Perceived social isolation was measured using the mean of two items from the UCLA Loneliness Scale (Russell et al. 1978); both items are included in a shortened 3-item version of the scale developed for survey research (Hughes et al. 2004), and both load on the same factor in adolescents (Shevlin et al. 2015) and adults (Hughes et al. 2004). These items read I feel left out and I feel isolated from others, with response options never, rarely, sometimes, often, and always. Cronbach’s alpha for these items was .91 for both parents and adolescents in this sample.
Self-rated health was measured with one item: In general, would you say your health is… with response options excellent, very good, good, fair, and poor. This item was coded 1–5 such that increasing values reflect higher levels of self-reported health. Such global measures of health status have been found to be strongly associated with outcomes such as mortality; authors of a review of 27 studies using such measures concluded that “the global rating represents an irreplaceable dimension of health status” (Idler and Benyamini 1997, p. 34).
Control variables included household income (dichotomized into under $100,000 or $100,000 and above), parent self-reported race and ethnicity (dichotomized into non-Hispanic White vs. other race or ethnicity; hereafter referred to as “race”), parent marital status (dichotomized into married or member of a couple vs. not), age of parent and adolescent (categorical). Because adolescent race was highly correlated with parent race (polychoric correlation = .83, p < .001), adolescent race was omitted from the models. Because self-rated health had only five response categories, it was treated as categorical in the main analyses.
Analysis Plan
Descriptive analyses were conducted in IBM SPSS Version 24 (Armonk, NY, 2016). Pearson correlations were calculated for self-reported health and social isolation score to determine the interdependence of both measures within dyads. The Actor Partner Interdependence Model (APIM; Kenny et al. 2006) was used to model the interdependence of dyadic data. The APIM allows for analysis of actor effects (the association of each individual’s characteristics with their own measures on other variables) and partner effects (the association between one person’s characteristics and the other person’s measures on other variables) (see Fig. 1). To estimate the main APIM, we used structural equation modeling in Mplus Version 8.2 (Los Angeles, CA, 1998–2018) with the robust maximum likelihood (MLR) estimator. Multiple group analyses to test for group differences used the robust weighted least squares (WLSMV) estimator. Because standardized coefficients can be misleading in dyads with distinguishable members (e.g., parents and children) (Kenny et al. 2006), unstandardized coefficients are provided in the results section.
Fig. 1.
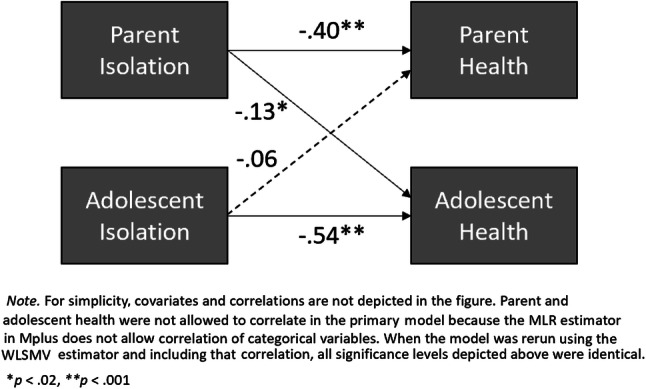
Actor Partner Interdependence Model showing unstandardized coefficients for parent–adolescent dyads (N = 1851) in the FLASHE study
Missing Data
The primary APIM analysis includes the 1851 dyads in which at least one member provided information for any of the variables included in the model. Participants in the main analysis with partially missing data were retained through the estimator’s handling of missing data. For the multiple-group analysis, those participants with missing data on the grouping variables or on parent age were not included. Thus, 73 dyads in which parents did not report race and one dyad in which they did not report age were excluded from the race multiple group analysis, whereas 195 dyads in which either parent or adolescent did not report sex were excluded from the dyad-type analysis. In the multiple group analyses, the additional partially missing data were handled by (a) estimating the variance of parent and adolescent ages; (b) regressing other covariates on parent and adolescent age. These two steps allowed missing data to be estimated for participants via the missing data estimation algorithm for the MLR estimator.
Results
Table 1 presents information about the sample. Approximately two-thirds of the dyads included a mother: 38% were mother–daughter, 36% were mother–son, 14% were father–son, and 12% were father–daughter. Parents were predominantly non-Hispanic White (69%) and married or in a couple (77%), with most between the ages of 35 and 59. Most parents (79%) reported household income under $100,000.
Table 1.
Sample characteristics
| Variable | % (N) or mean (SD) |
|---|---|
| Dyad type (N = 1656) | |
| Mother–daughter | 38% (632) |
| Mother–son | 36% (599) |
| Father–son | 14% (226) |
| Father–daughter | 12% (199) |
| Self-reported race of parent (N = 1778) | |
| Non-Hispanic Black | 18% (314) |
| Non-Hispanic White | 69% (1229) |
| Hispanic | 7% (130) |
| Other race | 6% (105) |
| Parent age (N = 1793) | |
| 18–34 | 11% (202) |
| 35–44 | 44% (781) |
| 45–59 | 42% (758) |
| 60 or older | 3% (52) |
| Adolescent age (N = 1682) | |
| 12 | 13% (224) |
| 13 | 20% (336) |
| 14 | 17% (280) |
| 15 | 18% (305) |
| 16 | 20% (331) |
| 17 | 12% (206) |
| Parent marital status (N = 1779) | |
| Married/in a couple | 77% (1374) |
| Not married or in a couple | 23% (405) |
| Household income (N = 1772) | |
| < $100,000 | 79% (1406) |
| $100,000 or above | 21% (366) |
Table 2 presents parent and adolescent responses to individual items assessing social isolation and health. Mean scores on the social isolation scale were 2.1 (SD = 1.0) for both parents and adolescents; this mean score falls between 2 (rarely) and 3 (sometimes) on the response scale. Mean scores on the self-reported health item were 3.6 (SD = .9) for parents (that is, between good and very good) and 4.1 (SD = .9) for adolescents (that is, between very good and excellent). The parent–adolescent correlation was .38 (p < .001) for social isolation and .32 (p < .001) for health status, indicating interdependence for each measure within dyads.
Table 2.
Parent and adolescent responses to survey items about perceived isolation and health in the FLASHE study
| Variable | % (N) or mean (SD) |
|---|---|
| Parent feels left out (N = 1793) | |
| Never | 33% (592) |
| Rarely | 32% (575) |
| Sometimes | 26% (459) |
| Often | 8% (135) |
| Always | 2% (32) |
| Parent feels isolated from others (N = 1787) | |
| Never | 37% (668) |
| Rarely | 28% (498) |
| Sometimes | 23% (418) |
| Often | 9% (166) |
| Always | 2% (37) |
| Parent health (N = 1785) | |
| Excellent | 16% (289) |
| Very good | 41% (726) |
| Good | 31% (557) |
| Fair | 10% (185) |
| Poor | 2% (28) |
| Adolescent feels left out (N = 1654) | |
| Never | 32% (527) |
| Rarely | 33% (540) |
| Sometimes | 26% (429) |
| Often | 7% (113) |
| Always | 3% (45) |
| Adolescent feels isolated from others (N = 1649) | |
| Never | 40% (655) |
| Rarely | 30% (488) |
| Sometimes | 21% (352) |
| Often | 6% (102) |
| Always | 3% (52) |
| Adolescent health (N = 1679) | |
| Excellent | 41% (693) |
| Very good | 38% (643) |
| Good | 15% (251) |
| Fair | 5% (84) |
| Poor | 1% (8) |
Figure 1 depicts the results of the primary Actor Partner Interdependence Model. For both parents and adolescents, there were significant actor effects of social isolation on health, meaning that each person’s own social isolation score was negatively associated with their own health status score (coefficient for parents = − .40, p < .001; coefficient for adolescents = − .54, p < .001). We observed significant partner effects for the association between a parent’s social isolation and their adolescent’s health (coefficient = − .13, p = .014), meaning that higher parental social isolation was associated with poorer adolescent self-rated health. The association between adolescent social isolation and parent health was also in a negative direction, but it was not significant (p = .268).
Multiple group models were tested to determine whether these parameters differed across (a) dyad type (based on sex of parent and adolescent, for four types) and (b) ethnicity (non-Hispanic White versus other races). Constraining these paths to be equal did not produce worse model fit (ps > .07, where very small ps and at least p < .05 indicates worse fit). Therefore, the paths in Fig. 1 appear to be relatively consistent across dyad type and race.
Discussion
Our study provides further evidence of the “linked lives” of adolescents and their parents (Goosby et al. 2013, p. 9). We found partial support for our hypotheses: For each individual, there was a statistically significant relationship between their social isolation and their own health. Furthermore, parents’ social isolation was negatively associated with their adolescents’ health, but the inverse was not the case; the relationship between an adolescent’s social isolation and their parent’s health was not statistically significant. Our findings are consistent with family systems theories (Bowen 1993; Whitchurch and Constantine 2009) and suggest that helping parents address their own social isolation may affect not only their own health but also the social and physical health of others in the household.
This work has several implications for clinical social work practice. Our findings add to the evidence that social isolation is associated with one’s own health and are consistent with calls to screen patients for social factors such as loneliness in health care settings (Lubben et al. 2015). Interventions may be effective in helping individuals and families address social isolation. A recent review found that interventions based on cognitive-behavioral therapy (CBT), delivered either in individual or group therapy, had the largest effects on loneliness in adults, but that interventions designed to improve social support may also be effective (Cacioppo et al. 2015). More work is needed to find effective interventions to address social isolation among adolescents. A meta-analysis of interventions to reduce loneliness found no interventions targeting adolescents (Masi et al. 2011). Targeted social support interventions have been piloted for particular adolescent populations including adolescents with disabilities (Stewart et al. 2011) and youth who are homeless (Stewart et al. 2009), but less is known about effective interventions for the general population. Qualter et al. (2015) argue that CBT-based interventions shown to be effective in adults could be modified to address adolescents’ maladaptive social cognitions while taking into account their developmental stage and particular sources of loneliness. When evaluating support interventions, it is important to investigate both the effects on target individual(s) and also potential broader spillover effects experienced by family members.
Interdisciplinary, cross-sector collaboration may engage not only individuals but also families and communities in eradicating social isolation, and social workers may be uniquely positioned to lead such collaborations due to their community knowledge and their experience working with complex systems (Lubben et al. 2015). Multisector policy solutions may promote positive social relationships and health within families and across the life span. Such initiatives may include delivering social-emotional skills trainings in schools, promoting civic engagement, and creating public places to allow people to congregate (Umberson and Montez 2010). Innovations in social media and other technologies may allow adolescents, adults, and their extended families to build meaningful social connections (Carvalho et al. 2015; Lim et al. 2019; Lubben et al. 2015; Zilberstein 2015).
This study has both strengths and limitations. We analyzed data from over 1800 parent–adolescent pairs in dyadic analyses to assess relationships between social isolation and health. One key limitation is that the cross-sectional nature of the study precluded us from examining processes over time, including the direction of relationships (i.e., whether social isolation affects health, or the reverse). Our measures were limited, with dichotomized or categorical measures of demographics, a one-item measure of self-reported health, and a two-item measure of social isolation. Future longitudinal work with more fine-grained measures will allow for a deeper examination the intergenerational interplay of social isolation and health over time. In addition, future research should examine whether these associations hold among populations with more racial, ethnic, and economic diversity.
Conclusion
Social workers have a long history of working with families, and family-specific approaches can promote health and support all family members in navigating their social environment (Bent-Goodley 2017). A biopsychosocial perspective is useful in social work practice in terms of exploring how individuals influence and are influenced by their families. The interdependent nature of social isolation and health among parent–adolescent dyads in this study suggests that family-level interventions may prove effective for improving health and wellbeing for multiple members of a household. In addition, if clinical social workers identify parental social isolation while delivering services to adolescents, referrals for social work services can be made for parents. Clinicians who treat adults should also recognize that interventions to address parental social isolation may potentially improve the health and wellbeing of entire families.
Acknowledgements
The authors would like to acknowledge the data source: National Cancer Institute 2014 Family Life, Activity, Sun, Health and Eating (FLASHE) Survey Data. Rockville, MD: U.S. Department of Health and Human Services, National Cancer Institute, 2018. FLASHE datasets are publicly available at http://cancercontrol.cancer.gov/brp/hbrb/flashe.html. Dr. Thompson’s time was supported in part by a Mentored Research Scholar Grant in Applied and Clinical Research from the American Cancer Society (MRSG-19-086-01-CPPB).
Biographies
Tess Thompson
is a Research Assistant Professor in the Brown School of Social Work, Washington University in St. Louis.
Thomas L. Rodebaugh
is a Professor and Director of Clinical Training in the Psychological and Brain Sciences Department, Washington University in St. Louis.
Melissa L. Bessaha
is an Assistant Professor in the School of Social Welfare, Stony Brook University.
Erika L. Sabbath
is an Assistant Professor in the Boston College School of Social Work.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Arnett JJ. Adolescence and emerging adulthood. Boston, MA: Pearson; 2014. [Google Scholar]
- Asher SR, Paquette JA. Loneliness and peer relations in childhood. Current Directions in Psychological Science. 2003;12(3):75–78. doi: 10.1111/1467-8721.01233. [DOI] [Google Scholar]
- Bent-Goodley TB. Challenges facing today’s families and why social work matters. Social Work. 2017;62(3):197–199. doi: 10.1093/sw/swx031. [DOI] [PubMed] [Google Scholar]
- Bessaha ML, Sabbath EL, Morris Z, Malik S, Scheinfeld L. A systematic review of loneliness interventions among non-elderly adults. Clinical Social Work Journal. 2019 doi: 10.1007/s10615-019-00724-0. [DOI] [Google Scholar]
- Bowen M. Family therapy in clinical practice. New York: Jason Aronson; 1993. [Google Scholar]
- Brody, J. (2017). The surprising effects of loneliness on health. Retrieved from https://www.nytimes.com/2017/12/11/well/mind/how-loneliness-affects-our-health.html.
- Cacioppo JT, Cacioppo S. Social relationships and health: The toxic effects of perceived social isolation. Social and Personality Psychology Compass. 2014;8(2):58–72. doi: 10.1111/spc3.12087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo S, Grippo AJ, London S, Goossens L, Cacioppo JT. Loneliness: Clinical import and interventions. Perspectives on Psychological Science. 2015;10(2):238–249. doi: 10.1177/1745691615570616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carvalho J, Francisco R, Relvas AP. Family functioning and information and communication technologies: How do they relate? A literature review. Computers in Human Behavior. 2015;45:99–108. doi: 10.1016/j.chb.2014.11.037. [DOI] [Google Scholar]
- Caspi A, Harrington H, Moffitt TE, Milne BJ, Poulton R. Socially isolated children 20 years later: Risk of cardiovascular disease. Archives of Pediatrics and Adolescent Medicine. 2006;160(8):805–811. doi: 10.1001/archpedi.160.8.805. [DOI] [PubMed] [Google Scholar]
- Chatterjee, R. Americans are a lonely lot, and young people bear the heaviest burden. Retrieved from https://www.npr.org/sections/health-shots/2018/05/01/606588504/americans-are-a-lonely-lot-and-young-people-bear-the-heaviest-burden.
- Dasgupta N, Beletsky L, Ciccarone D. Opioid crisis: No easy fix to its social and economic determinants. American Journal of Public Health. 2018;108(2):182–186. doi: 10.2105/AJPH.2017.304187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goosby B, Bellatorre A, Walsemann K, Cheadle J. Adolescent loneliness and health in early adulthood. Sociological Inquiry. 2013;83:505–536. doi: 10.1111/soin.12018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinrich LM, Gullone E. The clinical significance of loneliness: A literature review. Clinical Psychology Review. 2006;26(6):695–718. doi: 10.1016/j.cpr.2006.04.002. [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspectives on Psychological Science. 2015;10(2):227–237. doi: 10.1177/1745691614568352. [DOI] [PubMed] [Google Scholar]
- House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241(4865):540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A short scale for measuring loneliness in large surveys: Results from two population-based studies. Research on Aging. 2004;26(6):655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38(1):21–37. doi: 10.2307/2955359. [DOI] [PubMed] [Google Scholar]
- Jong-Gierveld JD, van Tilburg TG, Dykstra PA. Loneliness and social isolation. In: Vangelisti A, Perlman D, editors. The Handbook of Personal Relationships. Cambridge: Cambridge University Press; 2006. pp. 485–500. [Google Scholar]
- Kenny DA, Kashy DA, Cook WL. Dyadic data analysis. New York, NY: Guilford Press; 2006. [Google Scholar]
- Korkiamäki R. Rethinking loneliness: A qualitative study about adolescents’ experiences of being an outsider in peer group. Open Journal of Depression. 2014;3:125–135. doi: 10.4236/ojd.2014.34016. [DOI] [Google Scholar]
- Laser JA, Nicotera N. Working with adolescents: A guide for practitioners. New York, NY: Guilford Press; 2011. [Google Scholar]
- Lim MH, Gleeson JF, Rodebaugh TL, Eres R, Long KM, Casey K, et al. A pilot digital intervention targeting loneliness in young people with psychosis. Social Psychiatry and Psychiatric Epidemiology. 2019 doi: 10.1007/s00127-019-01681-2. [DOI] [PubMed] [Google Scholar]
- Lubben, J., Gironda, M., Sabbath, E. Kong, J., & Johnson, C. (2015). Social isolation presents a grand challenge for social work (Grand Challenges for Social Work Initiative Working Paper No. 7). Cleveland, OH: American Academy of Social Work and Social Welfare.
- Masi CM, Chen HY, Hawkley LC, Cacioppo JT. A meta-analysis of interventions to reduce loneliness. Personality and Social Psychology Review. 2011;15(3):219–266. doi: 10.1177/1088868310377394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murthy, V. (2017). Work and the loneliness epidemic. Retrieved from https://hbr.org/cover-story/2017/09/work-and-the-loneliness-epidemic.
- National Center for Health Statistics. (2016). Chapter I: Introduction. Healthy People 2020 Midcourse Review. Hyattsville, MD.
- Nebeling LC, Hennessy E, Oh AY, Dwyer LA, Patrick H, Blanck HM, et al. The FLASHE study: Survey development, dyadic perspectives, and participant characteristics. American Journal of Preventive Medicine. 2017;52(6):839–848. doi: 10.1016/j.amepre.2017.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oh AY, Davis T, Dwyer LA, Hennessy E, Li T, Yaroch AL, Nebeling LC. Recruitment, enrollment, and response of parent–adolescent dyads in the FLASHE study. American Journal of Preventive Medicine. 2017;52(6):849–855. doi: 10.1016/j.amepre.2016.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Keeffe GS, Clarke-Pearson K. The impact of social media on children, adolescents, and families. Pediatrics. 2011;127(4):800–804. doi: 10.1542/peds.2011-0054. [DOI] [PubMed] [Google Scholar]
- Poscia A, Stojanovic J, La Milia DI, Duplaga M, Grysztar M, Moscato U, et al. Interventions targeting loneliness and social isolation among the older people: An update systematic review. Experimental Gerontology. 2018;102:133–144. doi: 10.1016/j.exger.2017.11.017. [DOI] [PubMed] [Google Scholar]
- Qualter P, Brown SL, Munn P, Rotenberg KJ. Childhood loneliness as a predictor of adolescent depressive symptoms: An 8-year longitudinal study. European Child and Adolescent Psychiatry. 2010;19(6):493–501. doi: 10.1007/s00787-009-0059-y. [DOI] [PubMed] [Google Scholar]
- Qualter P, Vanhalst J, Harris R, Van Roekel E, Lodder G, Bangee M, et al. Loneliness across the life span. Perspectives on Psychological Science. 2015;10(2):250–264. doi: 10.1177/1745691615568999. [DOI] [PubMed] [Google Scholar]
- Russell D, Peplau LA, Ferguson ML. Developing a measure of loneliness. Journal of Personality Assessment. 1978;42(3):290–294. doi: 10.1207/s15327752jpa4203_11. [DOI] [PubMed] [Google Scholar]
- Shevlin M, Murphy S, Murphy J. The latent structure of loneliness: Testing competing factor models of the UCLA Loneliness Scale in a large adolescent sample. Assessment. 2015;22(2):208–215. doi: 10.1177/1073191114542596. [DOI] [PubMed] [Google Scholar]
- Steinberg L, Morris AS. Adolescent development. Annual Review of Psychology. 2001;52(1):83–110. doi: 10.1146/annurev.psych.52.1.83. [DOI] [PubMed] [Google Scholar]
- Stewart M, Barnfather A, Magill-Evans J, Ray L, Letourneau N. Brief report: An online support intervention: Perceptions of adolescents with physical disabilities. Journal of Adolescence. 2011;34(4):795–800. doi: 10.1016/j.adolescence.2010.04.007. [DOI] [PubMed] [Google Scholar]
- Stewart M, Reutter L, Letourneau N, Makwarimba E. A support intervention to promote health and coping among homeless youths. Canadian Journal of Nursing Research. 2009;41(2):54–77. [PubMed] [Google Scholar]
- Umberson D, Montez JK. Social relationships and health: A flashpoint for health policy. Journal of Health and Social Behavior. 2010;51(1_suppl):S54–S66. doi: 10.1177/0022146510383501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Hook MP. Social work practice with families: A resiliency-based approach. Chicago: Lyceum Books; 2008. [Google Scholar]
- Whitchurch GG, Constantine LL. Systems Theory. In: Boss P, Doherty WJ, LaRossa R, Schumm WR, Steinmetz SK, editors. Sourcebook of family theories and methods. Boston, MA: Springer; 2009. pp. 325–355. [Google Scholar]
- Williams SE, Braun B. Loneliness and social isolation: A private problem, a public issue. Journal of Family & Consumer Sciences. 2019;111(1):7–14. doi: 10.14307/JFCS111.1.7. [DOI] [Google Scholar]
- Zilberstein K. Technology, relationships and culture: Clinical and theoretical implications. Clinical Social Work Journal. 2015;43(2):151–158. doi: 10.1007/s10615-013-0461-2. [DOI] [Google Scholar]


